ABSTRACT
Background
Self-injected biologic therapies have gained significant prevalence across numerous therapeutic areas. A lack of specific guidance on best practices may lead to inadequate biologic initiation and training. We previously conducted a small-sample, qualitative analysis designed to identify gaps in self-injection training.
Methods
A total of 277 HCPs performing routine biologic initiation and 264 patients currently self-injecting biologics completed this quantitative study remotely using an online survey. The primary objective was to validate previous qualitative findings and firmly characterize the current paradigm. As an exploratory objective, the study examined associations that may exist between training experiences and patient-reported outcomes.
Results
Most patients (91.7%) reported receiving formal self-injection training, commonly conducted over one or two sessions. The mean overall training time reported was 37.8 and 30.4 minutes by patients and HCPs, respectively. Over one-third of patients reported lacking confidence that they could correctly self-inject during the first 6 months of treatment.
Conclusion
Current training practices may not be adequate to prepare patients to start their therapies. Considerable attention must be paid to providing patients with multiple opportunities for training sessions, training devices, and medical information for home access. Further studies should prospectively examine the impact of training techniques on patient-reported outcomes.
1. Introduction
1.1. Treatment burden
Although once scarce and innovative treatments, biologic therapies have gained significant prevalence across numerous therapeutic areas, most notably chronic immune-mediated diseases and oncology [Citation1]. While highly effective, biologic treatments must currently be delivered parenterally (i.e. by injection or infusion) and may therefore require a higher burden of treatment relative to more conventional oral medications. Burden of treatment, defined as the workload of healthcare and its effect on patient functioning and wellbeing, has become an increasingly important factor in the management of chronic disease [Citation2,Citation3].
In an effort to decrease burden of treatment, pharmaceutical companies have developed self-injectable biologic therapies to allow patients to avoid in-clinic infusions [Citation4,Citation5]. However, even with more convenient delivery methods, injectable medications may still pose significant burden of treatment. In one large cohort study of patients with a variety of chronic diseases, including those that are likely treated with biologics, an estimated 40% of patients viewed their burden of treatment as unsustainable [Citation6].
1.2. Self-Injection training
Effective self-injection therapy depends on patients performing their injections accurately and confidently giving rise to focus on proper self-injection training [Citation7]. Most self-injection product labels require that patients initially use injection devices under the supervision of a healthcare provider (HCP), who is then expected to instruct on appropriate injection technique and determine whether patients are suitable (willing and able) to self-inject [Citation8,Citation9]. While research on adherence to these training requirements is limited, available studies from both HCP and patient perspectives suggest that no self-injection training is provided in approximately 40% of instances [Citation10,Citation11].
When training is provided, the outcomes may still be variable, as the requirements for instruction found within product prescribing information do not offer specific guidance on best practice or what constitutes adequate training [Citation11,Citation12]. As a result, HCPs must create their own interpretation of how to train on device use, despite receiving minimal biologic-specific training themselves [Citation12]. Inconsistencies in injection training can create wide variability in patients’ experiences onboarding to self-injection therapy, which could have implications for medication adherence and persistence [Citation12,Citation13]. Training variability may have also been exacerbated by the current COVID-19 pandemic, as many in-person training sessions have likely shifted to virtual visits given the high reliance on telemedicine [Citation14].
In the absence of consistent in-office injection training, patients may seek out supplemental resources, including videos made available on the internet. While accurate and reliable instructional content exist, particularly from pharmaceutical manufacturers, some patients may be deterred away from these official resources in favor of patient-developed materials, such as those made available on YouTube [Citation12,Citation15]. Lack of regulation of such content can allow inaccurate guidance to propagate. One study assessing YouTube videos on methotrexate injection training found that less than 20% contained accurate, useful information, and over one-quarter were misleading [Citation15].
While both official and informal resources may provide some form of guidance on the functional aspects of injection training, few if any incorporate the emotional aspects of self-injection. In turn, studies show that HCPs often neglect the emotional aspects of self-administering injections [Citation11,Citation16–18]. Self-injection is known to evoke measurable apprehension and anxiety in some patients, including concerns about incorrect technique, fear of side effects, lack of self-confidence, stigma of illness, social embarrassment, frustration with illness and treatment, and fear of needles [Citation11,Citation19,Citation20]. The consequences of such emotional factors can be significant and may result in treatment nonadherence or discontinuation in otherwise physically capable patients [Citation17,Citation18]. Prior studies suggest that patients’ emotional state and self-efficacy may each play important roles in successful self-injection, and thus more focus on techniques to influence these factors alongside device competence could improve treatment initiation [Citation11,Citation13].
1.3. Study objectives
We previously conducted a qualitative analysis of biologic initiation designed to identify gaps in self-injection training and recommend potential approaches for improvement [Citation12]. While this study yielded valuable insights, the findings were qualitative in nature and its small sample size did not allow for statistical comparisons of training experience across different participant groups. The primary objective of the current study was to validate prior qualitative findings in a large sample of patients and HCPs with the intent to increase generalizability and more firmly characterize the biologic initiation experience. As an exploratory objective, this study also sought to examine the associations between training experiences and patient-reported outcomes, such as medication adherence, burden of treatment, and injection anxiety and confidence.
2. Study design and methods
2.1. Study design
This was a quantitative, retrospective, closed-ended survey administered to patients formally diagnosed with one of several chronic diseases treated with self-injection and HCPs experienced in biologic injection initiation. The sample was statistically powered to detect differences among various segmentation characteristics, establish generalizability, and determine the degree of difference (or lack thereof) in practices between patient and HCP groups.
Participants completed a series of survey questions related to their biologic training practices/experiences, self-reported validated assessments, and attitudes and beliefs toward biologic injections. Traditional participant demographics were collected alongside patient- and HCP-specific demographic information, including disease state (patients) and medical specialty (HCPs). All study procedures were conducted in accordance with the 1964 Declaration of Helsinki and its subsequent revisions. This was a non-interventional study and did not involve any new studies of human or animal subjects.
2.2. Participants
The recruiting rationale outlined below was modeled after the previously conducted qualitative research. Participants were recruited using commercially available, nationwide panels of HCPs and patients with chronic disease living in the United States. Participants completed an informed consent prior to survey initiation outlining steps taken to protect their privacy and study logistics (participation time, topics of focus, and terms of incentive).
For the HCP group, we recruited HCPs with routine experience (defined as daily, weekly, or monthly occurrence) training patients to self-inject biologic medications using an autoinjector (AI) or prefilled syringe (PFS). We recruited for a balanced sample across professional titles (physicians/physician’s assistants, nurses/nurse practitioners, and nurse educators) from the following six clinical specialties to represent diverse practice settings and varying biologic experience: neurology, rheumatology, gastroenterology, allergy/immunology, dermatology, and primary care. We also collected facility geography and size (measured by the number of biologic initiations and patients seen per month) from all HCP participants, although this was not a primary recruiting criterion.
For the patient group, we recruited adult patients (at least 18 years of age) currently self-injecting a biologic at home for the treatment of a chronic disease. The recruiting screener was designed to include patients with a range of biologic experience. Patients were considered biologic-naïve (BxN) if their only biologic experience was with their currently prescribed biologic therapy as the biologic initiation process being discussed in the survey would be their first. Biologic-experienced (BxE) patients have experience with previously prescribed biologic therapies other than the one they are currently on, therefore having experience with biologic initiation prior to their current biologic initiation session.
We recruited from the following six chronic disease areas to account for variability in marketed biologics: psoriasis/psoriatic arthritis (PsO/PsA), rheumatoid arthritis (RA), multiple sclerosis (MS), ulcerative colitis/Crohn’s disease (UC/CD), migraine, and severe asthma. Selected chronic disease areas were intentionally aligned to clinical specialties targeted in HCP recruiting to enable comparison and contrasting of experiences in lieu of a more complex, dyadic recruiting strategy. To control for bias toward self-injected medications that are more common or those that have been commercially available for longer periods of time, we established medication quotas based on market shares to ensure diversity within disease areas and avoid over-representation.
2.3. Data collection
At the survey outset, all participants completed quantitative assessments and survey questions about their biologic initiation experiences (patients) and facility practices (HCPs). Research topics were modeled after qualitative study questions and included time spent on initiation, physical demonstrations, demo-device use, caregiver presence, and demonstration video reliance. Patients also completed questions designed to quantify any negative experiences they could recall occurring within the first 6 months of biologic initiation, while HCPs completed questions on professional instruction and the impact of the COVID-19 pandemic on their facility training practices. If HCP practices changed due to impacts of COVID-19, they were asked to respond to questions about pre-pandemic practices to reduce the risk of situational bias.
In addition to questions related to practices and experiences, patients completed a variety of assessments designed to measure burden of treatment, injection anxiety and confidence, and medication adherence, where relevant. Burden of treatment was assessed using the Treatment Burden Questionnaire (TBQ) with Patient Acceptable Symptom State (PASS) and the medical information domain of Patient Experience with Treatment and Self-Management (PETS) measure [Citation6,Citation21–23]. Injection anxiety and confidence were assessed using the Self-Injection Assessment Questionnaire (SIAQ) [Citation24]. Medication adherence was assessed using the 8-item Morisky Medication Adherence Scale (MMAS-8) [Citation25]. Parallel assessments for patients and HCPs were developed (Supplemental File 1) using the medical information domain of PETS measure to facilitate comparative analysis in the perceived difficulty of comprehending and finding medical information. Patient assessments were primarily included to explore the potential effect of variables (e.g. disease state, injection experience, training received) on patients’ perceived burden of treatment, injection anxiety, and medication-taking behaviors. HCP participants additionally completed the Jefferson Scale of Empathy (JSE) to measure empathy in the context of patient care [Citation26].
Continuous semantic differential scales were used to collect attitudes and beliefs from both patient and HCP groups. Parallel questions/scales were developed for both groups surrounding roles and responsibilities of treatment and training. The parallel structure was designed to facilitate comparative analysis across patients and HCPs to further understand the perception of roles and accountability around this topic.
2.4. Data analysis
Quantitative assessment variables were compared between subgroups using Kruskal–Wallis tests, with Wilcoxon tests used in the case of a binary variable due to the non-normal nature of the subgroups. When appropriate, post-hoc multiple comparisons were calculated using a Dunn Test. All analyses used a two-sided Type I error of α = 5%. Quantitative variables were also compared against one another using Pearson correlations. When comparing two qualitative variables, Pearson’s chi-squared test was used, and standard residuals were calculated post-hoc.
2.5. Patient and public involvement
There was no patient or public involvement in the study design, management, or results generation.
3. Results
3.1. Participant characteristics
A total of 541 participants completed the remote study, including 264 patients and 277 HCPs. Participant characteristics are summarized in .
Table 1. Patient participant characteristics
Table 2. HCP participant characteristics
4. Participants were allowed to choose multiple ethnicities
4.1. Current biologic initiation paradigm
4.1.1. Time spent training patients on biologics
Findings related to time spent training and number of training sessions are summarized in and , respectively. Further information regarding number of training sessions can be found in Supplement . Among patient participants, 91.7% (242/264) reported receiving formal self-injection training. Of patients who received training, 64.9% (157/242) were trained in-clinic, 25.6% (62/242) were trained at their homes by an HCP, and 9.5% (23/242) received training remotely via phone or via call with an HCP. A caregiver was present during training for 67.4% (163/242) of trained patients.
Table 3. Injection time training
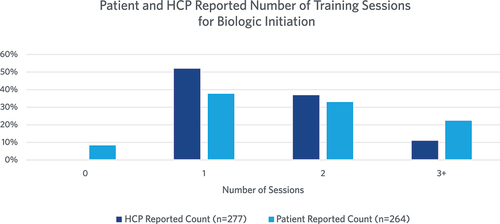
Over half of HCPs reported only providing one training session (52.3%, 145/277). HCPs reported that they spent a mean of 30.4 minutes (range: 3–200 minutes, median: 30.0 minutes) with patients during biologic initiation. There was a statistically significant difference in training time by specialty, with primary care HCPs spending the most time training patients on average (mean 45.6 minutes). The time HCP spent training patients was not significantly different by the overall quantity of biologics prescribed at the facility.
Of the total time spent training, HCPs reported a mean of 17 minutes (range: 1–120 minutes, median: 15 minutes) focused on instruction on injection steps. The amount of time training on injection steps was significantly different between different HCP specialties, with HCP’s practicing in primary care again spending the most time on injection steps. The time HCP spent training patients on injection steps was not significantly different by the overall quantity of biologics prescribed at the facility.
Patients reported significantly more time spent on overall training and training on injection steps compared to HCPs. However, there was not a statistically significant difference in patient reported overall training time by patient disease state. Of the total time spent training, patients reported a mean of 25.1 minutes (range: 0–120 minutes, median: 20 minutes) focused on instruction on injection steps.
4.1.2. Demonstration during training
Findings related to the type of demonstration, use of training devices during training, and the source of training devices are summarized in Supplement , Supplement , and Supplement , respectively. Most patients who were trained reported receiving a visual demonstration from their provider (93.8%, 227/242). Further, nearly all HCPs stated that a visual demonstration was included in training (98.2%, 272/277). However, their method of visual demonstration varied. Over half (50.4%, 137/272) of HCPs who provide a visual demonstration reported using a training device (also known as an injection trainer) to train patients, while 19.9% (54/272) reported using only a real device (injector with a needle and medication), and 29.8% (81/272) reported using both a training device and a real device to train.
Table 4. Negative experiences
A total of 90.6% (251/277) of HCPs reported that they have allowed patients to use training devices during training and 45.8% (127/277) reported that they always allow patients to do so. Of patients who received training, a total of 29.75% (72/242) reported they had the opportunity to use a training device with an HCP present. Training devices were offered to 71.2% (188/264) of patients to take home, with HCPs being the most common source of the offer (72.9%, 137/188). Of patients who accepted an offer of a training device for home use, 87.4% (160/183) report using the training device at home. Less than 3% (5/188) of patients who were offered a training device declined the offer.
4.1.3. COVID impact on training practices
Findings related to the potential impact of the COVID-19 pandemic on self-injection training are summarized in Supplement . Overall, most HCPs (51.3%, 142/272) reported that their facilities continued to train patients in person, although a substantial portion (39.3%, 107/272) reported that they relied on remote training for some period.
Table 5. MMAS, TBQ, and PASS findings
4.1.4. Conflicting perspective on training practices and responsibilities
Patients were significantly more likely to report that they were responsible for learning how to use their injection device themselves, while HCPs more often reported that they were responsible for training patients (p < 0.001). Among HCPs, the nurses/nurse practitioner and nurse educator subgroups were significantly more likely to report that training patients was their responsibility compared to the physician/PA subgroup (p = 0.039, p < 0.001). Nurses/nurse practitioners and nurse educators were also significantly more likely to want to personally train patients, whereas physicians/PAs were more likely to want a credible alternative party to do so (p = 0.005, p < 0.001). Patients were significantly more likely to report that their doctors made treatment decisions for them, while HCPs were more likely to report decisions that were made jointly with the patient (p < 0.001).
In terms of HCP empathy as measured by JSE scores, there was a significant numerical difference in scores between specialties (p = 0.04), although subsequent pairwise comparisons with Bonferroni adjustment failed to reach statistical significance. There was a significant difference in JSE scores by HCP title (i.e. nurse, nurse education, or physician/physician assistant), however (p = 0.005). Subsequent pairwise comparisons found significantly higher JSE scores for nurses and nurse educators compared to physician/physician assistants (p = 0.023, p = 0.015).
4.1.5. HCP Professional instruction
HCPs reported that they receive a mean of 52.9 hours of overall professional training per year (median 30.0, range 1–1000 hours). There was no statistically significant difference in the amount of overall training between different HCP specialties. HCPs reported that of the total hours of professional training per year, 17.4 hours (median 5 hours, range 0–600 hours) are focused on biologic initiation (32.9% of total yearly professional training).
Overall, 51.6% (143/277) of HCP participants reported ever receiving any form of ‘soft skill’ education (e.g. patient communication and coaching). There was a statistically significant difference in ‘soft skill’ education between specialty groups, with HCPs practicing in primary care more likely to have such training and dermatology and immunology/pulmonology less likely.
Among HCP participants, 44.8% (124/277) reported having a clinical educator on staff. There was a statistically significant difference in the availability of clinical educators between specialties, with gastroenterology physicians more likely to have a clinical educator on staff and dermatology less likely.
4.2. Post-training patient experience
4.2.1. Patient utilization of additional resources
Many patients (80.3%, 212/264) reported using additional video resources to aid in biologic initiation. A total of 40.9% (156/264) of patients used videos made by drug manufacturers, 39.4% (104/264) used videos on YouTube made by HCPs, 35.6% (94/264) used videos on YouTube made by patients, and 32.6% (86/264) used videos made by their prescribing healthcare facility.
4.2.2. Negative injection experiences
Patients were asked to recall their first 6 months of injection experience and select all negative experiences they had that were associated with their injection. Negative experiences included negative physical reactions, drug leakage or wastage, and emotional overwhelm during injection. A total of 89.8% (237/264) of patients reported at least one negative experience. Findings on negative experiences are summarized in .
4.3. Outcomes and hypothesis testing
Measures for TBQ, PASS, MMAS, and SIAQ were collected from all patients, and findings are summarized in .
4.3.1. Correlation of training time on patient burden, anxiety, and adherence
Total training time was slightly negatively correlated with SIAQ confidence scores (r2 = −0.104), while time focused on injection steps was not significantly correlated with SIAQ confidence scores. Neither total training time nor time spent focused on injection steps was significantly correlated with TBQ, PASS, MMAS, or SIAQ anxiety scores.
Patients who reported more than one training session reported significantly higher TBQ scores (69.3 vs 48.77, p < 0.001), lower MMAS scores (4.6 vs 5.3, p < 0.007), and lower SIAQ anxiety scores (5.6 vs 6.8, p < 0.001) than those who only reported one training session. Scores did not significantly differ for SIAQ confidence scales.
4.3.2. Correlation of training device use on patient burden, anxiety, and adherence
Patients who used a training device under HCP supervision in-office yielded statistically significant lower SIAQ anxiety scores than those who did not, indicating a higher amount of anxiety (5.4 vs 6.4, p = 0.023). Scores did not significantly differ for TBQ, PASS, MMAS, or SIAQ confidence scales. Patients who reported use of a training device at home reported significantly lower SIAQ anxiety scores (5.8 vs 7.5, p = 0.004), lower MMAS scores (4.6 vs 5.3, p = 0.004), and were more likely to be classified as ‘Low Adherence’ by MMAS (p = 0.03). Scores did not significantly differ for TBQ, PASS, or SIAQ confidence scales.
4.3.3. Correlation of device type on patient burden, anxiety, and adherence
Patients in our study who used PFSs reported a significantly higher treatment burden as measured by TBQ than those using AIs (68.1 vs 56.4, p = 0.014). Those who used PFSs also had significantly lower self-reported adherence measured by MMAS compared to those who used autoinjectors (4.5 vs 5.1, p = 0.004). No significant difference in injection anxiety, injection confidence, or PASS was observed between patients using either device.
4.3.4. Associations between treatment burden, injection anxiety, and adherence
Patients who reported being able to continue investing the same amount of time, energy, and money in their healthcare that they currently do for the rest of their lives (PASS) reported significantly lower TBQ scores (57.1 vs 81.2, p < 0.001). TBQ was strongly negatively correlated with SIAQ anxiety scores (r2 = −0.606) and moderately negatively correlated with MMAS (r2 = −0.445). Patients with severe injection anxiety as defined by SIAQ ≤ 2 had significantly higher TBQ scores (97.3 vs 57.6, p < 0.001). Patients classified as low adherence by MMAS reported significantly higher TBQ scores than those who were classified as medium adherence (75.08 vs 39.58, p < 0.001). TBQ was also weakly negatively correlated with SIAQ confidence (r2 = −0.169). SIAQ anxiety was moderately positively correlated to MMAS scores (r2 = 0.473).
5. Discussion
The rise in self-injection therapies has effectively begun to shift disease management out of the traditional healthcare setting and into patients’ homes. Self-injections not only lessen elements of HCP burden associated with in-clinic administration but also provide patients with more independence and generally more convenient treatment regimen [Citation20,Citation24]. While self-injections provide benefits for patients and HCPs alike, these benefits can only be realized if patients are able to self-inject correctly. Although proper onboarding to self-injection therapy may be crucial to developing self-injection skills and confidence, literature on the methods and impacts of effective biologic initiation is currently lacking.
While our prior study explored biologic initiation qualitatively in a relatively small sample, the current study sought to validate and generalize these findings in a larger sample of patients and HCPs. To our knowledge, this is the largest study designed to characterize numerous aspects of biologic initiation. This section will therefore center on comparing our current findings to prior literature, including our qualitative study, and discuss potential implications for self-injection therapy.
5.1. Incidence and duration of training
Over 90% of patients in our study reported that they received training from an HCP, a surprisingly high proportion compared to prior research, which reported figures between approximately 40–65% [Citation10–12]. In contrast, this study’s findings on the duration of training sessions and training specific to injection steps were largely consistent with our prior qualitative study. The weak correlation between higher patient injection anxiety and total training time may suggest that patients who feel anxious about injecting their medication may request more training time from their HCP.
Given the critical and sometimes-complex nature of the injection process, HCPs who prescribe biologics may be required to dedicate significant portions of their limited time to training in order to ensure proper injection. Interestingly, despite likely prescribing fewer biologics overall compared to other specialties, primary care HCPs in our study spent the most time training patients both overall and specifically on injection steps, and were more likely to provide two training sessions rather than one. This may indicate that HCP specialists may be particularly overwhelmed with time constraints during patient visits. Another possible explanation is that more experience prescribing biologics allows for greater training efficiency among specialist HCPs.
5.2. Number of training sessions and retention
While our qualitative study suggested that most patients receive training over 2 training sessions, the current study revealed that training is often conducted as a single session (as reported by 37.8% of patients and 52.3% HCPs). Limiting training to a single session could present challenges for patient learning, as prior research suggests patients may be overwhelmed during a single visit, and providing information in an incremental and iterative fashion could reduce this emotional burden [Citation27,Citation28]. Moreover, several studies have found that incorporating spaced repetition of training over time can enhance retention [Citation29,Citation30]. These multiple training sessions may provide ‘over-learning’ beyond what is required for initial proficiency, which may reduce knowledge and skill decay over time [Citation28]. Overall, distributing training in shorter, more frequent intervals is likely optimal, as it provides patients adequate time to absorb and retain information for the duration of their therapies.
Participants who reported more than one training session reported higher treatment burden, higher injection anxiety, and lower adherence than those who only had one training session. It is possible that patients with these characteristics may be more inclined to request multiple training sessions. These findings may be confounded by the retrospective nature of the study and require a controlled, prospective study to accurately assess the effects of multiple training sessions on injection anxiety and adherence.
5.3. Stakeholder ownership of the training process
Our previous qualitative study revealed differences in perceived stakeholder responsibility in the training process. This was also observed in our quantitative study, as there was significant discrepancy in responses regarding responsibility of injection training. HCP views on training differed significantly by title, with nurses and nurse educators being more inclined to claim responsibility for training compared to physicians and PAs. Perhaps more importantly, nurses and nurse educators appeared to be more passionate about training patients. Along with higher empathy scores as measured by JSE, nurses, and nurse educators were more inclined to want to personally train patients, while physicians and PAs were more willing to outsource training to other credible parties.
These findings suggest that while training is often generalized as a requirement for all HCPs, in practice the training requirement resonates greater with nurses and nurse educators. This means patients may also have significantly different training experiences based on the specific title and role of the HCP training them. Further, given the willingness of physicians and PAs to outsource training, credible third parties, such as patient support programs offered by pharmaceutical manufacturers, could be a welcomed means to help patients who require additional training to confidently self-inject.
Whereas perceptions of training responsibility were variable within the HCP group, the majority of patients reported that they themselves were responsible for training on their injections. These results may indicate that despite HCPs believing they provide ample training, patients still feel unprepared to self-inject and must therefore find resources to train themselves. Given the unreliability of some external sources, this disconnect may be particularly problematic [Citation15,Citation31,Citation32].
5.4. Finding medical information
Analysis of the medical information component of PETS revealed that HCPs perceive finding credible medical information as a patient more difficult than patients themselves do. One potential explanation for this finding is that HCPs have a higher standard than patients do for what sources of health information are credible. Further, it may also mean that patients may perceive untrustworthy medical information as credible. Indeed, in our qualitative study, patients reported that they perceived information offered by drug manufacturers as biased, and therefore often turned to other online sources such as social media and YouTube for information.
Further investigation in our quantitative study revealed that over 80% of patients watched demonstration videos online when beginning their injection, with over 35% of participants reporting that they watched YouTube videos made by patients. This may suggest that patients desire additional training resources than what was provided during their training sessions. While YouTube can be an effective education tool for patients performing self-injection, it also poses a risk of delivering medical misinformation [Citation15,Citation31,Citation32]. Videos posted on YouTube are largely unregulated and thus could and sometimes do contain misleading or inaccurate information. Previous studies assessing self-injection training videos found on YouTube revealed that there is a large proportion of videos with misleading information [Citation15,Citation31,Citation32]. Further, videos found to be useful by the researchers were not viewed more frequently [Citation15]. Additional studies are needed to assess how patients use the information in patient-made YouTube videos and if they verify the presented information with credible sources. The pharmaceutical industry should be cognizant of patient use of YouTube as a source of training material and consider efforts to create authentic and patient-friendly videos that also reflect best practice. Moreover, HCPs in clinical practice should recommend certain reliable videos to patients to decrease the risk of patients discovering inaccurate or misleading videos on their own.
5.5. Use of training devices and patient assessments
While nearly all HCPs reported providing a visual demonstration of the injection process during training, nearly 20% of demonstrations were conducted using a real device. As the real device is not actuated under these circumstances, this training method does not adequately represent key use steps associated with the injection itself, including proper pressure required for device activation, audiovisual device feedback (e.g. ‘clicks’ and viewing window changes), and appropriate holding time to allow for complete medication administration. Unfortunately, less than half of HCPs reported always letting patients use training devices themselves as part of standard training. Use of a training device was even less common among patients, as less than one-third of trained patients reported having the opportunity to use a training device. As over one-third of patients in our study reported a lack of confidence when injecting during the first six months, increased use of a training device under HCP supervision could help reinforce correct technique and increase confidence.
Further, less than one-third of HCPs reported that they offered a training device to their patients and a similar proportion of patients reported receiving an offer for a training device. Given that less than 2% of patients reported declining an offer for a training device, training devices seem to be highly coveted by patients despite not being universally available. Indeed, HCPs reported that the primary reason for not sending home a training device with patients was limited device availability. As HCPs were most commonly the supplier of training devices in our study, supplying HCPs with more training devices may help increase the use of these devices during in-office training as well as at home.
We hypothesized that the use of training devices would be associated with lower patient burden and injection anxiety, higher injection confidence, and higher patient-reported medication adherence. However, we found that the use of training devices in office had no statistically significant correlation with any hypothesized outcome with the exception of injection anxiety. Patients who reported that they used a training device in the office were found to have higher injection anxiety than those who reported they did not. Similarly, reported use of a training device at home was associated with higher injection anxiety scores and lower patient-reported medication adherence. While these are unexpected results, it is possible that patients with higher anxiety or lower adherence may be more inclined to use a training device, and thus these outcome measures reflect baseline values rather than any indication of the effect of training device use. A controlled, prospective study is needed to accurately assess the effects of training devices on confidence, anxiety, and adherence.
5.6. Training setting and COVID-19 impact
Interestingly, the overwhelming majority of training occurred in person, either at the HCP office or with HCP training at home, with less than 10% of patients reporting that they trained remotely. These results were gathered mid-pandemic but reflect pre-pandemic situations. We recognize that many training sessions may have since shifted to delivery via phone or video call. Over half of HCPs reported that they continued to train in-clinic throughout the pandemic and over one-third reported that they had shifted to remote at the start of the pandemic but had since moved back in-clinic. A small portion of HCPs reported that they continued to train remotely, and this may be a trend that continues given the increase in healthcare accessibility provided by remote appointments [Citation14]. Techniques to retain key components of in-person training, including use training devices, should be developed in order to ensure patients are successful regardless of training setting.
5.7. Device type and patient assessments
AI and PFS devices are the two most commonly available injection devices for biologics, with autoinjectors beginning to predominate. Several prior studies have reported patient preference for AIs relative to PFSs largely due to improved usability [Citation33,Citation34]. Patient preference for AIs may have been reflected in our study as well, as PFS users reported significantly higher treatment burden and lower medication adherence compared to AI users. Additional studies that explore the potential differences in training needs between AI and PFS users may be warranted.
5.8. Patient negative experiences
The majority of patients in our study reported at least one negative experience in their first 6 months of injection therapy. Despite advancements in drug formulation and drug delivery devices, over 70% of our patients reported physical reactions such as pain and bruising, and over one-third experienced drug leakage, drug waste, or both. Greater emphasis on training during injection initiation has the potential to reduce these negative experiences. While such physical complications are often reported as a part of post-market surveillance, emotional burdens are not. Our study found that nearly two-thirds of patients reported emotional burden associated with injection initiation. This is consistent with findings from prior studies and emphasizes the need to incorporate emotional aspects into self-injection training programs [Citation11,Citation12,Citation27]. Further, over one-third of patients reported lacking confidence that they would be able to self-inject the correct way, highlighting the need for improvements in training practices.
5.9. Inter-assessment relationships
Similar to other studies, our study found that patients with chronic disease struggle with excessive treatment burden, injection anxiety, and often have poor adherence to medications [Citation6,Citation11,Citation35]. The average treatment burden, as measured by TBQ, was higher in our study than what has been established by other authors [Citation6]. Although some relationships between chronic disease and treatment burden, injection anxiety, and medication adherence are well established, no studies have established correlations between all these measures in the same sample of patients [Citation36,Citation37]. Perhaps unsurprisingly, our study found a strong correlation between injection anxiety and treatment burden. Moreover, patients in our study who reported higher injection anxiety were also significantly more likely to have lower self-reported medication adherence. These findings appear to confirm that psychosocial and emotional burden play important roles for patients with chronic disease and call for the healthcare industry to better address patient anxiety as a means to lower treatment burden and potentially improve medication adherence. While we found significant correlations between these measures, our results should be treated as exploratory in nature. Future studies should examine the relationship between these factors more closely.
6. Limitations
The major limitation of this study is its retrospective, non-interventional nature, and thus sources of potential confounding and bias could not be completely controlled for. Second, participants were not recruited as dyads, and we were therefore unable to make direct comparisons between HCP and patient findings. Enrolling patient-HCP dyads may have yielded more insightful results; however, this approach would have likely severely restricted our sample size due to practical recruiting limitations. Still, we believe our approach to enroll patients and HCPs in common disease areas helped to mitigate this shortcoming. Conducting a similar study with patient-HCP dyads would be useful to confirm the gaps in biologic initiation described in our research. Third, due to practical constraints on the ability to recruit individuals with <6 months of experience injecting their current therapies, we could not enroll patients who had just recently been initiated or observe their initiation experiences directly. As a result, patients were required to recall their biologic initiation experiences, which poses risk of recall bias. Lastly, although we used purposeful sampling, our recruiting yielded a sample of HCPs that was dominantly female (74%), and a large subset of our sample of both HCPs and patients that were white (Patient: 85.6%, HCP: 78.3%). This difference in demographics is likely due to the sample available from recruiting. With that said, there were no noticeable differences by HCP gender or patient ethnicity. Despite these limitations, this large-scale survey of self-injection training practices, experiences, and perspectives offers valuable insight into to the biologic initiation process.
7. Conclusion
The current paradigm for biologic initiation has significant gaps, leaving patients inadequately supported to start their therapies. Training was often comprised of one or two brief sessions that may not be adequate to prepare patients. The mean overall training time reported was 37.8 and 30.4 minutes by patients and HCPs, respectively, with only a portion of that time focused on injection steps. Further, less than 25% of patients reported receiving more than 2 training sessions. Over 80% of patients reported utilization of supplemental online demonstration video resources when beginning their injection. Still, over one-third of patients reported lacking confidence that they were able to self-inject the correct way during the first 6 months of therapy.
Considerable attention must be paid to providing patients with multiple training sessions to aid memory, training devices for home use, and readily available and medically accurate medical information for access outside the office. The associations between training practices and patient-reported measures are limited by the retrospective survey nature of this study. Further studies should prospectively examine the impact of best practice training techniques on measures such as overall treatment burden, injection anxiety, and medication adherence.
Author contributions
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship, take responsibility for integrity of the work as a whole, and have given final approval to the version to be published. Secondary research of literature: J Hawthorne, D Katsaros; study design, execution: A Rinaldi, K Brigham, M D’Auria, E Bajars; Data Analysis: J Hawthorne, M D’Auria, K Brigham, D Katsaros; substantial contributions to manuscript preparation: J Hawthorne, D Katsaros; critical revision of manuscript for important intellectual content: C Franzese, M Coyne, J Hawthorne, D Katsaros; review of manuscript for clinical accuracy: C Franzese, J Hawthorne, D Katsaros.
Declaration of interest
All authors are employees of Matchstick. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Quant_Supplements_1DK_.docx
Download MS Word (16.6 KB)Supplementary material
Supplemental data for this article can be accessed here
Additional information
Funding
References
- Castelli MS, McGonigle P, Hornby PJ. The pharmacology and therapeutic applications of monoclonal antibodies. Pharmacol Res Perspect. 2019 Dec;7(6):e00535.
- Eton D, DR Egginton, JS Ridgeway, et al. Building a measurement framework of burden of treatment in complex patients with chronic conditions: a qualitative study. PROM. 2012 Aug 39. DOI:https://doi.org/10.2147/PROM.S34681
- Dobler CC, Harb N, Maguire CA, et al. Treatment burden should be included in clinical practice guidelines. BMJ. 2018 Oct; p. k4065. DOI:https://doi.org/10.1136/bmj.k4065
- Schwartzman S, Morgan GJ. Does route of administration affect the outcome of TNF antagonist therapy? Arthritis Res Ther. 2004 Jun;6(S2). DOI:https://doi.org/10.1186/ar996
- Navarro-Millán I, Herrinton LJ, Chen L, et al. Comparative effectiveness of etanercept and adalimumab in patient reported outcomes and injection-related tolerability. PLOS ONE. 2016 Mar;11(3):e0149781.
- Tran V-T, Montori VM, Ravaud P. Is My Patient Overwhelmed? Mayo Clin Proc. 2020 Mar;95(3):504–512.
- Weinhold T, Del Zotto M, Rochat J, et al. Improving the safety of disposable auto-injection devices: a systematic review of use errors. AAPS Open. Dec 2018;4(1).doi:https://doi.org/10.1186/s41120-018-0027-z
- “CIMZIA (certolizumab pegol) [package insert]. Smyrna GA: UCB, Inc.; 2019. Cited 2021 Feb 03: https://www.cimzia.com/themes/custom/cimzia/docs/CIMZIA_full_prescribing_information.pdf.
- “FASENRA (benralizumab) [package insert]. Wilmington DE: AstraZeneca Pharmaceuticals; 2019.
- Lang VA, Nalan D. Combination product patient training: how are patients trained and who conducts the training?, presented at the 2018 Design of Medical Devices Conference, Minneapolis, Minnesota, USA, Apr. 2018. doi: https://doi.org/10.1115/DMD2018-6956.
- Schiff M, Saunderson S, Mountian I, et al. Chronic disease and self-injection: ethnographic investigations into the patient experience during treatment. Rheumatol Ther. 2017 Dec;4(2):445–463.
- Rinaldi A, Katsaros D, Hawthorne J, et al. The current paradigm for biologic initiation: a mixed-methods exploration of practices, unmet needs, and innovation opportunities in self-injection training. Expert Opin Drug Deliv. 2021 Aug;18(8):1151–1168.
- Oleen-Burkey M, Pardo G. Examining the influence of behavioral factors on compliance and persistence with glatiramer acetate injection for relapsing-remitting multiple sclerosis. J Neurol Neurophysiol. 2014;05(3). DOI:https://doi.org/10.4172/2155-9562.1000205
- Mann DM, Chen J, Chunara R, et al. COVID-19 transforms health care through telemedicine: evidence from the field. J Am Med Inform Assoc. 2020 May;27(7):1132–1135.
- Rittberg R, Dissanayake T, Katz SJ. A qualitative analysis of methotrexate self-injection education videos on YouTube. Clin Rheumatol. 2016 May;35(5):1329–1333.
- Tallman K. Communication practices of physicians with high patient-satisfaction ratings. Perm J. 2007 Dec;11(1). DOI:https://doi.org/10.7812/TPP/06-106
- Cox D, Stone J. Managing self-injection difficulties e page in patients with relapsing-remitting ce multiple sclerosis. J Neurosci Nurs. 2006;38(3):5.
- Mohr DC, Cox D, Epstein L, et al. Teaching patients to self-inject: pilot study of a treatment for injection anxiety and phobia in multiple sclerosis patients prescribed injectable medications. J Behav Ther Exp Psychiatry. 2002 Mar;33(1):39–47.
- Zimmer PA, Braun LT, Fraser R, et al. Promoting Success in Self-Injection: listening to Patients. Medsurg Nurs. 2015 Aug;24(4):279–282.
- van den Bemt BJF, Gettings L, Domańska B, et al. A portfolio of biologic self-injection devices in rheumatology: how patient involvement in device design can improve treatment experience. Drug Deliv. 2019 Mar;26(1):384–392.
- Tran V-T, Harrington M, Montori VM, et al. Adaptation and validation of the Treatment Burden Questionnaire (TBQ) in English using an internet platform. BMC Med. 2014 Dec;12(1):109.
- Tran G, Dube B, Kingsbury SR, et al. Investigating the patient acceptable symptom state cut-offs: longitudinal data from a community cohort using the shoulder pain and disability index. Rheumatol Int. 2020 Apr;40(4):599–605.
- Rogers E, Yost K, Rosedahl J, et al. Validating the Patient Experience with Treatment and Self-Management (PETS), a patient-reported measure of treatment burden, in people with diabetes. PROM. 2017Nov;8:143–156.
- Keininger D, Coteur G. Assessment of self-injection experience in patients with rheumatoid arthritis: psychometric validation of the Self-Injection Assessment Questionnaire (SIAQ). Health Qual Life Outcomes. 2011;9(1):2.
- Morisky DE, Ang A, Krousel-Wood M, et al. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertension. 2008 May;10(5):348–354.
- Hojat M, Mangione S, Nasca TJ, et al. The Jefferson Scale of Physician Empathy: development and preliminary psychometric data. Educ Psychol Meas. 2001 Apr;61(2):349–365.
- Kottak N, Tesser J, Leibowitz E, et al. Ethnographic observational study of the biologic initiation conversation between rheumatologists and biologic-naive rheumatoid arthritis patients. Arthritis Care Res. 2018 Jul;70(7):997–1004.
- Arthur W Jr., Bennett W Jr., Stanush PL, et al. Factors that influence skill decay and retention: a quantitative review and analysis. Human Performance. 1998 Mar;11(1):57–101
- Clark SE. Training decay selection for usability validation. Proc Int Symp Hum Factors. 2016 Jun;5(1):76–83.
- Nakatani Y, Matsumura M, Monden T, et al. Improvement of glycemic control by re-education in insulin injection technique in patients with diabetes mellitus. Adv Ther. 2013 Oct;30(10):897–906.
- Singh AG, Singh S, Singh PP. YouTube for information on rheumatoid arthritis — a wakeup call? J Rheumatol. 2012 May;39(5):899–903.
- Tolu S, Yurdakul OV, Basaran B, et al. English-language videos on YouTube as a source of information on self-administer subcutaneous anti-tumour necrosis factor agent injections. Rheumatol Int. 2018 Jul;38(7):1285–1292.
- Vermeire S, D’heygere F, Nakad A, et al. Preference for a prefilled syringe or an auto-injection device for delivering golimumab in patients with moderate-to-severe ulcerative colitis: a randomized crossover study. PPA. 2018Jul;12:1193–1202.
- Borrás-Blasco J, Gracia-Pérez A, Rosique-Robles JD, et a.l Acceptability of switching Adalimumab from a prefilled syringe to an autoinjection pen. Expert Opin Biol Ther. 2010 Mar;10(3):301–307.
- Jüngst C, Gräber S, Simons S, et al. Medication adherence among patients with chronic diseases: a survey-based study in pharmacies. QJM. 2019 Jul;112(7):505–512.
- Heckman BW, Mathew AR, Carpenter MJ. Treatment burden and treatment fatigue as barriers to health. Curr Opin Psychol. 2015Oct;5:31–36.
- Turner AP, Williams RM, Sloan AP, et al. Injection anxiety remains a long-term barrier to medication adherence in multiple sclerosis. Rehabil Psychol. 2009;54(1):116–121.