ABSTRACT
Background
Chronic disease multimorbidity has become a major challenge for health systems. While a lot of research has evaluated the direct economic burden of multimorbidity on health care utilization and cost, little attention has been given to the impacts on work productivity and functional limitations, as indirect indicators of disease burden.
Objectives
This study aims to examine the prevalence of multimorbidity among Chinese adults and its impact on functional disability and work productivity. It also investigates urban-rural differences in these relationships.
Method
This study utilized the data from the China Health and Retirement Longitudinal Study (CHARLS) in 2015, including 11,176 participants aged 45 years and older. Multivariable logistic regression models were used to estimate the effect of multimorbidity on functional disability (i.e. ADL: activities of daily life; IADL: instrumental activities of daily life), and work productivity loss due to health problems. Negative binomial regression models were used to assess the association of multimorbidity with sickness absences from agricultural work and employed non-agricultural work.
Results
68.8% of total participants in CHARLS had multimorbidity in China in 2015. Rural residents with multimorbidity reported higher proportions of physical functions and days of sick leave than urban residents. Multimorbidity was positively associated with ADL limitation (odds ratio 1.924, 95% CI 1.656–2.236), IADL limitation (1.522, 1.326–1.748), limited work due to health problems (1.868, 1.601–2.178) and days of sick leave (for agricultural work, incidence rate ratio 1.676, 95% CI 1.390–2.020; for employed non-agricultural work, 2.418, 1.245–4.696). For the rural group, the impact of multimorbidity on functional limitations and work productivity loss (except for early retirement), was less than the urban group.
Conclusions
Multimorbidity poses significant challenges for functional health and work productivity These have significant negative economic consequences for individuals, the Chinese health system and the society.
Responsible Editor
Jennifer Stewart Williams
Background
Chronic diseases are a leading cause of global morbidity and mortality, with over 80% of chronic non-communicable disease (NCD) mortality occurring in low-and middle-income countries (LMICs), such as China [Citation1,Citation2]. The ageing population, coupled with the increasing prevalence of NCD risk factors, have led to a rise in the prevalence of multimorbidity. Multimorbidity is defined as an individual with two or more co-existing physical or mental health conditions. Recent studies in China have found that even though the overall prevalence of multimorbidity is estimated to be 61% in Chinese adults, the prevalence of multimorbidity is even higher (71%)for those aged 75 years and above [Citation3,Citation4]. With the rapidly increasing age of the Chinese population and the increasing levels of multimorbidity, it is imperative to understand the impacts of multimorbidity on individuals’ daily life and the broader society as this is crucial for diminishing the burden of chronic diseases in China.
An important impact of the individual burden of disease is the decline in individuals’ functional capacities in activities of daily life. Additionally, there is the direct economic burden of increased health care costs as well as the indirect economic burden that includes productivity loss at work. While health care utilization and the increased costs for people with multimorbidity in China and other countries have been widely evaluated [Citation5–12], little research has evaluated the impacts on the functional capacity and work productivity of Chinese adults and whether there are differences in these impacts between rural and urban populations in China. Although significant relationships between multimorbidity and increased difficulties in activities and instrumental activities of daily life have been observed in Chinese adults [Citation13–15], the indirect economic burden of multimorbidity related to productivity loss at work in China is still relatively unknown.
A few studies have investigated the impact of multimorbidity on work productivity in high-income countries, such as the USA, Netherlands, Australia, and Japan [Citation16–21]. Several outcomes related to work productivity have been assessed, including the incidence and duration of absenteeism, risk of long-term absenteeism (six or more consecutive weeks), unemployment (labor force participation), early retirement, presenteeism and critical incidents [Citation21]. But the conclusions and generalizability of these studies were limited by their small sample sizes and these studies have mostly been undertaken in high income countries, rather than in large and rapidly changing middle income countries like China [Citation19,Citation21]. In a study examining the association between physical conditions and non-agricultural work productivity loss among the middle-aged Chinese population, Pan and colleagues examined the association between mental-physical multimorbidity and disability, and work productivity [Citation13]. However, the urban-rural difference in relation to physical conditions and work productivity has not been investigated in the Chinese population [Citation13,Citation22].
It well known that there are great disparities in socioeconomic status, quality of life, and health services utilization between urban and rural residents in China [Citation23–26]. For example, elderly rural people are less likely to use inpatient services than those living in urban areas [Citation23]. Also, several previous studies have identified that residence (i.e. rural and urban) are important influential factors which are related to living with a disability [Citation27,Citation28]. Further, the difference in the prevalence of both single chronic diseases and multimorbidity has been observed between rural and urban populations [Citation29–31]. However, no study has investigated whether the associations between multimorbidity and functional limitations and productivity loss vary between rural and urban populations in China.
To address this knowledge gap, this study uses population-level and nationally-representative data from China, the most populous country and the second-largest economy in the world, in order to examine the rural-urban differences in associations between physical multimorbidity and functional limitations and work productivity loss among Chinese adults.
Methods
Data sources
This study used the second follow-up wave (2015) of data from the China Health and Retirement Longitudinal Study (CHARLS). The study collected high-quality data from a nationally representative sample of Chinese residents aged 45 and older, using multi-stage stratified probability-proportionate-to-size sampling. We used the second follow-up wave of CHARLS 2015 because it used objective measures including blood pressures, HbA1c, triglycerides, and total cholesterol, etc. Such measures are important and essential in order to be able to identify people with hypertension, diabetes and dyslipidemia more accurately and reliably than the most recent wave (2018) of CHARLS which only contained self-reported indicators.
The total sample size of the CHARLS baseline survey was 17,708 individual respondents. Ongoing follow-up surveys were conducted once every two or three years. A detailed description of the survey objectives and methods has been reported elsewhere [Citation32]. For this study, we identified 14,576 respondents without loss to follow-up. After removing respondents aged below 45 years and individuals with missing values of dependent or independent variables, our final sample had 11,176 respondents (76.7% of 14,576). Functional limitations were analysed using this entire sample, and sick leave days for employed non-agricultural work was analysed among the working-age population (5, 971 respondents) in China, defined as those who were aged below 55 years for females and 60 years for males.
Measures
In this study, multimorbidity was defined as the presence of two or more chronic conditions [Citation33,Citation34]. A total of 12 chronic diseases were used to measure physical multimorbidity, including hypertension, diabetes and dyslipidaemia which were measured based on biomarkers or blood test information, and 9 self-reported diagnosed chronic diseases (heart disease, stroke, cancer, chronic lung disease, digestive disease, liver disease, kidney disease, arthritis, and asthma). We counted the number of chronic diseases for each participant to identify those with multimorbidity.
In CHARLS, each respondent’s systolic blood pressure (SBP) and diastolic blood pressure (DBP) were recorded three times by a trained nurse using a HEM-7112 electronic monitor (Omron, Kyoto, Japan). The mean values for each respondent were then calculated but only given to the respondents once the interviews had ended. Diagnosed hypertension was defined as SBP ≥140 mmHg and/or DBP ≥90 mmHg by calculating the three mean readings, and/or being on antihypertensive medication for raised blood pressure [Citation35,Citation36]. In this study, diabetes was defined by 1) a fasting plasma glucose level of ≥126 mg/dL (7.0 mmol/L); and/or 2) HbA1c concentration of ≥6.5%; and/or 3) being insulin treatment and/or taking medication for raised blood sugar [Citation37,Citation38]. Dyslipidaemia was defined by 1) total cholesterol (TC) ≥ 240 mg/dL (6.22 mmol/L); and/or 2) low-density lipoprotein cholesterol (LDL-C) ≥ 160 mg/dL (4.14 mmol/L); and/or 2) high-density lipoprotein cholesterol (HDL-C) <40 mg/dL (1.04 mmol/L); and/or 2) triglyceride (TG) ≥ 200 mg/dL (2.26 mmol/L); and/or 2) taking anti-dyslipidaemia medication [Citation39,Citation40].
For primary outcomes of interest, the activities of daily living (ADL) and the instrumental activities of daily living (IADL) were used to evaluate the functional limitation [Citation41–43]. The ADL limitation referred to the difficulty in bathing, dressing, feeding oneself, using the toilet, getting in or out of bed, and controlling urination and defecation. The IADL limitation referred to the difficulty in doing household chores, cooking, shopping, making telephone calls, taking medications, and managing finances. For both ADL and IADL, answers were categorized as: ‘can do it by myself’, ‘have some difficulties’, ‘need help’ and ‘cannot do it’. Binary variables were constructed, so ADL/ IADL disability was defined as having difficulty in one or more ADL/IADL items. For the multivariable regression analysis, we used binary variables for no difficulty, and one or more difficulties.
The second outcome measure, work productivity loss, had four variables: (1) limited work due to health problems, which was a binary variable and was derived from the question ‘Are you unable to do some kind of work or cannot do that work for a long time because of a disability or health reasons?’; (2) early retirement, which was a binary variable and was derived from the question ‘Have you completed retirement procedures including early retirement and/or internal retirement?’; (3) number of days missed due to sick leave at agricultural work and (4) sick leave of employee’s primary non-agricultural work (including self-employed work), which was calculated based on the questions ‘How many days of work did you miss last year due to a health problem’ [Citation32].
Covariates included age, gender, marital status (married and partnered, unmarried and others), level of education (illiterate, primary school, secondary school, college and above), place of residence (rural, urban), household economic status quartiles (yearly per capita household consumption expenditure), social health insurance (yes, no) and geographical region (east, central, west). The Central and West referred to more deprived regions than the East with a high level of economic development in China.
Statistical analysis
We summarised the characteristics of all samples and the prevalence of multimorbidity. Means, proportion and 95% confidence intervals (CIs) for functional limitations and work productivity loss were calculated separately for individuals with different numbers of diseases (zero, one, two and above). Multivariable logistic regression models were performed to examine the impact of multimorbidity on functional limitations, limited work due to health problems, and early retirement. Negative binomial regression models were used to assess the association of multimorbidity with the number of days of sick leave at agricultural work and employed non-agricultural work. Moreover, we investigated the urban-rural differences in the relationship between multimorbidity and these outcomes. For the logistic regression analyses, the adjusted odds ratio (OR) and 95% confidence intervals (CIs) were reported. For the negative binomial regression analysis, we reported the incidence rate ratio (IRR) and 95% CIs.
We also performed sensitivity analyses to examine the association of the number of chronic diseases with functional health and work productivity loss using zero disease as a reference group (Appendix table S1, table S2 and table S3). Multivariable regressions also further adjusted for the Body Mass Index (BMI) [≥18.5 to <25.0, <18.5, ≥25.0 to <30.0, ≥30.0], depressive symptoms (no, yes), physical activity (low level, moderate level, high level). All descriptive analyses and regression results were weighted to account for the complex, multi-stage design, and non-response in the CHARLS data. All statistical analyses were conducted using Stata software 15.0 (Stata Corp., College Station, Texas). P values less than 0.05 were considered statistically significant.
Results
We analysed data from 11,167 respondents from CHARLS 2015. shows sample characteristics and the prevalence of single disease and multimorbidity across demographic groups. The mean age of respondents was 60.6 years. 43.2% of the respondents were illiterate, 63.3% resided in rural areas and 85.1% had social health insurance. A high prevalence of 68.8% had multimorbidity, which ranged from 62.0% in those aged 45–54 years, and 75.3% for those aged ≥ 75 years. The prevalence of multimorbidity was higher among individuals insured by social health insurance (77.4%) compared to people without health insurance (67.2%).
Table 1. Characteristics of participants by number of chronic diseases
Functional disability and productivity loss by the number of conditions and place of residence
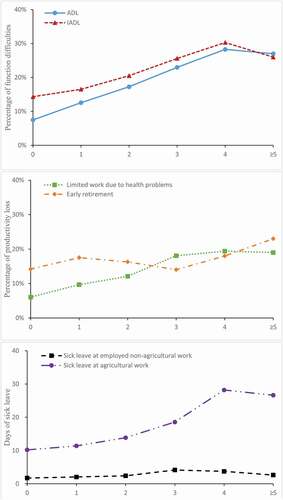
displayed the average proportion of subjects with ADL, IADL, limited work due to health problems, and early retirement (19.2%, 21.9%, 14.1% and 17.3%, respectively). The mean number of days of sick leave for agricultural work and employed non-agricultural works were 17.0 days and 2.5 days, respectively. The proportions of or mean of these outcomes increased as the number of conditions increased. Rural residents with multimorbidity reported higher proportions of physical functions and days of sick leave than urban residents.
Table 2. Functional limitations and productivity loss by number of chronic diseases and residence
The proportion of subjects with ADL limitation and IADL limitation rose as the number of NCDs increased from 0 to 4, but decreased slightly as the number of NCDs was 5 and above, which indicated a positive association of an increased number of co-morbidity and deteriorating physical and instrumental functions. Similarly, the proportion of limited work due to health problems, days of sick leave at agricultural work and employed non-agricultural work increased as the number of NCDs increased and then declined. Number of days of sick leave were greater in individuals at agricultural work than those having non-agricultural work. There was no linear association between multimorbidity and early retirement. ()
Association of multimorbidity with function difficulties and productivity loss
Compared with subjects with a single disease, patients with multimorbidity had a higher likelihood of ADL limitation (OR = 1.924, 95% CI = 1.656, 2.236) and IADL limitation (OR = 1.522, 95% CI = 1.326, 1.748). Meanwhile, participants aged 55 years and over were found to have greater odds of physical function limitations, compared to those aged below 55 years. Participants who were females, had lower education, from rural residences and deprived regions in China had greater odds of ADL and IADL. ()
Table 3. Association of functional limitations with multimorbidity and socio-demographic factors
showed the association between the number of chronic conditions and work productivity loss. Compared with individuals with a single disease, people with multimorbidity were more likely to be unable to do certain types of work or unable to do that type of work for a long time (limited work due to health problems: OR = 1.868, 95% CI = 1.601, 2.178). Subjects living in rural areas were more likely to be unable to do certain types of work or unable to do that type of work for a long time due to health problems (limited work due to health problems: OR = 1.715, 95% CI = 1.457, 2.018), compared to those in urban areas. Additionally, the education level and health insurance were risk factors of limited work due to health problems. Compared to those with a single disease, individuals with multimorbidity did not have significantly higher odds of having early retirement (P > 0.05).
Table 4. Association of work productivity loss with multimorbidity and socio-demographic factors
As shown in , after controlling covariates, compared to those with a single condition, individuals with multimorbidity had more days of sick leave at agricultural work (IRR = 1.676, 95% CI = 1.390, 2.020), and non-agricultural work (IRR = 2.418, 95% CI = 1.245, 4.696).
Table 5. Association of days of sick leave with multimorbidity and socio-demographic factors
Overall, the urban-rural differences in the association of multimorbidity with functional health and work productivity loss were comparable to the result of the whole regression analyses. Compared to the rural group, those in the urban group had a lower impact of multimorbidity on ADL limitation and IADL limitation. Moreover, except for the outcome on having early retirement, there were similar urban-rural differences in the relationships between multimorbidity and limited work due to health problems, as well as number of days of sick leave. ()
Sensitivity analysis
Compared with individuals in the zero-disease group, subjects with multimorbidity were at a higher likelihood of ADL limitation (OR = 3.283, 95% CI = 2.395, 4.498), IADL limitation (O = 1.714, 95% CI = 1.381, 2.126), and limited work due to health problems (OR = 2.955, 95% CI = 2.097, 4.165). Compared to those with a single disease, individuals with multiple chronic diseases did not have significantly higher odds of having early retirement. (Table S1 and Table S2) Individuals with multimorbidity compared to those people with zero disease are expected to have a 1.891 times more days of sick leave at agricultural work. (Table S3). After further adjusting for BMI, mental condition and physical activity in multivariable regression models, Table S4, Table S5 and Table S6 also showed consistent associations of multimorbidity with functional limitations and work productivity loss reported before.
Discussion
Summary of findings
Our findings demonstrate that there is a high prevalence of physical multimorbidity among middle-aged and elderly Chinese adults (68.8%), with the oldest age-groups having the greatest prevalence (75.3%). Multimorbidity has become a major health issue for the majority of Chinese adults and its prevalence increases with age.
Our findings also show that physical multimorbidity is associated with increased functional difficulties in daily life and instrumental daily life. This finding is consistent with our previous work in China [Citation14,Citation22], and research in USA [Citation44,Citation45], Japan [Citation46], and European countries [Citation47], where a higher number of chronic diseases were present for ADL and IADL difficulty. The decrease in physical functioning inevitably leads to an increased utilization of health services. This is then also associated with increasing health expenditure as well as an an increased burden on individuals, their families and the wider society [Citation33,Citation48,Citation49]. Quah and colleagues examined multimorbid older patients in Singapore and they highlighted the need for an enhanced model of primary care to address the quality of life and mental health demands [Citation50]. A strong primary care system needs to address multimorbidity. Universal health coverage for patients with multimorbidity has been proven to be cost-effective [Citation51,Citation52]. The improvement of patients’ self-efficacy and self-management under the guidance of primary care physicians, and the assessment and change of lifestyle behaviors is also proposed as an effective intervention in curbing the development of chronic conditions, while also maintaining physical functioning and emotional health [Citation53–55].
This study has also identified an association between physical multimorbidity and a higher number of sick-leave days at employed non-agricultural work as well as at agricultural work, with a greater effect on non-agricultural work. These findings are consistent with the small number of existing studies that have examined the association of multiple chronic diseases with a reduction in productivity in China [Citation14,Citation22], USA [Citation44,Citation45] and European countries [Citation47]. This could be due to social welfare for formally employed workers, such as social and endowment insurance, employee medical insurance or sick leave assistance, which are not available to those people engaged in agricultural production.
Importantly, this study suggests that there is less impact of multimorbidity on functional limitations and work productivity among rural participants, compared to those living in urban areas. This is because people in rural areas are relatively poorer than urban residents and may have no choice but to keep working due to limited economic means. The urban-rural differences were probably because of the greater proportion of functional difficulties and productivity loss among the single disease group in rural areas than urban areas (e.g. for ADL limitation, 15.8% vs 8.1%; for limited work due to health problem, 12.3% vs 6.1%). It indicates that the single disease could have a greater impact on functional health, limited work and sick leave to rural residents compared to urban citizens. These findings have implications for practice and policy, suggesting that prevention and self-management programs in rural areas should be targeted to decrease the incidence of any chronic disease, to delay high economic burden. Our results did not show an association between multimorbidity and early retirement which may be due to the lower age-group (45 to 60 years) of subjects that are not at retirement age yet.
Strengths and limitations
To our knowledge, this is the first study to examine the rural-urban differences in the relationship between physical multimorbidity and functional difficulties and work productivity loss in China. However, our study has some important limitations. First, the use of self-reported measures of chronic conditions may underestimate their prevalence, particularly for older persons and those from lower socio-economic and educational backgrounds who may be more likely to under-report. Second, previous systematic reviews found that in individuals without diabetes mellitus, HbA1c values are higher in Asians and Latinos when compared to persons with a Caucasian background [Citation56]. Using the diagnostic criterion by the American Diabetes Association (HbA1c concentration of ≥6.5%) for diabetes could potentially cause bias, but this bias is also minimised because the current study used three different criteria for the diabetes diagnosis. Third, we examined the effect of multimorbidity on productivity loss by just counting the number of chronic diseases without accounting for the different clusters and severity of chronic diseases.Future research should also consider mental health problems because effects of the combination of physical and mental health conditions on work ability tend to be greater than physical health problems alone, Fourth, the presence of unobserved determinants (i.e. residual confounding) biases the estimation in this study, and the directional or causal relationship between multimorbidity and outcomes (i.e. functional impairment) could not established with the cross-sectional design [Citation57]. Finally, this study only included middle-aged and older populations in China, which may limit the generalizability of the study. The prevalence of multimorbidity and its impacts on cost in terms of productivity loss among younger populations, as well as prospective study designs, should be considered for future studies.
Policy implications
Our findings provide new evidence on the burden of functional disability and the growing productivity loss due to multimorbidity in China. Multimorbidity is costly, not only to individuals and households, but also for the wider society, which is a major unaddressed challenge to health systems in China and other LMICs. Concerted efforts are needed in China with the largest ageing population in the world. Healthcare systems need to shift from single-disease models to new financing and service delivery models to more effectively manage multimorbidity [Citation58]. A strong primary healthcare system, behaviour monitoring, and behavioural change counselling led by more generalist physicians (less over-specialization) working with multi-disciplinary teams, is essential for cost-effective management of multimorbidity [Citation24,Citation55,Citation59].
Preventive strategies for multimorbidity can have substantial returns on health benefits as well as work productivity gains. Transforming the workplace environment might be a great preventive strategy to incorporate. By utilising strategies that maintain and improve the ability to work and secure sustainable employability for employees with multiple chronic conditions, such as providing on-site counselling services and worksite exercise space, businesses can reduce the effects that employees’ health conditions have on their productivity [Citation60–62].
A few studies from other countries have suggested that comorbid mental-physical health problems have reportedly led to a significant increase in disability and productivity loss [Citation13,Citation20]. Such interactions between mental conditions and physical multimorbidity are indirectly consistent with evidence suggesting that comorbid mental disorders can complicate the management of and exacerbate the course of chronic physical conditions [Citation63]. Future research in China is needed to examine the joint effects of mental-physical health conditions on work impairment.
Also, public health interventions should be better designed to consider physical-mental multimorbidity and be targeted to enable individuals with multimorbidity to improve functional health, job well-being and reduce absence from work. Such interventions should also address rural-urban disparities by accounting for elevated risks associated with functional disabilities and reduced labour force participation among rural residents. Future research related to mental-physical multimorbidity is also needed to enable the development of interventions that can be applied to the wider community.
Conclusion
Chronic disease multimorbidity is common among middle-aged and elderly Chinese adults. Multimorbidity poses health challenges and adversely affects productivity, which has negative economic consequences for individuals, the health system, and the wider society in China. Strategies for better management and control of multimorbidity could potentially improve the functional health of those affected as well as lead to productivity gains in China.
Ethics and consent
The Biomedical Ethics Review Committee of Peking University approved the CHARLS study, and informed consent was obtained from all interviewees prior to data collection. The ethical approval number was IRB00001052–11,015.
Paper context
Previous research has evaluated the direct economic burden of multimorbidity on health care utilization and cost. This nationally representative population-based study provides new evidence on the greater burden of functional disability and growing productivity loss due to multimorbidity in China, which is higher in rural residents than urban residents. Healthcare systems need to shift from single-disease models to new financing and service delivery models to more effectively manage multimorbidity and also address rural-urban disparities.
Supplemental Material
Download MS Word (47.9 KB)Acknowledgments
We gratefully acknowledge the China Health and Retirement Longitudinal Study team for providing data and training in using the datasets. We are grateful to the students who participated in the survey for their cooperation. The authors thank all volunteers and staff involved in this research.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed here.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Additional information
Notes on contributors
Li He
YZ and XL contributed to study design and data interpretation. YZ wrote the first draft of the paper. LH, CH, BO, GS, TH and XL contributed to manuscript editing. All authors reviewed and had final approval of the submitted and published versions.
References
- Yang GP, Kong LMD, Zhao WMD, et al. Emergence of chronic non-communicable diseases in China. Lancet. 2008;372:1697–12.
- Wang L, Kong L, Wu F, et al. Preventing chronic diseases in China. Lancet. 2005;366:1821–1824.
- Zhao Y, Zhang L, Zhao S, et al. Impact of multimorbidity on health service use and catastrophic health expenditure in China: an analysis of data from a nationwide longitudinal survey. The Lancet (British edition). 2019;394:S69–S69.
- Zhao Y, Atun R, Oldenburg B, et al. Physical multimorbidity, health service use, and catastrophic health expenditure by socioeconomic groups in China: an analysis of population-based panel data. Lancet Glob Health. 2020;8:e840–e849.
- Wang L, Si L, Cocker F, et al. A systematic review of cost-of-illness studies of multimorbidity. Appl Health Econ Health Policy. 2018;16:15–29.
- Sum G, Hone T, Atun R, et al. Multimorbidity and out-of-pocket expenditure on medicines: a systematic review. Eur J Public Health. 2017;27. DOI:https://doi.org/10.1093/eurpub/ckx187.233.
- Marthias T, Anindya K, Ng N, et al. Impact of non-communicable disease multimorbidity on health service use, catastrophic health expenditure and productivity loss in Indonesia: a population-based panel data analysis study. BMJ Open. 2021;11:e041870–e041870.
- Anindya K, Ng N, Atun R, et al. Effect of multimorbidity on utilisation and out-of-pocket expenditure in Indonesia: quantile regression analysis. BMC Health Serv Res. 2021;21:427.
- Zhao Y, Zhang P, Lee JT, et al. The prevalence of metabolic disease multimorbidity and its associations with spending and health outcomes in middle-aged and elderly chinese adults. Front Public Health. 2021;9:658706.
- Zhao Y, Atun R, Anindya K, et al. Medical costs and out-of-pocket expenditures associated with multimorbidity in China: quantile regression analysis. BMJ Glob Health. 2021;6:e004042.
- Chen H, Chen Y, Cui B. The association of multimorbidity with healthcare expenditure among the elderly patients in Beijing, China. Arch Gerontol Geriatr. 2018;79:32–38.
- Zhao Y, Zhang P, Oldenburg B, et al. The impact of mental and physical multimorbidity on healthcare utilization and health spending in China: a nationwide longitudinal population‐based study. Int J Geriatr Psychiatry. 2021;36:500–510.
- Pan T, Mercer SW, Zhao Y, et al. The association between mental-physical multimorbidity and disability, work productivity, and social participation in China: a panel data analysis. BMC Public Health. 2021;21:376.
- Su P, Ding H, Zhang W, et al. The association of multimorbidity and disability in a community-based sample of elderly aged 80 or older in Shanghai, China. BMC Geriatr. 2016;16:178.
- Zhao YW, Haregu TN, He L, et al. The effect of multimorbidity on functional limitations and depression amongst middle-aged and older population in China: a nationwide longitudinal study. Age Ageing. 2021;50:190–197.
- Meraya AM, Sambamoorthi U. Chronic condition combinations and productivity loss among employed nonelderly adults (18 to 64 Years). J Occup Environ Med. 2016;58:974–978.
- Ubalde López M, Arends I, Almansa J, et al. Beyond return to work: the effect of multimorbidity on work functioning trajectories after sick leave due to common mental disorders. J Occup Rehabil. 2017;27:210–217.
- Ishida M, Hulse ESG, Mahar RK, et al. The joint effect of physical multimorbidity and mental health conditions among adults in Australia. Prev Chronic Dis. 2020;17:E157–E157.
- Troelstra SA, Straker L, Harris M, et al. Multimorbidity is common among young workers and related to increased work absenteeism and presenteeism: results from the population-based Raine Study cohort. Scand J Work Environ Health. 2020;46:218–227.
- Sum G, Ishida M, Koh GC-H, et al. Implications of multimorbidity on healthcare utilisation and work productivity by socioeconomic groups: cross-sectional analyses of Australia and Japan. PloS One. 2020;15:e0232281–e0232281.
- Cabral GG, de Souza ACD, Barbosa IR, et al. Multimorbidity and its impact on workers: a review of longitudinal studies. Saf Health Work. 2019;10:393–399.
- Zhang W, Sun H, Li X. The association between chronic conditions and non-agricultural work productivity loss among the middle-aged Chinese population. J Occup Environ Med. 2018;60:832–838.
- Li Y, Chi I, Zhang K, et al. Comparison of health services use by Chinese urban and rural older adults in Yunnan province. Geriatr Gerontol Int. 2006;6:260–269.
- Ge D, Chu J, Zhou C, et al. Rural-urban difference in the use of annual physical examination among seniors in Shandong, China: a cross-sectional study. Int J Equity Health. 2017;16:86.
- Shi L. Health care in China: a rural-urban comparison after the socioeconomic reforms. Bull World Health Organ. 1993;71:723–736.
- You X, Zhang Y, Zeng J, et al. Disparity of the Chinese elderly’s health-related quality of life between urban and rural areas: a mediation analysis. BMJ Open. 2019;9:e024080–e024080.
- Chen N, Li X, Wang J, et al. Rural-urban differences in the association between disability and body mass index among the oldest-old in China. Arch Gerontol Geriatr. 2019;81:98–104.
- Liu M, Wang JH, Yang SS, et al. Evaluation of activities of daily living and related factors in community elderly people in urban and rural areas of Beijing. Zhonghua Liu Xing Bing Xue Za Zhi. 2018;39:268–272.
- Cheng C, Yang CY, Inder K, et al. Urban–rural differences in mental health among Chinese patients with multiple chronic conditions. Int J Ment Health Nurs. 2020;29:224–234.
- Yao -S-S, Cao G-Y, Han L, et al. Prevalence and patterns of multimorbidity in a nationally representative sample of older chinese: results from the china health and retirement longitudinal study. J Gerontol A Biol Sci Med Sci. 2020;75:1974–1980.
- Wang S, Kou C, Liu Y, et al. Rural–Urban differences in the prevalence of chronic disease in Northeast China. Asia Pac J Public Health. 2015;27:394–406.
- Yaohui Z, Yisong HU, Smith JP, et al. Cohort profile: the China health and retirement longitudinal study (CHARLS). Int J Epidemiol. 2014;43:61–68.
- Barnett KP, Mercer SWP, Norbury MM, et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380:37–43.
- Fortin M, Stewart M, Poitras M-E, et al. A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. Anna Family Med. 2012;10:142–151.
- Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34:2159–2219.
- Chobanian AV. National heart, lung, and blood institute joint national committee on prevention, detection, evaluation, and treatment of high blood pressure; national high blood pressure education program coordinating committee: the seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. Jama. 2003;289:2560–2572.
- American Diabetes A. 2. classification and diagnosis of diabetes: standards of medical care in diabetes-2019. Diabetes Care. 2019;42:S13–S28.
- Xu Y, Wang L, He J, et al. Prevalence and control of diabetes in Chinese adults. Jama. 2013;310:948–959.
- Zhang M, Deng Q, Wang L, et al. Prevalence of dyslipidemia and achievement of low-density lipoprotein cholesterol targets in Chinese adults: a nationally representative survey of 163,641 adults. Int J Cardiol. 2018;260:196–203.
- Hu D. Dyslipidemia and management of atherosclerotic cardiovascular diseases in China: new evidence and new guidelines. Cardiovasc Innovations Appl. 2017;2:143–145.
- Katz S, Ford AB, Moskowitz RW, et al. Studies of illness in the aged: the index of ADL: a standardized measure of biological and psychosocial function. jama. 1963;185:914–919.
- Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–186.
- Qian J, Ren X. Association between comorbid conditions and BADL/IADL disability in hypertension patients over age 45: based on the China health and retirement longitudinal study (CHARLS). Medicine (Baltimore). 2016;95:e4536–e4536.
- Bowling CB, Deng L, Sakhuja S, et al. Prevalence of activity limitations and association with multimorbidity among US adults 50 to 64 years old. J Gen Intern Med. 2019;34:2390–2396.
- Jindai K, Nielson CM, Vorderstrasse BA, et al. Multimorbidity and functional limitations among adults 65 or older, NHANES 2005-2012. Prev Chronic Dis. 2016;13:E151–E151.
- Jiao D, Watanabe K, Sawada Y, et al. Multimorbidity and functional limitation: the role of social relationships. Arch Gerontol Geriatr. 2021;92:104249.
- Singer L, Green M, Rowe F, et al. Trends in multimorbidity, complex multimorbidity and multiple functional limitations in the ageing population of England, 2002–2015. J Comorb. 2019;9:2235042–2235042X19872030.
- Wang HH, Wang JJ, Lawson KD, et al. Relationships of multimorbidity and income with hospital admissions in 3 health care systems. Anna Family Med. 2015;13:164–167.
- Van Merode T, Van De Ven K, Van Den Akker M. Patients with multimorbidity and their treatment burden in different daily life domains: a qualitative study in primary care in the netherlands and Belgium. J Comorb. 2018;8:9–15.
- Quah JHM, Wang P, Ng RRG, et al. Health‐related quality of life of older Asian patients with multimorbidity in primary care in a developed nation. Geriatr Gerontol Int. 2017;17:1429–1437.
- Smith SM, Soubhi H, Fortin M, et al. Managing patients with multimorbidity: systematic review of interventions in primary care and community settings. BMJ. 2012;345:809–e5205.
- Uijen AA, van de Lisdonk EH. Multimorbidity in primary care: prevalence and trend over the last 20 years. Eur J Gen Pract. 2008;14:28–32.
- Smith SM, Wallace E, O’Dowd T, et al. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev. 2016;2017:CD006560–CD006560.
- Wallace E, Salisbury C, Guthrie B, et al. Managing patients with multimorbidity in primary care. BMJ. 2015;350:h176–h176.
- Firth J, Siddiqi N, Koyanagi A, et al. The Lancet Psychiatry Commission: a blueprint for protecting physical health in people with mental illness. Lancet Psychiatry. 2019;6:675–712.
- Cavagnolli G, Pimentel AL, Freitas PAC, et al. Effect of ethnicity on HbA1c levels in individuals without diabetes: systematic review and meta-analysis. PLoS One. 2017;12:e0171315–e0171315.
- Calderon‐Larrañaga A, Vetrano DL, Ferrucci L, et al. Multimorbidity and functional impairment–bidirectional interplay, synergistic effects and common pathways. J Intern Med. 2019;285:255–271.
- Sturmberg JP, Bennett JM, Martin CM, et al. ‘Multimorbidity’ as the manifestation of network disturbances. J Eval Clin Pract. 2017;23:199–208.
- World Health Organization. Global status report on noncommunicable diseases 2014. Geneva: World Health Organization; 2014.
- Goetzel RZ, Henke RM, Tabrizi M, et al. Do workplace health promotion (wellness) programs work? J Occup Environ Med. 2014;56:927–934.
- Cancelliere C, Cassidy JD, Ammendolia C, et al. Are workplace health promotion programs effective at improving presenteeism in workers? A systematic review and best evidence synthesis of the literature. BMC Public Health. 2011;11:395.
- Mills PR, Kessler RC, Cooper J, et al. Impact of a health promotion program on employee health risks and work productivity. Am J Health Promot. 2007;22:45–53.
- Stoudemire A. Psychological factors affecting medical conditions. Washington DC: American Psychiatric Press; 1995.