ABSTRACT
Background
Respectful maternity care is a fundamental human right, and an important component of quality maternity care.
Objective
The aim of this study was to quantify the frequency and categories of D&A and identify factors associated with reporting D&A among women in north Showa zone of Ethiopia.
Method
A cross-sectional study was conducted with 435 randomly selected women who had given birth at public health facility within the previous 12 months in North Showa zone of Ethiopia. A digital (tablet-based) structured and researcher administered tool was used for data collection. Frequencies of D&A items organised around the Bowser and Hill categories of D&A and presented in the White Ribbon Alliance’s Universal Rights of Childbearing Women Framework were calculated. Multivariable logistic regression was used to identify the association between experience of disrespect and abuse and interpersonal and structural factors at p-value <0.05 and odds ratio values with 95% confidence interval.
Results
All participants reported at least one form of disrespect and abuse during childbirth. Types of disrespect and abuse experienced by participants were physical abuse 435 (100%), non-consented care 423 (97.2%), non-confidential care 288 (66.2%), abandonment/neglect (34.7%), non-dignified care 126 (29%), discriminatory care 99 (22.8%) and detention 24 (5.5%). Hospital birth [AOR: 3.04, 95% CI: 1.75, 5.27], rural residence [AOR: 1.44, 95% CI: 0.76, 2.71], monthly household income less than 1,644 Birr (USD 57) [AOR: 2.26, 95% CI: 1.20, 4.26], being attended by female providers [AOR: 1.74, 95% CI: 1.06, 2.86] and midwifery nurses [AOR: 2.23, 95% CI: 1.13, 4.39] showed positive association with experience of disrespect and abuse.
Conclusion
Hospital birth showed consistent association with all forms of disrespect and abuse. Expanding the size and skill mix of professionals in the hospitals, sensitizing providers consequences of disrespect and abuse could promote dignified and respectful care.
Responsible Editor
Maria Emmelin
Background
While motherhood is often considered a fulfilling positive experience, pregnancy and childbirth-related complications are a leading cause of death for women of child-bearing age in developing countries [Citation1]. Developing countries contribute 94% of global maternal deaths and more than half of these deaths occur in sub-Saharan Africa [Citation2]. Ethiopia’s maternal mortality ratio, 401 per 100,000 live births in 2017, is one of the highest globally [Citation3]. Birthing outside of a health facility without a skilled birth attendants present is the major reason behind this loss of life in Ethiopia [Citation4,Citation5].
Ethiopia aims to reduce its maternal mortality ratio to less than 70 per 100,000 live births by 2030 in order to achieve the United Nations Sustainable Development Goal 3 [Citation6]. The Sustainable Development Goals are the blueprint to achieve a better and more sustainable future for all. Sustainable Development Goal 3 is about ‘Good Health and Well-being’ and is one of the 17 Sustainable Development Goals established by the United Nations in 2015. Ensuring access to quality obstetric care is essential as it has the potential to reduce up to 75% of preventable deaths [Citation7,Citation8]. The proportion of Ethiopian women who report having difficulty accessing health care decreased from 96% in 2005, to 70% in 2016 [Citation9]. However, only 48% of women gave birth at health facility in 2019. Improving respectful maternity care has been flagged as a potential strategy for reducing preventable maternal mortality and morbidity, and to accelerate progress towards meeting the Sustainable Development Goal targets for improving maternal health [Citation10].
Respectful maternity care is a key element of quality maternity care [Citation11]. It is an approach that stresses positive interpersonal interactions between providers and women, throughout maternity care [Citation12]. Women’s right to respectful and dignified health care throughout pregnancy and childbirth has become a central focus in intervention strategies that seek to reduce maternal mortality [Citation13]; disrespect and abuse (D&A) affects women’s trust in care providers and the health system deterring them from seeking and using maternity care [Citation12]. This highlights the need for maternity care to be competent and respectful if women are to use it [Citation11].
Disrespectful treatment ranges from denial of a woman’s right to make informed decisions and being scolded for demanding their rights [Citation14], to denial of anaesthesia while performing and repairing episiotomies [Citation15]. The White Ribbon Alliance categorise D&A in childbirth into seven categories: physical abuse, non-dignified care, non-consented care, non-confidential care, abandonment, discrimination, and detention. Each category has more than one verification criteria with ‘Yes’ or ‘No’ dichotomized responses. According to White Ribbon Alliance, verification criteria/manifestations of D&A often fall into more than one category, so that categories are not intended to be mutually exclusive. Rather categories should be seen to be overlapping along a continuum [Citation16]. International human rights frameworks highlight D&A of women during childbirth as a key human rights issue [Citation17–20], and a human rights based approach to birthing care has become a primary concern [Citation21].
Research from different parts of Ethiopia has identified growing evidence of disrespectful and abusive care during labour and childbirth regardless of women’s socio-demographic characteristics, such as age and level of education. However, some groups of women, such as unmarried women, women from low economic status and women with HIV sero positive status are more vulnerable to D&A based on these specific attributes [Citation22–34]. Comprehensive information regarding D&A of women during childbirth is needed in order to more effectively implement policies, change practice, and culture and improve standards of care [Citation35]. However, the experience of D&A and its determinants are not well understood. Thus, the aim of this study is to quantify the frequency and categories of D&A during facility-based childbirth and identify factors associated with reporting D&A among women in north Showa zone of Ethiopia.
Methods
Study design and setting
This study was conducted as part of a larger mixed methods study that examined disrespect and abuse of women during facility-based childbirth in Ethiopia. A community-based cross-sectional study (conducted in community settings rather than in a facility or institution) was conducted from 5 October 2019 to 25 January 2020 in North Showa zone of Ethiopia. The zone is located 110 km to north of the capital Addis Ababa. Based on the 2007 Census conducted by the Central Statistical Agency of Ethiopia, the Zone has a projected total population of 1.5 million in 2016, of whom 48% were women. North Showa zone has an area of 10,322.48 square kilometers and population density of 138.66 [Citation36]. Three hospitals, 62 health centers, 268 health posts are currently functioning in the zone. Health posts were not included in the study as they do not provide birthing care. Women from across all districts (rural and urban areas) of the North Showa zone were included via a registry held by health extension workers.
Study population and eligibility
Participants were women who had given birth at public health facilities of North Showa zone during the last 12 months preceding the survey, regardless of the birth outcome. Women who gave birth at home, those who were acutely unwell physically or mentally and those with disability which would prevent them talking to a researcher were excluded.
Study variables
The dependent variables of this research were the seven categories of D&A women experience during facility-based childbirth (physical abuse, non-dignified care, non-consented care, non-confidential care, abandonment, discrimination, and detention) organised around the Bowser and Hill categories of D&A and presented in the White Ribbon Alliance’s Universal Rights of Childbearing Women Framework [Citation16]. The independent variables of this research were sociodemographic variables (age, residence, marital, education, occupation and monthly household income), obstetric history and experience of maternity care utilization (walking distance of health facility from home, total number of live births, number of birth at health facility, antenatal care checkups, antenatal and childbirth in same facility, type of health facility visited for birth (health center vs hospital), method of birth and number of babies in most recent childbirth, profession and sex of providers who attended the birth).
Sample size determination and sampling procedures
A single population proportion formula was used to calculate the sample size with assumptions of 78.6% proportion of disrespect and abuse [Citation22], 4% precision, 95% level of confidence and a 10% non-response rate, the final sample size was 443. A list, including contact details, of women who gave birth at public health facility is maintained by health extension workers. Using this list as a sampling frame, 443 eligible women were selected by computer generated random numbers in Excel spreadsheet (Microsoft Corporation, 2013). Selection and initial contact was made in person by the health extension workers and women were invited to choose time and place of survey.
All health extension workers involved in data collection are female, have attended a one-year formal pre-service training conducted by trainers [Citation37] Through a collaboration between the Ministry of Health and the Ministry of Education. The training includes didactic and clinical training regarding (1) family health services, disease prevention and control, (3) hygiene and environmental sanitation, and (4) health education and communication [Citation38]. The main responsibilities of HEWs include health promotion, disease prevention, and treatment of uncomplicated and non-severe illnesses, such as cases of malaria, pneumonia, diarrhea, and malnutrition in the community. HEWs split their time between health posts and community settings; they are not directly connected to any birthing facilities [Citation39].
Data collection tool and procedures
Data were collected using digital, tablet-based tools, Open Data Kit Collect. A validated tool was programmed and uploaded to tablets for the survey [Citation22,Citation40]. The tool consisted of three parts. The first part contained seven questions and was used to assess the sociodemographic characteristics of participants. The second part contained 10 questions focusing on the participants’ obstetric history and experience of maternity care utilisation, and the third part included the seven categories of disrespect and abuse along with the 48 verification criteria used to measure experience of D&A. The tool was designed in English and translated to the local language, Amharic, and then back to English by a third person to check for internal consistency. The Amharic version of the tool was piloted and used to collect data face to face. Participants were surveyed in their homes or another preferred location and were accompanied by person of their choice during the survey.
Measurement
We measured D&A using a framework developed by Bowser and Hill [Citation41]. The D&A were categorised into seven groups and prevalence was calculated for each specific category. Each category has more than one verification criteria with ‘Yes’ or ‘No’ dichotomised responses. A respondent was considered to have been disrespected and/or abused for the specific category if she reported ‘Yes’ to at least one of the verification criteria in that category [Citation22].
Data quality assurance
Digital, tablet-based data collection improves quality of the data as it allows predetermined options only. Health extension workers with prior experience of tablet-based survey implementation conducted the survey following 2 days of intensive training. The health extension workers also practiced collecting data using the tablets in order to familiarize themselves with the tool prior to data collection. The data collectors were all females to make sharing ideas easier, as the topic is sensitive. The principal investigator has closely supervised the data collection process.
Data processing and analysis
The data were exported to SPSS Window version 21. Descriptive statistics were used to describe the study population in relation to relevant variables. To identify predictors of each D&A categories, bivariate logistic regressions with each potential covariate were conducted, and variables that have p-value of <0.2 were included in the final multivariable binary logistic regression models. Then, four multivariable logistic regression models (one model for each category of D&A, except for physical abuse, non-consented care, and detention), with a 95% confidence interval were fitted. Physical abuse and non-consented care were reported by too many participants, whereas the number of women who reported detention was too small. As a result, these three categories were excluded as we could not perform further statistical analyses. Adjusted odds ratios and their 95% confidence intervals were computed and statistical significance was declared at p-value of <0.05.
Results
Out of the invited 443 women, 435 agreed to participate in the study yielding a response rate of 98.1%. The mean age of respondents was 28.65 (SD = ± 5.38) ranging from 18 to 46 years. Over two-thirds, 304 (69.9%), of respondents were urban dwellers. Most 378 (86.9%) of participants were married and 100 (23%) have attended tertiary level of education, and only 77 (17.7%) of the participants reported monthly household income ≥1,644 birr ().
Table 1. Sociodemographic characteristics of participants (N = 435)
Participants’ obstetric history and experience of maternity care utilisation
More than half of the participants, 248 (57.0%) walk between 30 to 60 minutes to reach the nearest health facility. The majority, 316 (72.6%), had prior experience of giving birth at a health facility. Most, 395 (90.8%), of the study participants had antenatal care follow-up for their recent pregnancy, of which, 345 (87.3%) gave birth in same facility where they received antenatal checkups. About half, 223 (51.3%) gave birth in health centres. Midwives/nurses attended 255 (58.6%) of the women during birth. Approximately half 217 (49.9%) of women participants reported they were attended by male care providers .
Table 2. Obstetric history of participants (N = 435)
Forms of disrespect and abuse reported by participants
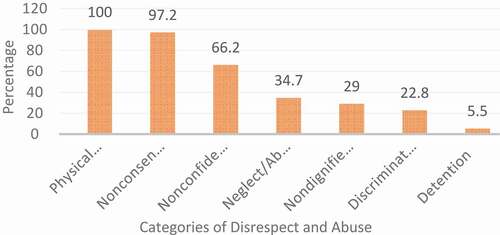
Frequencies of D&A items organised around the Bowser and Hill categories of D&A and presented in the White Ribbon Alliance’s Universal Rights of Childbearing Women Framework were calculated. As a result, the prevalence self-reported D&A ranged from 100% for physical abuse to 5.5 for detention in health facility ().
All women have reported at least one form of D&A during birth care. Physical abuse was found to be the most prevalent (100%) category. Among the verifications of physical abuse, 413 (94.9%) women reported that they were not allowed to give birth in their preferred birthing position; whereas for 381 (87.6%) women an episiotomy was given or sutured without anesthesia. Non-consented care was the second most common category of D&A reported by 423 (97.2%) of participants. A vast majority of participants, 362 (83.2%) reported that care providers had conducted a vaginal examination without their consent. In addition, 92 (21.1%) participants reported that intrauterine device was inserted without their consent. Two-thirds, 288 (66.2%) of participants reported confidentiality of their care was breached, of which 220 (50.6%) reported absence of curtains/partitions or other measures to provide privacy. Likewise, 204 (46.9%) of participating women said vaginal examinations were not conducted privately. About one-third (34.7%) of participants felt abandoned or neglected. More than one in ten (12.9%) women said providers were not present when the baby was born. Non-dignified care was the fifth most common D&A reported by 126 (29%) participants. Among verifications of non-dignified care, 75 (17.2%) of women said providers threatened them if they did not comply and indicated that they or their baby would have a poor outcome. Similarly, 71 (16.3%) of participating women reported that healthcare providers had shouted/screamed at them during labour or birth. Nearly quarter, 99 (22.8%) of participants reported that they felt discriminated against. Discrimination amongst this group included 51 (11.7%) respondents stating healthcare providers made negative comments regarding their HIV seropositive status, whereas 37 (8.5%) women received negative comments regarding their age. In addition, 24 (5.5%) of respondents said they were detained in the facility against their will, of which, 17 (3.9%) were detained due to inability to pay hospital bills, while 13 (3.0%) were instructed to clean up their own blood or other fluid after birth ().
Table 3. Experiences of disrespect and abuse during facility-based childbirth, Ethiopia, 2020 (N = 435)
Predictors of disrespect and abuse
Four logistic regression models were constructed to examine the relationship of interpersonal and structural factors with each of the four different categories of D&A. Three forms (physical abuse, non-consented care and detention) were excluded since bivariate analysis revealed that further statistical analyses could not be performed due to the number of women who reported these categories being either too high or too small .
Table 4. Bivariate and multivariate logistic regression analysis output of factors associated with disrespect and abuse during facility-based childbirth, North Showa zone, Ethiopia, 2019
The type of health facility at which childbirth takes place, monthly household income, profession and sex of providers were found to be significantly associated with most of the D&A categories. The type of health facility at which childbirth takes place was found to be the most important statistically significant predictor of all forms of D&A; those who gave birth at hospitals were three times more likely to experience disrespect or abuse [AOR: 3.04, 95% CI: 1.75, 5.27] than those who gave birth at health centers. Experiences of disrespect or abuse were 1.4 times more likely to be reported by rural women than their urban counterparts [AOR: 1.44, 95% CI: 0.76, 2.71]. Women who have monthly household income less than 1,644 Birr (USD 57) were about two times more likely to experience disrespect or abuse [AOR: 2.26, 95% CI: 1.20, 4.26]. Regarding sex and profession of care providers, those women who were attended by female providers [AOR: 1.74, 95% CI: 1.06, 2.86] and midwives/nurses [AOR: 2.23, 95% CI: 1.13, 4.39] were more likely to report disrespect or abuse compared to those who were attended by male providers and doctors, respectively.
Discussion
Disrespect and abuse during facility-based childbirth is a global problem with varying degrees of severity and differing drivers in different contexts [Citation42]. It is often a greater problem in developing countries where inadequate number of care providers serve large proportion of clients [Citation43]. There is growing evidence in Ethiopia that women are experiencing disrespect and abuse in birthing facilities [Citation44,Citation45]. Thus, this study sought to quantify the frequency and categories of D&A and identify factors associated with reporting D&A among women in north Showa zone of Ethiopia.
Respectful maternity care is a universal right of every childbearing women; however, this study reveals that D&A are common in health facilities. Every woman who participated in this study has experienced at least one form of D&A, and this rate is higher than for any other study. This disparity is attributed to the comprehensiveness of the current research which used 48 verification criteria for the seven categories of disrespect and abuse, whereas other studies used only 25 or less [Citation22,Citation24–26,Citation28,Citation32,Citation34], which may have led to under reporting of disrespectful and abusive care. However, two studies from Arbaminch, Ethiopia and Enugu, Nigeria have reported almost similar rate 98.9% [Citation33] and 98% [Citation46] of D&A.
Physical abuse is the most prevailing category with 100% prevalence. From these, 413 (94.9%) women were not allowed to give birth in their preferred birthing position and for 381 (87.6%) women an episiotomy was given or sutured without anesthesia. Whereas 34 (7.8%) and 12 (2.8%) participants were pinched/kicked/slapped and hit with an instrument, respectively. Other research from Ethiopia reported level of physical abuse that ranged from 2% to 75.2% [Citation22,Citation24–26,Citation29,Citation31,Citation32,Citation34].
When interventions become necessary, service providers should provide the mother with sufficient information in a language she can comprehend so that she can knowingly refuse or consent to the intervention [Citation47]. However, this study found that 97.2% of participating women reported non-consented care. This finding is higher than findings of previous research across all contexts [Citation26,Citation32,Citation48]. Most, 362 (83.2%) of women who reported at least one vaginal examination also reported that they did not provide consent, and a significant proportion 152 (34 · 9%) reported that vaginal examinations were not conducted privately. A cross-sectional study conducted in four African countries with labour observations and community-based surveys reported that among women with at least one observed vaginal examination, at their first vaginal examination 847 (59 · 0%) did not provide consent, whereas 2611 (59 · 4%) vaginal examinations were done without consent across all women [Citation48]. Best practice is that providers respect the privacy and confidentiality of every childbearing woman during counseling, physical examinations, and clinical procedures, as well as in the handling of patients’ medical records and other personal information. However, two-thirds of women who participated in this study had experienced a breach in confidentiality. Studies from other parts of the country have similarly revealed a high level of non-confidential care; common examples include the lack of privacy curtains and women not being appropriately covered during intimate examinations and/or labor and birth [Citation22,Citation24,Citation32].
Every woman is a person of value and is worthy of respect. All words, actions, and non-verbal communication of providers must honor the dignity of each woman. Unfortunately, in this study, 29% of women reported non-dignified care. Previous studies have documented similar result elsewhere in Ethiopia [Citation22,Citation24,Citation32,Citation34]. Likewise, Firew at al. found non-dignified care in agreement with these findings that 31.4% were shouted at, 13.7% experienced threat of withholding treatment and 17.2% were blamed or intimidated [Citation26]. Non-dignified care and insults may drive women away from healthcare facilities towards less trained providers who treat them with dignity and respect [Citation46]. Service providers must acknowledge that women have the right to be treated with respect and consideration. In this study, however, a number of women reported negative comments regarding their HIV seropositive status, age and literacy were 11.7%, 8.5% and 5.1%, respectively.
Attentive care is the right of each client and a woman should never feel abandoned during labour or immediately after birth. However, our study demonstrated that 40% of participating women felt ignored/abandoned and 12.9% of women reported healthcare providers were not present when the baby was born. This finding is in line with a study conducted in the southwest of Ethiopia [Citation32]. Furthermore, women should be able to have a birth companion of their choice. However, more than half of the women in this study reported that this was disallowed. The mere presence of a birth companion can ensure respectful care [Citation49], whereas restricting the presence of a birth companion is reported to be a significant barrier to humanized birth care [Citation26,Citation50,Citation51]. This suggests that healthcare providers know the way they behave in the absence of a companion is inappropriate and treat a client differently when a companion of the client is present [Citation52].
Freedom from detention is the right of each childbearing woman and a woman or her baby or her companion should never be forcibly kept in a facility. Detention is the least-reported category by participants, and this is similar to rates reported in other studies from Ethiopia [Citation22,Citation24,Citation26,Citation30,Citation32–34] possibly because maternity services are free of charge in Ethiopia and detention due to unaffordable service bills are rare. The economic status of women has been identified as a significant barrier to quality care. Unlike financially secure families, poor women are more likely to experience disrespectful birthing care [Citation53]. Similarly, women of low economic status were more likely to experience D&A in the current research. This indicates the prevailing social attitudes towards people from lower socioeconomic backgrounds. Studies from different contexts have also revealed likewise [Citation26,Citation54].
Women who gave birth at hospitals reported higher level of D&A compared to those who gave birth at health centers. Hospitals generally belong to the secondary and tertiary levels in Ethiopian three-tier healthcare system. They serve as referral sites for health centers, which are primary level. Many women prefer hospitals over health centers as they are higher-level and are expected to give better medical care [Citation27]. Increased client volume and insufficient staffing may impede the provision of respectful maternity care in hospitals [Citation55]. Previous studies have identified that working in under-equipped and overwrought health systems affects provider enthusiasm and is often labelled as significant contributor to D&A in facilities [Citation56]. Local studies have similarly reported higher incidence of D&A among women who gave birth at hospitals [Citation22,Citation25,Citation26,Citation31,Citation33].
Another predictor for experience of D&A was type of professional who attended the birth. Some professions were reported to disrespect and abuse women than the others. Women who were attended by midwives/nurses were more likely to experience disrespect and abuse compared to those who were attended by doctors. A study from Nigeria revealed that midwives found more of the presented scenarios of mistreatment to be acceptable practices, compared to doctors [Citation14]. Middle and lower level care providers, midwives/nurses, work the entire shift, whereas higher level (doctors) are mostly called to the labor ward to handle complications or cesarean delivery. Attending to the highly eventful and sensitive process of labor and delivery for long hours in poor working conditions may lead to providers burnout [Citation57] and increase their likelihood of inappropriate treatment of mothers. Negative attitudes of providers towards women is attributed in part to being overworked [Citation58]. Evidence shows that if lower level providers are the victims of D&A by managers or higher level providers, then it is more likely that they will use D&A as a tool to ascertain power [Citation59].
Female care providers are presumed to treat women better. Unexpectedly, women who were attended by female providers had a greater likelihood of experiencing D&A in this study. Similar findings have been indicated in a study from Mozambique where higher odds of D&A were reported among women attended by female care providers [Citation60]. On the other hand, rural residence was associated with increased likelihood of experiencing D&A. Similarly, in study from Mozambique, the occurrence of disrespect and abuse was much higher in the district hospitals compared to the central hospital [Citation60].
Limitation of the study
Only women who had given birth at a health facility were included. This possibly excluded women who might have chosen not to visit the health facility due to previous experiences of D&A.
Conclusion
The level of disrespect and abuse reported by participants is high. The drivers and enablers include both structural and interpersonal factors. Hospital birth showed consistent association with all forms of disrespect and abuse. Expanding the size and skill mix of professionals in the hospitals, sensitizing providers and health managers regarding the magnitude and consequences of D&A could decrease the workload and possibly promote more dignified and respectful maternity care, respectively.
Ethics approval and consent to participate
Ethical approval was obtained from The University of Adelaide human research ethics committee H-2019-153 and Salale University College of health sciences research ethics review committee A/G/H/S/C/768/11. Women meeting the eligibility criteria were provided with information about the study and those who agreed to participate consented and were enrolled. All women provided written consent. Participants were provided contact details of the study coordinator for any questions or concerns. To reduce the possibility of emotional distress due to describing past sensitive painful experiences, participants chose a convenient time and environment for the survey. In addition, they were accompanied by the person of their choice during the survey. No personal identifiers were used in the analysis to ensure anonymity.
Paper context
Disrespect and abuse of women during facility-based childbirth includes the way care providers act, behave or treat childbearing women and is against the basic human right of childbearing women. There are seven categories of disrespect and abuse and each category has its own verification criteria. No study known to the authors has been done on this issue in the study area so far. The authors surveyed mothers who had given birth at health facility to share their experience. The level of disrespect and abuse reported is high compared to previous studies.
Acknowledgments
We would like to express our gratitude to the women who participated in this study. We are sincerely grateful to the dedicated data collectors, without their tireless efforts, this project would not have been possible.
Additional information
Funding
Notes on contributors
Yohannes Mehretie Adinew
YMA conceived the proposal and collected and analyzed the data and wrote the manuscript. HH, AM and JK approved the proposal with some revisions, reviewed subsequent drafts of the manuscript for their scientific content. All authors read and approved the final manuscript.
References
- Exavery A, Kanté AM, Njozi M, et al. Access to institutional delivery care and reasons for home delivery in three districts of Tanzania. Int J Equity Health. 2014;13:48.
- Alkema L, Chou D, Hogan D, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet. 2016;387:462–10.
- Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva: World Health Organization; 2019.
- Fikre AA, Demissie M. Prevalence of institutional delivery and associated factors in Dodota Woreda (district), Oromia regional state, Ethiopia. Reprod Health. 2012;9:33.
- Amano A, Gebeyehu A, Birhanu Z. Institutional delivery service utilization in Munisa Woreda, South East Ethiopia: a community based cross-sectional study. BMC Pregnancy Childbirth. 2012;12:105.
- Callister LC, Edwards JE. Sustainable Development Goals and the ongoing process of reducing maternal mortality. J Obstet Gynecol Neonatal Nurs. 2017;46:e56–e64. .
- Harvey SA, Ayabaca P, Bucagu M, et al. Skilled birth attendant competence: an initial assessment in four countries, and implications for the Safe Motherhood movement. Int J Gynecol Obstet. 2004;87:203–210.
- Koblinsky MA, Campbell O, Heichelheim J. Organizing delivery care: what works for safe motherhood? Bull World Health Organ. 1999;77:399.
- Central Statistical Agency, ICF. ETHIOPIA demographic and health survey 2016.
- Organization WH. Strategies towards ending preventable maternal mortality (EPMM). 2015.
- Sheferaw ED, Mengesha TZ, Wase SB. Development of a tool to measure women’s perception of respectful maternity care in public health facilities. BMC Pregnancy Childbirth. 2016;16:67.
- Miller S, Lalonde A. The global epidemic of abuse and disrespect during childbirth: history, evidence, interventions, and FIGO’s mother− baby friendly birthing facilities initiative. Int J Gynecol Obstet. 2015;131:S49–S52.
- Bohren MA, Vogel JP, Hunter EC, et al. The mistreatment of women during childbirth in health facilities globally: a mixed-methods systematic review. PLoS Med. 2015;12:e1001847.
- Bohren MA, Vogel JP, Tunçalp Ö, et al. Mistreatment of women during childbirth in Abuja, Nigeria: a qualitative study on perceptions and experiences of women and healthcare providers. Reprod Health. 2017;14:9.
- Center for Reproductive Rights and Federation of Women Lawyers–Kenya. Failure to Deliver, Violations of Women’s Human Rights in Kenyan Health Facilities. 120 Wall Street, 14th Floor New York, NY 10005 USA: Center for Reproductive Rights; 2007.
- White Ribbon Alliance. Respectful maternity care: the universal rights of women and newborns. One Thomas Circle NW, Suite 200 Washington, DC 20005: 2019.
- UN GA. Universal declaration of human rights. UN General Assembly; 1948.
- UN GA. Declaration on the elimination of violence against women. UN General Assembly; 1993.
- Ga UN. International covenant on economic, social and cultural rights. United Nations Treaty Ser. 1966;993:3.
- UN GA. Convention on the elimination of all forms of discrimination against women. cited Apr. 1979;20:2006.
- Pillay N. Maternal mortality and morbidity: a human rights imperative. Lancet. 2013;381:1159–1160.
- Asefa A, Bekele D. Status of respectful and non-abusive care during facility-based childbirth in a hospital and health centers in Addis Ababa, Ethiopia. Reprod Health. 2015;12:33.
- Asefa A, Bekele D, Morgan A, et al. Service providers’ experiences of disrespectful and abusive behavior towards women during facility based childbirth in Addis Ababa, Ethiopia. Reprod Health. 2018;15:4.
- Banks KP, Karim AM, Ratcliffe HL, et al. Jeopardizing quality at the frontline of healthcare: prevalence and risk factors for disrespect and abuse during facility-based childbirth in Ethiopia. Health Policy Plan. 2018;33:317–327.
- Bekele W, Bayou NB, Garedew MG. Magnitude of disrespectful and abusive care among women during facility-based childbirth in Shambu town, Horro Guduru Wollega zone, Ethopia. Midwifery. 2020;83:102629.
- Bobo FT, Kasaye HK, Belachew Etana MW, et al. Disrespect and abuse during childbirth in Western Ethiopia: should women continue to tolerate? PloS One. 2019;14:6.
- Garedew M, Kerie M, Walle A. Choice of healthcare providing facility and associated factors among government employees in Nekemte Town, Western Part of Ethiopia. Health Syst Policy Res. 2019;6:83.
- Gebremichael MW, Worku A, Medhanyie AA, et al. Mothers’ experience of disrespect and abuse during maternity care in northern Ethiopia. Glob Health Action. 2018;11:1465215.
- Mihret MS. Obstetric violence and its associated factors among postnatal women in a Specialized Comprehensive Hospital, Amhara Region, Northwest Ethiopia. BMC Res Notes. 2019;12:600.
- Sheferaw ED, Bazant E, Gibson H, et al. Respectful maternity care in Ethiopian public health facilities. Reprod Health. 2017;14:60.
- Sheferaw ED, Kim Y-M, Van Den Akker T, et al. Mistreatment of women in public health facilities of Ethiopia. Reprod Health. 2019;16:130.
- Siraj A, Teka W, Hebo H. Prevalence of disrespect and abuse during facility based child birth and associated factors, Jimma University Medical Center, Southwest Ethiopia. BMC Pregnancy Childbirth. 2019;19:185.
- Ukke GG, Gurara MK, Boynito WG. Disrespect and abuse of women during childbirth in public health facilities in Arba Minch town, south Ethiopia–a cross-sectional study. PloS One. 2019;14:e0205545.
- Wassihun B, Deribe L, Worede N, et al. Prevalence of disrespect and abuse of women during child birth and associated factors in Bahir Dar town, Ethiopia. Epidemiol Health. 2018;40:e2018029.
- Mengesha MB, Desta AG, Maeruf H, et al. Disrespect and abuse during childbirth in Ethiopia: a systematic review. Biomed Res Int. 2020;2020:1–14.
- CSA. Summary and statistical report of 2007 population and housing censes. Federal Democratic Republic of Ethiopia Census Commission. Addis Abeba: Central Statistics Authority; 2007.
- Liu A, Sullivan S, Khan M, et al. Community health workers in global health: scale and scalability. Mount Sinai J Med. 2011;78:419–435.
- Dynes M, Buffington ST, Carpenter M, et al. Strengthening maternal and newborn health in rural Ethiopia: early results from frontline health worker community maternal and newborn health training. Midwifery. 2013;29:251–259.
- MOH E. Federal democratic republic of Ethiopia Ministry of health health sector development program IV October 2010 contents. cited Oct 2010. 2014.
- Bohren MA, Vogel JP, Fawole B, et al. Methodological development of tools to measure how women are treated during facility-based childbirth in four countries: labor observation and community survey. BMC Med Res Methodol. 2018;18:1–15.
- Bowser D, Hill K. Exploring evidence for disrespect and abuse in facility-based childbirth. Boston: USAID-TRAction Project, Harvard School of Public Health; 2010.
- Sando D, Abuya T, Asefa A, et al. Methods used in prevalence studies of disrespect and abuse during facility based childbirth: lessons learned. Reprod Health. 2017;14:127.
- WHO. The prevention and elimination of disrespect and abuse during facility based childbirth: WHO statement. 134588/1/WHO_RHR_14.23_eng.pdf. 2015 cited 2019 Feb 25. Available from: http://apps.who.int/iris/bitstream/10665/
- Molla M, Muleta M, Betemariam W, et al. Disrespect and abuse during pregnancy, labour and childbirth: a qualitative study from four primary healthcare centres of Amhara and Southern Nations Nationalities and People’s Regional States, Ethiopia. Ethiop J Health Dev. 2017;31:129–137.
- Gebremichael MW, Worku A, Medhanyie AA, et al. Women suffer more from disrespectful and abusive care than from the labour pain itself: a qualitative study from Women’s perspective. BMC Pregnancy Childbirth. 2018;18:392.
- Okafor II, Ugwu EO, Obi SN. Disrespect and abuse during facility‐based childbirth in a low‐income country. Int J Gynecol Obstet. 2015;128:110–113.
- Jansen L, Gibson M, Bowles BC, et al. First do no harm: interventions during childbirth. J Perinat Educ. 2013;22:83–92.
- Bohren MA, Mehrtash H, Fawole B, et al. How women are treated during facility-based childbirth in four countries: a cross-sectional study with labour observations and community-based surveys. Lancet. 2019;394:1750–1763.
- Hales DR, Johnson TR. Intensive Caring: new Hope for High-risk Pregnancy. New York, NY: Three Rivers Press; 1990.
- Behruzi R, Hatem M, Fraser W, et al. Facilitators and barriers in the humanization of childbirth practice in Japan. BMC Pregnancy Childbirth. 2010;10:25.
- Behruzi R, Hatem M, Goulet L, et al. The facilitating factors and barriers encountered in the adoption of a humanized birth care approach in a highly specialized university affiliated hospital. BMC Women’s Health. 2011;11:53.
- Abuya T, Warren CE, Miller N, et al. Exploring the prevalence of disrespect and abuse during childbirth in Kenya. PloS One. 2015;10:4.
- Adinew YM, Assefa NA. Experience of Facility Based Childbirth in Rural Ethiopia: an Exploratory Study of Women’s Perspective. J Pregnancy. 2017;2017.
- Bayo P, Belaid L, Tahir EO, et al. “Midwives do not appreciate pregnant women who come to the maternity with torn and dirty clothing”: institutional delivery and postnatal care in Torit County, South Sudan: a mixed method study. BMC Pregnancy Childbirth. 2020;20:1–14.
- Freedman LP, Kruk ME. Disrespect and abuse of women in childbirth: challenging the global quality and accountability agendas. Lancet. 2014;384:e42–e44.
- CRR W. Broken Promises: human Rights, Accountability, And Maternal Death in Nigeria. Center for Reproductive Rights/Women Advocates Research and Documentation Centre, USA; 2008.
- Ruotsalainen JH, Verbeek JH, Mariné A, et al. Preventing occupational stress in healthcare workers. Cochrane Database Syst Rev. 2014;13(11).
- Semachew A, Belachew T, Tesfaye T, et al. Predictors of job satisfaction among nurses working in Ethiopian public hospitals, 2014: institution-based cross-sectional study. Hum Resour Health. 2017;15:31.
- Mumtaz Z, Salway S, Waseem M, et al. Gender-based barriers to primary health care provision in Pakistan: the experience of female providers. Health Policy Plan. 2003;18:261–269.
- Galle A, Manaharlal H, Cumbane E, et al. Disrespect and abuse during facility-based childbirth in southern Mozambique: a cross-sectional study. BMC Pregnancy Childbirth. 2019;19:369.