ABSTRACT
Background: Despite substantial progress in antiretroviral therapy (ART) scale up, some people living with HIV (PLHIV) continue to present with advanced HIV disease, contributing to ongoing HIV-related morbidity and mortality.
Objective: We aimed to quantify population-level estimates of advanced HIV from three high HIV prevalence settings in Sub-Saharan Africa.
Methods: Three cross-sectional surveys were conducted in (Ndhiwa (Kenya): September–November 2012), (Chiradzulu (Malawi): February–May 2013) and (Eshowe (South Africa): July–October 2013). Eligible individuals 15–59 years old who consented were interviewed at home followed by rapid HIV test and CD4 count test if tested HIV-positive. Advanced HIV was defined as CD4 < 200 cells/µl. We used logistic regression to identify patient characteristics associated with advanced HIV.
Results: Among 18,991 (39.2% male) individuals, 4113 (21.7%) tested HIV-positive; 385/3957 (9.7% (95% Confidence Interval [CI]: 8.8–10.7)) had advanced HIV, ranging from 7.8% (95%CI 6.4–9.5) Chiradzulu (Malawi) to 11.8% (95%CI 9.8–14.2) Ndhiwa (Kenya). The proportion of PLHIV with advanced disease was higher among men 15.3% (95% CI 13.2–17.5) than women 7.5% (95%CI 6.6–8.6) p < 0.001. Overall, 62.7% of all individuals with advanced HIV were aware of their HIV status and 40.3% were currently on ART. Overall, 65.6% of individuals not on ART had not previously been diagnosed with HIV, while only 29.6% of those on ART had been on ART for ≥6 months. Individuals with advanced HIV disease were more likely to be men (adjusted Odds Ratio [aOR]; 2.1 (95%CI 1.7–2.6), and more likely not to be on ART (aOR; 1.7 (95%CI 1.3–2.1).
Conclusion: In our study, about 1 in 10 PLHIV had advanced HIV with nearly 40% of them unaware of their HIV status. However, a substantial proportion of patients with advanced HIV were established on ART. Our findings suggest the need for a dual focus on alternative testing strategies to identify PLHIV earlier as well as improving ART retention.
KEYWORDS:
Responsible Editor Stig Wall, Umeå University, Sweden
Background
Over the past decade, there have been substantial increases in antiretroviral therapy (ART) access for people living with HIV (PLHIV) [Citation1]. However, a substantial number of PLHIV continue to experience advanced HIV disease, contributing to ongoing HIV-related morbidity and mortality [Citation2]. About 940,000 HIV-related deaths occurred globally in 2017 and about 70% of these were from sub-Saharan Africa [Citation3]. Mortality is very high among individuals with advanced HIV disease particularly those with very low CD4 count [Citation4–Citation7].
Rapid ART initiation improves survival of PLHIV [Citation8,Citation9] and most countries have now implemented the WHO recommendation to start all PLHIV on ART regardless of CD4 count, called ‘treat all’, in the hope of improving survival of PLHIV [Citation10]. However, despite sharp increases in number of ART initiations, HIV-related mortality has declined little over recent years [Citation11] suggesting that even in the context of ‘treat all’, specific focus has to be directed towards patients with advanced HIV disease who are at highest risk of mortality. In order to reduce high HIV-related mortality and morbidity [Citation2,Citation12,Citation13], the WHO released guidelines in 2017 for managing individuals with advanced HIV disease including their rapid initiation on ART [Citation14]. In order to apply these recommendations effectively, we need to know the number and characteristics of people with advanced HIV to plan for their management and allocate resources appropriately.
Clinic-based studies have been used to estimate the burden of advanced HIV disease [Citation15,Citation16]. While these studies provide a quick and relatively inexpensive way to quantify this burden, the estimates from such studies may fail to accurately reflect the true number and characteristics of individuals with advanced HIV disease, because of selection bias in clinic populations rather than at population-level.
We aimed to quantify and describe the population-level characteristics of people with advanced HIV disease using data from HIV prevalence surveys that were conducted in three sub-Saharan African countries: Ndhiwa (Kenya), Chiradzulu (Malawi) and Eshowe (South Africa).
Methods
Study design
We used data from three population-based cross-sectional HIV prevalence surveys conducted in Ndhiwa (Kenya: September–November 2012), Chiradzulu (Malawi: February–May 2013) and Eshowe (South Africa: July–October 2013). All the surveys were not national representative surveys. The study methods have been described in detail elsewhere [Citation17–Citation19]. Briefly, a two-stage sampling design was used, first using systematic sampling to select clusters based on demarcations from the national population and housing censuses, which had been conducted prior to the surveys. Then, from each selected cluster, we randomly selected 25 households Chiradzulu (Malawi) and Eshowe (South Africa); 20 households for Ndhiwa (Kenya), making the sample selection self-weighting. More households than were needed were sampled to allow these additional households to be used as replacements if no one was found at home. All individuals aged 15–59 years old who were residents of the study area or visitors who had spent the previous night in the study area were eligible for inclusion.
At the time of the survey, countries were using different ART eligibility criteria. For all countries, PLHIV were ART eligible with CD4 ≤ 350 cells/µl or WHO Stage 3 or 4 disease. Kenya prevention of mother to child transmission (PMTCT) guidelines were ‘Option A’ (ART when CD4 ≤ 350/µl for pregnant and breastfeeding women and antiretroviral prophylaxis only if maternal CD4 > 350/µl), for South Africa ‘Option B’ (ART for all pregnant and breastfeeding women until cessation of breastfeeding) and for Malawi ‘Option B+’ (lifelong ART for all pregnant and breastfeeding women).
Data collection methods
We interviewed consenting individuals at their households using a structured questionnaire and conducted a rapid HIV test if they gave consent to be tested. For minors younger than 18 years, parental/guardian consent was sought first in Ndhiwa (Kenya) and Eshowe (South Africa) but was not required in Chiradzulu (Malawi) where minors aged 14–17 years old are considered able to give their own consent for HIV testing. Details of HIV rapid testing methods and other laboratory tests carried out including testing materials have been reported in more detail elsewhere [Citation20]. Data were double entered using EpiData and checked for inconsistencies before analysis.
Statistical methods and analysis
Detailed description of the demographic characteristics of the study population has been reported elsewhere [Citation20]. For this analysis, we compared the characteristics of PLHIV with and without advanced HIV disease using chi-square tests. Since we did not have clinical data of individuals who participated in the studies, we considered all PLHIV with CD4 count <200 cells/µl as having ‘advanced HIV’ disease, with the remainder of PLHIV referred to as ‘individuals without advanced HIV’. Only data collected during the surveys were used for this analysis.
We compared the cascade of care (from diagnosis (those who knew they were HIV-positive), to those on ART, to virologically suppressed) for all individuals with advanced HIV disease stratified by country and sex using chi-square tests. As the risk of mortality and morbidity increases with decreasing CD4 cell count [Citation4–Citation6], we also evaluated the cascade of care only among individuals with CD4 < 100 cells/µl. Among those on ART, we further examined the distribution of advanced HIV by duration on ART, categorized as <6 months or ≥6 months on ART. We chose ≥6 months as the comparison period as WHO indicates this is long enough for a positive effect of treatment on CD4 count for those taking their medications consistently [Citation21].
For patients on ART for ≥6 months, we compared their median period on ART between individuals with and without advanced HIV disease. We also summarized virologic suppression (<1000 copies/ml) among those on ART for ≥6 months. All estimates were weighted to account for sampling design.
We used logistic regression to assess the association between age, sex, ART status and knowing one’s HIV status and advanced HIV disease for each country and random effects logistic regression for the overall data to allow for clustering by country. Using stepwise model building, age and sex were included a priori and ART status was added as a main explanatory variable for advanced HIV. HIV status knowledge and viral load were not included in the final model because they were collinear with ART status. We analysed the data using STATA 15 (Stata Corporation, College Station, Texas).
Ethics
All surveys received ethical approval from local and international ethics committees. For Ndhiwa (Kenya), local approvals were obtained from the Kenya Medical Research Institute Ethical Review Committee (KEMRI, protocol number 347), Chiradzulu (Malawi) from the National Health Sciences Research Committee (protocol number 1085) and Eshowe (South Africa) from the University of Cape Town Human Research Ethics Committee (HREC) protocol number 461/2012, and the Health Research Committee of the Health Research and Knowledge Management Unit of the Kwazulu–Natal Department of Health. International approval for all studies was obtained from the Comite´ de Protection des Personnes d’Ile de France (protocol number 12056 Ndhiwa (Kenya), 12084 Chiradulu (Malawi) and 12091 Eshowe (South Africa) [Citation20]. All study participants were given sufficient information about the aims of the surveys and provided written consent for their inclusion in the study.
Results
Of 21,798 eligible individuals, (6833 (31.4%) Ndhiwa (Kenya)), (8277 (38.0%) Chiradzulu (Malawi)), (6688 (30.7%) Eshowe (South Africa)), 18,991 (87.1%) participated and accepted an HIV test of which 4113 (21.7%) tested HIV-positive. Of the 2807 (12.1%) who did not participate, (757/6833 (11.1%) Ndhiwa (Kenya)), (1008/8277 (12.2%) Chiradulu (Malawi)) and (1042/6688 (15.6%) Eshowe (South Africa)), the reasons for non-participation were; 51.9% not at home, 38.6% refused, 6.1% were incapacitated and for 3.4% the reasons were unspecified. Proportion of adolescents aged 15–17 years old who refused to provide consent to participate in the study was slightly higher in Eshowe (South Africa) with 63/937 (6.7%) followed by 36/851 (4.2%) in Ndhiwa (Kenya) and 35/1066 (3.3%) in Chiradzulu (Malawi).
HIV prevalence was highest in Eshowe (South Africa), 25.2% (95% Confidence Interval [CI]: 23.6–26.9) followed by Ndhiwa (Kenya) 24.1% (95%CI 22.7–25.6) and Chiradzulu (Malawi) 17.0% (95%CI 16.0–18.1). Overall, CD4 count results were available for 3957/4113 (96.2%) individuals with 5.6% from Ndhiwa (Kenya), 4.2% Chiradzulu (Malawi) and 1.6% Eshowe (South Africa) missing CD4 count results. The majority of those missing CD4 count results were unaware of their HIV status 77.1% and not on ART 90.3%. Missing CD4 count results were mostly due to individuals refusing to provide venous blood for other tests.
shows the distribution of baseline characteristics by HIV status. The overall distribution shows that in comparison to those without HIV, among PLHIV there was a lower proportion of HIV-positive men, youth aged 15–19 years and a higher proportion of people with no schooling, widow/ers and those doing farming as a source of income.
Table 1. Distribution of baseline characteristics by HIV status of 18,991 individuals who participated in the three surveys Kenya, Malawi and South Africa.
Overall, 385/3957 (9.7%) PLHIV had advanced HIV disease; 7.8% (95%CI 6.4–9.5) in Chiradzulu (Malawi), 9.8% (95%CI 8.0–11.9) in Eshowe (South Africa) and 11.8% (95%CI 9.8–14.2) in Ndhiwa (Kenya). The proportion of patients with advanced HIV was higher among men 15.3% (95%CI 13.2–17.5) than women 7.5% (95%CI 6.6–8.6) p < 0.001 overall and by country; 17.4% (95%CI 13.7–22.0) vs 9.3% (95%CI 7.4–11.8) in Ndhiwa (Kenya), 12.9% (95%CI 9.8–17.0) vs 5.6% (95%CI 4.2–7.4) in Chiradzulu (Malawi) and 17.0% (95%CI 12.5–22.7) vs 7.4% (95%CI 6.0–9.1) in Eshowe (South Africa). Of the individuals with advanced HIV disease, 27.0% had CD4 < 100 cells/µl and 11.7% were severely immunosuppressed (CD4 < 50 cells/µl). In all three countries, sex, ART coverage and viral load level distribution varied with CD4 level. HIV status awareness varied with CD4 level only in Chiradzulu (Malawi) and Eshowe (South Africa) (). We found no difference in proportion of patients with advanced disease by age.
Table 2. Distribution of baseline characteristics of 3957 HIV-positive individuals by CD4 count (CD4 < 200 vs CD4 ≥ 200 cells/µl) in the three surveys Ndhiwa (Kenya), Chiradzulu (Malawi) and Eshowe (South Africa).
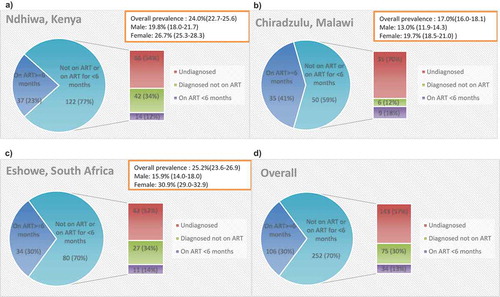
The cascade of care for individuals with advanced HIV disease is shown in . In , we present the cascade of care restricted to those individuals with CD4 < 100 cells/µl. Overall 240/383 (62.7%) individuals with advanced HIV disease were aware of their HIV status (two had missing HIV status awareness information), 165/365 (45.2%) had ever initiated ART (20 had missing ART status information; 11 from Chiradzulu (Malawi) and 9 from Eshowe (South Africa)), 147/365 (40.3%) were currently on ART and 103/381 (27.0%) had suppressed viral load (VL) (four had missing VL information). The cascade of care was similar for individuals with CD4 < 100 cells/µl in all three countries.
Table 3. Cascade of care of 385 individuals with advanced HIV disease.
Table 4. Cascade of care of 104 advanced HIV disease individuals with CD4 < 100 copies/ml (to be added to the appendix).
Overall, 252/358 (70.4%) of individuals with advanced HIV disease were not on ART or were on ART for <6 months. Most of those not on ART 143/218 (65.6%) had not previously been diagnosed as HIV infected. Of those diagnosed but not on ART 13/74 (17.6%) were not linked to care (one had missing linkage to care information). We found no differences in knowledge of HIV-positivity status by age group and sex among those not on ART. Ndhiwa (Kenya) had the highest proportion of individuals not on ART or on ART for <6 months 76.7%, followed by Eshowe (South Africa) 70.2% and Chiradzulu (Malawi) 58.8% (). We found 18/75 (24.0%) of individuals with advanced HIV disease not currently on ART had been on ART previously. Almost all were from Eshowe (South Africa) and were mostly women.
Figure 1. Showing distribution of 358 individuals with advanced HIV disease by ART status for each survey and overall.
(a) Kenya: ART eligibility at the time of survey was CD4 ≤ 350 cells/µl or WHO Stage 3 or 4 disease and ART prophylaxis for pregnant and breast-feeding women if CD4 > 350 cells/µl (Option A)(b) Malawi: ART eligibility at the time of survey was CD4 ≤ 350 cells/µl or WHO Stage 3 or 4 disease and lifelong ART for pregnant and breastfeeding women (Option B+)(c) South Africa: ART eligibility at the time of survey was CD4 ≤ 350 cells/µl or WHO Stage 3 or 4 disease and ART for pregnant and breastfeeding women until cessation of breastfeeding (Option B).
Among those who knew their HIV diagnosis with advanced HIV, the proportion who had ever been on ART ranged from 53/93 (57.0%) in Ndhiwa (Kenya), 44/61 (72.1%) Chiradzulu (Malawi) to 68/86 (79.1%) Eshowe (South Africa) and overall, the majority of them 147/165 (89.1%) were still on treatment. Most people who were still on treatment had been on ART for ≥6 months. Overall, among those who knew their HIV diagnosis with advanced HIV the proportion of men on ART for ≥6 months was lower than women ( and ).
Table 5. Distribution by time on ART for 147 individuals with advanced HIV disease on ART.
Of the 365/385 (94.8%) with ART status information, a further 7 were missing information about period on ART leaving 358 (93.0%) with complete ART information. Among 106/358 (29.6%) individuals with advanced HIV disease who were currently on ART for ≥6 months, the median (interquartile range (IQR)) number of months on ART was slightly lower than that of individuals without advanced HIV disease in all countries (23.1 (14.0–39.9) vs 30.4 (16.7–54.4) Ndhiwa (Kenya), 33.5 (13.8–78.1) vs 46.8 (13.0–72.2) Chiradzulu (Malawi) and 32.7 (14.2–61.9) vs 40.9 (18.9–68.6) Eshowe (South Africa)). Among all PLHIV on ART for ≥6 months, those with advanced HIV disease included fewer females (61.3% vs 74.8%) than those without advanced HIV disease ().
Table 6. Distribution by sex, age and viral load of 106 individuals with advanced HIV disease who had been on ART for at least 6 months.
In the multivariable analysis, those with advanced HIV disease were (adjusted Odds Ratio [aOR]); 2.1 (95%CI 1.7–2.6) times more likely to be males, and aOR; 1.7 (95%CI 1.3–2.1) times more likely to not be on ART compared to those without advanced HIV disease ().
Table 7. Crude and adjusted ORs for the effect of sex, age and ART on individuals with advanced HIV disease.
Discussion
The proportion of PLHIV with advanced disease at population level ranged from 8% to 11% with men twice as likely to have advanced HIV disease as women. We found that more than half of individuals with advanced HIV disease were not on ART; most of them were not previously aware of their HIV status highlighting the need for expanded and innovative approaches to HIV testing. However, we also showed that 40% of advanced HIV patients were currently on ART. As countries move to ‘treat all’, it is likely that fewer people will experience advanced HIV. However, there may be an increasing proportion still of some PLHIV with advanced HIV disease who have a history of previously having started ART and subsequently disengaged from care; interventions to ensure retention on treatment will therefore be crucial.
To our knowledge, this is the first study to give an estimate of the prevalence of advanced HIV disease from a population-based study. Our population estimates of the prevalence of advanced HIV were generally lower than most clinical cohort-based estimates which are almost 3 times as high. A study conducted between 2013 and 2015 in Kenya [Citation16] found that 33% of HIV-positive individuals presenting for care had advanced HIV. Another study that measured trends in CD4 count at the start of ART in 55 countries [Citation22] found that about 37% of individuals who initiated ART in 2015 had advanced HIV overall and the proportion was even higher in some countries [Citation15,Citation23]. However, these higher proportions for clinic-based studies should be expected considering that many individuals present to HIV care because they are already sick and their CD4 count is measured at initiation of ART. Our population level estimates are not subject to this bias, though absence of clinical definition of advanced HIV in our survey may lead to an underestimate of true advanced HIV in the community.
Although our estimate of advanced HIV looks relatively low, this may be due to the more dynamic nature of individuals with advanced HIV disease. Individuals with advanced HIV disease are at high risk of mortality and morbidity especially if they are not started on treatment rapidly. Cross-sectional population surveys cannot estimate the longitudinal burden of advanced HIV over time as cohort studies do. Undiagnosed individuals with advanced HIV disease, however, pose a greater risk than patients in clinical care on ART, with respect to onward transmission, and also have much higher morbidity and mortality. Recent systematic reviews [Citation5,Citation24] looking at predictors of mortality among individuals taking ART have shown that most deaths which occurred within the first 6 months of ART initiation were associated among other factors with advanced HIV (stage 3 and 4) and low CD4 count.
While the high proportion of undiagnosed advanced HIV is a major cause of concern, another important group are those who have advanced HIV despite having initiated ART more than 6months previously, especially those that have not achieved viral suppression and those that have disengaged from care and are no longer on ART. However, our study was not designed to address this issue as we did not collect data on the cause of viral non-suppression, which could be due to inaccurate information of duration on ART, treatment failure, previous gaps in care or poor adherence. Nevertheless, we found a high proportion of individuals with advanced HIV disease who had been on ART for ≥6 months to have unsuppressed viral load. Improving access to VL testing could help identify patients who are failing on first-line treatment and facilitate earlier switch to second-line.
We found men to be twice as likely to have advanced HIV, reflecting the fact that men generally tend to access treatment later [Citation25–Citation27], have physiologically lower CD4 count than women and are slower in immune reconstitution while on ART [Citation7,Citation28]. The fact that the cascade of care among individuals with advanced HIV disease was similar by sex supports a partial contribution of poorer immune recovery among men to the burden of advanced HIV disease. Indeed, we found that among individuals with advanced HIV disease on ART for ≥6 months, men were more likely to be suppressed. Several studies have shown that because of sex differences in immune reconstitution of individuals on ART, men with lower CD4 took longer than women to recover and reach CD4 count levels associated with lower risk of mortality and morbidity [Citation7,Citation28]. Knowing CD4 count at diagnosis and subsequent time points, especially for older men, could assist in identifying those who are taking their treatment properly but have suboptimal immune recovery.
Although our results showed no difference in terms of HIV status awareness by sex and age group among individuals with advanced HIV disease not on ART, this could be due to small numbers in the youngest age group. Unrestricted analysis (all HIV-positive regardless of ART status) of HIV status awareness by age showed that those at youngest age were less likely to be aware of their HIV status. Although Chiradzulu (Malawi) had the highest ART coverage at the time of the survey, it also had the highest proportion of individuals with advanced HIV disease not on ART who did not know their HIV status, suggesting ongoing gaps in diagnostic coverage. Implementation of ‘treat all’ should, therefore, give special attention to individuals with advanced HIV disease to realize greater impact in reducing the burden of HIV.
The inclusion of population-level data from three different countries and comparison of patients with advanced HIV across three settings are strengths of our study. A number of people did not participate either due to refusal or not being at home. However, it is difficult to tell how these would affect the results as we did not collect data on non-participants. Other limitations include missing data especially of ART status and duration on ART. Accuracy of date of ART initiation was difficult to ascertain for the calculation of duration on ART and we did not have information on whether some individuals had defaulted and were restarting treatment. Importantly, this was a secondary data analysis of studies conducted in 2013 or earlier and the prevalence and characteristics of people with advanced HIV may have changed. Nevertheless, although most countries have adopted ‘treat all’ there may be delays in implementation at the level of all facilities and our results would thus remain relevant for settings where ‘treat all’ has not yet been fully implemented [Citation29]. Finally, as stated in the methods, the surveys were not representative at country level and subgroup analysis was not planned at the design stage analysis, therefore, our results should be interpreted with caution.
Conclusion
Our study demonstrates firstly that there is a substantial proportion of people with advanced HIV unaware of their status, indicating that there may be a role for different testing strategies to reach this group. Example of strategies includes HIV oral self-testing which WHO recommends [Citation30], community-based testing strategies especially for men [Citation31], HIV testing promotion in schools for the youngest generation and door-to-door testing campaigns. In addition, critical to reducing mortality and morbidity among individuals with advanced HIV disease is to identify them early among those newly tested HIV-positive using CD4 count test and to effectively and rapidly link them to care [Citation14]. Although implementation of ‘treat all’ has rendered CD4 testing less important for determining ART eligibility [Citation32], continued use of CD4 cell count test to identify individuals with advanced HIV disease ‘high risk’ will be important. Secondly, a high proportion of individuals with advanced HIV disease had previously initiated ART, suggesting the need for improved retention and outcomes after ART start, through initiatives such as using more effective first-line regimens, access to viral load testing to identify treatment failure and peer-support to encourage re-engagement in ART care in those who have become lost to follow up.
Author contributions
Menard Chihana: Study design, data analysis and write up and approval of the final manuscript
Helena Huerga: Study design, critical revision of the manuscript and approval of the final manuscript
Gilles Van Cutsem: Critical revision of the manuscript and approval of the final manuscript
Tom Ellman: Critical revision of the manuscript and approval of the final manuscript
Eric Goemaere: Critical revision of the manuscript and approval of the final manuscript
Stephen Wanjala: Critical revision of the manuscript and approval of the final manuscript
Charles Masiku: Critical revision of the manuscript and approval of the final manuscript
Elisabeth Szumilin: Critical revision of the manuscript and approval of the final manuscript
Jean-Francois Etard: Study design, critical revision of the manuscript and approval of the final manuscript
David Maman: Study design, critical revision of the manuscript and approval of the final manuscript
Mary-Ann Davies: Study design, critical revision of the manuscript and approval of the final manuscript
Ethics and consent
All surveys received ethical approval from both the local and international ethics committee. In Kenya, local approval was granted by Kenya Medical Research Institute Ethical Review Committee (KEMRI, protocol number 347), in Malawi it was granted by the National Health Sciences Research Committee (protocol number 1085) and in South Africa by the University of Cape Town Human Research Ethics Committee (HREC) protocol number 461/2012, and the Health Research Committee of the Health Research and Knowledge Management Unit of Kwazulu-Natal Department of Health. International approval was granted for all studies by the Comite´ de Protection des Personnes d’Ile de France (protocol number 12056 for Kenya, 12084 for Malawi and 12091 for South Africa). All study participants in all the three surveys were asked to sign a written consent if they understood the objectives of the study and accepted to be included in the study. For minors younger than 18 years, parental/guardian consent was sought first in Kenya and South Africa but was not required in Malawi where minors aged 14–17 years old are considered able to give their own consent for HIV testing.
Paper context
Despite substantial progress in antiretroviral therapy scale up, a number of people living with HIV continue to experience advanced HIV disease. Most available estimates of advanced HIV are based on clinical cohort data which is prone to selection bias. This may be the first study to quantify advanced HIV at population level. Our results suggest the need for alternative testing strategies to identify people living with HIV earlier, improving retention and virologic suppression on ART.
Acknowledgments
The following are acknowledged for the success of the study: Study participants, survey field teams and MSF staff, all the individuals who contributed towards the success of the surveys in all three countries and The South African Department of Science and Technology/National Research Foundation (DST-NRF), Centre of Excellence in Epidemiological Modeling and Analysis (SACEMA), Stellenbosch University, South Africa for their support.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- UNAIDS. GLOBAL AIDS UPDATE. Geneva, Switzerland: UNAIDS; 2016.
- Ford N, Doherty M. The enduring challenge of advanced HIV infection. N Engl J Med. 2017 Jul 20;377:283–12. PubMed PMID: 28723319.
- UNAIDS. Global HIV & AIDS statistics — 2018 fact sheet. 2018. Available from: http://www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf
- May MT, Vehreschild JJ, Trickey A, et al. Mortality according to CD4 count at start of combination antiretroviral therapy among HIV-infected patients followed for up to 15 years after start of treatment: collaborative cohort study. Clin Infect Dis. 2016 Jun 15;62:1571–1577. PubMed PMID: 27025828; PubMed Central PMCID: PMCPMC4885653.
- Biset Ayalew M. Mortality and its predictors among HIV infected patients taking antiretroviral treatment in ethiopia: a systematic review. AIDS Res Treat. 2017;2017:5415298. PubMed PMID: 29214077; PubMed Central PMCID: PMCPMC5682904.
- Bisson GP, Ramchandani R, Miyahara S, et al. Risk factors for early mortality on antiretroviral therapy in advanced HIV-infected adults. AIDS. 2017 Oct 23;31:2217–2225. PubMed PMID: 28742529; PubMed Central PMCID: PMCPMC5633516. eng.
- Kroeze S, Ondoa P, Kityo CM, et al. Suboptimal immune recovery during antiretroviral therapy with sustained HIV suppression in sub-Saharan Africa. AIDS. 2018 May 15;32:1043–1051. PubMed PMID: 29547445; eng.
- Grinsztejn B, Hosseinipour MC, Ribaudo HJ, et al. Effects of early versus delayed initiation of antiretroviral treatment on clinical outcomes of HIV-1 infection: results from the phase 3 HPTN 052 randomised controlled trial. Lancet Infect Dis. 2014 Apr;14:281–290. PubMed PMID: 24602844; PubMed Central PMCID: PMCPMC4144040.
- Group ISS, Lundgren JD, Babiker AG, et al. Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med. 2015 Aug 27;373:795–807. PubMed PMID: 26192873; PubMed Central PMCID: PMCPMC4569751.
- WHO. Treat all: policy adoption and implementation status in countries. 2017. Available from: http://apps.who.int/iris/bitstream/10665/258538/1/WHO-HIV-2017.35-eng.pdf?ua=1
- UNAIDS. HIV estimates with uncertainty bounds 1990–2018. 2019. Available from: https://www.unaids.org/en/resources/documents/2019/HIV_estimates_with_uncertainty_bounds_1990-present
- Gbd Hiv Collaborators. Estimates of global, regional, and national incidence, prevalence, and mortality of HIV, 1980–2015: the global burden of disease study 2015. Lancet HIV. 2016 Aug;3:e361–e387. PubMed PMID: 27470028; PubMed Central PMCID: PMCPMC5056319.
- Roser M, Ritchie H HIV/AIDS. 2018. Available from: OurWorldInData.org; ‘https://ourworldindata.org/hiv-aids’
- WHO. Guidelines for managing advanced HIV disease and rapid initiation of antiretroviral therapy. Geneva, Switzerland: World Health Organization; 2017 Jul.
- Auld AF, Shiraishi RW, Oboho I, et al. Trends in prevalence of advanced HIV disease at antiretroviral therapy enrollment - 10 countries, 2004–2015. MMWR Morb Mortal Wkly Rep. 2017 Jun 2;66:558–563. PubMed PMID: 28570507.
- van der Kop ML, Thabane L, Awiti PO, et al. Advanced HIV disease at presentation to care in Nairobi, Kenya: late diagnosis or delayed linkage to care?–a cross-sectional study. BMC Infect Dis. 2016 Apr 18;16:169. PubMed PMID: 27091128; PubMed Central PMCID: PMCPMC4835937.
- Huerga H, Van Cutsem G, Ben Farhat J, et al. Who needs to be targeted for HIV testing and treatment in KwaZulu-Natal? Results from a population-based survey. J Acquir Immune Defic Syndr. 2016 Dec 01;73:411–418. PubMed PMID: 27243903; PubMed Central PMCID: PMCPMC5172512.
- Maman D, Chilima B, Masiku C, et al. Closer to 90-90-90. The cascade of care after 10 years of ART scale-up in rural Malawi: a population study. J Int AIDS Soc. 2016;19:20673. PubMed PMID: 26894388; PubMed Central PMCID: PMCPMC4760102.
- Maman D, Zeh C, Mukui I, et al. Cascade of HIV care and population viral suppression in a high-burden region of Kenya. AIDS. 2015 Jul 31;29:1557–1565. PubMed PMID: 26244395; PubMed Central PMCID: PMCPMC4502986.
- Chihana ML, Huerga H, Van Cutsem G, et al. Impact of “test and treat” recommendations on eligibility for antiretroviral treatment: cross sectional population survey data from three high HIV prevalence countries. PloS One. 2018;13:e0207656. PubMed PMID: 30475865.
- WHO. Antiretroviral therapy for HIV infection in adults and adolescents: recommendations for a public health approach.– 2010 revision. Geneva, Switzerland: WHO; 2010.
- Anderegg N, Kirk O; on behalf of IeDEA - Global Adults and COHERE. Immunodeficiency at the start of combination antiretroviral therapy in low-, middle- and high-income countries. 21st International Workshop on HIV and Hepatitis Observational Databases; Mar 30 - Apr 1 2017; Lisbon; 2017. Abstract 12.
- Gunda DW, Godfrey KG, Kilonzo SB, et al. Cytopenias among ART-naive patients with advanced HIV disease on enrolment to care and treatment services at a tertiary hospital in Tanzania: A cross-sectional study. Malawi Med J. 2017 Mar;29:43–52. PubMed PMID: 28567196; PubMed Central PMCID: PMCPMC5442491. eng.
- Brennan AT, Long L, Useem J, et al. Mortality in the first 3 months on antiretroviral therapy among HIV-positive adults in low- and middle-income countries: a meta-analysis. J Acquir Immune Defic Syndr. 2016 Sep 1;73:1–10. PubMed PMID: 27513571.
- UNAIDS. On world AIDS day, UNAIDS warns that men are less likely to access HIV treatment and more likely to die of AIDS-related illnesses. 2017. Available from: http://www.unaids.org/en/resources/presscentre/pressreleaseandstatementarchive/2017/december/20171201_blind_spot
- Cornell M, Cox V, Wilkinson L. Public health blindness towards men in HIV programmes in Africa. Trop Med Int Health. 2015 Dec;20:1634–1635. PubMed PMID: 26325025.
- Cornell M, Johnson LF, Wood R, et al. Twelve-year mortality in adults initiating antiretroviral therapy in South Africa. J Int AIDS Soc. 2017 Sep 25;20:21902. PubMed PMID: 28953328; PubMed Central PMCID: PMCPMC5640314.
- Maman D, Pujades-Rodriguez M, Subtil F, et al. Gender differences in immune reconstitution: a multicentric cohort analysis in sub-Saharan Africa. PLoS One. 2012;7:e31078. PubMed PMID: 22363550; PubMed Central PMCID: PMCPMC3281917.
- Tymejczyk O, Brazier E, Yiannoutsos CT, et al. Changes in rapid HIV treatment initiation after national “treat all” policy adoption in 6 sub-Saharan African countries: regression discontinuity analysis. PLoS Med. 2019 Jun;16:e1002822. PubMed PMID: 31181056; PubMed Central PMCID: PMCPMC6557472.
- WHO. Guidelines on HIV self-testing and partner notification. Geneva, Switzerland: WHO; 2016.
- Sharma M, Barnabas RV, Celum C. Community-based strategies to strengthen men’s engagement in the HIV care cascade in sub-Saharan Africa. PLoS Med. 2017 Apr;14:e1002262. PubMed PMID: 28399122; PubMed Central PMCID: PMCPMC5388461.
- Hakim J, Musiime V, Szubert AJ, et al. Enhanced prophylaxis plus antiretroviral therapy for advanced HIV infection in Africa. N Engl J Med. 2017 Jul 20;377:233–245. PubMed PMID: 28723333; PubMed Central PMCID: PMCPMC5603269.
