Abstract
Various studies have reported that university students, who are mostly young people, rarely use existing HIV/AIDS preventive methods. Although studies have shown that young university students have a high degree of knowledge about HIV/AIDS and HIV modes of transmission, they are still not utilising the existing HIV prevention methods and still engage in risky sexual practices favourable to HIV. Some variables, such as awareness of existing HIV/AIDS prevention methods, have been associated with utilisation of such methods. The study aimed to explore factors that influence use of existing HIV/AIDS prevention methods among university students residing in a selected campus, using the Health Belief Model (HBM) as a theoretical framework. A quantitative research approach and an exploratory-descriptive design were used to describe perceived factors that influence utilisation by university students of HIV/AIDS prevention methods. A total of 335 students completed online and manual questionnaires. Study findings showed that the factors which influenced utilisation of HIV/AIDS prevention methods were mainly determined by awareness of the existing university-based HIV/AIDS prevention strategies. Most utilised prevention methods were voluntary counselling and testing services and free condoms. Perceived susceptibility and perceived threat of HIV/AIDS score was also found to correlate with HIV risk index score. Perceived susceptibility and perceived threat of HIV/AIDS showed correlation with self-efficacy on condoms and their utilisation. Most HBM variables were not predictors of utilisation of HIV/AIDS prevention methods among students. Intervention aiming to improve the utilisation of HIV/AIDS prevention methods among students at the selected university should focus on removing identified barriers, promoting HIV/AIDS prevention services and providing appropriate resources to implement such programmes.
Résumé
Diverses études ont rapporté que les étudiants universitaires, qui sont pour la plupart jeunes, utilisent rarement les méthodes de prévention du VIH/SIDA à leur porté. Bien que les études ont montré que les jeunes étudiants universitaires ont un niveau élevé de connaissances du VIH/SIDA ainsi que les modes de transmission du VIH, ces étudiants n'utilisent pas ces méthodes de prévention du VIH et se livrent encore à des pratiques sexuelles risquant et favorables au VIH. Certaines variables, telles que la sensibilisation aux méthodes de prévention du VIH/SIDA existants à l'université, ont été associées à l'utilisation de ces méthodes. Cette étude avait l'objectif d’étudier les facteurs qui influencent l'utilisation des méthodes de prévention du VIH/SIDA qui sont disponibles aux étudiants universitaires résidant dans un campus sélectionné, en utilisant le modèle de croyance à la santé (HBM) comme un cadre théorique. L'approche quantitative et la conception exploratoire-descriptive ont été utilisés pour décrire les facteurs qui influencent l'utilisation des méthodes de prévention du VIH/SIDA tels que perçus par les étudiants universitaires. Un total de 335 étudiants ont rempli des questionnaires électroniquement et manuellement. Les résultats de cette étude ont montré que les facteurs qui ont influencé l'utilisation des méthodes de prévention du VIH/SIDA étaient principalement déterminés par la sensibilisation des stratégies de prévention du VIH/SIDA disponibles à l'université. Les méthodes de prévention les plus utilisées étaient les services de conseil et dépistage volontaires et les préservatifs gratuits. Le score de susceptibilité et de menace du VIH/SIDA perçues a montré une corrélation avec le score de l'indice de risque du VIH.La susceptibilité et la menace du VIH/SIDA perçues a montré de corrélation avec l'auto-efficacité sur les préservatifs et leur utilisation. La plupart des variables du modèle de croyance à la santé (HBM) n’étaient pas des prédicteurs de l'utilisation des méthodes de prévention du VIH/SIDA parmi les étudiants.Intervention visant à améliorer l'utilisation des méthodes de prévention du VIH/SIDA parmi les étudiants de l'université choisie devrait se concentrer sur l'élimination des obstacles identifiés, la promotion des services de prévention du VIH/SIDA, et fournir des ressources appropriées pour implémenter ces programmes.
1. Introduction
UNAIDS/WHO (Citation2008) reported that by the end of 2007, approximately 33.2 million people worldwide were living with HIV, and 2.5 million people were newly infected with HIV – 45% of these being young people aged between 14 and 25 years. The report emphasised that preventing new HIV infections remains the most powerful weapon to fight and reverse the epidemic, especially among young people. Sub-Saharan Africa remains the most heavily affected region of the world, accounting for approximately two-thirds of all incident and prevalent HIV infections and three-quarters of all AIDS deaths (Shisana, Rehle, Simbayi, Zuma, Jooste, Pillay-van-Wyk, et al. Citation2009; Vitoria, Granich, Gilks, Gunneberg, Hosseini, Were, et al. Citation2009).
In South Africa, the national HIV/AIDS prevalence rate at the end of 2007 was estimated to be 18.1% (UNAIDS/WHO Citation2008). Young people between 15 and 24 years of age account for over five million new HIV infections worldwide each year, with an estimated 6000 youth becoming infected each day across the globe (UNAIDS Citation2006). The findings of a survey conducted in South Africa by Pettifor, Straten, Dunbar, Shiboski and Padian (Citation2004) showed that young South Africans aged 15–24 years had a high HIV prevalence of 10.2%; of these, 77% were women.
Studies conducted in African countries such as Ghana, Nigeria and Kenya have identified university students as a group at high risk for HIV infection due to their risky sexual behaviours (Adam & Mutungi Citation2007; Mberia & Mukulu Citation2011; Oppong & Oti-Boadi Citation2013; Osonwa, Eko, Abeshi & Offiong Citation2013). Various studies have reported on female university students engaging in cross-generational sex (Ntata, Muula, Siziya & Kayambazinthu Citation2008) where female students have sex with older men who are able to offer financial compensation in the form of school fees, clothing, food and cell phones. Cross-generational sex seems to be a substantial source of infection among South African youth, with one generational population presenting with higher and the other with lower HIV prevalence (Katz & Low-Beer Citation2008). Such relationships expose female students to risky sexual behaviours. Nor are young women the only ones engaging in risky sexual behaviours. Recent studies have shown that 68% of South African young women and 56% of young men under 25 years of age were engaging in high-risk sexual behaviours (Simbayi, Kalichman, Jooste, Mfecane & Cain Citation2005).
In response to the HIV/AIDS pandemic, HIV/AIDS policies and HIV prevention programmes have been put in place in all institutions of higher learning in South Africa and most have implemented interventions aimed at preventing HIV/AIDS (Van Wyk & Pieterse Citation2006). These interventions comprise existing HIV/AIDS prevention policy, education and awareness raising – especially the ABC message (Abstain, Be faithful, use a Condom) – voluntary counselling and testing (VCT) for HIV, affordable antiretroviral therapy (ART), HIV/AIDS wellness programmes, peer education programmes and support services, and integration of HIV/AIDS issues in teaching, research and service activities (Van Wyk & Pieterse Citation2006). Reviewed literature shows that HIV prevention methods at institutions of higher learning have mainly focused on knowledge, awareness and practices (Mberia & Mukulu Citation2011; Reddy & Frantz Citation2011), but Reddy and Frantz argue that high level of knowledge about HIV/AIDS is not in itself sufficient to promote behaviour change among South African university students.
To increase utilisation of HIV prevention strategies, some institutions of higher learning have made condoms freely available, extensively promoting their use and helping to overcome social and personal obstacles that limit their use (Mberia & Mukulu Citation2011; Policy Project Citation2000; William & Cherly Citation1999). A study on HIV/AIDS risk factors among students conducted at the University of the Free State by Badenhorst, van Staden and Coetsee (Citation2008) showed that there was improved utilisation of HIV/AIDS prevention methods by university students and that students were highly aware that they were at high risk of contracting HIV infection. While these HIV prevention strategies have been widely advocated as potentially effective in the fight against the AIDS pandemic, it has nevertheless emerged in various studies that the sexual behaviour of young university students does not correspond with their heightened awareness and knowledge about HIV/AIDS and HIV modes of transmission (Ntata et al. Citation2008; Simbayi et al. Citation2005), as they continued to engage in unprotected sexual behaviour that put them at high risk of contracting HIV infection (Badenhorst et al. Citation2008; Hartell Citation2005; Kaiser Family Foundation Citation2006). These findings demonstrate that existing HIV prevention methods continue to be underutilised by university students.
There is therefore a need to determine what factors influence the utilisation of existing HIV/AIDS prevention methods, and what the barriers are to their utilisation (as perceived by students) so that relevant measures can be put in place.
2. Purpose of the study
The purpose of this study was to explore factors that influence the use of existing HIV/AIDS prevention methods among university students residing at a selected campus.
3. Methodology
The study was guided by the Health Belief Model (HBM), as developed in the 1950s by a group of psychologists (Hochbaum, Rosenstock, and Kegels) working in the US Public Health Services (Glanz, Rimer & Viswanath Citation2008:46). The model attempts to describe health-seeking behaviours (Rosenstock Citation1974) and has been widely used both to explain change and maintenance of health-related behaviours and as a guiding framework for health behaviour interventions. The HBM suggests that health-related action depends upon (a) the existence of sufficient motivation or health concern to make health issues relevant (Perceived Susceptibility) (b) the belief that one is susceptible to a serious health problem or to sequelae of that illness (Perceived Threat) and (c) the belief that following a particular health recommendation would be beneficial in reducing the perceived threat (Perceived Severity), at a subjectively acceptable cost (Rosenstock, Strecher & Becker Citation1988). The model hypothesises that for an individual to take action, he must decide that the behaviour creates a serious health problem, and that he is personally susceptible to its health harm, and that moderating or stopping the behaviour will be beneficial.
For instance, in HIV/AIDS-related studies, the theory may seek to explain why sexually active youth indulge in risky sexual behaviours. The guiding components of the model may explain that youth who have low risk perception of being infected with HIV or sexually transmitted infection (STI) (Perceived Susceptibility) are likely to engage in risky sexual behaviour, and that such behaviour will expose them to serious health problems such as HIV or STIs, unwanted pregnancy or other sexual and reproductive health problems (Perceived Severity). The youth who decide to use condom correctly and consistently will always be protected from these unwanted health problems and consequently live a healthy life (Perceived Benefit). In previous studies, the HBM has concluded that the youth who were adherent to consistent condom usage had higher perceived susceptibility scores and lower perceived barrier as compared to those who did not intend to use HIV preventive measures, whose perceived benefits were lower. Perceived susceptibility is necessary before commitment to change these risky behaviours can occur (Glanz et al. Citation2008).
A quantitative research approach was followed to explore variables and examine relationships among them. An exploratory–descriptive design was used to describe the perceived factors that influence the utilisation by university students of HIV/AIDS prevention methods.
4. Research setting
The study was conducted at on- and off-campus residences of a selected campus at the University of KwaZulu-Natal (UKZN), South Africa.
5. Population, sampling and sample size
The university residences of selected Durban campuses accommodate approximately 2162 students. The on-campus residences are grouped into two halls; one of these halls comprises 12 individual residences, and the other has two components: a cluster residence and a six-storey residence. There are also two off-campus residences, giving a total of 14 residences. Students residing in selected halls of these residences were invited to participate in the study.
Simple random sampling was used to select three on-campus residences, and purposive sampling was used to select one off-campus residence. Purposive sampling was chosen because there were only two off-campus residences, and including them in the sampling frame for random sampling would reduce their chance of being selected in the sample. Respondents were selected using convenience sampling. In each residence, students who were available at the time of data collection were invited to participate in the study. Online questionnaires were linked to a created web link whereby the questionnaires were sent back by respondents after completion.
6. Data collection procedure
The researcher approached respondents in their respective residences in the evenings. Students who consented to participate in the study completed the questionnaires manually. A ballot box where respondents deposited their completed questionnaires was provided. A similar questionnaire was sent and completed by respondents online. This questionnaire incorporated a link whereby completed questionnaires could be sent back.
7. Research instrument description
A pre-existing questionnaire by Simbayi et al. (Citation2005) on ‘Risk Factors for HIV/AIDS among Youth in Cape Town, South Africa’ was used. The questionnaire was adapted to make it relevant to the current study.
The questionnaire comprised six sections in which questions were designed to collect data relating to the following categories: (a) socio-demographic data, (b) perceived susceptibility, perceived threat and attitude towards HIV/AIDS, (c) knowledge of HIV/AIDS and sources of information, (d) sexual experiences and risky sexual behaviour, (e) awareness of on-campus HIV prevention methods and their utilisation and (f) perceived barriers, perceived benefits and self-efficacy in relation to utilisation of HIV/AIDS prevention methods.
Additional questions were added to the original questionnaire drawn up by Simbayi et al. (Citation2005), and the research was conducted in a different setting from the earlier study. A pilot study was therefore conducted to test design issues.
The online pilot questionnaire was sent by the researcher to five students and another five students were given the questionnaires manually to complete. Findings of the pilot study showed that the questionnaire was easy to understand and contained no ambiguities or misunderstandings.
8. Data analysis
Data from both online and manual questionnaires were analysed using the Statistics Package of Social Sciences (SPSS) Version 15–0.
8.1. Descriptive statistics
Categorical variables were summarised using frequency distributions (counts and percentages) in tables, bar charts and graphs. Numerical variables were summarised by measures of central tendency; mean, mode and median; and measures of variability.
8.2. Analytic statistics
The chi-square test was used to further describe relationships, similarities and differences between categorical independent variables and dependent variables, and to establish demographic differences among respondents. Correlations were performed to assess relationships between quantitative variables. Because most compared variables did not show statistically significant differences, the multivariate regression to assess many independent variables simultaneously was not performed.
9. Ethical consideration
The research proposal was approved by the Ethics Committee of the University. Permission to conduct the study was also obtained from the Dean of Students and the Housing Administrator. Informed consent was duly sought from respondents. For the online questionnaire, consent was obtained by the fact that respondents accepted to complete the questionnaire, and this was clarified in the Information document. Assurance and adherence to confidentiality of elicited information were maintained throughout the study. Participation in the study was voluntary. Respondents were informed that they could stop or withdraw from participating in the study at any time without any penalty.
10. Results
Three hundred and sixty questionnaires were distributed among students who reside in 4 residences in a selected campus, out of which 261 (72.5%) returned the completed questionnaires. With the online questionnaires, completed and returned questionnaires were received from 74 respondents. There were thus a total of 335 respondents, which represented 15.5% of the whole population.
Students were asked a series of questions relating to variables such as awareness of existing HIV/AIDS prevention methods on their campus and university-wide, knowledge of HIV/AIDS and encouraging factors and perceived barriers to utilising these methods. Furthermore, they were asked questions relating to their utilisation of these existing methods.
10.1. Socio-demographic characteristics of respondents
The age of the participants ranged from 17 to 48 years with a mean age of 22.9 years, a median of 22 years and a mode of 21 years. Other demographic information is presented in .
Table 1. Socio-demographic data of respondents.
10.2. Awareness of HIV/AIDS prevention methods
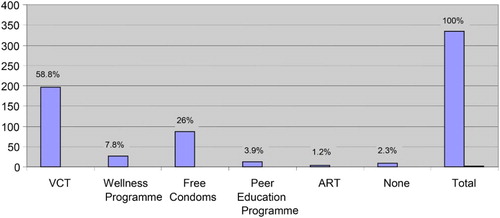
Just over half of respondents were aware of VCT, 197 (58.8%); of free condoms, 87 (26%); and of the Wellness Programme, 26 (7.8%). Only 13 (3.9%) were aware of the Peer Education Programme and just 4 (1.2%) were aware of ART. Eight (2.3%) respondents did not report awareness of any HIV/AIDS prevention methods ( and ).
Table 2. Awareness and utilisation of HIV/AIDS prevention methods.
10.3. Utilisation of on-campus HIV/AIDS prevention methods
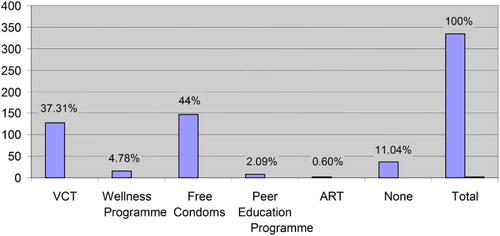
Even though a majority of students indicated awareness of VCT as an HIV/AIDS prevention method, only 37.9% of students had utilised this service, while 43.9% had utilised free condoms, making this the most utilised on-campus HIV/AIDS prevention method. The least utilised preventive methods were the Wellness Programme, by 4.8% of respondents; the Peer Education Programme, by 2%; and ART by just two respondents (0.6%) ( and ).
10.3.1. ABC methods
Respondents were asked to report on their utilisation of ABC as a prevention method, on- and off-campus. One hundred and sixty-two (49.5%) respondents reported that they used condoms, 86 (26.3%) reported that they abstained and 79 (24.2%) reported that they were faithful.
10.3.2. HIV testing and other HIV/AIDS prevention methods
Altogether, more than two-thirds, 249 (76.4%) respondents had been tested for HIV, while 76 (23%) had never been tested for HIV. A large majority, totalling 283 (86.3%) respondents, reported that they planned to be tested and 45 (13.7%) reported that they did not plan to be tested.
10.4. Relationship between identified variables and utilisation of HIV prevention methods
There was no relationship between any socio-demographic variables and utilisation of HIV/AIDS prevention methods.
10.4.1. Awareness
A chi-square test to compare awareness and utilisation of HIV/AIDS prevention methods showed a statistically significant difference between awareness and utilisation; the χ2 value was 5.838, with p-value .047. There was a strong association between awareness and HIV/AIDS prevention methods utilisation. The degree of agreement between these two variables was also high (98.3%) ().
Table 3. Association between awareness and utilisation of HIV/AIDS prevention methods.
10.5. Relationships between demographic variables and HIV testing
Fifty-six per cent of female respondents had been tested for HIV, as compared to 43.9% of males. There was, however, no statistically significant difference between HIV testing and gender; the χ2 value was 3.367 and the p-value was .052 at 95% CI.
In relation to condom usage, 50.8% of females compared with 49.2% of males had used condoms in the most recent sexual intercourse. There was also no gender difference on condom usage: the χ2 value was 1.623; the p-value was .203 at 95% CI.
10.6. Perceived barriers, benefits and self-efficacy, and HIV/AIDS prevention methods utilisation
10.6.1. Perceived barriers and self-efficacy on abstinence
A majority, totalling 286 (86.4%) of respondents, were in agreement that abstinence was a way to protect oneself from getting HIV infection, while 59 (37.1%) agreed that abstinence was not practical (). The perceived barriers and self-efficacy minimum score value was 1, the maximum was 20 and the mean was moderately low to high at 12.06 (60.3%).
10.6.2. Perceived susceptibility/perceived threat and self-efficacy on abstinence
The perceived susceptibility and perceived threat mean score was 21.3881 against 12.0604 abstinence score. The Pearson correlation value was 0.057, at 95% confidence interval. There was therefore no correlation between perceived susceptibility/perceived threat and self-efficacy on abstinence.
10.6.3. Perceptions and self-efficacy on condom usage
Fourteen (4.4%) and 30 (9.5%) respondents, strongly agreed, or agreed, respectively, that they did not use condoms because they trusted their sexual partner. Forty-three (13.7%) and equally 43 (13.7%) respondents agreed strongly, or agreed, that condoms were unnatural. In addition, 6 (2%) and 25 (8.2%) respondents strongly agreed, or agreed, that their sexual partners did not like condoms. Thirteen (4.2%) and 59 (18.9%) respondents strongly agreed, or agreed, that condoms decrease sexual pleasure, and 29 (9.4%) and 20 (6.5%) respondents strongly agreed, or agreed, that they were not able to negotiate condom usage with their sexual partner. A substantial majority of 197 (60.8%) and 74 (22.8%) respondents strongly agreed, or agreed, that condoms were easy to get, but 62 (19.4%) and 77 (24.1%) strongly agreed, or agreed, that condoms were sometimes not available ().
Table 4. Perceived barriers, perceived benefits and self-efficacy.
10.6.4. Relationships between perceived susceptibility and perceived threat score and self-efficacy on condom use
The mean score for perceived susceptibility and perceived threat was 21.3881 against 23.4667 for perceptions score on condom use. A Pearson correlation to test the relationship between perceived susceptibility/perceived threat of HIV/AIDS and self-efficacy on condom use was 0.80 at 95% confidence interval. There was therefore correlation between perceived susceptibility and perceived threat of HIV/AIDS and self-efficacy on condom and condom use ().
10.6.5. Relationship between perceptions and self-efficacy on VCT services, condoms and their utilisation
Mean difference between condom perceptions/self-efficacy score and condom usage was −0.725054; p-value was .539 at 95% confidence interval [CI = −3.02576 to 1.58469]. In addition, mean difference between VCT perceptions/self-efficacy score and HIV testing was −0.62331; p-value was .537 at 95% confidence interval [CI = −2.60903 to 1.36241]. There was therefore no relationship between these perceptions and utilisation of HIV/AIDS prevention methods.
10.7. Factors encouraging the use of HIV/AIDS preventive methods
The most-reported factors encouraging HIV preventive method utilisation were student movements against HIV/AIDS, reported by 19 (5.9%); inclusion of HIV/AIDS programme in academic curriculum, reported by 19 (5.9%); and having open days against HIV/AIDS, reported by 15 (4.7%).
10.8. Perceived barriers to the use of HIV/AIDS prevention methods
The most reported barriers were chiefly issues around VCT and awareness, as summarised in and .
Table 5. Reported barriers to the use of HIV/AIDS prevention methods among students.
Table 6. Reported barriers to the use of HIV/AIDS prevention methods among students (n = 225).
11. Discussion of results
The findings of this study showed that student demographics such as age and gender were not predictors of utilisation of HIV/AIDS prevention methods. However, though there were no significant statistical differences among these variables, results showed that Indian respondents used on-campus VCT more than black students, in the order of 5 (71.4%) against 120 (43.6%). It was also noted that White respondents made no use of on-campus VCT but they all used condoms, 100% (12), whereas less than half of black respondents, 130 (47.3%), used condoms and only 28.6% of Indian respondents used condoms. These findings suggest very low condom use among black and Indian respondents, which is a concern for HIV/AIDS prevention among university students. Also, there was no significant difference between undergraduate and postgraduate students in utilisation of HIV/AIDS prevention methods.
The findings of the current study showed further that the overall mean of perceived susceptibility and perceived threat of HIV/AIDS was high (76.4%), with standard deviation (SD = 3.185). In addition, 76.5% of respondents were in agreement that the possibility of become infected with HIV/AIDS was a matter of concern for them. However, their high perceived susceptibility to HIV/AIDS did not correlate with use of any HIV/AIDS prevention methods. This finding differed from the findings of previous studies carried out in the former University of Durban-Westville which revealed that students did not perceive themselves as susceptible to contracting HIV/AIDS and that their use of those prevention methods was very low (Stremlau & Nkosi Citation2001; Uys, Alexander, Martin & Ichharam Citation2001).
While similar studies conducted in Nepal (Iriyama, Nakahara, Jimba, Ichikawa & Wakai Citation2007) and in Kenya (Othero, Aduma & Opil Citation2009) showed that students did perceive themselves as susceptible to HIV infection as a consequence of their previous sexual experience, these studies nonetheless showed troublingly low utilisation of existing on-campus HIV/AIDS prevention methods.
The findings of the current study also showed that even though the overall mean knowledge of HIV/AIDS score among students was high, at 82.22%, students nonetheless harboured significant misconceptions about HIV modes of transmission; a very large majority of 209 (92.8%) students reported that one cannot get HIV by having sex with a virgin, and a mere 8 (2.4%) respondents reported that they did not know how one could contract HIV. As predicted in previous studies, knowledge of HIV/AIDS in this study did not correlate with utilisation of any of the HIV/AIDS prevention methods. These findings correspond with earlier studies conducted in South Africa, China and Kenya which reported that university students had gaps in knowledge of HIV mode of transmission that needed to be addressed through health education (Lonn, Sahlholm, Maimaiti, Abdukarim & Anderson Citation2007; Othero et al. Citation2009; Stremlau & Nkosi Citation2001; Uys et al. Citation2001). This finding suggests that even though there are strategies in place that focus on HIV/AIDS awareness and information giving, there is still an urgent need to address issues relating in particular to HIV/AIDS modes of transmission that are a potential concern for young people. Although the previous studies have reported that students' awareness and high level of knowledge about existing HIV/AIDS prevention methods did not correlate with their utilisation (Ergene, Cok, Tumer & Unal Citation2005; Fagen & Flay Citation2009), the current study showed positive results in that the prevention methods which students reported awareness of were also those most utilised – two examples being free condoms, 146 (43.58%) and VCT, 127 (37.91%). As expected, the findings showed that students were unlikely to utilise programmes that they were not aware of. The least utilised preventive methods were the Wellness Programme, 16 (4.78%); the Peer Education Programme, 7 (2.09%); and ART, 2 (0.6%). Only 31.2% perceived peer educators to be helpful, and 44.5% felt that the programme was not helpful. This was a disappointing finding, as one would expect wellness and peer education programmes to be at the forefront in providing necessary information regarding HIV/AIDS prevention.
Identified barriers to HIV testing included fear of being stigmatised, fear of testing positive, low self-efficacy and low perceived susceptibility. Similar barriers were identified in the study conducted in India by Chakrapani, Shanmugam, Michael, Velayudham and Newman (Citation2008) on factors influencing HIV testing. Also identified as barriers were: location of HIV testing centres closer to residences; waiting time for counselling, testing and getting test results; lack of same-day HIV testing methods; and incompetent and insensitive counsellors.
12. Conclusion and recommendations
It emerged from the findings of this study that most HBM variables were not predictors of HIV/AIDS prevention methods utilisation among university students. Interventions for HIV/AIDS prevention among students at UKZN should consequently focus on removing identified barriers by providing a favourable HIV testing venue that would ensure confidentiality, employing the same-day HIV testing method, advertising HIV/AIDS prevention services, providing correct knowledge of HIV/AIDS (especially in relation to HIV modes of transmission) and focusing on behavioural change.
Follow-up studies should explore the appropriateness and comprehensiveness of the existing HIV prevention methods, including wellness programmes, in order to determine why they are not being utilised.
A specific recommendation would be to include HIV/AIDS information in the academic curriculum so as to offer comprehensive and correct information on HIV/AIDS to students. Also needed is a comparative follow-up study, involving several countries, to explore measures and best practices to improve utilisation of HIV/AIDS prevention methods.
References
- Adam, M. B. & Mutungi, M. (2007). Sexual Risk Behavior among Kenyan University Students. Journal of the Arizona-Nevada Academy of Science, 39(2), 91–98. doi: 10.2181/036.039.0205
- Badenhorst, G., van Staden, A. & Coetsee, E. (2008). HIV/AIDS Risk Factors among Residence Students at the University of the Free State. Curationis, 31(3), 27–35. doi: 10.4102/curationis.v31i3.1028
- Chakrapani, V., Shanmugam, M., Michael, S., Velayudham, J. & Newman, P. A. (2008). HIV Testing Barriers and Facilitators among Populations At-Risk in Chennai, India. A Qualitative Study among Men Who Have Sex with Men, Injecting Drug Users, Aravanis/Transwomen, and Sex Workers. http://www.inpplus.net/images/DL_APCASO%20Research%20Report-Jun2008.pdf (Accessed 25 November 2009).
- Ergene, T., Cok, F., Tumer, A. & Unal, S. (2005). A Controlled-Study of Preventive Effect of Peer Education and Single-Session Lectures on HIV/AIDS Knowledge and Attitudes among University Students in Turkey. AIDS Educational and Prevention, 17(3), 268–278. doi: 10.1521/aeap.17.4.268.66533
- Fagen, M. C. & Flay, B. R. (2009). Sustaining a School-Based Prevention Program: Results from the Aban Aya Sustainability Project. Health Education Behavior, 36(1), 24–28.
- Glanz, K., Rimer, B. K. & Viswanath, K. (2008). Health Behaviour and Health Education: Theory Research and Practice, 4th ed., San Francisco, Jossey-Bass.
- Hartell, C. G. (2005). HIV/AIDS in South Africa: A Review of Sexual Behavior among Adolescents: A Review. Adolescence Spring, 157(40), 171–181.
- Iriyama, S., Nakahara, S., Jimba, M., Ichikawa, M. & Wakai, S. (2007). AIDS Health Beliefs and Intention for Sexual Abstinence among Male Adolescent Students in Kathmandu, Nepal: A Test of Perceived Severity and Susceptibility. Public Health, 121(1), 64–72. doi: 10.1016/j.puhe.2006.08.016
- Kaiser Family Foundation (2006). HIV Prevalence among Young People in Southern India Has Declined by about 35%, Study Says. http://www.thebody.com/content/news/art7222.html (Accessed 1 May 2009).
- Katz, I. & Low-Beer, D. (2008). Why Has HIV Stabilized in South Africa, Yet Not Declined Further? Age and Sexual Behavior Patterns among Youth. Sexually Transmitted Diseases, 35(10), 837–842. doi: 10.1097/OLQ.0b013e31817c0be5
- Lonn, E., Sahlholm, K., Maimaiti, R., Abdukarim, K. & Anderson, R. (2007). A Traditional Society in Change Encounters HIV/AIDS: Knowledge, Attitudes, and Risk Behavior among Students in Northwestern China. AIDS Patient Care and STDs, 21(1), 48–56. doi: 10.1089/apc.2006.0063
- Mberia, H. K. & Mukulu, E. (2011). Persuasive Communication Factors That Influence University Students in Their Response to HIV and AIDS Prevention Campaign Message [Special Issue]. International Journal of Humanities and Social Science, 1(11), 254–260.
- Ntata, P. R. T., Muula, A. S., Siziya, S. & Kayambazinthu, E. (2008). Gender Differences in University Students’ HIV/AIDS-Related Knowledge and Sexual Behaviours in Malawi: A Pilot Study: Brief Report. SAHARA: Journal of Social Aspects of HIV/AIDS Research Alliance, 5(4), 201–205. doi: 10.1080/17290376.2008.9724920
- Oppong, A. K. & Oti-Boadi, M. (2013). HIV/AIDS Knowledge among Undergraduate University Students: Implications for Health Education Programs in Ghana. African Health Sciences, 13(2), 270–277.
- Osonwa, K., Eko, J., Abeshi, S. & Offiong, D. (2013). Factors Affecting Accessibility and Utilization of Condom for HIV Prevention among Students in University of Calabar Community, Nigeria. International Journal of Learning & Development, 3(4), 46–63. doi: 10.5296/ijld.v3i4.4243
- Othero, D. M., Aduma, P. & Opil, C. O. (2009). Knowledge, Attitudes and Sexual Practices of University Students for Advancing Peer HIV Education. East African Medical Journal, 8(1), 11–15.
- Pettifor, A. E., Straten, A., Dunbar, M. S., Shiboski, S. C. & Padian, N. C. (2004). Early Age of First Sex: A Risk Factor for HIV Infection among Women in Zimbabwe. AIDS, 18(10), 1435–1442. doi: 10.1097/01.aids.0000131338.61042.b8
- Policy Project (2000). Factors Affecting Accessibility and Utilization of Condom (a Community Based Study), Addis Ababa, The Futures Group International – Ethiopia.
- Reddy, P. & Frantz, J. (2011). HIV/AIDS knowledge, behaviour and beliefs among South African university students. SAHARA J (Journal of Social Aspects of HIV/AIDS Research Alliance), 8(4), 166–170. doi: 10.1080/17290376.2011.9725000
- Rosenstock, I. M. (1974). Historical Origins of the Health Belief Model. Health Education Monographs, 2(4), 328–335.
- Rosenstock, I. M., Strecher, V. J. & Becker, M. H. (1988). Social Learning Theory and the Health Belief Model. Health Education Quarterly, 15(2), 175–183. doi: 10.1177/109019818801500203
- Shisana, O., Rehle, T., Simbayi, L. C., Zuma, K., Jooste, S., Pillay-van-Wyk, V., et al. (2009). South African National HIV Prevalence, Incidence, Behaviour and Communication Survey 2008: A Turning Tide among Teenagers? Cape Town, South Africa, HSRC Press.
- Simbayi, L. C., Kalichman, S. C., Jooste, S., Cherry, C., Mfecane, S. & Cain, D. (2005). Risk Factors for HIV-AIDS among Youth in Cape Town, South Africa. AIDS and Behavior, 9(1), 53–61. doi: 10.1007/s10461-005-1681-4
- Stremlau, J. & Nkosi, N. (2001). The AIDS Crisis at South African Universities. http://idrc.ca/en/ev-5398-201-1-DO_TOPIC.html (Accessed 29 November 2009).
- UNAIDS. (2006). AIDS Epidemic update: Special report on HIV/AIDS. http://data.unaids.org/pub/epireport/2006/2006_epiupdate_en.pdf (Accessed 7 March 2014).
- UNAIDS/WHO. (2008). Report on the global AIDS epidemic. http://www.unaids.org/en/KnowledgeCentre/HIVData/GlobalReport/2008/2008_Global_report.asp (Accessed 15 May 2009).
- Uys, T., Alexander, P., Martin, L. & Ichharam, M. (2001). HIV/AIDS and Students at RAU Centre for sociological research. Interim Report. Johannesburg. http://www.uj.ac.za/Portals/159/docs/CSRAnnualReport2001.doc (Accessed 10 March 2009).
- Van Wyk, B. & Pieterse, J. (2006). Institutional Responses to HIV/AIDS from Institutions of Higher Education in the Southern African Development Community. http://www.sarua.org/files/publications/SARUA_HEI_HIV_AIDS_Study.pdf (Accessed 7 March 2014).
- Vitoria, M., Granich, R., Gilks, C. F., Gunneberg, C., Hosseini, M., Were, W., et al. (2009). The Global Fight Against HIV/AIDS, Tuberculosis, and Malaria: Current Status and Future Perspectives. American Journal of Clinical Pathology, 131(6), 844–848. http://ajcp.ascpjournals.org/content/131/6/844.short (Accessed 25 November 2013). doi: 10.1309/AJCP5XHDB1PNAEYT
- William, K. A. & Cherly, S. A. (1999). Determinants of Condom Use to Prevent HIV Infection among Youth in Ghana. Journal of Adolescent Health, 24(1), 63–72. doi: 10.1016/S1054-139X(98)00062-7