ABSTRACT
Introduction: Incorrect inhaler technique is one reason why the efficacies of inhaled asthma treatments in clinical trials and effectiveness in the real world differ. Inhaler technique is critical for drug delivery to the lungs; incorrect technique negatively impacts asthma control and long-term outcomes. Breath-triggered inhalers (BTIs) can simplify drug administration and are suitable for most patients, including those with reduced inspiratory flow. Until recently, no inhaled corticosteroid/long-acting β2-agonist combination BTI was available in Europe. The flutiform® (fluticasone propionate/formoterol fumarate [FP/FORM]) k-haler® is the first combination BTI now approved in Europe for asthma maintenance treatment.
Areas covered: We review studies examining the challenges posed to patients by different inhaler types and explore evidence demonstrating the clinical efficacy of FP/FORM administered via a pressurized metered-dose inhaler. We also review the pharmacokinetic/pharmacodynamic studies supporting FP/FORM k-haler use, and consider data showing high lung deposition with the device. Finally, we review patient experiences using the BTI, device characteristics, and health economic aspects.
Expert opinion: Despite the availability of therapies, asthma control levels remain low, and there is a clear need for easy-to-use inhalers. Research to increase our understanding of critical errors with each inhaler and how to overcome them is important for improving care.
Abbreviations: AUCt: area under the plasma concentration–time curve from the time of dosing to the last measurable concentration; BDP: beclometasone dipropionate; BTI: breath-triggered inhaler; BUD: budesonide; CI: confidence interval; Cmax: maximum observed plasma concentration; DPI: dry powder inhaler; FDC: fixed-dose combination; FEV1: forced expiratory volume in 1 s; FORM: formoterol fumarate; FP: fluticasone propionate; HCP: health-care professional; ICS: inhaled corticosteroid; LABA: long-acting β2-agonist; OR: odds ratio; PIL: patient information leaflet; pMDI: pressurized metered-dose inhaler; SAL: salmeterol xinafoate
1. Introduction
The effectiveness of inhaled asthma treatments depends on the extent to which the inhaler device facilitates delivery of drug into the lungs. Inhaler errors are frequent with all device types; most patients (70–80%) make mistakes when using their inhaler, and are often unaware that there is a problem with their technique [Citation1]. Compared with individuals with good inhaler technique, those using inhalers suboptimally are more likely to have poorer asthma control, with an increased risk of exacerbations and more adverse events [Citation1–Citation6].
1.1. Dry powder and metered-dose inhalers
The majority of devices for the treatment of asthma fall into one of two types: dry powder inhalers (DPIs) and pressurized metered-dose inhalers (pMDIs). pMDIs are ‘active’ devices because they propel the aerosolized drug. For effective delivery to the lungs, patients must actuate the device after starting to inhale and while continuing to do so (). Patients can use a spacer to help overcome this challenge; use of a spacer in conjunction with a pMDI can improve drug delivery to the lungs [Citation7]. However, at least one large study has shown no improvement in outcomes associated with using compared with not using a spacer (which may relate to poor actual adherence) [Citation8]. Despite recommendations in national and international guidelines, spacers are generally underused [Citation7]. In contrast to pMDIs, DPIs are ‘passive’ because they provide no driving force to release the drug from the device. For effective deposition of drug into the lungs, DPIs require patients to generate enough inspiratory force to extract the powdered drug and to disaggregate the powder into respirable particles () [Citation9]. Although DPIs do not rely on a patient’s ability to actuate during inhalation, their effectiveness can be limited if individuals do not inhale with enough force. This can be due to inability, lack of effort, or insufficient prior emptying of the lungs.
Table 1. Key characteristics and availability of DPIs, pMDIs, and BTIs for the treatment of asthma, as of May 2019.
Although it is well known that poor inhaler technique contributes to poor asthma control, the effect of specific errors on asthma outcomes is less well understood. With this in mind, the cross-sectional, observational, CRITical Inhaler mistaKes and Asthma controL (CRITIKAL) study was carried out. The CRITIKAL study included patients with moderate-to-severe asthma and was designed to identify critical errors by exploring direct relationships between specific inhaler errors and asthma outcomes in patients using either a DPI (Symbicort® Turbohaler® [AstraZeneca, Södertälje, Sweden] [n = 2074] or Seretide® Diskus® [GlaxoSmithKline, Brentford, UK] [n = 826]) or a pMDI (Seretide Evohaler® [GlaxoSmithKline, Brentford, UK] [n = 760]) [Citation10]. Inhaler errors were frequent with all devices tested in this study: poor coordination with actuation before inhalation was seen in around a quarter of pMDI users, and insufficient inspiratory effort was made by around a third of DPI users. Both errors were associated with an increased risk of uncontrolled asthma (adjusted odds ratio [OR] [95% confidence interval (CI)]: Turbohaler, 1.30 [1.08–1.57]; Diskus, 1.56 [1.17–2.07]; pMDI, 1.55 [1.11–2.16]) and were also associated with an increased exacerbation rate in DPI users [Citation10].
1.2. Breath-triggered inhalers
An alternative to DPIs and pMDIs is the breath-actuated or breath-triggered inhaler (BTI), which releases a dose of medication in response to the user’s inhalation. The first breath-actuated pressurized aerosol inhaler was a pocket-sized device developed in 1970 for delivery of inhaled corticosteroid (ICS) alone. Patients found it convenient and simple to use but it had limited commercial success [Citation11]. Historically termed breath-actuated inhalers (Autohaler® [3M Health Care Limited, Loughborough, UK]; Easi-Breathe® [Norton Healthcare Limited, London, UK]), they can also be described as ‘breath-triggered inhalers’, a term proposed to be more readily understood by patients. Mechanistically, BTIs offer advantages over both conventional pMDIs and DPIs. Compared with pMDIs, automatic release of a drug dose upon inhalation negates the need for coordinating actuation during inhalation; unlike most DPIs, the use of a propelled aerosol negates the need for forcible inhalation to generate respirable particles (). A drawback of the Autohaler in particular is the forceful spring mechanism that causes a small proportion of patients to stop inhaling either immediately or too soon after the device is triggered. As a result, the amount of drug delivered is reduced [Citation3].
Several studies have evaluated device handling and asthma control with the Autohaler and Easi-Breathe BTIs. Successful actuation rates are higher among patients using BTIs than in those using DPIs [Citation12] or pMDIs [Citation13]. In a randomized crossover study of 51 hospitalized children with asthma who had acute exacerbations, all participants had a sufficient peak inspiratory flow rate with which to actuate the BTI; 99 of 100 actuations were successful with the BTI compared with 74 of 100 with a DPI [Citation12]. Similarly, 79% of actuations with a BTI by a group of elderly patients were judged successful, compared with 60% of actuations with a conventional pMDI [Citation13]. Studies have also shown that correct inhaler use is more common with BTIs than with other device types [Citation12–Citation15]. In one such study, 100 patients who had been referred for inhaler assessment were shown how to use seven different inhalers in a random sequence [Citation15]. Having been assessed for their technique, patients were asked to nominate their three preferred devices. Inhaler technique was best with the two BTIs included in the study; these devices were also awarded the highest preference scores by patients [Citation15]. Scintigraphy studies showed that a BTI obtains the same lung deposition of drug as a pMDI used correctly and three times that obtained with a pMDI used with poor coordination [Citation16].
These benefits are consistent with data showing that the use of BTIs can improve measures of asthma control [Citation16–Citation22]. Compared with patients using other inhalers, a retrospective, matched-cohort, registry analysis of 1958 patients found improved overall asthma control among individuals switching to BTIs (OR [95% CI], 1.26 [1.05–1.52]) [Citation17]. Moreover, patients with asthma who did not coordinate actuation and inhalation with a pMDI experienced significant improvements in lung function when using a BTI (based on the area under the curve for forced expiratory volume in 1 s [FEV1] and for the maximum velocity [Vmax] of bronchodilator response; p < 0.05 [both measures]) [Citation16]. After switching from another device, asthma control (assessed by the Asthma Control Questionnaire) improved significantly after 4 weeks of using a BTI, based on responses from 1510 patients with asthma who participated in the SYSTER survey; the survey also found a significant increase in self-reported patient adherence to treatment (p < 0.0001 for both effects) [Citation22].
2. The k-haler® device: the first BTI to deliver an ICS/long-acting β2-agonist combination in Europe
Until August 2018, only two BTIs (Autohaler and Easi-Breathe) were available in Europe for the delivery of asthma medication, but neither offered an ICS/long-acting β2-agonist (LABA) fixed-dose combination (FDC) (). Together with ICS monotherapy, ICS/LABA FDC products comprise one of the most important options available for asthma maintenance therapy [Citation1]. In September 2018, the fluticasone propionate/formoterol fumarate (FP/FORM; flutiform® [Jagotec AG, Muttenz, Switzerland]) k-haler® (Mundipharma AG, Basel, Switzerland & Clinical Designs Ltd., Cambridge, UK) became the first BTI containing an ICS/LABA combination product to launch in Europe. The aim of this review is to summarize the available published studies with the k-haler BTI.
Development of inhaler devices is based on guidance from the European Medicines Agency [Citation23], which is currently under review [Citation24], and on guidance from the Food and Drug Administration in the USA [Citation25]. Applicants are required to submit information about the drug substance, including its physicochemical characteristics, and the device, including manufacturing and quality assurance measures, uniformity of dosage, and particle size distribution [Citation25]. The k-haler contains the same ICS/LABA combination as the existing asthma maintenance combination treatment, flutiform pMDI. Within this formulation, FP offers rapid and sustained anti-inflammatory effects [Citation26,Citation27] and FORM is a fast-acting LABA [Citation28].
2.1. FP/FORM clinical data
An extensive clinical dataset exists for FP/FORM administered via a pMDI () [Citation29–Citation38]. Furthermore, long-term data from two clinical studies have demonstrated good efficacy, safety, and tolerability with this ICS/LABA combination, including a low rate of exacerbations, over study periods of up to 60 weeks [Citation33,Citation35]. Real-world data from non-interventional studies in over 4000 patients with asthma support the effectiveness and safety/tolerability of FP/FORM pMDIs in general clinical practice [Citation29,Citation37]. In addition, real-world data from a randomized pragmatic trial demonstrated that asthma control was maintained when the FP/FORM pMDI dose was stepped down from high to medium [Citation36]. Analyses indicate that the particle size characteristics of FP/FORM are well suited to the drug deposition requirements of ICS/LABA combinations, with a high fine-particle fraction that should help promote increased lung deposition with reduced oropharyngeal deposition [Citation39]. Consistent with the notion that FP/FORM acts throughout the airways, objective improvements in small airway ventilation heterogeneity (measured using multiple-breath nitrogen washout) have been demonstrated with FP/FORM in patients with normal spirometry characteristics but poor asthma control [Citation30]. Delivery of FP/FORM to the peripheral airways by pMDI and the rapid onset of action after inhalation were also shown to be favorable compared with other ICS/LABA formulations delivered by DPIs [Citation38]. The importance of small airways is increasingly recognized in the control of patients with asthma [Citation40]
Table 2. Summary of key clinical studies with FP/FORM pMDI in patients with asthma.
2.2. The k-haler: a modern BTI
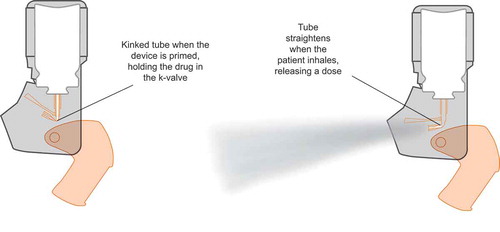
The k-haler is currently the only ICS/LABA BTI available in Europe. It includes the same formulation as flutiform pMDI, which has an extensive supporting dataset from clinical studies and real-life practice. Moreover, the k-haler’s innovative, award-winning design [Citation41] helps patients by obviating the shortcomings of both DPIs (the need for forceful inhalation) and pMDIs (the need to coordinate actuation during inhalation). Normal functioning of the k-haler BTI depends on innovative ‘kinked-hose’ technology, known as the ‘k-valve®’ (Mundipharma AG, Basel, Switzerland), in the core of the device (). When the mouthpiece cover is opened, drug is released into the k-valve, where it is retained because of the kinked shape of the tubing, similar to how a kink in a garden hose restricts the flow of water. When the patient inhales, the flow through the device causes an internal ‘flap’ to tilt, straightening the tubing of the k-valve and releasing the dose of drug as a spray or plume. There is no spring mechanism like that in the Autohaler, which as described previously ‘jolted’ on dose release, causing a small proportion of patients to stop their inhalation. A novel bung design was also conceived to accommodate variations in canister height and tolerance stack up from the various components in the device. This unique mechanism ensures that the canister stem is always depressed correctly.
The k-haler incorporates several key, user-friendly attributes () [Citation42,Citation43]. It is compact and has a classic pMDI shape that is familiar to patients. FP/FORM is a suspension and must therefore be shaken before being used. Once shaken, the operating procedure is a simple ‘open–inhale–close’ [Citation44]. Another key design element is its single-digit, front-facing, and color-coded dose counter () [Citation44]. This allows patients to see clearly how many doses are left in the inhaler, and the numbers on the counter are shown in a font designed by the UK Royal National Institute for Blind People for maximum legibility [Citation43]. The k-haler initially contains 124 actuations; the first four are used to prime the device. A red bar appears in the dose counter when fewer than 28 actuations, equivalent to 1 week’s use, remain in the inhaler. This serves as a reminder for the patient to request a replacement from their prescriber. The inhaler should not be used after the dose indicator reads ‘0ʹ or is completely red [Citation44]. As with any inhaled therapy, correct use of the device is essential for successful treatment. The patient should be shown how to use the inhaler correctly by a physician or other health-care professional (HCP) [Citation44], including the procedure for priming it for first use and dose administration thereafter.
Table 3. Key attributes and benefits of the k-haler [Citation44].
3. FP/FORM k-haler – in vitro and clinical data
The k-haler contains the same FP/FORM formulation in the same canister as the pMDI, providing 120 actuations after priming and delivering either 50/5 μg FP/FORM or 125/5 μg FP/FORM per metered dose (for adults and adolescents aged ≥12 years) [Citation44]. Clinical development studies were undertaken to compare delivery of FP/FORM via the k-haler with that from the pMDI when used correctly.
3.1. Pharmacokinetic and pharmacodynamic studies
Two studies were conducted to investigate the pulmonary bioavailability [Citation46] and systemic bioavailability [Citation47] of FP/FORM delivered by the k-haler.
3.1.1. Pulmonary bioavailability
Pulmonary bioavailability was assessed in a single-dose, randomized, three-arm, open-label, crossover study in 47 healthy adults. The study compared uptake of FP/FORM delivered by the k-haler with that from a pMDI with and without a spacer ()) [Citation46]. Participants received a charcoal block so that drug levels in plasma represented lung rather than gastrointestinal uptake associated with the devices. The study met its primary objective, showing that pulmonary bioavailability of FORM with the k-haler was comparable to that achieved with the pMDI device with a spacer (). Based on this demonstration of equivalence, efficacy data previously reported for FP/FORM delivered with the pMDI can reasonably be extrapolated to delivery of FP/FORM with the k-haler.
Figure 2. Pharmacokinetic and pharmacodynamic study designs. (a) FP/FORM k-haler® pulmonary bioavailability study [Citation46]. (b) FP/FORM k-haler systemic bioavailability study [Citation47]. (c) FORM k-haler pharmacodynamic study [Citation47].
aAeroChamber Plus® spacer (Trudell Medical International, Nottingham, UK). (a) and (b) were single-dose, randomized, open-label, three-treatment, three-period, crossover studies with a 7-day washout between treatment periods. All treatments were two puffs of FP/FORM 125/5 μg (total dose 250/10 μg). In total, 24 blood samples were taken per treatment period, at pre-dose and up to 36 h post-dose. Pharmacokinetic parameters determined were the area under the plasma concentration–time curve from the time of dosing to the last measurable concentration (AUCt) and the maximum observed plasma concentration (Cmax). In (a), all individuals ingested a charcoal suspension before each dose and 15 min and 1 h after each dose to ensure negligible gastrointestinal drug absorption. (c) was a single-dose, randomized, open-label, five-treatment, five-period, crossover study with a 7-day washout between treatment periods. Three treatments were 12 puffs of FP/FORM 125/5 μg (total dose, 1500/60 μg) via each of the three devices, one treatment was four puffs of FP/FORM 125/5 μg (total dose, 500/20 μg) included to test the dose–response sensitivity of the pharmacodynamic assay, and one treatment was an exploratory formulation irrelevant to this pharmacodynamic investigation. The primary efficacy variable was serum potassium levels, assessed pre-dose and up to 6 h post-dose. FORM, formoterol fumarate; FP, fluticasone propionate; pMDI, pressurized metered-dose inhaler; R, randomization; V, visit.
![Figure 2. Pharmacokinetic and pharmacodynamic study designs. (a) FP/FORM k-haler® pulmonary bioavailability study [Citation46]. (b) FP/FORM k-haler systemic bioavailability study [Citation47]. (c) FORM k-haler pharmacodynamic study [Citation47].aAeroChamber Plus® spacer (Trudell Medical International, Nottingham, UK). (a) and (b) were single-dose, randomized, open-label, three-treatment, three-period, crossover studies with a 7-day washout between treatment periods. All treatments were two puffs of FP/FORM 125/5 μg (total dose 250/10 μg). In total, 24 blood samples were taken per treatment period, at pre-dose and up to 36 h post-dose. Pharmacokinetic parameters determined were the area under the plasma concentration–time curve from the time of dosing to the last measurable concentration (AUCt) and the maximum observed plasma concentration (Cmax). In (a), all individuals ingested a charcoal suspension before each dose and 15 min and 1 h after each dose to ensure negligible gastrointestinal drug absorption. (c) was a single-dose, randomized, open-label, five-treatment, five-period, crossover study with a 7-day washout between treatment periods. Three treatments were 12 puffs of FP/FORM 125/5 μg (total dose, 1500/60 μg) via each of the three devices, one treatment was four puffs of FP/FORM 125/5 μg (total dose, 500/20 μg) included to test the dose–response sensitivity of the pharmacodynamic assay, and one treatment was an exploratory formulation irrelevant to this pharmacodynamic investigation. The primary efficacy variable was serum potassium levels, assessed pre-dose and up to 6 h post-dose. FORM, formoterol fumarate; FP, fluticasone propionate; pMDI, pressurized metered-dose inhaler; R, randomization; V, visit.](/cms/asset/722ee5e7-9b5d-467b-9014-253acd4bca05/iedd_a_1689957_f0002_oc.jpg)
Table 4. Pharmacokinetic and pharmacodynamic study data.
3.1.2. Systemic bioavailability
Total systemic bioavailability of FP/FORM delivered by the k-haler was assessed in the first stage of a two-stage study in 48 healthy adults [Citation47]. Stage 1 had a similar design to that used to determine pulmonary bioavailability, although participants did not receive a charcoal block so both pulmonary and gastrointestinal uptake occurred ()). Following the European Medicines Agency requirements, stage 2 was only conducted if the stage 1 primary objective was not met. In stage 1, there were two primary comparisons: i) systemic FP exposure between the k-haler and the pMDI plus a spacer. For this comparison, systemic exposure to FP was no greater with the k-haler than with the pMDI plus a spacer; ii) systemic FORM exposure between the k-haler and the pMDI without a spacer. For this comparison, exposure to FORM was similar to the k-haler and the pMDI device (). However, the upper confidence limit for the maximum observed plasma concentration (Cmax) marginally exceeded the prespecified 125% threshold. Therefore, stage 2 of the study was undertaken to examine the pharmacodynamic effects of FORM.
Stage 2 of the systemic bioavailability study [Citation47] extended the basic design of stage 1 with a total of five dose groups (). The pharmacodynamic effects of FORM on serum potassium levels were examined when the drug was delivered using different devices. The primary endpoint was maximum reduction in serum potassium concentration at 4 h post-dose, and equivalence was achieved if the 95% CI of the ratio of the reduction in serum potassium concentration with the k-haler versus pMDI and versus pMDI plus a spacer was in the range 0.5–2.0.
The k-haler met the equivalence criteria compared with the pMDI with a spacer (ratio [95% CI]: 0.97 [0.73–1.28]) but not compared with the pMDI alone (ratio [95% CI]: 0.79 [0.43–1.46]). However, because the upper confidence limit was within the equivalence range, the effect of the k-haler on serum potassium levels was no greater than that seen with the pMDI. Taken together, the results of these studies demonstrate that delivery of FP/FORM to the lungs was as efficient with the k-haler as it was with the pMDI without a spacer, and led to systemic exposure similar to that observed with the pMDI either with or without a spacer.
3.2. In vitro characteristics and pulmonary drug deposition
Inhaled drug efficacy is dependent on adequate pulmonary drug deposition. As the FP/FORM k-haler contains the same canister as the FP/FORM pMDI, it was expected that the fine-particle fraction, which correlates well with total lung deposition, would be similar. This was confirmed in a study carried out by Kappeler and colleagues, which showed a high fine-particle fraction of 38% and 39% of the delivered dose of FP and FORM, respectively [Citation48], compared with 40% for each component with the pMDI [Citation49]. However, plume force from aerosol inhalers may also affect drug delivery to the lungs, with fast forceful plumes increasing impaction at the back of the throat and reducing the amount available for delivery to the lungs. Throat impact force and plume temperature have been associated with ‘cold freon effect’ (sudden interruption of inhalation when the aerosol reaches the pharynx), which can also result in reduced drug delivery to the lungs. Newer pMDIs usually generate softer and warmer aerosols than older devices, which is likely to reduce the ‘cold freon effect’ [Citation50]. Previously, it had been shown that the FP/FORM pMDI has a favorable lower plume force than the Seretide pMDI, but it was not known if this would be true when the spray passed through the k-valve. An initial study, therefore, evaluated the in vitro plume force characteristics of the FP/FORM BTI; a second study then examined the in vivo pulmonary deposition of FP/FORM delivered by the k-haler.
3.2.1. In vitro plume force study
The plume force of the FP/FORM k-haler (125/5 μg) was compared with that of Seretide and Sirdupla® (Mylan EMEA, Saint Priest, France) pMDIs (both FP/salmeterol xinafoate [SAL]; 125/25 μg) in vitro [Citation51]. The typical distance between an inhaler and the back of the throat is 60–95 mm in adults, so plume force was measured at multiple distances up to 95 mm using a plastic disk target attached to a sensitive load cell, connected to a force tester. The FP/FORM k-haler had a less forceful plume than either of the pMDI devices, notably in the range 60–90 mm, within which the k-haler was approximately 70–87% less forceful than the other devices. The lower in vitro plume force of the k-haler may have the potential to reduce the impaction of the drug in the throat and, together with a high fine-particle fraction, may lead to improved drug delivery to the lungs. This was therefore examined in a subsequent scintigraphic study.
3.2.2. In vivo lung deposition study
In an in vivo study by Kappeler and colleagues, two-dimensional γ-scintigraphy was used to assess lung deposition of FP/FORM delivered by the k-haler in 12 patients with asthma (Global Initiative for Asthma step 2 or higher; FEV1, ≥60% and ≤90%) [Citation48]. Following training, participants inhaled a technetium-99 radiolabeled suspension of FP/FORM (two puffs × 125/5 µg FP/FORM) via the k-haler. In total, 44.7% of the delivered dose was deposited in the lung, equivalent to 43.0% of the metered dose. The mean penetration index (the ratio of peripheral to central lung deposition) with the k-haler was 0.31, demonstrating that FP and FORM were deposited in both central and peripheral regions of the lung (–), suggesting that FP/FORM delivered by the k-haler effectively reaches small-caliber bronchi [Citation48]. The 43.0% lung deposition, as a percentage of metered or nominal dose, of the FP/FORM k-haler compares well with that of other ICS/LABA inhalers in patients with asthma, with a higher deposition than that reported for the FP/SAL pMDI (14.7% of nominal dose) [Citation52], beclometasone dipropionate [BDP]/FORM pMDI (30.9% of nominal dose) [Citation53], and BDP/FORM NEXThaler® (Chiesi Farmaceutici, Parma, Italy) (40.3% of nominal dose) [Citation54]. Thus, the promising in vitro characteristics seem to translate to high levels of lung deposition. Indeed, Kappeler and colleagues argue that their findings challenge the view that the major determinant of pulmonary drug deposition is small particle size [Citation48]. Analysis of the FP/FORM pMDI reported a mass median aerodynamic diameter (MMAD) of 3.2–3.5 μm for the ICS and LABA components compared with 0.5–1.2 μm for both components of a BDP/FORM pMDI [Citation55]. Kappeler and colleagues therefore suggest that the high fine-particle fraction and favorable plume characteristics, which have been reported with both treatments, are more important determinants of high lung deposition than small particle size [Citation48].
Figure 3. Posterior scintigraphic images from a healthy individual (a), and from individuals with asthma (b) and chronic obstructive pulmonary disease (c), after administration of 99mTc-labeled fluticasone propionate/formoterol fumarate by a breath-triggered inhaler (k-haler®) [Citation48]. (‘Reprinted from Respiratory Medicine, Vol 138, Dominik Kappeler, Knut Sommerer, Claudius Kietzig, Bärbel Huber, Jo Woodward, Mark Lomax, Prashant Dalvi, Pulmonary deposition of fluticasone propionate/formoterol in healthy volunteers, asthmatics and COPD patients with a novel breath-triggered inhaler, with permission from Elsevier.’). Tc, technetium.
![Figure 3. Posterior scintigraphic images from a healthy individual (a), and from individuals with asthma (b) and chronic obstructive pulmonary disease (c), after administration of 99mTc-labeled fluticasone propionate/formoterol fumarate by a breath-triggered inhaler (k-haler®) [Citation48]. (‘Reprinted from Respiratory Medicine, Vol 138, Dominik Kappeler, Knut Sommerer, Claudius Kietzig, Bärbel Huber, Jo Woodward, Mark Lomax, Prashant Dalvi, Pulmonary deposition of fluticasone propionate/formoterol in healthy volunteers, asthmatics and COPD patients with a novel breath-triggered inhaler, with permission from Elsevier.’). Tc, technetium.](/cms/asset/cf9a4a48-157f-44d9-83a0-f09f80631fe9/iedd_a_1689957_f0003_oc.jpg)
3.3. Inspiratory force: flow and power
DPIs are passive devices and require a high inspiratory force to extract the drug from the device and to deagglomerate it from its powder carrier. Inspiratory force, or power, relates to the patient’s inhalation flow rate and the intrinsic resistance of the device [Citation56]. About a third of patients cannot or do not exert adequate inspiratory power when using DPI devices, and this is associated with poor asthma control and increased exacerbations [Citation10]. The k-haler is a low-resistance device [Citation48] designed to trigger at low inspiratory force and flow rates. Most DPIs do not have a threshold inspiratory force at which they are triggered. Therefore, drug is extracted from the device even when inspiratory flow is suboptimal. One exception, however, is the NEXThaler, which releases the drug only when a set threshold inspiratory force is reached.
A study was conducted to investigate the inspiratory flow rate and power required to trigger the NEXThaler DPI (extrafine BDP/FORM), the k-haler, and the Easi-Breathe BTI (Qvar® [BDP]) [Citation57]. The study used a novel laboratory test method based on an ‘airflow characterization rig’, driven by a switched vacuum pump and incorporating pressure sensors and mass flow sensors. Each device was triggered at relatively low flow rates of 20–40 L/min.
The inspiratory power required to trigger each device was calculated as the product of inhalation flow rate and the measured pressure drop. The inspiratory power required to trigger the NEXThaler was 8 times greater than that required to trigger the Easi-Breathe BTI and 5.5 times greater than that required to trigger the k-haler.
3.4. Patient use
Poor adherence to therapy contributes to the poor rates of asthma control in addition to incorrect inhaler use. Patient preference for a device and the ability to use it are important factors affecting adherence [Citation5,Citation58]. Inhaler ease of use is, therefore, an important factor that can contribute to asthma control. Two studies have investigated the ease of use of the k-haler device as assessed by the proportion of patients who could handle the inhaler correctly at different time points.
A randomized, open-label, observational, crossover study in 307 patients aged ≥12 years taking regular ICS/LABA therapy compared ease of use and patient preference for FP/FORM delivered by the k-haler versus a pMDI [Citation59]. Characteristics of patients enrolled were reviewed on an ongoing basis during the study to ensure the inclusion of individuals across different age and FEV1 status groups. Patient training included an initial step-by-step explanation and demonstration of how to handle their device, after which participants had a practice attempt using the inhaler that the trainer critiqued. All subsequent use of the device was assessed as correct or incorrect based on the criteria listed in . Over three-quarters (77%) of patients successfully used the k-haler and FP/FORM pMDI correctly at their first attempt after initial training (primary endpoint); this proportion increased to 93% with the k-haler after one or two attempts. In the first attempt, 87% patients using the k-haler performed all critical steps correctly (vs 82.4% with the pMDI), and 99% of patients using the k-haler were able to trigger the device. The proportion of elderly patients (>65 years) who handled both devices without any errors at first attempt was lower than those observed for the younger age groups (12–17 and 18–65 years); however, all age subgroups performed similarly following additional training for those who needed it. Irrespective of age or FEV1 status, almost all patients were able to perform all handling steps with the k-haler correctly at the final time point in the study (15 min). A post hoc analysis of the same study revealed that the majority of patients found the k-haler easier to use than ()) and preferable to ()) their current maintenance therapy inhaler [Citation59].
Figure 4. (a). Ease of use of and (b) patient preference for the fluticasone propionate/formoterol fumarate k-haler® compared with other inhalers. Reproduced with permission from Bell et al. [Citation59].
pMDI, pressurized metered-dose inhaler.
![Figure 4. (a). Ease of use of and (b) patient preference for the fluticasone propionate/formoterol fumarate k-haler® compared with other inhalers. Reproduced with permission from Bell et al. [Citation59].pMDI, pressurized metered-dose inhaler.](/cms/asset/e62a5f18-48ac-4917-aa11-a38319ea3513/iedd_a_1689957_f0004_oc.jpg)
Table 5. Criteria to assess correct handling of the k-haler® BTI and a comparator pMDI (reproduced with permission from Bell et al. [Citation59]).
Another study was undertaken to determine the proportions of patients who could correctly handle the k-haler BTI compared with the budesonide (BUD)/FORM (Symbicort) Turbohaler DPI [Citation60]. The study used a randomized, open-label, two-period, crossover, multicenter design and included patients with persistent asthma, chronic obstructive pulmonary disease, or asthma–chronic obstructive pulmonary disease overlap syndrome. A total of 369 adults were randomized and received FP/FORM k-haler or BUD/FORM DPI treatment twice daily for 12 weeks before crossing over to the other treatment arm. Patients were trained on device handling on the first day of each treatment period and were assessed on day 1 and after 12 weeks. The proportion of patients performing all critical steps correctly after 12 weeks (primary endpoint) was 94% for the k-haler BTI compared with 82% for the DPI (OR: 2.89; 95% CI: 1.57–5.33; p < 0.001). The proportion of patients performing all steps correctly was also greater with the k-haler than with the DPI (74% vs 62%; OR: 1.85; 95% CI: 1.30–2.62; p < 0.001). This finding is particularly notable given that the assessment was undertaken 12 weeks after training. Furthermore, on day 1, significantly more patients correctly performed all critical steps with the k-haler than with the DPI after reading the instructions for use (i.e. without training by a health-care professional [HCP]) (72.7% vs 36.1%, respectively; p< 0.001). In addition, a greater proportion of patients demonstrated correct inhaler technique with the k-haler than with the DPI (88.0% versus 81.6%, respectively; p < 0.05) after a single training round from their HCP. Therefore, less time may be needed to train patients to use the k-haler than the DPI, which may potentially lead to health-care cost savings with the k-haler over time. However, this needs to be formally tested.
These studies investigating device handling and patient use demonstrated that, with training, most patients could operate the k-haler correctly, found it easy to use, and preferred it to their current inhaler. This is important because ease of use, patient preference, and patient satisfaction have been associated with improved adherence to treatment [Citation59,Citation61]. Given the positive effects on ease of use and patient preference reported with the k-haler, future studies evaluating the impact of the k-haler on treatment adherence would be of interest. In addition, studies in specific patient populations, such as the elderly and those with severely impaired lung function, who may experience difficulties with particular inhaler devices, would also be informative.
3.5. Health economics and outcomes research
A cost–utility analysis using a Markov model simulation explored the societal and economic impact of the FP/FORM k-haler compared with DPIs (delivering BUD/FORM and FP/SAL) [Citation62]. The analysis assumed that all inhalers had the same drug efficacy, but that the k-haler lacked the critical handling error of insufficient inspiratory effort (relative risk data were derived from the results of the CRITIKAL study). The FP/FORM k-haler was more cost-effective than either BUD/FORM or FP/SAL; it was associated with direct cost savings of £98 and £142 per patient per year, with 0.0117 and 0.0169 additional quality-adjusted life-years, respectively. At a £20,000/quality-adjusted life-year threshold, the k-haler device had the highest probability (100%) of being cost-effective of all the inhalers investigated. As discussed above, the short training time required with the k-haler may result in additional cost savings compared with other devices. Future health economics studies to confirm this hypothesis are needed.
4. Patient training and support materials for the k-haler BTI
4.1. The need for adequate patient training and support
A lack of patient education about asthma or a lack of regular follow-up may be associated with poor inhaler technique [Citation2]; training in device handling from an HCP and follow-up checks of technique can significantly reduce the risk of critical errors [Citation5]. However, real-world evidence suggests that provision of training on inhaler technique remains inconsistent [Citation22,Citation63]. A survey revealed that only 18% of French general practitioners ‘always’ demonstrate inhaler technique to patients at the initial visit, with 34% ‘often’ demonstrating it; moreover, 12% and 42%, respectively, ‘always’ or ‘often’ checked handling during follow-up visits [Citation22]. Some patients with asthma never receive verbal instructions from an HCP [Citation9].
A study of patients in multiple therapy areas found that as few as half of them read the patient information leaflet (PIL) associated with their medication [Citation64]. This is a concern because the main device-operating instructions available to patients for ICS/LABA products are found in the PIL. Patient support materials should demonstrate the correct inhaler technique in an easy-to-follow and accessible format [Citation3,Citation65,Citation66]. Materials should be prepared in formats that have been shown to improve inhaler technique, such as training DVDs and web-based platforms [Citation66,Citation67].
4.2. Support materials for the k-haler
The k-haler is a simple to use BTI; however, all patients should be trained on any new device regardless of its ease of use, and some individuals will require more training than others or need reminding of the correct technique. Hence, it is important to cater for all types of patients and consider their learning styles and needs. A wide range of informative packaging and innovative web-based tools (interactive training tool, training video, access to the PIL) are available to support individuals using the FP/FORM k-haler device; a link to the patient web-based tool is also provided in the PIL [Citation68]. Clear, informative diagrams are presented in the PIL and on the flaps of the box to maximize exposure to operating instructions (). These diagrams were developed based on guidance obtained from iterative, qualitative patient research to ensure that the information provided was clear and useful. Patients were consulted throughout the design, development, and testing of these materials, and the range of formats in which information can be accessed from the web-based PIL and packaging should help to accommodate the different learning styles and preferences of users [Citation69]. As a result, the k-haler was awarded an international design award for its innovative packaging [Citation69].
Figure 5. Guidance for preparing and for using the fluticasone propionate/formoterol fumarate k-haler® on the packaging.

A training device, the ‘k-trainer®’ (Clement Clarke International, Harlow, UK), which is the same size and shape as the k-haler but contains no active drug, has been produced to support patient education from HCPs. It has been designed to provide audible feedback for key device-operational steps to reinforce the correct use of the device (shaking [ball bearing rattle], opening [click], inhaling [whistle], and closing [click]). A k-trainer app is also being developed for additional support on k-haler technique training. These materials should help to support the effective use of the FP/FORM k-haler in addition to the user-friendly mechanism.
5. Trade mark statements
FLUTIFORM® is a registered trade mark of Jagotec AG and is used under license.
K-HALER®, K-VALVE®, and K-TRAINER® are registered trade marks of Mundipharma AG or Clinical Designs Ltd.
DISKUS®, EVOHALER®, and SERETIDE® are registered trade marks of Glaxo Group Limited.
NEXTHALER® and FOSTAIR® are registered trade marks of Chiesi Farmaceutici S.p.A.
SIRDUPLA® is a registered trade mark of Mylan EMEA SAS.
SYMBICORT® and TURBOHALER® are registered trade marks of AstraZeneca AB.
EASI-BREATHE® is a registered trade mark of Norton Healthcare Limited.
QVAR® is a registered trade mark of Teva Pharmaceuticals International GmbH
AUTOHALER® is a registered trade mark of 3M Company.
AEROCHAMBER® and AEROCHAMBER PLUS® are registered trade marks of Trudell Medical International.
6. Clinical relevance
There is an unmet need for easy-to-use asthma inhalation devices that do not require coordination of actuation and inhalation, such as pMDIs, or a high inspiratory force, such as many DPIs; these two inhaler errors are associated with poor asthma control [Citation1–Citation5,Citation7]. BTIs obviate these two errors, and clinical data (including real-world evidence) have shown improved asthma control with BTIs compared with other device formats [Citation22]. The FP/FORM k-haler is simple to use and innovative, and is currently the only BTI containing an ICS/LABA available in Europe. The FP/FORM k-haler therefore has the potential to improve real-world asthma control for some patients requiring an ICS/LABA who may have struggled to operate other device types.
Patients’ attitudes toward their inhalers are also important, and there is evidence of an association between negative views of inhalers and poor asthma control. Data from the recognize Asthma and LInk to Symptoms and Experience (REALISE) survey of asthma control and management in 8000 European patients indicate that proportionally more individuals with uncontrolled asthma than with controlled or partly controlled asthma found it difficult to use their inhaler, but they also felt that it was a nuisance and were embarrassed to carry it with them and to use it in front of other people [Citation70]. Accordingly, the k-haler BTI has been developed as a patient-focused device. There was extensive patient involvement in the preparation of support materials for the device, and results of studies of patient preference and ease of handling have indicated that users’ attitudes toward it are generally positive [Citation59].
7. Conclusion
The FP/FORM k-haler is the only BTI offering an ICS/LABA combination in Europe. In addition to the existing, extensive clinical dataset for the same ICS/LABA combination administered using a pMDI, data support for the k-haler is growing and includes information on drug delivery to the lungs, device handling, and health economics and outcomes. As well as having many user-friendly features, the FP/FORM k-haler is supported by a range of materials to enable patients to use the device effectively.
8. Expert opinion
It is well documented that inhaler errors are common with all device types. This results in suboptimal inhaler use and has been associated with poor asthma control and an increased risk of exacerbations. Until recently, however, there was a scarcity of information on critical device-specific errors and their effect on outcomes. The CRITIKAL study addressed this gap and identified different critical errors for DPIs and pMDIs. The most common critical error with DPIs (seen in up to 38% of users) was an insufficient inspiratory effort, which was associated with uncontrolled asthma and an increased exacerbation rate. In parallel, the most common critical error with pMDIs (seen in ~25% of users) was actuation before inhalation, which was also associated with uncontrolled asthma [Citation10].
Information on device-specific critical errors is important because it can inform the development of new devices to help users avoid them. BTIs are an example of devices designed to overcome these key DPI and pMDI errors (actuation before inhalation error seen with pMDIs and the insufficient respiratory effort observed with DPIs). While BTIs for the delivery of inhaled ICS have been available for many years, until 2018, when the k-haler was approved for use, no BTIs delivering an ICS/LABA FDC were available in Europe. Results of short-term clinical trials with the k-haler suggest that it is easier for patients to achieve and maintain correct inhaler technique with this device than with DPIs or pMDIs [Citation59,Citation60]. However, long-term outcomes based on real-world data in a broader asthma population should be investigated to confirm these findings.
In addition, research into device-specific critical errors can also inform device choice, which can be tailored to patients’ needs and preferences. This has the potential to reduce key critical errors made by patients further, resulting in improved inhaler technique while improving adherence to treatment, which may ultimately increase asthma control without the need for escalating therapy. Therefore, this research could be instrumental in achieving the ultimate goal of improved patient outcomes and reduced exacerbations with minimal effective therapy, as a result of fewer errors made in real-life device use.
Nonetheless, several barriers to achieving this goal remain. One barrier is suboptimal awareness by HCPs of the critical errors associated with each inhaler type as well as limited ability to identify patients who are not using their inhaler correctly. Training HCPs to recognize device-specific critical errors and incorrect device use is important to enable the tailoring of inhaler choice to specific patient needs. Another barrier is the variable quality of patient training available on how to use inhalers correctly and a lack of regular monitoring of correct use over time as part of routine clinical practice. Limited availability of informative and accessible training support materials to suit different patient learning styles and needs is also a barrier.
In coming years, we are likely to see the greater use of real-world studies to complement clinical trial data on how critical errors affect outcomes in clinical practice. In addition, it is likely that greater emphasis will be placed on phenotyping patients to identify optimal treatment options based on individual characteristics, which would further facilitate the tailoring of device choice to specific needs.
Inhaler devices will continue to evolve in line with new developments in telemedicine and mobile health. Connected devices, including inhalers, wearable sensors, and mobile phone apps, are increasingly available. These devices can track, monitor, and prompt medication use, providing valuable information to patients and HCPs, and empowering individuals to manage their disease. These connected devices have huge potential as a new way to deliver asthma care, facilitating closer monitoring than can be achieved currently through infrequent face-to-face asthma reviews. In the future, e-inhalers that provide optimal drug delivery and ease of use while monitoring adherence to treatment and correct use may be widely available. Nonetheless, tailoring inhaler type and treatment to individual patient needs will remain important.
Backing these trends, current research areas of interest include prospective determination of how device choice affects treatment effectiveness, particularly in clinical practice; further improvement of inhaler devices to minimize critical errors; assessment of how patient-related factors may influence treatment success with different inhaler types; optimization of educational approaches to device use; development of support platforms for connected inhalers; and continuing exploration of the role of mobile health in the management of patients with asthma.
Article highlights
The effectiveness of inhaled asthma therapy depends on the efficiency and reliability of drug delivery to the lungs.
Asthma is poorly controlled in many individuals, a large proportion of whom are unable to use their inhaler correctly.
Breath-triggered inhalers may help to reduce critical usage errors because they do not require the forceful inhalation needed with dry powder inhalers or the coordination of actuation and inhalation required with pressurized metered-dose inhalers.
The flutiform® (fluticasone propionate/formoterol fumarate [FP/FORM]) k-haler® is the first inhaled corticosteroid/long-acting β2-agonist fixed-dose combination available in a breath-triggered inhaler approved for the regular treatment of asthma in Europe.
The clinical study set for the FP/FORM k-haler includes data on drug delivery to the lungs, systemic exposure, device handling and preference, and health economics and outcomes.
A range of support materials is available to help patients learn and maintain the correct technique with the FP/FORM k-haler.
This box summarizes key points contained in the article.
Declaration of interest
OS Usmani and/or his department has received research grants, unrestricted educational grants, and/or fees for lectures and advisory board meetings from Aerocrine, AstraZeneca, Boehringer Ingelheim, Chiesi, Cipla, Edmond Pharma, GlaxoSmithKline, Napp, Mundipharma International, Prosonix, Sandoz, Takeda, Zentiva. N Roche reports grants and personal fees from Boehringer Ingelheim, Novartis, Pfizer and personal feed from Teva, GlaxoSmithKline, AstraZeneca, Chiesi, Mundipharma, Cipla, Sanofi, Sandoz, 3M, Trudell, Zambon. J Marshall and H Danagher report being an employee of Mundibiopharma Ltd., at the time of writing. D Price is a board member with Amgen, AstraZeneca, Boehringer Ingelheim, Chiesi, Circassia, Mylan, Mundipharma Ltd., Napp, Novartis, Regeneron Pharmaceuticals, Sanofi Genzyme, Teva Pharmaceuticals; consultancy agreements with Amgen, AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Mylan, Mundipharma Ltd., Napp, Novartis, Pfizer, Teva Pharmaceuticals, Threvance; grants and unrestricted funding for investigator-initiated studies (conducted through Observational and Pragmatic Research Institute Pte Ltd.) from AKL Research and Development Ltd., AstraZeneca, Boehringer Ingelheim, British Lung Foundation, Chiesi, Circassia, Mylan, Mundipharma Ltd., Napp, Novartis, Pfizer, Regeneron Pharmaceuticals, Respiratory Effectiveness Group, Sanofi Genzyme, Teva Pharmaceuticals, Theravance, UK National Health Service, Zentiva (Sanofi Generics); payment for lectures/speaking engagements from AstraZeneca, Boehringer Ingelheim, Chiesi, Cipla, GlaxoSmithKline, Kyorin, Mylan, Merck, Munipharma Ltd., Novartis, Pfizer, Regeneron Pharmaceuticals, Sanofi Genzyme, Teva Pharmaceuticals; payment for manuscript preparation from Mundipharma Ltd., Teva Pharmaceuticals; payment for the development of educational materials from Mundipharma, Novartis; payment for travel/accommodation/meeting expenses from AstraZeneca, Boehringer Ingelheim, Circassia, Mundipharma Ltd., Napp, Novartis, Teva Pharmaceuticals; funding for patient enrollment or completion of research from Chiesi, Novartis, Teva Pharmaceuticals, Zentiva (Sanofi Generics); stock/stock options from AKL Research and Development Ltd, which produces phytopharmaceuticals; owns 74% of the social enterprise Optimum Patient Care Ltd (Australia and UK) and 74% of Observational and Pragmatic Research Institute Pte Ltd (Singapore); and is a peer reviewer for grant committees of the Efficacy and Mechanism Evaluation program, and Health Technology Assessment.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Acknowledgments
Medical writing support was provided by Oxford PharmaGenesis Ltd.
Additional information
Funding
References
- Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention; 2018. [cited 2019 Nov]. Available from: https://ginasthma.org/reports/
- Al-Jahdali H, Ahmed A, Al-Harbi A, et al. Improper inhaler technique is associated with poor asthma control and frequent emergency department visits. Allergy Asthma Clin Immunol. 2013;9(1):8.
- Giraud V, Allaert FA, Roche N. Inhaler technique and asthma: feasability and acceptability of training by pharmacists. Respir Med. 2011;105(12):1815–1822.
- Maricoto T, Rodrigues LV, Teixeira G, et al. Assessment of inhalation technique in clinical and functional control of asthma and chronic obstructive pulmonary disease. Acta Med Port. 2015;28(6):702–707.
- Melani AS, Bonavia M, Cilenti V, et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir Med. 2011;105(6):930–938.
- Usmani OS, Lavorini F, Marshall J, et al. Critical inhaler errors in asthma and COPD: a systematic review of impact on health outcomes. Respir Res. 2018;19(1):10.
- Vincken W, Levy ML, Scullion J, et al. Spacer devices for inhaled therapy: why use them, and how? ERJ Open Res. 2018;4(2):00065–2018.
- Guilbert TW, Colice G, Grigg J, et al. Real-life outcomes for patients with asthma prescribed spacers for use with either extrafine- or fine-particle inhaled corticosteroids. J Allergy Clin Immunol Pract. 2017;5(4):1040–1049.
- Lavorini F, Magnan A, Dubus JC, et al. Effect of incorrect use of dry powder inhalers on management of patients with asthma and COPD. Respir Med. 2008;102(4):593–604.
- Price DB, Roman-Rodriguez M, McQueen RB, et al. Inhaler errors in the CRITIKAL study: type, frequency, and association with asthma outcomes. J Allergy Clin Immunol Pract. 2017;5(4):1071–1081 e1079.
- Stein SW, Thiel CG. The history of therapeutic aerosols: a chronological review. J Aerosol Med Pulm Drug Deliv. 2017;30(1):20–41.
- Ruggins NR, Milner AD, Swarbrick A. An assessment of a new breath actuated inhaler device in acutely wheezy children. Arch Dis Child. 1993;68(4):477–480.
- Chapman KR, Love L, Brubaker H. A comparison of breath-actuated and conventional metered-dose inhaler inhalation techniques in elderly subjects. Chest. 1993;104(5):1332–1337.
- Price DB, Pearce L, Powell SR, et al. Handling and acceptability of the Easi-Breathe device compared with a conventional metered dose inhaler by patients and practice nurses. Int J Clin Pract. 1999;53(1):31–36.
- Lenney J, Innes JA, Crompton GK. Inappropriate inhaler use: assessment of use and patient preference of seven inhalation devices. EDICI Respir Med. 2000;94(5):496–500.
- Newman SP, Weisz AW, Talaee N, et al. Improvement of drug delivery with a breath actuated pressurised aerosol for patients with poor inhaler technique. Thorax. 1991;46(10):712–716.
- Price D, Thomas V, von Ziegenweidt J, et al. Switching patients from other inhaled corticosteroid devices to the Easyhaler®: historical, matched-cohort study of real-life asthma patients. J Asthma Allergy. 2014;7:31–51.
- Price D, Haughney J, Sims E, et al. Effectiveness of inhaler types for real-world asthma management: retrospective observational study using the GPRD. J Asthma Allergy. 2011;4:37–47.
- Kemp L, Haughney J, Barnes N, et al. Cost-effectiveness analysis of corticosteroid inhaler devices in primary care asthma management: a real world observational study. Clinicoecon Outcomes Res. 2010;2:75–85.
- Price D, Thomas M, Mitchell G, et al. Improvement of asthma control with a breath-actuated pressurised metred dose inhaler (BAI): a prescribing claims study of 5556 patients using a traditional pressurised metred dose inhaler (MDI) or a breath-actuated device. Respir Med. 2003;97(1):12–19.
- Diggory P, Bailey R, Vallon A. Effectiveness of inhaled bronchodilator delivery systems for elderly patients. Age Ageing. 1991;20(5):379–382.
- Giraud V, Allaert FA. Improved asthma control with breath-actuated pressurized metered dose inhaler (pMDI): the SYSTER survey. Eur Rev Med Pharmacol Sci. 2009;13(5):323–330.
- Agency EM. Guideline on the pharmaceutical quality of inhalation and nasal products; 2006; [cited 2018 Nov]. Available from: https://www.ema.europa.eu/documents/scientific-guideline/guideline-pharmaceutical-quality-inhalation-nasal-products_en.pdf
- Agency EM. Concept paper on revision of the guideline on the pharmaceutical quality of inhalation and nasal products. 2017; [cited 2018 Nov]. Available from: https://www.ema.europa.eu/documents/scientific-guideline/concept-paper-revision-guideline-pharmaceutical-quality-inhalation-nasal-products_en.pdf.
- Administration FaD. Metered Dose Inhaler (MDI) and Dry Powder Inhaler (DPI) Products – quality considerations – guidance for industry. 2018; [cited 2018 Nov 07]. Available from: https://www.fda.gov/downloads/drugs/guidances/ucm070573.pdf
- Ketchell RI, Jensen MW, Lumley P, et al. Rapid effect of inhaled fluticasone propionate on airway responsiveness to adenosine 5ʹ-monophosphate in mild asthma. J Allergy Clin Immunol. 2002;110(4):603–606.
- Luijk B, Kempsford RD, Wright AM, et al. Duration of effect of single-dose inhaled fluticasone propionate on AMP-induced bronchoconstriction. Eur Respir J. 2004;23(4):559–564.
- Politiek MJ, Boorsma M, Aalbers R. Comparison of formoterol, salbutamol and salmeterol in methacholine-induced severe bronchoconstriction. Eur Respir J. 1999;13(5):988–992.
- Backer V, Ellery A, Borzova S, et al. Non-interventional study of the safety and effectiveness of fluticasone propionate/formoterol fumarate in real-world asthma management. Ther Adv Respir Dis. 2018;12:1753466618796987.
- Dame Carroll JR, Bertolin AI, Farrow CE, et al. High fine particle fraction combination therapy improves symptoms and small airway function in poorly controlled asthma. Am J Crit Care Med. 2015;191:A5034. Abstract.
- Dunlop W, Heron L, Fox G, et al. Budget impact analysis of a fixed-dose combination of fluticasone propionate and formoterol fumarate (FP/FORM) in a pressurized metered-dose inhaler (pMDI) for asthma. Adv Ther. 2013;30(10):933–944.
- Farrington E, Saunders A, Heron L, et al. FP/FORM versus FP/SAL within clinical practice: an updated budget impact analysis in asthma. Adv Ther. 2016;33(5):794–806.
- Mansur AH, Kaiser K. Long-term safety and efficacy of fluticasone/formoterol combination therapy in asthma. J Aerosol Med Pulm Drug Deliv. 2013;26(4):190–199.
- Martínez-Moragón E, Delgado J, Ojeda P, et al. Economic evaluation of fluticasone propionate/formoterol fumarate (Flutiform®) vs fluticasone/salmeterol and budesonide/formoterol in Spain. Value Health. 2015;18:A501.
- Papi A, Mansur AH, Pertseva T, et al. Long-term fluticasone propionate/formoterol fumarate combination therapy is associated with a low incidence of severe asthma exacerbations. J Aerosol Med Pulm Drug Deliv. 2016;29(4):346–361.
- Usmani OS, Kemppinen A, Gardener E, et al. A randomized pragmatic trial of changing to and stepping down fluticasone/formoterol in asthma. J Allergy Clin Immunol Pract. 2017;5(5):1378–1387 e1375.
- Schmidt O, Petro W, Hoheisel G, et al. Real-life effectiveness of asthma treatment with a fixed-dose fluticasone/formoterol pressurised metered-dose inhaler – results from a non-interventional study. Respir Med. 2017;131:166–174.
- Ohbayashi H, Kudo S, Ariga M. Evaluation of rapid onset of action of ICS/LABA combination therapies on respiratory function in asthma patients: a single-center, open-label, randomized, crossover trial. Pulm Ther. 2018;4(2):159–169.
- Dissanayake S, Grothe B, Kaiser K. Fluticasone/formoterol: a new single-aerosol combination therapy for patients with asthma. Respir Med. 2012;106(Suppl 1):S20–28.
- Usmani OS, Singh D, Spinola M, et al. The prevalence of small airways disease in adult asthma: a systematic literature review. Respir Med. 2016;116:19–27.
- Napp Pharmaceuticals Limited. Novel asthma device, k-haler®, celebrates two A’ design award & competition wins. 2016: Press release; [cited 2019 Jun]. Available from: http://napp.co.uk/archives/secondary_news/novel-asthma-device-k-haler-celebrates-two-design-award-competition-wins
- Napp Pharmaceuticals Ltd. flutiform summary of product characteristics; 2018; [cited 2019 Apr 5]. Available from: https://www.medicines.org.uk/emc/medicine/26954
- Brandt C RNIB’s free Tiresias font makes text easier to read for the partially sighted 2013 [cited 2018 Jun 22]. Available from: https://www.digitalartsonline.co.uk/news/typography/rnibs-tiresias-font-makes-text-easier-read-for-partially-sighted/
- Napp Pharmaceuticals Limited. flutiform k-haler (50/5μg and 125/5μg): summary of product charactertistics; 2017.
- Lee HY, Kang JY, Yoon HK, et al. Clinical characteristics of asthma combined with COPD feature. Yonsei Med J. 2014;55(4):980–986.
- Bell D, Mundin G, Lomax M, et al. Relative pulmonary bioavailability (BA) of fluticasone propionate/formoterol (FP/FORM) via pressurised metered-dose inhaler (pMDI) and a novel breath triggered inhaler (BTI). Eur Respir J. 2017;50(suppl 61):PA523.
- Bell D, Mundin G, Lomax M, et al. Systemic bioavailability (BA) and pharmacodynamics (PD) of fluticasone propionate/formoterol (FP/FORM) via pressurised metered-dose inhaler (pMDI) or a novel breath-triggered inhaler (BTI). Eur Respir J. 2017;50(suppl 61):PA3950.
- Kappeler D, Sommerer K, Kietzig C, et al. Pulmonary deposition of fluticasone propionate/formoterol in healthy volunteers, asthmatics and COPD patients with a novel breath-triggered inhaler. Respir Med. 2018;138:107–114.
- Johal B, Howald M, Fischer M, et al. Comparison of the fine particle fraction of fluticasone propionate/formoterol fumarate combination with other combination products. Eur Respir J. 2012;40(Suppl 56):A4865.
- Scichilone N, Rossi A, Melani A. Revising old principles of inhaled treatment in new fixed combinations for asthma. Pulm Pharmacol Ther. 2015;33:32–38.
- Tuohy J, Marshall J, Danagher H. Plume spray force of three HFA-propelled ICS/LABA combination inhalers. Eur Respir J. 2017;50(suppl 61):PA524.
- Leach CL, Kuehl PJ, Chand R, et al. Characterization of respiratory deposition of fluticasone-salmeterol hydrofluoroalkane-134a and hydrofluoroalkane-134a beclomethasone in asthmatic patients. Ann Allergy Asthma Immunol. 2012;108(3):195–200.
- De Backer W, Devolder A, Poli G, et al. Lung deposition of BDP/formoterol HFA pMDI in healthy volunteers, asthmatic, and COPD patients. J Aerosol Med Pulm Drug Deliv. 2010;23(3):137–148.
- Virchow J, Poli G, Herpich C, et al. Lung deposition of the dry powder fixed combination beclometasone dipropionate plus formoterol fumarate using NEXThaler® device in healthy subjects, asthmatic patients, and COPD patients. J Aerosol Med Pulm Drug Deliv. 2018;31(5):269–280.
- Johal B, Howald M, Fischer M, et al. Fine particle profile of fluticasone propionate/formoterol fumarate versus other combination products: the DIFFUSE study. Comb Prod Ther. 2013;3(1–2):39–51.
- Dal Negro RW. Dry powder inhalers and the right things to remember: a concept review. Multidiscip Respir Med. 2015;10(1):13.
- Espeso BJ, Rhima C, Tibbatts J, et al. A Study on the Inspiratory Flow Rate and Power Required to Trigger flutiform® k-haler®, Qvar® Easi-Breathe® and Fostair® NEXThaler® Breath Actuated Inhalers; 2018. RDD; Tucson, Arizona, 22-26 April.
- Small M, Anderson P, Vickers A, et al. Importance of inhaler-device satisfaction in asthma treatment: real-world observations of physician-observed compliance and clinical/patient-reported outcomes. Adv Ther. 2011;28(3):202–212.
- Bell D, Mansfield L, Lomax M, et al. Crossover trial evaluating patient handling, preference, and ease of use of the fluticasone propionate/formoterol breath-triggered inhaler. J Aerosol Med Pulm Drug Deliv. 2017;30(6):425–434.
- Bell D, Timmer W, Mansfield L, et al. Patients’ ability to use a novel fluticasone propionate/formoterol breath-triggered inhaler (BTI) vs. budesonide/formoterol dry powder inhaler (DPI); 2018. Abstract #9732 presented at ERS International Congress, 15–19 September 2018; Paris, France.
- Price D, Harrow B, Small M, et al. Establishing the relationship of inhaler satisfaction, treatment adherence, and patient outcomes: a prospective, real-world, cross-sectional survey of US adult asthma patients and physicians. World Allergy Organ J. 2015;8(1):26.
- Forster R, Ratcliffe A, Crossley A, et al. Cost-utility analysis of a novel breath-triggered aerosol inhaler which has been designed to reduce the critical handling error of insufficient inspiratory effort. Value Health. 2017;20:A586.
- Molimard M, Raherison C, Lignot S, et al. Assessment of handling of inhaler devices in real life: an observational study in 3811 patients in primary care. J Aerosol Med. 2003;16(3):249–254.
- Vinker S, Eliyahu V, Yaphe J. The effect of drug information leaflets on patient behavior. Isr Med Assoc J. 2007;9(5):383–386.
- Basheti IA, Obeidat NM, Reddel HK. Effect of novel inhaler technique reminder labels on the retention of inhaler technique skills in asthma: a single-blind randomized controlled trial. NPJ Prim Care Respir Med. 2017;27(1):9.
- Takita K, Kondo R, Horiguchi T. Effectiveness of training patients using DVD in the accurate use of inhalers for the treatment of bronchial asthma. Allergol Int. 2017;66(4):545–549.
- Muller T, Muller A, Hubel C, et al. Optimizing inhalation technique using web-based videos in obstructive lung diseases. Respir Med. 2017;129:140–144.
- AG M. Flutiform® K-haler® Patient Information Leaflet; [cited 2018 Oct]. Available from: https://www.medicines.org.uk/emc/files/pil.9412.pdf
- Napp Pharmaceuticals Limited. Mundipharma’s novel device, k haler®, recognised for innovative packaging by iF DESIGN AWARDS. 2018: press release; 2018; [cited 2019 Jun]. Available from: https://www.mundipharma.com/wp-content/uploads/2018/2002/k-haler-iF-Design-Award-press-release.pdf
- Price D, Fletcher M, van der Molen T. Asthma control and management in 8,000 European patients: the REcognise asthma and link to symptoms and experience (REALISE) survey. NPJ Prim Care Respir Med. 2014;24:14009.