ABSTRACT
Problems in growth and undernutrition manifest in early infancy, with suboptimal breastfeeding and inadequate complementary feeding remaining strong risk factors for chronic undernutrition in infants. No published studies exist on educational interventions to improve infant feeding practices among refugees or displaced persons in low and middle-income (LMIC) settings. The objective of this study was to create and pilot educational materials for home-based counseling of refugee mothers along the Thailand–Myanmar border to improve appropriate infant feeding and water, sanitation, and hygiene (WASH) behaviors. Mothers of infants received counseling on appropriate infant feeding and WASH practices on a monthly basis for a total of six months from infant age three months until nine months. Educational materials were designed to feature a basic script for health workers and photos of locally available, appropriate foods. Of the 20 mothers participating in this pilot, infant feeding and WASH behaviors improved within 1 to 2 months of the first visit, including exclusive breastfeeding, minimum acceptable diet, and safe disposal of infant stool. This pilot demonstrates improvement in maternal infant feeding and WASH practices in a small set of refugee mothers, providing evidence for counseling measures to improve infant health in vulnerable populations.
Trial registration: ClinicalTrials.gov identifier: NCT00840502.
Responsible Editor
Jennifer Stewart Williams, Umeå University, Sweden
Background
Recent analyses reveal that problems in growth and undernutrition manifest in early infancy [Citation1–Citation4]. Suboptimal breastfeeding and inadequate complementary feeding remain strong risk factors for chronic undernutrition in infants [Citation1]. There is a growing number of studies demonstrating benefit and impact of counseling and educational interventions to improve breastfeeding and complementary feeding for infant nutrition [Citation5–Citation10]. However, in spite of displaced persons having reached record numbers nearing 68.5 million people globally [Citation11], publications to date have only focused on preserving breastfeeding in crisis situations [Citation12,Citation13]. No published studies exist on educational interventions to improve infant feeding practices among refugees or displaced persons in low and middle-income (LMIC) settings. In addition, there is limited information available on creation of materials for populations with low literacy rates. This study piloted home-based, one-on-one counseling for a largely illiterate population of refugee mothers in Mae La refugee camp in Thailand to validate potentially, effective counseling techniques for improved maternal infant feeding and water, sanitation, and hygiene (WASH) practices. This paper highlights methods and materials used for the counseling intervention and reports the results of the pilot.
Methods
Study population
This pilot was conducted with recently delivered women attending the Shoklo Malaria Research Unit (SMRU) clinic in Mae La refugee camp (MLA) from October 2013 to June 2014. The SMRU MLA clinic provides antenatal , obstetric, pediatric, and general medical care to refugees. Refugees are predominantly of Burman or Karen ethnicity who identify as Buddhist or Christian. Muslims constitute a significant minority within the MLA refugee camp. Importantly, nutrition education was performed in a refugee camp where meal rations were provided to this food secure population.
Study design
Mother–infant pairs from a cohort evaluating the impact of malaria in pregnancy on fetal growth were selected to receive a home-based, one-on-one counseling intervention. Mothers with term, healthy infants aged two months at the time of recruitment were approached in the SMRU MLA clinic and, after giving consent to participate, received monthly household visits from infant age three months onwards for a total of six months. House visits took 30 minutes or less and were conducted by a study nurse previously unknown to the participants. The study nurse would record mothers’ practices through direct questions and/or observations, following World Health Organization (WHO) recommendations and definitions for appropriate infant feeding [Citation14] and additional indicators to assess appropriate WASH practices (). In addition to recording behaviors of interest according to WHO definitions, monthly surveys collected information on household expenditures, food resources accessed, and food items purchased the week prior. Feeding practices and meal preparation were observed when possible. Each home visit would culminate with the study nurse counseling mothers on appropriate behaviors for feeding, sanitation, and hygiene. Statistical analysis focused on behavior change over time.
Table 1. Outcomes of interest for feeding, hygiene, and sanitation behaviors in the 24 hours prior to cross-sectional survey (WHO 2007).
Educational materials: ‘The Healthy Baby Flipbook’
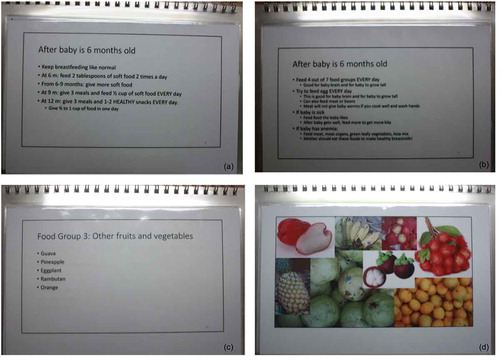
Researchers (AH, VC) prepared and provided the study nurse with a flipbook featuring a script in basic English and photos of locally available foods acceptable for complementary feeding of the infant after six months of age (). Designed for a largely illiterate population, each page of the flipbook was double-sided: one side with the script faced the study nurse while the opposite side was simultaneously visible to the woman and showed photos of locally available foods (). The flipbook begins with counseling on WASH behaviors, followed by exclusive breastfeeding for infants of less than six months, then highlights the seven food groups and amounts of breastfeeding and complementary foods according to infant age as outlined by the WHO [Citation14]. Important elements of the script were adapted and updated based on findings from focus group discussions that provided common rationale among refugee mothers for inappropriate behaviors (). Although this population may be considered ‘food secure’ with rations providing a large proportion of daily nutritional requirements for households, households supplement remaining nutritional needs according to their financial means. As home-based counseling sessions also collected data on monthly household expenditures for food, the study nurse could tailor counseling for mothers by providing cheaper food options for infants and specific examples of low-cost meals to meet minimum acceptable diet and diet diversity requirements. Training of the study nurse took approximately one week, which included testing the intervention with pregnant women prior to implementation of the pilot. The basic English script allowed the study nurse to develop her own style in delivering the counseling in either Karen or Burmese language. Researchers (AH, MCD) provided supervision and support for counseling over the course of the pilot.
Figure 1. Examples of pages in the “Healthy Baby Flipbook” flipbook. (a) and (b) includes examples of script tailored to behaviors common among refugee mothers; (c) has food items listed to remind the counselor, while the opposite side (d) features photos of locally available, nutritious foods facing the mother receiving counseling.
Results
Out of the 34 mothers with infants eligible for inclusion at the time of recruitment, 20 mothers consented to participate in the longitudinal cohort (59%). A total of 132 household visits were conducted and a median of 7 visits per household (range 3 to 7) between October 2013 and June 2014. One mother lived outside MLA and was interviewed in the clinic at four, six, and nine months. The remaining 19 were followed up monthly in their homes from baseline at age 3 months until the infant reached 9 months of age; 15 (79%) were seen every month with 3 mothers missing only one appointment due to travel to neighboring Myanmar.
The proportion of exclusively breastfed infants increased from 42% (8/19) at 3 months to 65% (11/17) at 5 months. Among mothers who had prepared the family meal the day prior to interview, handwashing was 94% (15/16) at baseline and reached 100% at 6- (13/13) and 9-month (20/20) visits. Infants at 6 months of age were fed inadequately; 5% (1/20) were fed adequate dietary diversity; 10% (2/20) had received the appropriate meal amount, and no infants had consumed a minimum acceptable diet. These proportions increased to 90% (18/20), 100% (20/20), and 90% (18/20), respectively, by the time the infants reached 9 months. Appropriate dietary diversity and minimum acceptable diet increased within 2 months from the 6-month interview from 5% (1/20) to 58% (11/19, p < 0.001) and from 0% (0/20) to 47% (9/19, p < 0.001), respectively. After excluding the one mother living outside MLA without an improved form of sanitation, safe disposal of infant stool improved progressively from 16% (10/19) at 6 months to reach 100% (19/19; p = 0.040) at the 9-month interview.
Discussion
Given the growing burden of displaced populations globally, this study presents a counseling program conducted by local health workers for improved infant feeding practices in a marginalized, largely illiterate, refugee population [Citation15]. Baseline data from a cross-sectional survey of 103 women with infants between 6 and 12 months from the same original cohort in MLA camp showed poor rates of diet diversity and minimum acceptable diet at 20% and 2%, respectively (Hashmi, unpublished data). It is important to reiterate that this nutrition counseling was conducted in what can be considered a food secure population, but likely representative of displaced persons establishments elsewhere under the purview of the United Nations High Commissioner for Refugees. It is also important to note that this population already has baseline data suggesting high rates of breastfeeding initiation and breastfeeding duration [Citation16], which may also positively impact uptake of behavior change education [Citation8]. This pilot follows recommendations from recent systematic studies summarizing findings for appropriate counseling for improved outcomes in infant feeding – including exclusive breastfeeding, breastfeeding duration, and complementary feeding – in meeting diet diversity and minimum acceptable diet requirements for infants six months of age or older [Citation5–Citation10]. Although the sample size is quite small and inferences as to the significance of these behavior changes are therefore limited, the rapidity with which mothers changed behaviors in this pilot study is promising and provides further evidence that verbal messaging in the home and/or the community can improve infant feeding practices in resource-poor settings with low rates of literacy [Citation10]. Results of this pilot have been communicated with local stakeholders, including health worker staff at SMRU, local organizations engaged in programming for infant feeding in refugee and migrant communities along the border, and the nutrition working group of The Border Consortium – a technical working group bringing together organizations providing rations and working on nutrition across all refugee camps in Thailand. Further research includes studying the impact of this counseling intervention on infant growth and its cost-effectiveness along the Thailand–Myanmar border.
Conclusions
This pilot demonstrates improvement in maternal infant feeding and WASH practices in a small set of refugee mothers, providing evidence of counseling measures to improve infant health in vulnerable populations.
Author contributions
All authors meet the International Committee of Medical Journal Editors requirements for authorship.
Ethics and consent
This investigation was part of a larger study (ClinicalTrials.gov Identifier: NCT00840502), and was approved by the University of Oxford (OxTREC (14–08)) and Mahidol University (TMEC 2008–028) Ethics Committees. The current study also received ethical approval by the University of Texas Medical Branch (Galveston, Texas) Institutional Review Board (14-0211). All institutions approved this study in accordance with the Declaration of Helsinki. In addition, the Tak Province Community Advisory Board (Tak, Thailand) based along the Thailand–Myanmar border also approved this study (TCAB-03.13).
Paper context
Suboptimal breastfeeding and complementary feeding remain strong risk factors for chronic infant malnutrition. No published studies exist on educational interventions to improve infant feeding practices among refugees or displaced persons in LMIC settings. This study created and piloted educational materials for counseling of refugee mothers along the Thailand–Myanmar border to improve infant feeding and water, sanitation, and hygiene practices. This pilot provides evidence of counseling measures to improve infant health in vulnerable populations.
Acknowledgments
We would like to acknowledge the pregnant women participating in this study. We would also like to thank the local health staff at the SMRU MLA clinic that helped support the logistics and implementation of this study.
Disclosure statement
The authors report no conflicts of interest.
Additional information
Funding
References
- Mason J, Shrimpton R, Saldanha L, et al. The first 500 days of life: policies to support maternal nutrition. Glob Health Action. 2015;7:23623.
- Prendergast A, Humphrey J. Stunting persists despite optimal feeding: are toilets part of the solution? Low-birthweight baby: born too soon or too small. Basel: Kargers Publishers; 2015. p. 99–5.
- Prendergast A, Humphrey J. The stunting syndrome in developing countries. Paediatr Int Child Health. 2014;34:250–265.
- Solomons N, Vossenaar M, Chomat A, et al. Stunting at birth: recognition of early-life linear growth failure in the western highlands of Guatemala. Public Health Nutr. 2015;18:1737–1745.
- Imdad A, Yakoob M, Bhutta Z. Effect of breastfeeding promotion interventions on breastfeeding rates, with special focus on developing countries. BMC Public Health. 2011;11:S24.
- Imdad A, Yakoob M, Bhutta Z. Impact of maternal education about complementary feeding and provision of complementary foods on child growth in developing countries. BMC Public Health. 2011;11:S25.
- Lumbiganon P, Martis R, Laopaiboon M, et al. Antenatal breastfeeding education for increasing breastfeeding duration. Cochrane Database Syst Rev. 2016;12:CD006425.
- McFadden A, Gavine A, Renfrew M, et al. Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database Syst Rev. 2017;2:CD001141.
- Panjwani A, Heidkamp R. Complementary feeding interventions have a small but significant impact on linear and ponderal growth of children in low- and middle-income countries: a systematic review and meta-analysis. J Nutr. 2017;147:2169S–2178S.
- Sinha B, Chowdhury R, Upadhyay R, et al. Integrated interventions delivered in health systems, home, and community have the highest impact on breastfeeding outcomes in low- and middle-income countries. J Nutr. 2017;147:2179S–2187S.
- United Nations High Commissioner for Refugees. Figures at a glance 2018. [ cited 2018 Dec 11]. Available from: http://www.unhcr.org/figures-at-a-glance.html
- Ayoya M, Golden K, Ngnie-Teta I, et al. Protecting and improving breastfeeding practices during a major emergency: lessons learnt from the baby tents in Haiti. Bull World Health Organ. 2013;91:612–617.
- Sami S, Kerber K, Tomczyk B, et al. “You have to take action”: changing knowledge and attitudes towards newborn care practices during crisis in South Sudan. Reprod Health Matters. 2017;25:124–139.
- World Health Organization. Indicators for assessing infant and young child feeding practices part 2: measurement. Geneva: WHO; 2008.
- Carrara V, Hogan C, De Pree C, et al. Improved pregnancy outcome in refugees and migrants despite low literacy on the Thai-Burmese border: results of three cross-sectional surveys. BMC Pregnancy Childbirth. 2011;11:45.
- White A, Carrara V, Paw M, et al. High initiation and long duration of breastfeeding despite absence of early skin-to-skin contact in Karen refugees on the Thai-Myanmar border: a mixed methods study. Int Breastfeed J. 2012;7:19.
