ABSTRACT
To achieve universal health coverage, health system strengthening (HSS) is required to support the of delivery of high-quality care. The aim of the National Institute for Health Research Global Research Unit on HeAlth System StrEngThening in Sub-Saharan Africa (ASSET) is to address this need in a four-year programme, with three healthcare platforms involving eight work-packages. Key to effective health system strengthening (HSS) is the pre-implementation phase of research where efforts focus on applying participatory methods to embed the research programme within the existing health system. To conceptualise the approach, we provide an overview of the key methods applied across work-package to address this important phase of research conducted between 2017 and 2021.
Work-packages are being undertaken in publicly funded health systems in rural and urban areas in Ethiopia, Sierra Leone, South Africa, and Zimbabwe. Stakeholders including patients and their caregivers, community representatives, clinicians, managers, administrators, and policymakers are the main research participants.
In each work-package, initial activities engage stakeholders and build relationships to ensure co-production and ownership of HSSIs. A mixed-methods approach is then applied to understand and address determinants of high-quality care delivery. Methods such as situation analysis, cross-sectional surveys, interviews and focus group discussions are adopted to each work-package aim and context. At the end of the pre-implementation phase, findings are disseminated using focus group discussions and participatory Theory of Change workshops where stakeholders from each work package use findings to select HSSIs and develop a programme theory.
ASSET places a strong emphasis of the pre-implementation phase in order to provide an in-depth and systematic diagnosis of the existing heath system functioning, needs for strengthening and stakeholder engagement. This common approach will inform the design and evaluation of the HSSIs to increase effectiveness across work packages and contexts, to better understand what works, for whom, and how.
Responsible Editor
Jennifer Stewart Williams
Background
Substantial gains have been made in survival within low- and middle-income countries (LMICs), mainly through vertical programmes targeting infectious diseases including malaria, HIV and tuberculosis (TB), maternal, newborn and child conditions, and vaccine-preventable deaths [Citation1]. However, siloed approaches to care are inefficient and undermine the aspiration of integrated people-centred care [Citation2]. Furthermore, the epidemiological transition to greater disease burden from chronic and often multi-morbid disease, driven by increased life expectancy and globalisation of behaviours associated with unhealthy lifestyles, brings new challenges to the provision of high-quality care [Citation1]. The coronavirus disease 2019 (COVID-19) pandemic has intensified these issues, resulting in health systems being unable to cope with the increased service use [Citation3].
This accelerated demand and recently exposed fragility of health systems, presents challenges to the United Nations Sustainable Development Goals (SDGs). The need for Universal Health Coverage (UHC), with an implicit requirement for access to quality healthcare with financial risk protection has been amplified [Citation4,Citation5]. The 2017 Lancet Commission for High-Quality Health Systems, emphasises the requirement for resilient, high-quality health systems to meet the escalating demands, and to prevent against health crisis such as Ebola epidemic in west Africa [Citation6]. The Commission describes high-quality health systems as ‘consistently delivering care that improves or maintains health, being valued and trusted by all people and responding to changing population needs’.
Achieving UHC with high-quality care is an urgent priority for health systems strengthening (HSS) in LMICs, requiring the translation of knowledge (evidence-based care) into policy and routine practice (evidence-informed care) [Citation6,Citation7]. HSS involves comprehensive changes to policies and regulations, organisational structures, and relationships across the health system building blocks that motivate behaviour changes among providers and patients, allowing more effective use of resources to improve healthcare across the board [Citation8,Citation9]. Interventions for HSS, by their very nature, improve health outcomes by providing components that influence several mechanisms, both simultaneously and also at various time points and levels of the health system levels [Citation8].
Implementation research is a multidisciplinary approach to understand which interventions and implementation strategies work for whom, and how. This can be usefully applied to HSS by identifying and addressing barriers and opportunities to the delivery of high-quality care and testing potential solutions [Citation10]. Of particular importance is the pre-implementation phase of research that involves a careful assessment of context to understand and address barriers to the implementation of high-quality evidence-informed health care [Citation11]. This approach can be used to inform the development of a set of health system strengthening interventions (HSSIs) to deliver high-quality evidence-informed care, supporting the specific needs of a community and health system [Citation9].
The ASSET research programme
The National Health Institute of Research (NIHR) Global Research Unit on Health System Strengthening in sub-Saharan Africa (ASSET) is a four-year programme with a 10-month no-cost extension (2017–2022) that is closely aligned with the SDG goal of UHC, and the recommendations of the Lancet Commission for High-Quality Health Systems. ASSET is one of the first implementation research programmes for HSS that involves diverse care platforms, across different contexts, that also applies a common implementation science approach to the design and evaluation of HSSIs, thus allowing for comparability across settings and potential generalisability.
The aim of ASSET is to develop and evaluate effective and sustainable HSSIs, promoting consistent delivery of high-quality, people-centred care [Citation12]. ASSET is working on three healthcare platforms in Ethiopia, Sierra Leone, South Africa, and Zimbabwe: (1) primary care for the integrated treatment of chronic conditions in adults; (2) maternal and newborn care; and (3) surgical and dental care. Eight work packages (i.e. separate research studies with work package-specific aims and objectives) use a common approach to develop context-specific HSSIs that address locally relevant and platform-specific challenges, while bringing wider system benefits. Summaries of the care platforms and associated work packages can be found in .
Table 1. Description of the ASSET work packages for the different healthcare platforms
The ASSET programme is being conducted in two phases including the pre-implementation and piloting/rolling implementation phase. The pre-implementation phase that runs between 2017 to 2021, aims to map comprehensive care pathways of a patient’s journey through the health system including the community, different providers (e.g. private sector and non-governmental organisations), and health facilities, documenting what care is provided at what level of the health system and the associated health system bottlenecks. At the end of this phase, findings are fed back to stakeholders using focus group discussions and Participatory Theory of Change (ToC) workshops [Citation13,Citation14]. Stakeholders then select HSSIs and develop a programme theory. The second phase of ASSET that runs from March 2021 until January 2022 involves work packages initially piloting the set of selected HSSIs, making any necessary adaptations. This is followed by a rolling implementation phase that is an iterative process of testing, making necessary adaptations, then re-testing HSSIs. Quasi-experimental designs are used to test the effectiveness of the set of HSSIs on selected implementation and clinical outcomes and to identify factors that may influence the implementation of the proposed interventions. Integration of the interventions into routine care is being conducted in close collaboration with Ministry of Health partners in each site to support sustainability [Citation12].
ASSET requires an extensive pre-implementation phase. A combination of different methods are used to effectively account for gaps in the provision of high-quality healthcare. The importance of taking time to engage with stakeholders who are part of the public health system cannot be underestimated, as this helps to ensure their needs and priorities are addressed and a set of HSSIs are selected to address local barriers identified for people in need of care. Another factor shaping the pre-implementation phase, is the lack/absence of routinely available data that is of sufficient quality to provide insight into key issues that need addressing (i.e. disease burden, quality of care).
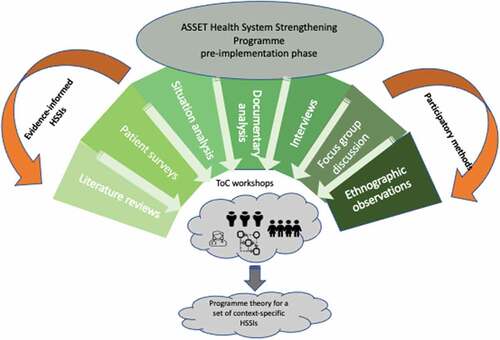
To conceptualise the pre-implementation phase of the work packages within the ASSET programme, we provide an overview of methods (). We then review how findings are used to inform the selection and adaptation of contextually relevant HSS intervention. We also describe the synthesis of work package activities to draw conclusions on the general requirements of the health system to deliver high-quality people-centred care in LMICs [Citation15]. To enable reproduction of individual work packages, protocols for the pre-implementation phase of ASSET are reported in Appendix 1.
The overall objectives for the pre-implementation phase (phase 1) of ASSET are:
To generate engagement and build relationships with stakeholders from the outset to ensure co-production and ownership of HSSIs that will survive the programme and help to generate both capacity building and sustainability.
To apply a mixed-methods approach (qualitative and quantitative) to evaluate the following for each of the work packages:
(I) Barriers to accessing care;
(II) Bottlenecks (critical shortage of a particular resource that results in care being blocked) in the care processes and pathways and associated outcomes;
(III) Quality of care (detection, diagnosis and treatment); and
(IV) People-centred care and its determinants.
(3) For each work package, the outputs from the different studies are used to inform the following:
(I) ToC workshops to develop a programme theory Illustrating how and why the package of HSSIs are hypothesised to deliver valued outcomes in practice [Citation16];
(II) A set of HSSIs to overcome the contextual determinants of problems identified for the different care pathways at the micro, meso and macro levels; and
(III) Selection and development of process, clinical and implementation outcome measures for the different HSSIs.
Methods
Study location
The eight work packages cover a range of demographic populations (i.e. with respect to age, gender, socioeconomic status, medical and social needs), located in rural, peri-urban and urban geographical settings [Citation12]. describes the different study sites and types of publicly funded health facilities for each work package.
Participants
The participants in the pre-implementation phase of ASSET are a combination of stakeholders, including patients and their caregivers, clinicians, managers, administrators and policy makers. ASSET also engages with important community/multi sectorial stakeholders such as non-governmental organisations and private healthcare providers.
Study designs used within the pre-implementation phase of ASSET
To ensure the pre-implementation phase of ASSET addresses the first objective of research including engagement with stakeholders to facilitate embedding the different work packages within the existing health system, the following mixed-methods are applied across the work packages: interviews with different stakeholders, focus group discussions, and Participatory Theory of Change workshops. Other methods are also applied including literature/scoping reviews; situation analyses; cross-sectional surveys involving patients identified in healthcare facilities; cohort studies in the communities involving patients who received surgical interventions in participating healthcare facilities; documentary analyses, ethnographic observations of provision of healthcare. , describes the objectives of for the different studies that are applied in the pre-implementation phase of ASSET.
Table 2. Study locations and relevant health facilities of each Work Package (WP)
Table 3. Rational/Objectives of pre-implementation phase studies
At the end of the pre-implementation phase, data from each work package is analysed and findings from the different studies are triangulated to help substantiate and add validity to the overall findings. This process illuminates where important differences and commonalities exist between different studies such as ethnographic observations and semi-structured interviews. Findings are then used to identify a set of HSSIs to overcome the contextual barriers at the micro, meso and macro levels identified for the different care pathways.
Details of the studies conducted within the pre-implementation phase of ASSET
Literature review (WPs 1-8)
Individual work package teams use literature reviews to establish HSSIs that are most effective to address the relevant public health issues in the local context. As an example, work package 4 is publishing a scoping review of tuberculosis and mental health disorders and person-centred care [Citation17]. Unpublished literature reviews are also used to inform ASSET’s cross-cutting requirements for health systems strengthening including the role of non-technical skills (e.g. clinical communication skills, leadership skills, quality improvement skills); integrated primary health care; people-centred care, and; mHealth.
Situation analyses (WPs 1-8)
According to the World Health Organization (WHO), a situation analysis is not only a collection of facts describing the epidemiology, demography and health system status of the population, but also a comprehensive assessment of the full range of current and potential future health issues and their determinants [Citation18]. A situation analysis therefore assesses the current disease burden and whether the health system is equipped to provide the associated high-quality care to treat the population needs.
Work packages 1–3, 6 and 7 conduct situation analyses of primary health facilities using an adapted version of the situation analysis tool developed by Programme for Improving Mental Health Care (PRIME) [Citation19]. The PRIME situation analysis tool was originally developed to appraise district and sub-district mental health systems and services in LMICs for primary care but has broader applicability to chronic care. The ASSET programme uses the adapted PRIME tool to assess publicly available information such as existing policies and guidelines and data to determine the location and nature of the gaps between what services intend to provide compared to what is achieved in practice. The tool is also used to identify some of the critical shortages (staff, skills, knowledge) that contribute to these gaps. Of particular relevance to ASSET is using the tool to assess the availability and quality of HMIS data [Citation19].
Work Packages 3 and 7 also use the Hospital Assessment Tool, developed by the Ethiopian Federal Ministry of Health in collaboration with the WHO and Programme in Global Surgery and Social Change, to assess secondary and tertiary care facilities for surgical care [Citation20,Citation21].
Cross-sectional patient questionnaires in health facilities (WPs 1, 2, 5, 6, 8)
Patients presenting at the different health facilities are recruited consecutively when they attend for care. Following consultation, work packages teams administer validated and bespoke questionnaires to patients who present at primary and secondary health facilities. The questionnaires are used to evaluate the local health systems context including demographic characteristics, epidemiology, and patient’s care pathways based on both local and national guidelines. The clinical notes are also reviewed to identify diagnoses and management plans that are compared to the research clinical measures from the questionnaires. Patients identified as having a condition of interest, are asked additional questions including about their awareness about self-management and their involvement in decision-making and care planning. This information is critical in order to establish the extent of the care gaps and to describe parameters that can influence local HSSI development.
Although in many instances similar questionnaires are used to measure the same outcome (i.e. PHQ-9) for different work packages, in some cases work packages use questionnaires with specific relevance to their local context. The assessment tools are described in . All scales are available from the corresponding author upon request.
Table 4. Data collection tools and instruments used in quantitative patient surveys
Community surveys for cohort study of surgical patients recruited in health care facilities in Ethiopia and Sierra Leone
Work packages that are a part of the surgical care platform, recruit patients who are identified in participating health facilities for follow-up assessment in the community post discharge. Patients are administered questionnaires to identify peri and post-operative infection rates, unmet need for care, disability, help-seeking behaviour, satisfaction with care, household economic impact of surgery, and healthcare satisfaction. Outcomes are linked to clinical processes documented for the associated hospital admission to understand gaps in care that can be addressed with the HSSIs. Unique to WP3 in Ethiopia, is the HSS for dental care. describes the specific surveys administered by each work package.
Documentary analyses (WPs 1-4, 7-8)
A documentary analysis is used to identify the extent and quality of clinical documentation, through review of clinical records, guidelines, policies, and Health Management Information Systems (HMIS). Clinical records are compared to policy guidelines using methods such as process mapping, checklists, observations of patient flow, review of HMIS data, and review of clinical records using proformas. Findings are used to assess for adherence to guideline-based care or evidence-based care. describes the relevant guidelines.
Table 5. Data sources and data collection instruments for documentary analysis
Ethnographic and structured observations of healthcare practices and context (WPs 1-4, 6)
ASSET applies both unstructured and structured ethnographic observations of clinician-patient encounters to complement quantitative methods. Unstructured observations are used extensively to understand quality of care and the broader context of patient interactions. Unstructured ethnographic observations are the best approach for exploring stigmatised conditions like TB, mental illness and domestic violence, that also captures the quality of clinician–patient interactions from a non-clinical perspective. In particular, these methods are useful for looking at issues like respect, compassion, and quality of listening. Communication of healthcare workers amongst themselves and with patients are observed to understand adherence to guideline-based care and the extent to which care is respectful and people-centred. Structured observation of clinician-patient encounters is conducted using observational checklists, including the enhancing assessment of common therapeutic factors (ENACT) rating scale for competence in elements of person-centred care [Citation60]. Checklists are also used to help to determine the extent to which clinicians are adhering to guideline-based care.
Semi-structured interviews and focus group discussions (WPs 1-8)
Qualitative semi-structured interviews and focus-group discussions are used by all work packages to triangulate findings with data from the quantitative surveys and observational data, and to explore perspectives of various stakeholders. Interviews are held with different groups of participants separately, allowing for frank expression of what people experience when probing around sensitive topics. Such an approach provides the human narrative component to complement the quantitative methods and understand trends in data. describes objectives, processes and participants for the interviews and group discussions.
Table 6. Summary of qualitative data collection methods and samples
Data analyses
A combination of mixed methods are used to analyse the data collected as part of the pre-implementation phase. Quantitative outcomes of interest are reported as means and proportions, accounting for clustering where appropriate. Mixed regression analysis accounting for clustering where appropriate, is used to identify determinants of quality of care (i.e. accurately detecting conditions), satisfaction with care, recovery, and risk factors for the condition in question.
Qualitative analyses use simple descriptive summaries for the outcomes of interest. Thematic framework analysis is used for in-depth interviews and focus group discussions. An inductive approach is used to analyse unstructured ethnographic observations.
Methods to inform the piloting and rolling evaluation phases of ASSET
Theory of change workshops to develop a programme theory
Findings from the pre-implementation phase of ASSET are shared with the stakeholders during ToC workshops in order to elicit their ideas and priorities for quality improvement. Findings which reflect negatively on quality of care provided within a service are conveyed in such a way so that they can be shared with staff to engage in quality improvement. Confidentiality is key to this process, as is the use of patient narratives (including patient quotes). This approach helps to engage staff in constructive ways conveying how they could work differently. This shifts the quality improvement process from a culture of inspection and punishment to one of true reflection and change.
In the pre-implementation phase of ASSET, work package teams oversee between one and three ToC workshops to develop an initial programme theory. In subsequent phases of the ASSET programme, work package teams use a series of ToC workshops to adapt and refine the initial programme theory as the implementation process progresses. The result is a final programme theory that articulates pathways to change, intermediate outcomes, clinical and implementation outcomes, and underlying assumptions including contextual barriers and enablers. Each work package team invites different cadres of stakeholders to relevant meetings and workshops. describes the ToC workshops used in each work package.
Table 7. ToC workshops conducted for each work package in the pre-implementation phase of ASSET
Implementation science methods
Implementation science theory-based determinant frameworks provide a systematic approach to the identification and description of contextual factors that are known to influence implementation outcomes, as well as key factors to consider in the design, implementation and evaluation of the HSSIs [Citation61]. Implementation science frameworks are applied to findings from the pre-implementation phase of ASSET to help interpret the results, identify commonalities and differences across platforms and countries and ultimately help identify how context at the micro, meso and macro levels may influence the implementation of evidence-informed care.
The implementation science element of the ASSET programme is reported in a separate protocol, due to its breadth and complexity, as the ASSET diagnostic phase gets underway. Ultimately, the implementation science component of ASSET helps to determine the following: (1) whether any additional health systems strengthening interventions are required, (2) finalise process indicators and outcomes of interest in the programme theory developed in the ToC workshops, and (3) inform the design of the piloting and evaluation phases in terms of contextual factors that may influence the effectiveness of the HSSIs in delivering evidence-based and people-centred care.
Patient public involvement
Patients and the public were not involved in the designing/writing protocol for pre-implementation phase of ASSET. However, extensive participatory methods that involve both the patients and public are used in this phase of research to design, select and evaluate the HSSIs for ASSET.
Ethical considerations
All work packages have received separate ethics approval from the Research Ethics Committee at Kings College London (KCL) as well as the relevant country institutional and local government ethics review committees. See Appendix 2 for details for the different work packages.
Discussion
HSS for universal health coverage with high-quality care requires the critical engagement with policy makers, researchers, service providers, and patients from the outset, to co-design interventions using high-quality, routinely available data that is responsive to the changing requirements of the users and health systems [Citation62]. However, the current approach to strengthen heath systems in LMICs, is failing to meet these demands and is demonstrated by vertical programmes and academic research initiatives having little impact on broader health systems [Citation62].
ASSET is a health system strengthening programme that involves the participatory design and evaluation of a set of contextually appropriate HSSIs across three healthcare platforms, within are eight work packages, in four countries in sub-Saharan Africa. Each work package addresses complex public health issues that are relevant to local requirements and contexts. Such a diverse programme requires a flexible approach to develop a set of HSSIs tailored to the local context.
This protocol describes how robust and extensive formative research methodologies are applied to identify limitations in the delivery of, and access to, quality care. A strong emphasis is placed on engagement of relevant stakeholders and embedding ASSET within the health systems from the onset, including people with health conditions, their carers, communities, clinicians and policy makers. It is anticipated that the use of participatory methods through group and individual consultations, and ToC workshops at various stages of the pre-implementation phase, helps to foster partnership and local ownership for the different interventions that are acceptable and feasible to implement, responding to the patient needs, that be sustained in the longer term. The COVID-19 pandemic demonstrates how ASSET has embedded itself within the health system whereby ministries have engaged with the different work packages to help manage the crisis.
A critical component of the pre-implementation work is mapping the care pathway into and through health services that allows the work we do to be people-centred, facilitating more compassionate conversations about how and why health systems fail people. We emphasise health systems as opposed to health providers because health systems are also failing people who provide the care, making it extraordinarily difficult to deliver care, let alone a respectful, people–centred approach. Mapping care pathways also helps to engage stakeholders, facilitating the co-production of HSSIs. Couching problems in systems language and using patient narratives to humanise them helps to ensure the health systems strengthening is inherently people-centred.
ASSET is also investing heavily in capacity building for HSS. Extensive training is provided in implementation science and other methodologies that invites a wide range of stakeholders both from the ASSET programme as well as the wider community. Training on the different methodologies for HSS not only ensures comparability of findings across different work packages and platforms with hopeful generalisability, but importantly increased capacity for research led HSSI within these countries.
The extensive process ASSET is undertaking in the pre-implementation phase, is in part due to the absence of high-quality data available in the HMIS that can be used to inform the requirements for HSS relevant to the local context. However, this process may have negative bearing on short-term outcomes as it puts delivery of the entire programme of work at risk where completed evaluations with follow-up of adequate duration to influence policy/ practice may not be delivered. Nevertheless, engaging in these activities is critical if HSS interventions seek to bring evidence-informed care to scale in a sustainable manner [Citation62].
At the end of the pre-implementation phase of ASSET, it is hoped the common approach taken across different countries, care platforms and health conditions will facilitate cross platform learning and understanding of how differences in health systems and broader contextual influences shaped the development of the interventions. The overarching expectation is that by using an in-depth participatory process to engage with the stakeholders and map care pathways to and through the health system, we develop a HSS programme that can be implemented at scale that meets the needs and priorities of the local community. Ultimately it is hoped that this approach will provide people–centred high-quality care that is resilient to the changing dynamic of an aging population that can also prevent future shocks like Ebola and COVID-19.
Authors contributions
NSeward wrote the first and subsequent drafts of the paper MP, CH and NSeward conceptualised the idea for the paper CH, and NSeward reviewed and edited all drafts of the paper MP offered overall guidance All other authors (CL, AAbulahi, ZA, AAlem, RA, MB, BB, NB, DC, RC, JD, AD, F, SF, JG, WG, RH, MK, AL, CL, KN, JM, IP, RP, JS, AT, GT, AR, NSevdalis, RV, CW) edited and offered input to various drafts of the paper
Data sharing statement
No additional data available as a protocol paper
Ethics approval
See appendix 2
Paper context
The need to design resilient health system strengthening interventions (HSSIs) to support high-quality care in sub-Saharan Africa is urgently required. We describe the protocol applied to the pre-implementation phase of a five-year research programme to strengthen health systems across four countries in sub-Saharan Africa. This work is providing the required evidence to develop HSSIs which are effective, sustainable and which promote consistent delivery of high-quality, people-centred care. The subsequent evaluation will involve comparison of HSSIs across diverse care platforms and contexts, facilitating concrete recommendations for wider generalisability to other LMICs on how to strengthen health systems to improve the quality of care.
Patient consent
Protocol paper so consent not applicable
Preprint
A preprint, also known as the Author’s Original Manuscript (AOM) is available online https://www.medrxiv.org/content/10.1101/2021.01.06.20248468v1 [doi: 10.1101/2021.01.06.20248468].
Supplemental Material
Download PDF (1.2 MB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed here.
Additional information
Funding
References
- Global Burden of Disease Mortality Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117–15.
- World Health Organisation. Framework on integrated, people-centred health services. 2016.
- Walker P, Whittaker C, Watson O, et al. The impact of COVID-19 and strategies for mitigation and suppression in low- and middle-income countries. Science. 2020;369:413–422.
- United Nations. Transforming our world: the 2030 Agenda for Sustainable Development. 2015 [cited 2019 Oct 17]. Available from: http://www.un.org/ga/search/view_doc.asp?symbol=A/RES/70/1&Lang=E
- World Bank Group WHO. Tracking universal health coverage: first global monitoring report. Washington DC Geneva: The World Bank Group; World Health Organization; 2015.
- Kruk M, Gage A, Arsenault C, et al. High-quality health systems in the sustainable development goals era: time for a revolution. Lancet Glob Health. 2018;6:e1196–e252.
- Al-Janabi A, Al-Wahdani B, Ammar W, et al. Bellagio declaration on high-quality health systems: from a quality moment to a quality movement. Lancet. 2018. DOI:10.1016/S2214-109X(18)30372-3.
- Savigny Don AT. Systems thinking for Health system strengthening. Geneva: Alliance for Health Policy and Systems Research, WHO; 2009.
- World Health Organization. Everybody business: strengthening health systems to improve health outcomes: WHO’s framework for action. Geneva: WHO; 2007.
- Peters DH, Adam T, Alonge O, et al. Implementation research: what it is and how to do it. BMJ. 2013;347. DOI:10.1136/bmj.f7086
- Peters DTN, Adam T. Implementation research in health: a practical guide. Alliance for Health Policy and Systems Research, World Health Organization; 2013.
- ASSET Health System StrEngThening in Sub Saharan Africa. [cited 2020 Dec 01]. Available from: https://healthasset.org/
- Weiss C. Nothing as practical as good theory: exploring theory-based evaluation for comprehensive community initiatives for children and families. In: Jp C, editor. New Approaches to evaluating community initiatives: concepts, methods, and contexts. Washington DC: Aspen Institute; 1995.
- Vogel I. Review of the use of theory of change in international development. UK: Department for International Development; 2012.
- Seward N, Hanlon C, Abdulahi A, et al. HeAlth System StrEngThening in four sub_Saharan African countries (ASSET) to achieve high-quality, evidence-informed surgical, maternal and newborn, and primary care: protocol for pre-implementation phase studies. medRxiv. 2021 Jan 06;20248468. DOI:10.1101/2021.01.06.20248468.
- Andersen A. A community builder’s approach to theory of change: a practical guide to theory development. New York: The Aspen Insitute; 2004.
- Janse Van Rensburg A, Dube A, Curran R, et al. Comorbidities between tuberculosis and common mental disorders: a scoping review of epidemiological patterns and person-centred care interventions from low-to-middle income and BRICS countries. Infect Dis Poverty. 2020;9:4.
- Rajan D. Situation analysis of the health sector. In: Schmets G, Rajan D, Kadandale S, editors. Strategizing national health in the 21st century: a handbook. Geneva: World Health Organization; 2016.
- Hanlon C, Luitel N, Kathree T, et al. Challenges and opportunities for implementing integrated mental health care: a district level situation analysis from five low- and middle-income countries. PLoS One. 2014;9:e88437.
- Iverson K, Ahearn O, Citron I, et al. Development of a surgical assessment tool for national policy monitoring & evaluation in Ethiopia: a quality improvement study. Int J Surg. 2020;80:231–240.
- Groen R, Samai M, Petroze R, et al. Pilot testing of a population-based surgical survey tool in Sierra Leone. World J Surg. 2012;36:771–774.
- Burney PG, Laitinen LA, Perdrizet S, et al. Validity and repeatability of the IUATLD (1984) Bronchial Symptoms Questionnaire: an international comparison. Eur Respir J. 1989;2:940–945.
- Martinez F, Raczek A, Seifer F, et al. Development and initial validation of a self-scored COPD Population Screener Questionnaire (COPD-PS). Copd. 2008;5:85–95.
- Garrod R, Bestall JC, Paul EA, et al. Development and validation of a standardized measure of activity of daily living in patients with severe COPD: the London Chest Activity of Daily Living scale (LCADL). Respir Med. 2000;94:589–596.
- Jones P, Harding G, Berry P, et al. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34:648–654.
- Harding R, Selman L, Agupio G, et al. Validation of a core outcome measure for palliative care in Africa: the APCA African Palliative Outcome Scale. Health Qual Life Outcomes. 2010;8:10.
- Abernethy A, Shelby-James T, Fazekas B, et al. The Australia-modified Karnofsky Performance Status (AKPS) scale: a revised scale for contemporary palliative care clinical practice [ISRCTN81117481]. BMC Palliative Care. 2005;4:7.
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613.
- Cox J, Chapman G, Murray D, et al. Validation of the Edinburgh postnatal depression scale (EPDS) in non-postnatal women. J Affect Disord. 1996;39:185–189.
- Spitzer R, Kroenke K, Williams JB, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Internal Med. 2006;166:1092–1097.
- Patel V, Simunyu E, Gwanzura F, et al. The shona symptom questionnaire: the development of an indigenous measure of common mental disorders in Harare. Acta Psychiatr Scand. 1997;95:469–475.
- WHO ASSIST Working Group. The alcohol, smoking and substance involvement screening test (ASSIST): development, reliability and feasibility. Addiction. 2002;97:1183–1194.
- Ustun TB, Kostanjesek N, Chatterji S, et al. World Health Organization. Measuring health and disability: manual for WHO disability assessment schedule (WHODAS 2.0). 2010.
- Radloff L. The CES-D scale: aself-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
- Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32:705–714.
- Zink T, Levin L, Putnam F, et al. Accuracy of five domestic violence screening questions with nongraphic language. Clin Pediatr (Phila). 2007;46:127–134.
- Mayston R, Habtamu K, Medhin G, et al. Developing a measure of mental health service satisfaction for use in low income countries: a mixed methods study. BMC Health Serv Res. 2017;17:183.
- Gray M, Litz BT, Hsu JL, et al. Psychometric properties of the life events checklist. Assessment. 2004;11:330–341.
- Blevins C, Weathers F, Witte T TD, et al. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress. 2015;28:489–498.
- Abrahams Z, Schneider M, Field S, et al. Validation of a brief mental health screening tool for pregnant women in a low socio-economic setting. BMC Psychol. 2019;7:77.
- Webster T, Mantopoulos J, Jackson E, et al. A brief questionnaire for assessing patient healthcare experiences in low-income settings. Int J Qual Health Care. 2011;23:258–268.
- Anderson G, Ilcisin L, Kayima P, et al. Out-of-pocket payment for surgery in Uganda: the rate of impoverishing and catastrophic expenditure at a government hospital. PLoS One. 2017;12:e0187293.
- World Health Organization. Oral Health Surveys: basic Methods. 5th ed. France: World Health Organization; 2013.
- O’ Sullivan I, Lader D, Beavan-Seymour C, et al. Foundation Report: adult Dental Health Survey 2009 (Technical information). Report No. 2011 Mar 24.
- Anderson T, Thomas C, Ryan R, et al. Children’s dental health survey 2013 technical report England, Wales and Northern Ireland. Health Social Care Inf Centre hscic. 2015 Mar 19. Report No.
- Beecham JKM. Measuring mental health needs. In: Costing psychiatric interventions. London: Gaskell/Royal College of Psychiatrists; 1992. p. 163–183.
- Ochonma OG, Onwujekwe OE. Patients’ willingness to pay for the treatment of tuberculosis in Nigeria: exploring own use and altruism. Int J Equity Health. 2017;16:74.
- Agency for Healthcare Research and Quality. Hospital survey on Patient Safety Culture. 2010. 2019. Available from: http://www.ahrq.gov/qual/patientsafetyculture/
- Feyissa YM, Hanlon C, Emyu S, et al. Using a mentorship model to localise the Practical Approach to Care Kit (PACK): from South Africa to Ethiopia. BMJ Glob Health. 2019;3:e001108.
- National Medicine Therapeutics Policy Advisory Committee. EDLIZ 2015: 7th essential medicines list and standard treatment guidelines for Zimbabwe. National Medicine and Therapeutics Policy Advisory Committee; 2015.
- National Department of Health. Ideal clinic South Africa. Ideal Clinic Manual Version 16. Pretoria, South Africa; 2015.
- Cornick R, Picken S, Wattrus C, et al. The practical approach to care kit (PACK) guide: developing a clinical decision support tool to simplify, standardise and strengthen primary healthcare delivery. BMJ Glob Health. 2018;3:e000962.
- Yau M, Timmerman V, Zwarenstein M, et al. e-PC101: an electronic clinical decision support tool developed in South Africa for primary care in low-income and middle-income countries. BMJ Glob Health. 2019;3:e001093–e.
- National Department of Health. National tuberculosis management guidelines. South Africa: Department of Health; 2014.
- National Department of Health. National infection prevention control guideline for TB, MDR-TB and XDR-TB. South Africa: Department of Health; 2015.
- Haynes A, Weiser T, Berry W, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360:491–499.
- Hlongwa MNJ, Tshabala M. Profiling TB deaths in Amajuba District, KwaZulu-Natal province, South Africa. 2020.
- Hlongwa MNJ, Tshabalala. Characteristics of patients who died while on TB treatment in AMajuba District 2017-1018. Durban South Africa: Department of Health; 2020.
- University of Sierra Leone Teaching Hospitals Complex. Sierra Leone early warning scoring system (SLEWS). Sierra Leone: Connaught Freetown.
- Kohrt BA, Ramaiya MK, Rai S, et al. Development of a scoring system for non-specialist ratings of clinical competence in global mental health: a qualitative process evaluation of the Enhancing Assessment of Common Therapeutic Factors (ENACT) scale. Glob Ment Health (Camb). 2015;2. DOI:10.1017/gmh.2015.21
- Nilsen P. Making sense of implementation theories, models and frameworks. Implement Sci. 2015;10:53.
- English M, Irimu G, Agweyu A, et al. Building learning health systems to accelerate research and improve outcomes of clinical care in low- and middle-income countries. PLoS Med. 2016;13:e1001991.