ABSTRACT
Background: One key challenge in improving surgical care in resource-limited settings is the lack of high-quality and informative data. In Ethiopia, the Safe Surgery 2020 (SS2020) project developed surgical key performance indicators (KPIs) to evaluate surgical care within the country. New data collection methods were developed and piloted in 10 SS2020 intervention hospitals in the Amhara and Tigray regions of Ethiopia.
Objective: To assess the feasibility of collecting and reporting new surgical indicators and measure the impact of a surgical Data Quality Intervention (DQI) in rural Ethiopian hospitals.
Methods: An 8-week DQI was implemented to roll-out new data collection tools in SS2020 hospitals. The Kirkpatrick Method, a widely used mixed-method evaluation framework for training programs, was used to assess the impact of the DQI. Feedback surveys and focus groups at various timepoints evaluated the impact of the intervention on surgical data quality, the feasibility of a new data collection system, and the potential for national scale-up.
Results: Results of the evaluation are largely positive and promising. DQI participants reported knowledge gain, behavior change, and improved surgical data quality, as well as greater teamwork, communication, leadership, and accountability among surgical staff. Barriers remained in collection of high-quality data, such as lack of adequate human resources and electronic data reporting infrastructure.
Conclusions: Study results are largely positive and make evident that surgical data capture is feasible in low-resource settings and warrants more investment in global surgery efforts. This type of training and mentorship model can be successful in changing individual behavior and institutional culture regarding surgical data collection and reporting. Use of the Kirkpatrick Framework for evaluation of a surgical DQI is an innovative contribution to literature and can be easily adapted and expanded for use within global surgery.
Responsible Editor Jennifer Stewart Williams, Umeå University, Sweden
Background
One of the challenges in improving global surgical care is the lack of data on the current state of surgical systems, especially in resource-limited settings [Citation1]. In 2015, the Federal Ministry of Health (FMoH) of Ethiopia launched Saving Lives Through Safe Surgery (SaLTS), a 5-year national flagship initiative to build capacity at all levels of the healthcare system to improve access to safe surgical and anesthesia care [Citation2]. One of SaLTS’ key focus areas, Monitoring, and Evaluation, is intended to build evidence around the current state of surgery in Ethiopia and the impact of SaLTS implementation [Citation2].
SaLTS, in collaboration with Harvard Medical School’s Program in Global Surgery and Social Change (PGSSC), developed 15 surgical key performance indicators (KPIs) () that could feasibly be collected at the facility level and reported nationally. This was one component of the Safe Surgery 2020 (SS2020) program, a multi-stakeholder initiative funded by GE Foundation with the primary objective of building surgical capacity in developing countries through implementation of a suite of interventions [Citation2,Citation3]. These indicators are intended to provide a longitudinal and comprehensive overview of national surgical performance. A 16th indicator, surgical referrals out of the hospital, was added to specifically evaluate SS2020 programs.
Table 1. Surgical key performance indicators (KPIs) developed by PGSSC and FMoH SaLTS team
To assess the feasibility of collecting and reporting these indicators at the facility level, new data collection methods were developed and piloted in 10 SS2020 intervention hospitals in the Amhara and Tigray regions of Ethiopia [Citation4]. These methods expanded on existing collection and reporting mechanisms to ensure a more streamlined implementation process. Existing FMoH surgical patient registries were updated to include all data components needed for calculation of 12 core KPIs (). Alternate data collection methods were developed for four indicators that were not feasible to capture in these registries. To efficiently roll-out the new tools in pilot hospitals, a Data Quality Intervention (DQI) was implemented and consisted of (1) a comprehensive 3-day training program and (2) 7 weeks of on-site mentoring for all training participants.
This study measures the successes and challenges of the DQI using the Kirkpatrick Method, the most widely utilized and verified mixed-method evaluation tool for training programs [Citation5]. This study is one of the first to use the Kirkpatrick framework to evaluate a training program in a global surgery context and aims to evaluate (1) the impact of the intervention on surgical data quality improvement, (2) the feasibility of a new data collection system, and (3) the potential for national scale-up.
Methods
Program design
As part of the SS2020 initiative, the Ethiopian FMoH selected five hospitals in the Amhara region and five hospitals in the Tigray region to receive a number of interventions to increase surgical capacity. These hospitals were used as the pilot sites for the DQI and are evaluated in this study. Site visits were conducted prior to implementation to inform the training and overall design of the intervention. Current data collection and reporting methods were noted in these visits, which informed the development of novel collection methodology.
Led by the PGSSC team, the 8-week DQI included a regional training of local surgical mentors, hospital management, and key surgical staff from each hospital. Participants were trained on the importance of data quality and monitoring and evaluation in surgery, understanding the surgical KPIs, and using new registries for data collection. A subgroup of participants known as KPI focal persons were also trained to enter registry data on REDCap, an electronic data capture platform [Citation6]. Post-training, local mentors and PGSSC team members conducted weekly supportive supervision visits to the hospitals with the goal of collecting 1 month of high-quality patient registry data, which would be used to calculate the KPIs. The hospitals’ progress and experiences were shared at a reporting workshop at the conclusion of the intervention. Additional details about the program and the preliminary KPI data are found in this study’s complementary abstracts on implementation of a surgical data quality improvement intervention [Citation4,Citation7–10].
Evaluation of the training program
The regional training and its subsequent period of facility-based mentorship were evaluated using the Kirkpatrick model, which is used across many disciplines to measure impact of training courses [Citation5]. Main outcomes were assessed across four levels. Level 1 (reaction) assesses participants’ perceptions on the enjoyment, relevance, and engagement in the training. Level 2 (learning) assesses the degree to which knowledge and skills are acquired and learned. Level 3 (individual behavior) assesses the application of knowledge and/or skills into personal practice. Level 4 (institutional behavior) assessed institutional change and data quality improvements in the hospital. A mixed-methods approach was used to understand the impact of the DQI on these components and guide future improvements.
Kirkpatrick Level 1 assessed the reactions, perceptions, and attitudes of the participants immediately after the initial 3-day DQI training. Individuals were provided with a questionnaire consisting of (1) trainer-centered and learner-centered statements accompanied by a 4-point Likert scale and (2) open-answered questions to provide more feedback and opportunity for participants to reflect on the training.
Level 2 assessed (a) KPI knowledge attainment and (b) subsequent accuracy of implementation of that knowledge. Level 2a consisted of a pre- and post-test of 15 multiple-choice questions covering the training material, administered at the beginning and end of the 3-day training, respectively. Participants were encouraged to indicate their answer and their confidence in the correctness of that answer. Level 2b assessed the overall quality of data captured in the new surgical patient registries and accuracy of electronic data entry. Three registry and REDCap data quality checks were retrospectively conducted immediately post-intervention using registry accuracy, data entry verification, and KPI calculation accuracy.
Level 3 consisted of a 16-item Likert-scale questionnaire administered at the end of the DQI, which assessed the extent of individual behavior change among participants.
Level 4 measured the extent of institutional change and consisted of a 10-item Likert-scale questionnaire administered to all participants, and a focus group at each hospital to discuss the training, data collection and reporting, the intervention as a whole, and other concerns regarding the improvement of the quality of surgical data at their facility. This was performed at the conclusion of the 8-week intervention. All DQI participants were invited, in-person, to attend the focus groups for their respective hospitals. Focus group discussions (FGDs) were semi-structured and included questions designed to understand the primary facilitators and barriers to new learning and behavior change during the DQI. The FGDs were moderated by two male Ethiopian doctoral student researchers trained in qualitative research. PGSSC staff that led the DQI assisted in facilitation of each group since participants did not have prior relationships with the researchers. Researchers assured participants of their external, unbiased roles as evaluators. Each group was conducted over 45 minutes in Amharic and Tigrinya, the local languages of Amhara and Tigray, respectively. Responses were audio-recorded, translated, and transcribed into English for analysis. Field notes were also recorded.
All tools were developed by PGSSC, and informed by existing literature on application of the Kirkpatrick model in evaluations [Citation5,Citation11–14]. Surveys were administered in English, on paper, with interpreters available if needed. All survey and focus group participants were informed of the study components and provided verbal consent to participate. IRB approval was obtained for all activities by both Harvard Medical School and the Ethiopian Public Health Institute.
Data analysis
This evaluation study used a concurrent embedded approach to mixed-methods analysis [Citation15]. Quantitative tools assessed the degree of knowledge gain by the participants and their perception of behavior change in themselves and the surgical team, while the qualitative tools allowed more in-depth exploration of the mechanisms for change and the extent of impact.
Level 1 results were analyzed quantitatively by calculating median responses to Likert questions. Open-ended questions were recorded and saved to inform further iterations of the training design.
For level 2a, test score, confidence score, and confidence indicator were all calculated pre- and post-test to determine knowledge improvement during the regional training component of the DQI. First, knowledge test scores were calculated on a percentage scale indicating the percentage correct. Second, a confidence score was developed based on Gardner-Medwin confidence-based assessments [Citation12]. Responses were weighted based on whether the answer was correct and the participant-indicated degree of confidence. Respondents were able to indicate Low Confidence (C = 1), Medium Confidence (C = 2), and High Confidence (C = 3). This methodology rewards high confidence, correct answers and punishes high confidence, incorrect answers. Finally, dividing the confidence score by the test score provides the value of the confidence indicator, which measures the degree to which participants are confident in their understanding of the subject material. A value of 1.00 to 1.50 shows high confidence and understanding, while values less than 1.00 indicate over- or under-confidence in the participant’s understanding of the knowledge. Over-confidence results from many high confidence, wrong answers; under-confidence results from many low confidence, correct answers. The lower the confidence indicator, the more overconfident a participant is in their knowledge.
Level 2b data quality checks were analyzed using a three pronged-approach: (1) Cross-Registry Consistency in data components found across multiple registries was assessed with enumeration of inconsistencies in a 10% random sample of patient cases, (2) Data Entry Verification was conducted by reviewing a random sample of 10% of patients to tally errors in data entry of paper registries, and (3) Calculation Accuracy was evaluated by determining percent error between 5 KPI values calculated from REDCap data (the measured value) and values calculated directly from registries (the accepted value from source data).
Individual and institutional behavior change were assessed in Levels 3 and 4. Likert scale responses from questionnaires were tabulated in Excel and the median response was measured for each item. Behavior change was also measured by FGDs in Level 4 and analysis consisted of multiple steps that follow standard qualitative analysis methodologies, primarily focusing on grounded theory [Citation16,Citation17]. Five authors coded each transcript independently to generate preliminary thematic codes and identify representative quotes. After a series of discussions, the team consolidated and summarized emerging themes when consensus and saturation were reached.
Results
Training reaction (level 1)
From February to March 2018, 34 personnel from 5 hospitals attended the Amhara regional training, while 38 personnel participated across 5 hospitals from April to May 2018 in Tigray. All 72 attendees were enrolled in the Kirkpatrick study with verbal assent. Of these attendees, approximately 66% were male and 34% were female. About 66% reported having clinical roles in their respective hospitals, while 23% reported having an administrative or data management role. The remaining 11% were in leadership roles with clinical backgrounds. Overall, the reaction to the training was positive, with the majority of participants either ‘agreeing’ or ‘strongly agreeing’ with the largely positive, trainer- and learner-centered statements provided on reaction surveys [Citation13]. The median response for each of the seven statements was 4, indicating that the participants strongly agreed that the training was enjoyable, helpful, valuable, and increased understanding and confidence in the participants about collection and reporting of the surgical key performance indicators.
Knowledge gain (level 2)
Testing & confidence
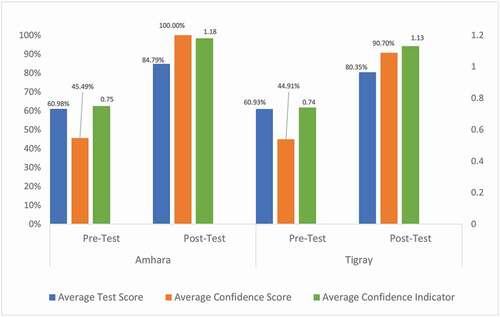
There was an overall increase in participants’ test scores, confidence scores, and confidence indicators from pre-test to post-test (). Average test score increased by 23.81% in Amhara and 19.42% in Tigray. Average confidence score increased by 54.51% in Amhara and 45.79% in Tigray. Average confident indicator increased by 0.43 points in Amhara (0.75 to 1.18) and 0.39 points in Tigray (0.74 to 1.13). Both confident indicator improvements represent changes in participants’ confidence in correct answers. At pre-test, 37 of the 72 (51%) participants across regions were overconfident in their answers, while at post-test 16 of 72 (22%) participants were overconfident.
Registry & data entry accuracy
The results of the data quality assessments are as follows:
(1) Cross-Registry Consistency: A manual review of 932 data fields across 85 randomly selected patient cases in the 10 intervention hospitals found minimal inconsistencies across registries (7.6%); (2) Data Entry Verification: An assessment of the same 85 patient cases in REDCap identified data entry errors from the registries to REDCap in 14.7% of all data fields reviewed; (3) Calculation Accuracy: The percent error between KPIs calculated using the patient registries (source data) and REDCap data were greater than 5% for 17 of 50 compared values ().
Table 2. Key performance indicator (KPI) calculation comparison, REDCap v. registry (Kirkpatrick level 2)
Behavioral change (levels 3–4)
Quantitative results
On the Level 3 and 4 questionnaires, individual behavior change was measured by nine items and institutional behavior change was measured by 5. Median response for both sets of items was 3. On average, 84% of participants ‘agreed’ or ‘strongly agreed’ that individual behavior changes were observed after attending the training, while, on average 93%, agreed that institutional behaviors were observed ().
Figure 2. Percentage of participants who agree and strongly agree with program success, individual behavior change, and institutional behavior change items following the intervention (Kirkpatrick levels 3 & 4)
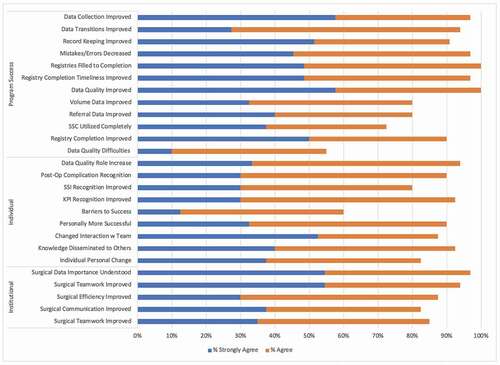
Twelve items on the questionnaires were designed to measure program-related change (). These focused on data quality change, implementation of the data collection system, and how understanding of the indicators improved. Median response for program success items was 3. On average, 92% of participants ‘agreed’ or ‘strongly agreed’ that program successes were observed after attending the training.
Qualitative results
Of the 72 participants that assented to this study, 64 (89%) participated in the FGDs. Ten focus groups were implemented, one in each intervention hospital; approximately four to eight participants attended each FGD. Non-response was attributed to lack of availability. Examples of behavior change emerged in FGDs. Participants shared how the intervention changed their roles and perspectives on data. Five prominent themes emerged that provide a positive overview of the effect of the training program and subsequent mentorship on intervention hospitals (). Participants identified areas of improvement and three primary challenges to intervention implementation ().
Table 3. Qualitative impact of training as perceived by participants, grouped by theme (Kirkpatrick level 4)
Table 4. Reported challenges to implementation, grouped by theme (Kirkpatrick level 4)
Training successes
Knowledge gain and data usage
The trainees’ understanding of the necessity of data and consequences of inaccurate or missing data was stressed among all hospitals. Respondents highlighted core KPIs that they believed to be especially necessary, including Safe Surgery Checklist (SSC) utilization, surgical referrals out, surgical volume, and anesthesia complications (). On-site mentoring was highlighted as a significant reason for the improved data knowledge. The hospitals developed quality improvement projects with a better understanding of the indicators and their importance in ‘planning, research, and decision [making]’ regarding surgical care.
Increased sense of agency
Participants expressed improved confidence in and understanding of their role, including expanded responsibilities for data collection and reporting. Most respondents agreed that a sense of ownership and/or accountability of the data management systems increased in their hospitals due to the greater clarity of data ownership roles following the trainings.
Improved teamwork and communication
The training provided opportunity for greater collaboration among surgical teams to collect and report data. Many respondents noted improvement to the workflow within surgical teams, with everyone doing their part to record and report data. Some respondents noted that training objectives were embraced by hospital management. One hospital reported that the learnings were applied to other non-surgical units. Teamwork and communication were stressed as being crucial to the successful implementation of an improved data management system.
Improved data management systems and data quality
Translating the trainings into practice is a critical component of the intervention. Respondents almost unanimously agreed that the new registries better captured KPIs than the old data system, especially the new Surgical Site Infection Logbook. With clarity on data ownership established during the trainings, the process of recording and reporting data was simplified and facilitated the input of more complete and accurate data.
Motivation to improve quality of surgical services
A long-term goal of this intervention was to affect change in the patient safety culture, utilizing the new understanding of data and collection mechanisms to inform safer practices. Participants spoke about how surgical safety is important but had not been a priority prior to this intervention. The DQI helped them better understand how data informs better surgical services and motivated them to apply KPIs to improve services and processes.
Challenges to implementation
The primary challenge to implementation immediately post-training was lack of staff buy-in. While many key staff at each hospital were present during training, other integral staff to the data management process were absent. Training participants experienced difficulties in receiving ‘second-hand’ support from these staff. Attempting to shift the culture around data for non-training staff proved to be difficult, but, ultimately, successful.
Lack of human resources to effectively implement training objectives in the long term was another challenge. New responsibilities for existing staff under the new data management system led to additional work. Respondents suggested automation of data entry and reporting to combat the lack of human resources while also acknowledging that the lack of computers and reliable internet connectivity were major impediments. There were specific complaints about the format of the new registries, which were not customized to each facility. Some hospitals would have preferred separate OR registries for the obstetrics units and surgical units; others felt that the registries were missing important data fields.
Due to frequent turnover of staff, respondents identified the need for additional training and on-site mentorship to build institutional knowledge of the KPIs and the new data management systems. Regular ‘review’ meetings were noted as a means to prevent relapse to the old system. Some respondents requested periodic training refreshers for ‘timely identification of the strong and weak parts of our activities,’ as they were concerned that ‘unless mechanisms are designed for continuous onsite training, there might be interruption on data quality management.’
Discussion
Interpretation of results
This paper describes the evaluation of a DQI for the collection and reporting of surgical KPIs in Ethiopia using the Kirkpatrick model. Participants agreed that the DQI effectively met its objectives. Knowledge and confidence improved pre to post-testing. Data quality checks identified areas of improvement in data captured, yet discrepancies and mistakes were seen in fewer than 15% of cases. Qualitatively, participants agreed that there were impactful changes in individual behavior and institutional culture.
Each evaluation tier provided insight into key areas of impact. Level 1 training reaction results showed improved knowledge of the KPIs, increased comfort with the new registries, and better understanding of the data collection methods. Improvement in participant test scores, confidence scores, and confidence indicators in Level 2a reflect the increase in understanding of the aforementioned components. A post-test confidence indicator greater than 1.00 in both regions indicates all participants had a good grasp of what information they know versus information they do not. To our knowledge, this is the first time that Gardner-Medwin confidence scores and indicators have been included in the Kirkpatrick Evaluation [Citation14].
Level 2b revealed quality issues in data collection and entry. The input of data in the paper-based surgical registries had minimal inconsistencies across registries and few missing fields. However, verification of data entered into REDCap shows discrepancies from the paper-based source data. The electronic data entry errors reflect a misunderstanding of REDCap, a new tool to all participants. Lack of adequate staffing to implement this task may have contributed to the mistakes identified. This shows the difficulty of implementing an accurate and reliable registry and data entry system in a low-resource setting [Citation6].
Mixed-method analysis in Levels 3 and 4 revealed that participants agreed that both individual behavior and team behavior changed because of the intervention. The DQI was perceived to be successful in improving data quality, indicator understanding, and data collection system use. The main FGD themes () indicate that this program can be effective in providing the knowledge and agency that individuals and teams need to successfully implement a DQI. The combination of intensive training and supportive supervision created an environment in which participants felt comfortable and knowledgeable on the indicators, the use of the new registries, and the data collection [Citation18].
The challenges to implementation highlight difficulties in changing data culture within a hospital. Main challenges resulted from lack of buy-in, lack of human resources, and need for additional training and mentorship. Staff turnover also affected implementation. Individuals on-boarded after the training did not feel knowledgeable about the DQI. More emphasis on human resource pipelines and additional trainings and mentorship could alleviate these issues. Modifying the intervention specifically to each hospital setting also could lead to higher uptake and success.
Results in the context of literature
While the Kirkpatrick Model has been used to assess a training for the WHO SSC, this is the first instance it has been used to evaluate a DQI in global surgery [Citation19]. Previous mentoring training programs in Sub-Saharan Africa using Kirkpatrick agree that mentoring is critical to the implementation of training programs in global surgery [Citation19–21].
Improved knowledge is consistent with other trainings evaluated using the Kirkpatrick method in low-and-middle income countries (LMICs). Dorri and colleagues found favorable reaction, knowledge gain, and behavior change among a CPR in-service training in Iran [Citation22]. A study in Laos found positive results of continuing professional development training among providers [Citation23].
FGDs revealed that buy-in from local, regional, and national partners was important to program success. These findings are consistent with other studies that found that scale-up is dependent on active partners, mentorship, and collaboration [Citation20,Citation21] Participants also reflected on the benefit of mentors’ visits. In order to maintain high-quality data systems, literature supports that routine audits and mentoring need to continue to ensure sustainability [Citation24,Citation25].
Implications and recommendations
The results of this study are largely positive and make evident that surgical data capture is feasible in low-resource settings and warrants more investment in the field of global surgery. This type of training and mentorship model can be successful in changing individual behavior and institutional culture regarding surgical data collection and reporting. The use of the Kirkpatrick Framework for evaluation of a surgical DQI is an innovative contribution to the literature and can be easily adapted and expanded for use within global surgery.
This study has provided sufficient evidence to warrant further exploration of scale-up of surgery DQIs in Ethiopia and other LMICs. To further this end and ensure sustainability of positive changes seen in intervention hospitals, the Ethiopian FMoH and collaborating partners should be encouraged to take ownership of the program. We recommend a two-pronged approach to adaptation and scale-up at a national level: (1) scaling the surgical registries that were piloted for this intervention across all hospitals providing surgical care in the country, and (2) implementing a similar DQI to accompany a national rollout of the aforementioned registries. Because our DQI was resource-intensive, significant adaptation of the latter component may be necessary to accommodate national implementation.
Limitations
Our evaluation has limitations. Since the KPI knowledge post-test was only administered immediately following the regional training, knowledge retention was not measured. Surveys were conducted in English with translation available upon request, which may have been a barrier for non-English speaking respondents who did not make this request.
Since most data are self-reported, responder bias may exist. Bias from participants’ fear of speaking critically about colleagues or hospital systems may arise as well. The study subjects were limited to training participants; perspectives of non-participants affected by the intervention were not assessed.
Only primary and general hospitals participated in the intervention, so lessons learned cannot be generalized to regional and national hospitals. Despite these limitations, our mixed-methods evaluation design remains rigorous and holistically captures the impact the training made on the participants and the hospitals.
Conclusion
The results of this DQI provide insights into a few key areas of impact: a measurable gain in knowledge and understanding of surgical data; mixed results about the efficiency of data quality and electronic entry; increased confidence on the subject; general consensus on positive individual behavior change through proactive engagement in data collection and reporting; and noticeable impact on institutional culture around data integrity and its role in decision-making. To ensure sustained impact of the program and to potentially motivate national scale-up, further alignment of our efforts with Ethiopian stakeholders will be crucial. It will be important to act quickly to build on the momentum of the program and the global surgery movement.
Author contributions
All authors have made substantial contributions to the conception or design of the work or the acquisition, analysis, or interpretation of data for the work; have been involved in drafting the work or revising it critically for important intellectual content; have provided final approval of the version to be published; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ethics and consent
All study participants were informed of the study components and provided verbal consent to participate. IRB approval was obtained for all activities by both Harvard Medical School and the Ethiopian Public Health Institute.
Paper context
The availability of high-quality surgical data is an ongoing challenge in low-resource settings. An innovative Data Quality Intervention (DQI) was implemented in rural Ethiopia. Evaluation results were positive and make evident that surgical data capture is feasible in low-resource settings and warrants more investment in global surgery efforts. This type of training and mentorship model can be successful in changing individual behavior and institutional culture regarding surgical data collection and reporting and should be scaled.
Acknowledgments
Authors would like to acknowledge all partners involved in implementation of this project: The SaLTS team within the Federal Ministry of Health and Tigray and Amhara Regional Health Bureaus were instrumental in the development of the key performance indicators (KPIs) and surgical logbooks for data collection. Jhpiego, Assist International, and Dalberg were integral programmatic partners as part of Safe Surgery 2020. The World Federation of Societies of Anesthesiologists and Lifebox provided support during development of the KPIs and training materials. The Surgical Society of Ethiopia (SSE) and Ethiopian Society of Anesthesiologists (ESA) provided collaboration and mentors for the project. Specifically, we would like to thank the lead mentors involved in implementation: Zebenaye Bitew, Bazezew Fekad, Mulat Mosse, Minwuyelet, Haftom Berhane, Yibrah Berhe, Tadesse Teklit, and Reiye Esayas.
Disclosure statement
Financial support for this research, including partial salary support for some authors, was provided through a grant from the GE Foundation [5R18HS024235-02]. All authors have completed the ICMJE uniform disclosure form for our records.
Additional information
Funding
References
- Meara JG, Leather AJM, Hagander L, et al. Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386:569–11.
- Burssa D, Teshome A, Iverson K, et al. Safe surgery for all: early lessons from implementing a national government-driven surgical plan in Ethiopia. World J Surg. 2017;41:3038–3045.
- Tadesse H, Sibhatu M, Maina E, et al. Savings lives through safe surgery in Ethiopia: project implementation manual. Addis Ababa; 2019. Dalberg.
- Incorvia J, Bari S, Garringer K, et al. Results of a surgical key performance indicator data intervention in rural Ethiopia hospitals. 10th Annual Consortium of Universities for Global Health Global Health Conference; 2019 Mar 8–10; Chicago (IL).
- Kirkpatrick DL, Kirkpatrick JD. Evaluating training programs: the four levels. 3rd ed. San Francisco (CA): Berrett-Koehler; 1998.
- Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381.
- Bari S, Incorvia J, Drown L, et al. Data quality assessment of surgical registries & electronic data entry in rural Ethiopian hospitals. 10th Annual Consortium of Universities for Global Health Global Health Conference; 2019 Mar 8–10; Chicago (IL).
- Drown L, Incorvia J, Bekele A, et al. Development of an intervention to improve surgical data quality at hospitals in Ethiopia. 2nd Yale Global Surgery Symposium; 2018 Apr 28–30; New Haven (CT).
- Drown L, Ahearn O, Garringer K, et al. Developing the monitoring and evaluation pillar of Ethiopia’s national surgical plan: saving lives through safe surgery. College of Surgeons of East, Central, and Southern Africa (COSECSA) 2018 AGM and Scientific Conference; 2018 Dec 5–8;Kigali (Rwanda).
- Garringer K, Ahearn O, Incorvia J, et al. Reasons for surgical referral in rural Ethiopian hospitals. 14th Annual Academic Surgical Congress; 2019 Feb 5–7; Houston (TX).
- Rouse DN. Employing Kirkpatrick’s evaluation framework to determine the effectiveness of health information management courses and programs. Perspect Health Inf Manag. 2011;8:1c.
- Gardner-Medwin AR, Gahan M. Formative and summative confidence-based assessment. Proceedings of the 7th CAA Conference; 2003; London (UK).
- Kirkpatrick J. The new world level 1 reaction sheets. Newnan (GA): The Kirkpatrick Partners, LLC; 2016.
- Gardner-Medwin AR, Curtin NA. Certainty-based marking (CBM) for reflective learning and proper knowledge assessment. REAP International Online Conference on Assessment Design for Learner Responsibility; 2007 May 29–31; Online.
- Creswell JW, Plano Clark VL, Gutman ML, et al. Advanced mixed methods research designs. In: Tashakkori A, Teddlie C, editors. Handbook of mixed methods in social & behavioral research. Thousand Oaks (CA): Sage Publications; 2003:209–240.
- Glaser BG, Strauss AL. The discovery of grounded theory: strategies for qualitative research. 1st ed. New Brunswick (NJ): Aldine Transaction; 1967.
- Miles M, Huberman A. Qualitative data analysis: an expanded sourcebook. Thousand Oaks (CA): Sage Publications; 1994.
- Rowe SY, Peters DH, Holloway KA, et al. A systematic review of the effectiveness of strategies to improve health care provider performance in low- and middle-income countries: methods and descriptive results. PLoS One. 2019;14:e0217617.
- Close KL, Baxter LS, Ravelojaona VA, et al. Overcoming challenges in implementing the WHO surgical safety checklist: lessons learnt from using a checklist training course to facilitate rapid scale up in Madagascar. BMJ Glob Health. 2017;2:e000430.
- White MC, Randall K, Ravelojaona VA, et al. Sustainability of using the WHO surgical safety checklist: a mixed-methods longitudinal evaluation following a nationwide blended educational implementation strategy in Madagascar. BMJ Glob Health. 2018;3:e001104.
- White MC, Baxter LS, Close KL, et al. Evaluation of a countrywide implementation of the world health organization surgical safety checklist in Madagascar. PLoS One. 2018;13:e0191849.
- Dorri S, Akbari M, Sedeh MD. Kirkpatrick evaluation model for in-service training on cardiopulmonary resuscitation. Iran J Nurs Midwifery Res. 2016;21:493–497.
- Yoon HB, Shin J, Bouphavanh K, et al. Evaluation of a continuing professional development training program for physicians and physician assistants in hospitals in Laos based on Kirkpatrick model. J Educ Eval Health Prof. 2016;13:21.
- Gimbel S, Mwanza M, Nisingizwe MP, et al. Improving data quality across 3 sub-Saharan African countries using the consolidated framework for implementation research (CFIR): results from the African health initiative. BMC Health Serv Res. 2017;17:828.
- Wagenaar BH, Hirschhorn LR, Henley C, et al. Data-driven quality improvement in low-and middle-income country health systems: lessons from seven years of implementation experience across Mozambique, Rwanda, and Zambia. BMC Health Serv Res. 2017;17:830.