ABSTRACT
Introduction
Many small molecules and biologic therapeutics have been developed for solid tumor therapy. However, the unique physiology of tumors makes the actual delivery of these drugs into the tumor mass inefficient. Such delivery requires transport from blood vessels, across the vasculature and into and through interstitial space within a tumor. This transportation is dependent on the physiochemical properties of the therapeutic agent and the biological properties of the tumor. It was hoped the application of nanoscale drug carrier systems would solve this problem. However, issues with poor tumor accumulation and limited drug release have impeded clinical impact. In response, these carrier systems have been redesigned to be paired with targetable external mechanical stimuli which can trigger much enhanced drug release and deposition.
Areas covered
The pre-clinical and clinical progress of thermolabile drug carrier systems and the modalities used to trigger the release of their cargo are assessed.
Expert opinion
Combined application of mild hyperthermia and heat-responsive liposomal drug carriers has great potential utility. Clinical trials continue to progress this approach and serve to refine the technologies, dosing regimens and exposure parameters that will provide optimal patient benefit.
1. Introduction
The diffusion of oxygen in tissue is limited to the range of 100–200 µm, a distance which helps determine the ordered structure and spacing of blood vessels within normal tissue. Vessels supplying surrounding tissues can effectively perfuse tumors provided the tumors are less than approximately 2 mm in size. However, growth of a tumor beyond this size is dependent on the acquisition of its own blood supply. To achieve this cells within the tumor undergo a hypoxia inducible factor 1 α (HIF-1α) driven activation of pro-angiogenic and tumor microenvironment remodeling gene expression [Citation1]. This process lacks temporal and spatial control and the vasculature which develops is therefore far from normal. Indeed, blood and lymphatic vessels in tumors are functionally and morphologically different from vessels in normal tissues. Tumor blood supply plays a vital role in delivering therapeutic agents to solid tumors, but the average blood flow in tumors is less well-regulated compared to normal tissues. Tumor vasculature is highly heterogeneous and its rapid growth leads to a loss of pericyte coverage and a highly fenestrated phenotype, where gaps of up to 1 µm between neighboring endothelial cells have been reported [Citation2]. This can have the effect of uncontrolled influx of fluid and solutes through these gaps and into the tumor interstitium. The dysfunctional state of the lymphatic vessels which collapse under the raised interstitial pressure only serves to exacerbate this effect. This creates a vicious cycle whereby raised pressure leads to loss of lymphatic drainage, leading to a loss of convective flow across the tumor, leading to further increases in pressure [Citation3]. Indeed, measurements in a range of human tumors shows the interstitial pressure can match that of the pressure within the arterioles [Citation4]. Such increases in interstitial fluid pressure and loss of convective flow cause inefficient uptake and distribution of therapeutic agents, the movement of which becomes entirely diffusion dependent [Citation5]. A further challenge is that the extracellular matrix of tumors is composed of a dense mesh of fibrous proteins and polysaccharides. This extracellular matrix further hinders drug transport through the interstitium. In response, the diffusive gradient can be maximized by dosing with higher levels and/or multiple cycles of drug, but the dose of drug required to achieve clinically effective cytotoxicity in tumors may result in severe damage to nonmalignant cells and therefore treatment limiting toxicity in healthy organs [Citation6].
A key concept in the field of drug encapsulation is that the pharmacokinetic profile, and therefore the therapeutic index of cytotoxic drugs, can be made more favorable by their encapsulation within carrier systems. Much work has been performed to formulate drugs within carrier systems that have dimensions in the range of 80–200 nm. Notably, highly fenestrated tumor vasculature can provide a mechanism for accumulation of such nanoparticles, which may be large enough to avoid capture through fenestrated endothelia in liver and spleen, but small enough to pass through gaps in tumor vessels [Citation7]. This effect, known as the enhanced permeability and retention effect (EPR), has stimulated huge amounts of historical research interest [Citation8–11] and more recently some level of controversy [Citation12]. Indeed, Chan et al. recently suggested an average of just 0.7% of the total dose of a nanoparticulate system can accumulate in the tumor as a result of the EPR [Citation13]. Further studies by this group have demonstrated that, in the models they used for testing, the prime driver for tumor uptake was an active trans-endothelial cell transport mechanism, rather than the EPR effect [Citation14]. It is important to note that regardless of the true mechanism responsible, the level of tumor accumulation achieved by nano-carriers, even at 0.7%, can still be far in excess of what is achieved by the vast majority of non-encapsulated, non-targeted (free) drugs. Indeed, the real limitation may not be that insufficient level of drug is reaching the tumor. It is firstly that the tumor uptake is restricted to the perivascular regions, as diffusive penetration of nanoparticles through the dense extracellular matrix, is a very inefficient process [Citation15], and secondly that nanoparticles designed to be stable in the bloodstream often fail to effectively release their cargo upon entry into the tumor. These two limitations are exemplified elegantly by papers by Dromi et al. and Laginha et al. who demonstrate that liposomal formulations of doxorubicin (Dox) lead to perivascular accumulation of drug and just a third of the drug being released over a 24-hour period [Citation2,Citation16]. Indeed, one study suggested that the bioavailability is as little as 0.4% of the Dox in a dose of Doxil even in in vitro studies where cells are effectively bathed in the liposomal drug carrier [Citation17].
When introduced into the body drug carrier systems undergo a complex journey before arriving at the target site. To achieve extended circulation carriers are required to avoid the two primary mechanisms of particulate clearance namely capture by the reticuloendothelial system (RES), and passage through fenestrated tissue beds in the liver, spleen and kidney. Having achieved extended circulation, they may then adhere to the vasculature of the target site or permeate across the vasculature into the target site. Particle size is critical for carrier systems in determining circulation time and also influences the extent of cellular uptake by phagocytosis and/or endocytosis. Particles smaller than 5–10 nm can be cleared by kidney filtration, particles below 100 nm by liver filtration and particles larger than 200 nm are typically eliminated by splenic filtration [Citation18,Citation19].
In response to these limitations, a range of approaches have been studied to provide carrier systems that are more fit-for-purpose and can release cargo within tumors more effectively.
Liposomes are a common approach to formulating a carrier system for drug delivery. These spherical vesicles can range in size from nanometers to a few micrometers and typically consist of various lipid bilayers arranged concentrically to trap there in one or more aqueous compartments. Their diameter and number of layers can be modified by the manufacturing process used, leading to classifications such as small unilamellar vesicles, large unilamellar vesicles and multilamellar vesicles. Their unique structure offers the prospect of encapsulating hydrophilic (in the aqueous core) as well as lipophilic drugs (in the phospholipid bilayers). Liposomes used for clinical purposes are commonly composed of neutral phospholipids and cholesterol. The bilayer has low permeability to charged molecules and is impermeable to large molecules (proteins and enzymes). A protective surface layer of polyethyleneglycol (PEG) is often added to provide stability in the blood stream. In the recent years, advances in commercialization of liposomal formulations have been seen with, for example, Doxil (Sequus Pharmaceuticals), DAU (NeXtar Inc.) and Marqibo (Index Pharmaceuticals Corporation), gaining clinical approval [Citation19]. However, the potential clinical impact of these systems has been stymied by suboptimal accumulation at the target tumor site and limited release of drug payload there in. Approaches to address these limitations using externally applied, targetable mechanical stimuli are discussed here.
2. Methods of triggering release
The challenge of triggering the release of payload only at the tumor site and at a controllable rate has been addressed in several ways. Crucially achieving such a trigger requires a shift in the drug-carrier relationship from stable during the delivery phase to gross instability at the target site. A range of mechanical and biological stimuli have been tested as methods for instigating release, including but not limited to, pH, enzymes, light, electromagnetic field change and heat. This review will focus exclusively on heat as it represents the most clinically mature approach.
2.1. Heat
At one extreme, modalities such as high intensity focussed ultrasound [Citation20] or radiofrequency ablation can be used to deposit sufficient energy to directly kill cells [Citation21]. However, the technology and time required to achieve such deposition makes the approach rather expensive and hard to apply on a widespread basis. In response, a range of preclinical studies have been performed to validate the relationship between milder heating and chemotherapy [Citation22,Citation23]. Indeed, there is now compelling data to show that the combination of chemotherapy and mild hyperthermia shows better results in patients than chemotherapy alone [Citation23–25]. The precise mechanisms behind this effect are still to be defined and are dependent on the particular level of heating used, but it is thought that enhanced vasodilation, increased membrane permeability and improved sensitivity to the cytotoxic impact of drugs are all important factors [Citation26]. To take further advantage of the effect of localized heating its potential to trigger release of payload from carrier systems has also been investigated. Hence, a range of thermosensitive carrier systems has been developed and tested [Citation27]. Whilst they differ markedly in composition, and also the source of energy used to achieve heating, they all share the potential to allow hyperthermia to increase the therapeutic effectiveness by providing triggered raised drug levels at the target [Citation28,Citation29]. This has also been evidenced in studies using the hyperthermic intraperitoneal chemotherapy (HIPEC) approach where drug is warmed pre-infusion into the intraperitoneal compartment [Citation30].
Studies have shown that standard thermosensitive liposomes release their payload in around 30 mins when they are triggered in the range of 42–45°C whereas at 39.5–41°C low temperature sensitive liposomes release the payload in seconds [Citation31].
The remainder of this review will focus on hyperthermia triggered drug release from thermosensitive drug carriers. These trials have reported a range of approaches to achieve and monitor heating and drug release and many promising clinical outcomes. A detailed assessment of the field and the approaches that have been taken is important in ensuring further trials provide optimal outcomes.
3. Means of achieving targeted heating
Having developed heat responsive drug carrier formulations, a range of modalities have been investigated for their ability to deposit energy in tissue to achieve the temperature increase required to trigger release from these formulations. These include high intensity focussed ultrasound (HIFU), radiofrequency ablation (RFA), microwaves and near infrared (NIR) (see ); their benefits, limitations and clinical progress are discussed below:
Table 1. Frequencies of the modalities used to instigate triggered release.
3.1. High-Intensity Focused Ultrasound (HIFU)
The term ultrasound encompasses sound waves with frequencies higher than the upper audible limit of human hearing. Ultrasound can produce a mechanical wave which can be focused on a defined region inside the patient, where energy absorption causes focal and rapid heating. In high intensity focussed ultrasound (HIFU), focused ultrasound is applied for local ablation therapy in the treatment of tumors using between 0.35 and 5 MHz and 100 and 10,000 W/cm2. In ablation therapy the aim is to maximize energy deposition at target site to initiate coagulative necrosis without instigating harm to the surrounding healthy tissues. At temperatures above 55°C coagulative necrosis is induced with sharp margins between healthy and tumor tissues. Such discrimination has drawn comparisons to a ‘thermal knife’ which provides surgical precision without the need to perform open surgery and physically remove tumor masses. HIFU treatments can be performed under two imaging methods either ultrasound or magnetic resonance imaging (MRI), depending on the treatment regime and exact application [Citation32–34]. HIFU has the potential to improve the precision and widen the clinical application of thermosensitive liposomes due to the capability it provides to focus and control heating (see ). Such focus and control are achieved by careful selection of acoustic parameters such as whether pulsed or continuous acoustic energy is applied as well as the frequency of the ultrasound and the magnitude of the pressure amplitude that is applied [Citation35,Citation36]. HIFU is also compatible with MRI for real-time monitoring of tissue temperature [Citation37], although reliance on such an expensive technology may ultimately be limiting and there are additional challenges of working in an MRI environment which must be free of ferromagnetic materials. HIFU has also been used in a range of preclinical studies to compare the efficiency of ultrasound sensitive drug carriers. The preclinical and clinical evidence relating to the use of HIFU in enhancing drug delivery is discussed in section 5 and 6.
3.2. Near infrared
Application of NIR is another method of noninvasively generating heat within the body. To achieve this the target is irradiated with continuous wave NIR laser light at ~800 nm wavelength (at intensities that don’t damage the skin) causing an increase in temperature which can then be used to induce rapid release of cargo from liposomes. The disadvantage of NIR is that its transmission in soft tissues is limited to just 3 cm [Citation38] as even light in 600–950 nm region is markedly attenuated during passage through tissue [Citation39]. This may limit its use to surface exposed tumors such as melanoma. Work using different types of nanoparticles, e.g. gold has been performed to study whether the provision of such photothermal conducting agents can enhance NIR and thereby improve its utility in tumor ablation and/or drug release [Citation40–43]. Upon irradiation of NIR laser light, gold nanoparticles absorb the incident energy and convert it to heat to raise the temperature above what would be achieved by the NIR alone [Citation44,Citation45]. Liu et al designed photothermal carboxymethyl chitosan nanospheres for drug loading and delivery. They showed excellent NIR-responsive and photothermal conversion behavior in vitro [Citation46]. A recent review by Raza et al captures developments in this field [Citation47].
3.3. Radiofrequency ablation
Another source for locoregional thermal therapy is radiofrequency ablation (RFA). RFA is minimally invasive image guided technique which uses heat to kill cancer cells. The process involves image guided placement of a needle like electrode into the tumor either laparoscopically, percutaneously or during open surgery. Local tissue heating is caused by exposure of tissue to the alternating current in the range 350–500 kHz. This radiofrequency applied to the tissues adjacent to the electrode results in coagulation necrosis. Ablation typically targets an approximate 1 cm margin around the tumor with the intention of achieving complete destruction, but this is not always achieved due to the heat sink effect of the extensive vascularity of the tissue, location of the tumor, limitations of existing probe design and because of the existence of distant microsatellites from the macroscopic tumor [Citation48,Citation49]. RFA has been used for clinical treatment of tumors within the liver, kidney, lung and bone [Citation50]. RFA has been combined with TSL in several studies (see sections 4 and 5). A challenge faced by RFA is local recurrence of tumors, however this is an acceptable risk if patients are too co-morbid for surgical resection.
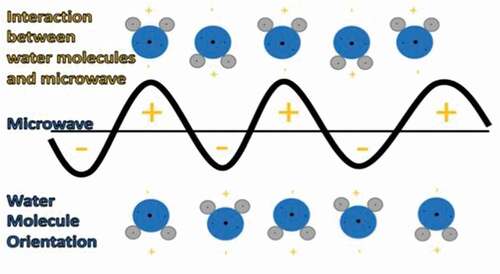
3.4. Microwaves
Another means of applying a local source of energy deposition for heating is the use of microwaves (See ). Microwave ablation utilizes high frequency electromagnetic waves of 900 MHz to 2450 MHz to produce heating via oscillation of polar molecules, notably water, leading, to tissue necrosis within solid tumors [Citation51]. Microwave ablation can be applied regionally by surface applicators (pads) or percutaneously (minimally invasive) [Citation52]. There is less clinical experience of pad applicators, but systems such as the Pyrexar Medical BSD2000 have enabled regional deep hyperthermia to be utilized in combination with non-encapsulated chemotherapy and radiotherapy in a range of cancer indications [Citation53].
Key features of insertion of a probe for percutaneous microwave ablation are that they can offer deep depths of penetration (probes are currently available up to a length of 19 cm), attenuation by bone and air in the path to the tumor is not a limitation and the thermal efficiency and can be controlled by altering various parameters including time and power of application [Citation54]. As the use of microwaves is not dependent on the completion of an electric circuit it allows multiple applicators to be used simultaneously [Citation51]. Phenomena such as water vaporization, tissue contraction, and desiccation have been reported and may be unique to the use of microwaves due to the higher temperatures that can be achieved.
One of the limitations of microwave application is the loss of microwave energy as a result of the electromagnetic waves spreading in tissues due to high water content. Technical issues such as shaft heating, underpowered systems, large diameter probes and difficulty in predicting the shape and size of the ablation zone have previously limited clinical translation [Citation55] although technology developments have since overcome some of these limitations. Moreover, the technique requires CT guidance, an interventional radiologist, anaesthetic, and nursing team. Cost of treatment by microwave ablation of 3 cm kidney lesions has been calculated at about $8000 [Citation56].
Microwave sensitive carrier systems such as nanocarriers can help in efficient use of microwave energy as microwaves can induce enough heat in tumors for drug release to be achieved, avoiding prolonged heating required for ablation [Citation51]. The combination of TSLs with microwave surface applicators is in clinical trials for recurrent chest wall cancer [Citation57] (see section 5). The combined therapy showed objective responses in heavily treated patients in these clinical trials. Future clinical trials will explore how the combination works in less advanced patients.
Each of these modalities has its own benefits and limitations, (as summarized in Supplementary Table S1). It is likely that the advocates of these different approaches will continue to drive forward and optimize clinical testing and translation, and each technology may ultimately find its niche ablation application or indication. However, there is also strong scientific and commercial rationale for developing these technologies in combination with thermosensitive drug delivery agent, as discussed in the following sections.
4. Preclinical studies of heat induced release from liposomes
The previous sections have established the value of triggered release, the advantages of instigating it using heat and described some of the technologies that have been applied to achieve heating. In this section the pre-clinical data relating to the combination of heat with heat-labile drug carriers is assessed. The reports are critiqued as a means of setting the context for the clinical studies which have followed. As there are reviews already reporting the discovery and development of Thermosensitive carriers this content is placed in the Supplementary Table S2 and this following text section will focus on more recent approaches with multimodal carrier systems.
4.1. More complex multicomponent carriers
Beyond the relatively simple and readily translatable studies discussed in the Supplementary Table S2 a range of research using more complex formulations and combinations of drugs, delivery stimuli and monitoring technologies have also been reported. Some studies have sought to combine the approach of heat sensitive carriers with other targeting, imaging or therapeutic modalities. For example, Peng and coworkers developed magnetic drug targeting for co-delivery of Dox and SATB1 shRNA using thermosensitive magnetic cationic liposomes (TSMCL) incorporating iron and ammonium sulfate (liposomal magnetofection). The anti-tumor activity of the system was evaluated in a murine xenograft MKN-28 cell gastric cancer model using external magnetic field of 5000 Gauss positioned on the tumor for magnetic targeting. Mice were injected with free Dox, TSMCL-DOX, TSMCL-shSATB1, TSCL-DOX-shSATB1 or TSMCL-DOX-shSATB1, with normal saline used as control. Loading of the shRNA did not affect the thermosensitive release of Dox, the formulation was refined with optimization of cholesterol levels and co-delivery of shSATB1 and Dox by TSMCL showed improved anti-tumor effects [Citation58]. Dou et al. engineered thermosensitive liposomes to enhance the delivery of cisplatin with laser-based heating, with magnetic resonance imaging to provide feedback on the temperature elevations achieved within the tumor. Such magnetic resonance thermometry measured the heat through proton resonance frequency shift (PRE-shift) on a 7 Tesla MR imaging system, jointly with fiber optic temperature probe measurements. MR signals from the heated tumor give information about the highest relative signal increase as compared to the unheated tumor and also the muscle, after liposome administration which is maintained until the end of the heating duration. In murine ME-180 cell models, tumor heating pattern was confirmed by the magnetic resonance thermometry, with preheating for 5 minutes prior to administration and 20 minutes after dosing, achieving temperatures of 42°C. Effective release of cisplatin, and ultimately improved therapeutic efficacy, was reported compared to unheated tumor controls. Whilst light-based heating may be limited by penetration depths the authors stated that their custom-made heating apparatus was designed to heat tumors of 5–7 mm in the largest dimension but could potentially be modified to heat larger tumors [Citation59]. Kono et al reported work on preparation of polymer-modified liposomes to control temperature sensitivity and hence drug targeting. Among different thermosensitive polymers, poly(N-isopropylacrylamide) [poly(NIPAM)] has shown promising results [Citation60]. Whilst MR provides useful feedback on the heating achieved it adds a level of expense and complexity to potential clinical translation. Kokuryo et al. investigated multimodal thermo-sensitive polymer-modified liposomes (MTPLs) containing poly[2-(2-ethoxy)ethoxyethyl vinyl ether (EOEOVE)] as theranostic nano-devices to provide feedback on the delivery achieved. They encapsulated Dox, fluorescent dye, and magnetic resonance contrast agent in the MTPLs and used RFA exposure to achieve heating. Dosing was achieved by delivering a large volume (0.3 mL) of MTPLs via the tail vein whilst the mouse remained in the MRI scanner. Results in a Balb/C nude mouse model showed accumulation in kidney and liver tumor cell lines was enhanced (p < 0.05) for 4–12 hours after mild heating (42.5°C) as compared to untreated MTPLs without heating, and heating without MTPLs showing no signal. In accordance with this finding the magnetic resonance signal showed a pattern of increased tumor signal upon heating. The role of heating in both facilitating drug release and also enhancing entry of drugs into tumor cells by altering membrane properties, was noted [Citation61]. Lu and coworkers developed a formulation of thermosensitive liposomes to carry the anthracycline idarubicin. It was hypothesized that the hydrophobicity of idarubicin could improve its release from liposomes and in turn give better cellular uptake when combined with hyperthermia. In BLM melanoma bearing mice, intravital microscopy imaging showed efficient in vivo intravascular triggered release under water bath induced mild hyperthermia (42°C) and enhanced uptake by tumor cells. This formulation also overcame the leakage problem previously reported with idarubicin [Citation62], specifically when using cholesterol containing liposomes [Citation63]. Yu et al. used gold nanoparticles and thermosensitive liposomes to try and improve the spatial accuracy of heating and the level of tumor accumulation [Citation29]. In a rather complex approach, gold nanorods were PEGylated and their accumulation in the tumor by EPR was then hoped to provide a means of generating localized heating in response to near infrared (NIR) exposure. Liposomes were formulated to encapsulate ammonium bicarbonate and thereby produce CO2 bubbles under hyperthermia with the intention of increasing the level of membrane disintegration and Dox release. In vitro, and in vivo experiments using MDA-MB-435 cells in nude mice, showed high cytotoxicity and improved tumor selectivity of thermosensitive liposomes when used with gold nanorods, when compared to a saline, free DOX, low temperature sensitive liposomes and high temperature-sensitive liposomes +NIR. The recorded decrease in the tumor blood flow and vascular density was enhanced by heat sensitive liposomes with NIR, but without gold nanorods included [Citation29]. In a yet more involved strategy, Lin et al. designed a novel targeting system with a triple-pronged approach comprising magnetic fluid Fe3O4, thermosensitive lipids and Dox with cell penetrating peptides (CPPs). In in vivo experiments using an MCF-7 xenograft murine model the Dox-CPPs (comprised of the sequence (CGRRMKWKK)-thermosensitive magnetic liposome formulation showed a 1.3-fold increase in anti-tumor efficacy as compared to Dox-CPPs/TSLs, a level of enhancement that may not justify the extra complexity of Fe3O4 inclusion. So although Dox-CPPs/TSMLs under a magnetic field, showed improved tumor accumulation and delayed tumor progression in the early stage [Citation64], the increasing complexity may ultimately limit scale-up and feasibility of clinical translation.
Santos et al. used short bursts of heating by a HIFU+HT in vivo to try and overcome the limitations of long heat exposures during clinical trials of HIFU induced HT treatments using TSL. In a murine FaDu model, the amount of drug delivered by a short burst (30 seconds) of heating to 42°C achieved by HIFU was about half of that achieved with 20 mins of continuous HIFU induced HT at 42°C. Crucially the short burst heating technique can be used to enhance tumor response for clinical purposes where continuous heating can cause damage [Citation65]. Centelles et al. also found short burst of hyperthermia useful for maximum tumor drug accumulation when they used imageable thermosensitive liposomes to deliver the drug, topotecan in murine cancer models. They applied mild hyperthermia (42°C) induced by two HIFU exposures, once for 3 mins and also at 30 mins post I.V administration. It was rationalized that the first heating would provide intravascular release and the second would provide a combination of intravascular release and interstitial release for TSLs already present in the tumor [Citation66]. Markedly enhanced TSLs uptake was seen as a result of heating (p < 0.05 t-test). Elk et al. found that thermosensitive liposomes grafted with cholesterol-conjugated poly(N-(2-hydroxypropyl) methacrylamide (chol-pHPMA) are not rapidly cleared from the circulation after injection, don’t induce detrimental biological responses and do not activate platelets in buffered solution and whole blood. The potential of this formulation to be used as carrier system under hyperthermia therefore seems high [Citation67]. Lyu et al. prepared lysolipid containing thermosensitive liposomes MATT-LTSL (MATT 86/DPPC 10/DSPE-PEG20004) to deliver the MMP inhibitor, merimastat (MATT), to the tumor environment to inhibit matrix metalloproteinase activity. After exposure to water bath induced hyperthermia (42°C, 45 min) the MATT-LTSL treatment group showed approximately half the 4T1 tumor growth rate compared to the control saline treatment group. Although merimastat showed low cytotoxicity against cancer cells rapid release of payload and therefore efficient delivery inside the micro vessels in the tumor was observed [Citation68]. Supplementary Table S3 provides a breakdown of some of the important aspects of the studies discussed in this section.
It is notable that whilst the complexity of the carrier systems and modes and regimes of dosing and activation have increased, there is still a lack of fundamental understanding of the mechanisms of tumor delivery. This is exemplified by the recent debate about the scale and nature of the enhanced permeability retention effect and the proposed alternative mechanisms [Citation8,Citation13,Citation14]. Indeed, the mechanism of the passage of liposomes across or through the tumor endothelium has still to be fully defined. Sindhwani et al. [Citation14] recently proposed that the transport of nanoparticles into solid tumors is not dominated by passive transport through gaps in the endothelium, but by an active transcytosis process. Four different cancer models were used to probe the mechanism of transport and the results obtained showed a vast discrepancy between the number of endothelial gaps that would be needed to permit passive diffusion and the number of gaps in tumor endothelium actually present. Such studies are crucial in building a true picture of the barriers faced in trying to achieve delivery to solid tumors and similar studies probing the impact of heating the tumor would be an important step for the field of thermolabile drug carrier development. Such fundamental understanding is an important precursor to achieving optimal clinical and commercial translation, as understanding the mechanism of transport helps understand how heat may impact upon, and hopefully enhance it. However, despite these remaining questions, there has been progress in trialing some of the earliest developed thermolabile liposomal formulations and this is detailed below.
5. Clinical trials of heat induced release from liposomes
The analysis performed here identified 12 clinical trials (see ) that have investigated the use of thermosensitive liposomes. In addition, Wood et al. [Citation69] carried out phase I dose-escalated study to test thermosensitive liposomes for hepatic malignancies which was reported in the literature. The main objective of the study was to determine safe maximum tolerated dose (MTD), dose limiting toxicity (DLT) and pharmacokinetic profile of LTSL administered systemically in direct combination with RFA for induction of thermal ablation and drug release.
Table 2. Description of clinical trials discussed in section 6 along with their identifier number, status of the study, date of publication, drug used, disease targeted and heating modality as of January 2022, all trials involved the delivery of the drug dox.
The biggest problem associated with RFA as a monotherapy is the recurrence of disease at the treatment margins. Specifically, tumor sizes greater than 3 cm have a greater chance of local recurrence. This risk is attributed to the presence of untreated microscopic disease. Wood and coworkers therefore sought to combine chemotherapy and RFA to minimize the recurrence effect and maximize the drug delivery from liposomes. LTSL were used to minimize the systemic toxicity of the chemotherapy used. Pre-clinical data [Citation49] and mathematical models suggest that beyond the ablated tumor core near the RFA probe, there is a zone of mild hyperthermia in the same region which tends to seed recurrent disease. Using RFA to ablate the tumor core and the mild hyperthermia in the periphery to release cargo from LTSL was rationalized as an effective approach.
Six dose levels: 20, 30, 40, 50, 60 and 70 mg/m2, were administered with 3–6 patients per dose level. All the patients had unresectable primary/metastatic liver tumors with a diameter less than 7 cm, and not more than 4 lesions. LTLD was administered IV over a period of 30 mins and RF ablation was applied with a probe 15 mins after starting a 30 mins LTLD infusion. To avoid non-targeted drug release as a result of general elevation of body temperature and heating of skin, patients were covered with cooling blankets. Patients were evaluated over the first 24 hours, and at 48 hours intervals thereafter depending on clinical indications. Laboratory and imaging assessments were repeated every 3 months in the first year and in the 2nd year every 6 months.
A 50 mg/m2 dose was established to be the maximum tolerated dose (MTD) based on 3 dose limiting toxicities (DLTs) observed in patients. Two DLTs related to alanine aminotransferase (ALT) increase with a grade 4 neutropenia at 60 mg/m2 dose. The 3rd DLT was a grade 4 neutropenia at 50 mg/m2. The peak of Dox concentration was achieved at 30 mins after the start of infusion from which point plasma concentration decreased with a half-life of 0.92 hour. More than 92% of drug was released within 3.5 hours. Plasma pharmacokinetics show that at the MTD cohort of 50 mg/m2 RF ablation was applied for 2.1 hours. RF was turned on for 56% of the overall ablation time due to intermittent application. Following infusion during the first three hours almost 90% of liposomal Dox plasma area under the curve (AUC0- ¥) was observed, establishing that it is the optimal time to apply RFA. This study therefore served to establish crucial dosing and heating parameters for many of the studies that have followed.
Another phase I dose escalation study was also carried out to test drug delivery under RFA hyperthermia for the treatment of primary and metastatic tumors of the liver. 30 patients with age 18 or above, ECOG performance status 0–2, life expectancy of at least 3 months, platelet count ≥ 75,000/mm3 and WBC ≥ 1,500/mm3 were enrolled to this study. Patients had no more than 4 lesions (less than 7 cm in maximum diameter). Primary outcome of the study was to determine MTD also pharmacokinetics and pharmacodynamics at 15, 30, 45, 60, 75 minutes, at a range of time-points up to 8-days following infusion of lysothermosensitive liposomal Dox. Patients received LTSL by IV over 30 mins at 20 mg/m2 and RFA was applied for 12–60 mins after 15 mins of Dox infusion. Tumor treatment was deemed a success, however Hong et al. described in a case study from this trial [Citation21] that CT imaging minutes after treatment showed a 34 × 25 mm thermal lesion of devascularization after completion of ablation. Scans from the same patient showed 53 × 29 mm devascularization after one month. The reason behind increase and delay in the ablation zone may be attributed to chemoablation in the peripheral zone of hyperthermia. On-going cytotoxic chemotherapeutic effect, altered atrophy of necrotic cells or adjacent hepatocyte hypertrophy caused by chemotherapy might explain increase in the devascularization zone [Citation21]. Whilst a larger ablation zone is welcome, such devascularization could potentially pose a challenge to delivery of drug across the entire tumor, perhaps as evidenced in HEAT trials. Indeed, it is possible to envisage a situation where RFA ablation of a tumor and the vasculature feeding it within the central ablative zone prevents delivery of liposomal drug to the entire tumor thereby preventing exposure and release, a situation which may not be accurately predicted in much smaller scale animal models.
To evaluate this drug/device further, a placebo, randomized controlled phase III trial was conducted. This Phase III ‘HEAT’ clinical trial (identifier number NCT00617981) was carried out in 701 patients in 55 centers across the globe with inoperable hepatocellular carcinoma (HCC) with tumor sizes between 3 and 7 cm. The aim was to investigate the effectiveness of a 50 mg/m2 dose of ThermoDox in combination with RFA. All the patients enrolled were above the age of 18 with one to four unresectable HCC lesions. This study had two arms to compare RFA+LTLD treatment to RFA + dextrose alone. Patients were randomly and blindly administered 30 mins IV infusion of either dextrose in water or 50 mg/m2 LTLD. RFA was applied after 15 mins of this infusion and completed within 3 hours. Patients had CT scan 14 days prior to treatment to confirm HCC and 28 days after to evaluate initial complete response. CT scans were also performed at 3, 5, 7, 9 and 12 months followed by every 3 months until progression. Patients with incomplete ablation were re-treated at the 21st day after initial treatment. The primary end point was progression free survival (PFS) based on the independent radiological assessment and the secondary end points were overall survival (OS), patient-reported outcomes (PRO), safety and time to local recurrence. RFA + LTLD treatment was found to be as safe as RFA+LTLD and RFA alone both had reversible myelosuppression and addition of LTLD did not show any increase in cardiac toxicity, which is a common cumulative side effect when using free Dox. However, unfortunately response outcomes were not met, intention to treat analysis recorded 0.96 (p = 0.67) hazard ratio (hazard rate ratio in the treated versus controlled group) for PFS of RFA + LTLD as compared to RFA alone and 0.95 (p = 0.67) for OS HR. Sub-group analysis revealed patients with solitary lesions and prolonged heating appeared to receive greater benefit [Citation70]. The role played by LTSL was not established in this study, but preclinical studies and computational models have shown that Dox concentration in the target tissue increases with increase in hyperthermia duration [Citation49], 75% of Dox is released in first 45 mins and the remaining 25% releases in next 75 mins [Citation71]. In this HEAT study all the patients with one lesion had RFA dwell time >45 mins and patients with multiple lesions had not sufficient time to heat the tumors for more than 45 mins, hence this may be a cause of suboptimal Dox distribution. It also explains the absence of marked effect of addition of LTLD on the overall treatment population. Although HEAT failed to reach its primary endpoint of improvement in progression free survival (PFS) of at least 33%, on the basis of favorable subgroup analysis of data obtained from the study, and in order to acquire further clinical validation, a placebo controlled, double blinded, randomized phase III trial ‘OPTIMA’ (NCT02112656) was designed to optimize RFA dwell time.
In the OPTIMA trial 556 patients were IV dosed with ThermoDox and RFA was applied for 45 mins or longer to treat HCC in patients with lesion sizes of 3–7 cm. Primary endpoint of the study is overall survival and secondary endpoints are safety, PFS and time to disease progression. The subgroup of HEAT trial patients which received more than 45 mins of RFA showed median time to death of 7.5 years and 2 years survival benefit in their follow up for 2.5 years as compared to the control group. OPTIMA trial’s study design is based on this subgroup. As of August 2019, median PFS reached 17.3 months for OPTIMA study which is extended compared to the median PFS (16.8) of the 285 patients with dwell time > 45 mins in the HEAT study subgroup [Citation72,Citation73]. Hazard ratio for this subgroup was 0.63 whereas hazard ratio for OPTIMA study’s first analysis was 0.70 which doesn’t mark a substantial difference [Citation72]. However, the field awaited the OPTIMA results with great anticipation but unfortunately the trial was ultimately ceased following the recommendation of an independent data monitoring committee based on the analysis of second preplanned interim analysis for reasons of futility [Citation74]. In Aug 2020 a decision was made to continue to monitor patients on the grounds of data maturity issues.
Two phase I trials (Trail A & B (DIGNITY)- NCT00346229, NCT00826085) were performed to explore the feasibility of using thermolabile drug delivery in the treatment of chest wall recurrence (CWR) in breast cancer [Citation57]. These trials were designed to treat patients whose previous treatment failures made the choice of next-line systemic agents and modalities difficult to identify. The primary endpoint of these trials was to determine MTD and the secondary endpoint was to characterize the safety and pharmacokinetic profile of LTLD in every dosing cycle and also to compute the local response rate. All the patients enrolled in these trials were females (above 18 and not pregnant) with recurrent or metastatic adenocarcinoma <3 cm in largest dimension, left ventricular ejection fraction >50% and with Zubrod performance status of 0–1. Trial A enrolled 18 and trail B enrolled 11 patients. Both trials A + B were 3 + 3 dose finding studies, with all patients given LTLD every 21–35 days in six cycles. In trial A, an initial dose of 20 mg/m2 and sequential doses of 30, 40, 50 and 60 mg/m2 were administered intravenously over the period of 30 mins whereas in trail B, 40 and 50 mg/m2 doses were used with the previously identified MTD of 50 mg/m2 not exceeded. After 30–60 mins of LTLD infusion, microwave hyperthermia was applied. For trial A, 13 patients and in trial B 10 patients were evaluable for MTD. Non-evaluable patients withdrew due to progression of disease. In trial A one patient experiencing grade 2 hypersensitivity reaction and 2 patients with grade 4 neutropenia experienced a DLT. Whereas in trial B one out of 6 patients had a DLT at 50 mg/m2. After six LTLD treatments and a prior anthracycline exposure of 240 mg/m2 one asymptomatic decline in LVEF was observed. Other than this there were no clinically significant cardiac toxicities observed in the trials. Although the primary end point was not met, the combined local response rate was 48%, which indicates it can be further improved in future studies. Ultimately the LTLD + hyperthermia procedure was found to be safe and local control of tumor growth was reported in almost half of the patients. It was suggested that patients with less advanced disease might show better results for this intervention. It has been demonstrated in several preclinical studies (see section 5) that rather than heating after drug administration, heating during drug administration can lead to as much as two-fold increase in drug delivery because LTLD has considerably shorter half-life (35 mins) as compared to Dox (20–48 hours) and DOXIL (55 hours) [Citation57], and co-heating provides a stimulus for both vascular dilation and drug release.
On the basis of the results of trials NCT00346229 and NCT00826085, a phase 2 study NCT02850419 (EURO-DIGNITY) was initiated to investigate the tri-modal approach to treat locoregional recurrence of breast cancer using LTLD, hyperthermia and radiotherapy. This study was terminated before reaching the endpoint, probably due to funding problems and results remain unpublished.
Another interventional clinical trial (NCT03749850, i-GO) is in the process of recruitment to test delivery of Dox by LTLD with cyclophosphamide and local hyperthermia produced by MR-HIFU for the treatment of metastatic breast cancer. This is a single arm study with 12 patients who have not received chemotherapy previously. Patients with de novo stage IV HER-2 negative breast cancer are eligible for the trial. The protocol involves 6 cycles with 21 days interval of 50 mg/m2 administration during MR-HIFU induced hyperthermia applied for 60 mins (40–42°C) and subsequent 600 mg/m2 cyclophosphamide administration. Safety, feasibility and tolerability are the primary end points. Efficacy based on the radiological response of distant metastasis and local tumor.
A phase I Clinical trial (NCT02536183) is also in the recruitment stage for LTLD delivery with MR-HIFU induced heating in children and young adults with refractory or relapsed solid tumors, comprising 2 parts. Part A is to determine MTD and recommended phase 2 dose (RP2D) of LTLD in ablation and peri-ablation zone under MR-HIFU induced hyperthermia. Part B will check LTLD delivery in an expanded cohort.
Another interventional study (NCT00441376) tested ThermoDox delivery for the treatment of primary and metastatic liver tumors using RFA as heat source. ThermoDox was administered over period of 30 mins under RFA to determine MTD, pharmacokinetics and safety of ThermoDox in combination with RFA. Secondary outcomes of the study were assessing any anti-tumor activity and recurrence, determination of post ablation lesion volume and cardiotoxicity of Thermodox. Results from this trial have yet to be published.
A phase II trial (NCT01640847) was designed to evaluate treatment combining ThermoDox and HIFU to reduce patient’s burden with painful bone metastases, breast cancer, small & non- small cell lung cancer and adenocarcinoma. The reasons for the withdrawal of this trial are not clear.
An open label phase II trial (NCT01464593, ABLATE) was performed to evaluate the use of ThermoDox in conjunction with thermal ablation induced by RFA to treat metastatic Colorectal Cancer (mCRC) liver lesions. All patients were above the age of 18, with LVEF ≥ 50% and ECOG performance status ≤ 2 and had at least 1 unresectable mCRC liver lesion at the baseline with clinical indication for RFA. The study was designed to administer intravenous 50 mg/m2 Thermodox for 30 mins with thermal ablation being applied after 15 mins of drug infusion. The primary end point was determination of the effect of drug and hyperthermia on tumor growth while the secondary outcomes were evaluation of safety, time to local recurrence and overall survival time. It was terminated for unknown reasons.
Lyon et al. presented a first-in-human Phase I study to assess safety and drug delivery in liver tumors using Thermodox in combination with HIFU for targeted mild hyperthermia (NCT02181075, TarDox) [Citation75]. This trial design incorporated intratumoral temperature monitoring and ensured drug accumulation and release could be quantified [Citation76]. Patients with chemorefractory primary liver tumors and advanced liver metastasis (suitable for ultrasound and radiological intervention) were enrolled in the study. All the patients had life expectancy of more than 3 months, WHO performance status 1 or lower and LVEF ≥ 50%. Patients had not had radiotherapy on the target area in the preceding 2 months. The study was divided in 2 parts. Part I involved use of an intratumoral thermometry device to identify optimal HIFU exposure parameters for different tumor locations and depths within the liver. During HIFU exposures, real time thermometry data was acquired at a central anatomical location within the target tumor. Plasma and biopsy samples of the tumors were taken pre-LTLD dosing, post LTLD but before HIFU, and post LTLD+HIFU. Based on the data from part 1 of the study, HIFU parameters were identified and validated for part 2 of the study, removing the need to implement the thermometry device. Part 2 involved the determination of the efficacy and feasibility of drug delivery without thermometry to assess the clinical behavior of noninvasive heating. The primary endpoint was to assess safety and to achieve a least a two-fold increase in total intratumoral Dox concentration in half of the participants or more. The secondary endpoints included achievement of mild hyperthermia monitored by the thermometry device implanted in patients in part 1, determination of cell viability staining after HIFU exposures (to show absence of instantaneous ablation) and assessment of clinically important bone marrow suppression and liver toxicity. The intervention did not pose any safety concerns in addition to the known adverse effects of standard Dox chemotherapy regimes alone, with 5 out of 10 patients showing self-resolving grade IV neutropenia. Noninvasive HIFU mediated hyperthermia did not cause any skin burns, off target tissue damage and appeared to be clinically safe.
Specifically, 10 patients were recruited for the study (6 for part 1 and 4 for part 2). The trial met its endpoints by demonstrating between two and ten-fold increases in Dox concentration in 70% of the patients in samples collected post LTLD +HIFU as compared to immediately post LTLD dosing at peak circulating levels of drug. The mean tumoral biopsy Dox concentration in samples of post LTLD + HIFU was 7.74 μg/g (3.3-fold times more compared to post-LTLD alone). Furthermore, the presence of nuclear Dox, as demonstrated by fluorescence microscopy, was used to evidence liposomal release upon focused ultrasound exposure. In support of this intratumoral drug distribution data PET-CT scans showed new focal regions of photopenia in several of the targeted tumors compared to pre-treatment scans in the same patient’s consequent with chemo-ablation of previously chemo-refractory tumors from a single cycle of treatment. The transport mechanisms of LTLD formulation in this study are hypothesized to be rapid diffusion of Dox into the tumor interstitium, released from the LTSL circulating in the tumor microvasculature under conditions mild hyperthermia. Ultrasound cavitation might also have a further role in the release and delivery of Dox due to microstreaming effects. The effort dedicated to confirming the required intratumoral temperatures were reached and validating that nuclear delivery of Dox had been achieved, played an important role in the success and impact of this trial [Citation76].
6. Conclusion
A large number of therapeutic agents have been tested over the last few decades for anti-cancer efficacy. Although many of these agents have demonstrated safety and activity in in vitro and pre-clinical experiments, their clinical success is often limited by their inefficient delivery to target cells in solid human tumors. The unique physiology of solid tumors makes delivering drugs into and throughout the tumor masses a major challenge. Specifically, highly disorganized vasculature increased interstitial pressure and dense extracellular matrix make the transport of therapeutic levels of drugs into tumors a real clinical challenge which remains largely unaddressed by traditional non-targeted intravenous chemotherapy infusion regimens.
Whilst encapsulation in a carrier system in the range of 80–200 nm may allow extended circulation of the drug and EPR or non-EPR mediated uptake into tumor, the particles created may be too stable to achieve effective release of their cargo upon arrival at the tumor. Studies have shown that delivery of drugs such as Dox by liposomes and triggered release within the tumor increase its therapeutic index. Liposomes offer many advantages as carrier systems because of their size, ease of synthesis, loading capacity and adaptability to such triggered release strategies. Among different kinds of triggers for instigating drug release, mild hyperthermia is showing promising results and may have synergistic effects with high-dose chemotherapy delivery. Mild hyperthermia can be achieved by different means i.e. superficial, or percutaneous microwave devices, focused ultrasound, light, and radiofrequency exposure. Many pre-clinical studies and now clinical trials have shown triggered release to be beneficial for targeted drug delivery, tumor growth retardation and survival. This accumulating body of research has revealed important considerations for future optimization of both the drug carrier system and the stimulus for hyperthermia.
Research has shown that matching the liposomal carrier system and its pharmacokinetics with the trigger is helpful in increasing the therapeutic index of drug. Indeed, it has been demonstrated that the plasma half-life of Dox is higher with non-thermosensitive liposomal Dox (10 hours) and with lyso-thermosensitive liposomal Dox (~1 hour) as compared to free Dox which has a half-life is only few minutes [Citation69,Citation77], demonstrating the provision of high blood concentrations for stimuli such as heat to impact upon. Notably, lysolipid thermosensitive liposomes (LTSL) have shown increased drug concentration at tumor sites compared to traditional thermosensitive liposomes [Citation78].
Initially observed issues with premature release and instability even at the physiological temperatures was dealt with by composition and coatings optimization. Whilst composition also influenced efficacy with different DPPC, HSPC, MSPC and PEG2000-DSPE ratios showing differences in drug delivery and reduction in tumor size in vitro and in vivo.
Initial translation of thermosensitive liposomes was limited mainly due to inadequate heating modalities. Different modalities such as microwaves, radiofrequency, focussed ultrasound and near infrared light can be used for creation of hyperthermia. Each modality has its own pros and cons and has to be adjusted carefully according to the method for a given tumor type and body location. Hyperthermia modalities are typically complex, costly and require much clinical expertise. Among all the different formulations so far proposed, only ThermoDox, originally developed by Needham and Dewhirst, has entered clinical evaluation to date following remarkable efforts. Indeed, ThermoDox has maintained its progress toward clinical translation whilst many more complex and involved formulations with what might be considered more compelling pre-clinical data have stalled. This is likely a consequence of manufacturing, scale-up and pharmacovigilance challenges. However, regardless of the heating approach used, the large improvement seen in preclinical studies of thermosensitive liposomes plus chemotherapy as compared conventional chemotherapy alone, has perhaps not been fully recapitulated in all clinical trials. Indeed, although the pre-clinical data has allowed researchers to settle on ThermoDox as the formulation of choice to form the vanguard for the approach, no similar commitment to a single heating modality and dosing/heating strategy has been made, although there is promising and confounding data resulting from trials using RFA, microwave and HIFU. In addition, the number of patients under treatment in the trials performed has typically been low, and patient cohorts on different trials are often of different age groups and are under treatment in different centers around the world. Rationalizing these aspects might give a better and more complete and reliable perspective of relative success. Ultimately a direct head-to-head comparison of different modalities in the same patient cohort with the same dosing regimen would be of great use, but the complexity of running such a trial and ensuring the equipment and expertise for all modalities is available, make it unlikely.
Another reason for the lack of clear clinical progression of the TSL + device paradigm may relate to the EPR effect. The dogma of EPR mediated delivery meant this was considered to be an important aspect of the strategy, with dosing and heating timings designed around the need to allow a level of passive accumulation before heating was triggered. Recent questioning of the role and scale of the EPR in animal models, seems to fit with the enhanced results obtained in studies where heat is instigated whilst drug + carrier blood concentrations are at their highest [Citation71]. Clinical trials have shown that the results predicted by pre-clinical studies have not been fully translated to the clinic for many reasons e.g. expenses of clinical trials, need for improving HT technologies, suboptimal trial design etc. However, thermolabile liposomes along with appropriate heating modalities have clearly demonstrated effective delivery and better penetration of therapeutic agents. Indeed, trials which have been designed to specifically verify that intratumoral heating and delivery has been achieved are an important step in optimization of heating time, choice of heating modalities and the stage of study at which heating needs to be applied. Low-cost technologies for image guidance of treatment and real-time feedback to confirm the required level of heating has been achieved, or sophisticated modeling using anatomical data to predict exposure settings, will be important stepping-stones to achieving clinical outcomes which match the true potential of the approach, which is still anticipated to be substantial.
7. Expert opinion
Drug carrier systems robust enough to survive the delivery phase following intravenous injection have made good progress. Such systems can increase the blood residence time of small molecule chemotherapeutic agents from tens of minutes to tens of hours, potentially providing more opportunity for uptake into solid tumors. However, poor penetration of these drug carriers and their cargo into and throughout solid tumors still limits their therapeutic efficacy. Furthermore, although stability in the bloodstream is important, if the carrier is too stable the payload is not released, even if penetration into the tumor is achieved. An attractive approach to address both these limitations is to design a drug carrier which is destabilized in response to mild hyperthermia and apply localized heat at the point at which the carrier transits through the tumor vasculature. Great progress in providing heat responsive liposomal drug carrier systems has been made and the most clinically advanced of these, Thermodox, demonstrates the blood stability and triggered release characteristics required. Indeed, although some of the clinical trials outputs have been underwhelming in terms of tumor response, much crucial data defining the optimal timing, duration and coordination of heat application with Thermodox dosing, has been obtained. Such data will be important in ensuring more encouraging tumor responses in future trials. Indeed, we believe Thermodox may form the vanguard of what may eventually become a popular clinical approach. Such success will continue to encourage the development of ever more sophisticated alternative carrier systems. Crucially, when adding features and multimodality to carrier systems the impacts on manufacturing, scale-up feasibility and healthcare economics must be considered at the outset. Indeed, it could be argued that Thermodox already fulfills all the criteria required of a stimuli-responsive drug carrier, and such ‘gilding the lily’ with more functionality is a distraction when research endeavor is actually now best focussed on improving the efficiency, precision and control of the technologies used to provide heating. This point is emphasized by the fact that there is still uncertainty concerning which heat-generating technology is the most optimal to pair with Thermodox. Ultimately this argument may be settled on a cancer indication-by-indication basis, with the optimal dosing and heating regimens being determined from previous clinical trial data and the strengths and limitations of each technology. Certainly, further optimization of the heating modality to Thermodox offers a much quicker and easier route to improved functionality than the optimization of new generations of Thermodox to a particular heating modality, in terms of regulatory route and manufacturing (i.e. the ease and cost of device development vs that of drug development). A prime example of this is how passive acoustic mapping has the potential to be used as a low-cost, noninvasive, reliable proxy for successful triggered drug release, using existing approved technology without the need to modify the already scalable and regulatory approved Thermodox formulation. The alternative of incorporating imaging functionality within a new, more sophisticated thermoresponsive carrier system, seems like a less attractive option.
This review aims to provide an analysis of the pre-clinical and clinical trials data produced using heat labile drug carriers. It should therefore form a useful resource for researchers and clinicians so they can focus on the most appropriate carrier and the most appropriate heating modality, whether it be high intensity focussed ultrasound, or microwave or radiofrequency exposure, for their particular indication.
Figure 1. Mechanism of action of thermosensitive liposomes under hyperthermia. The green lining is showing lipid shell whereas drug is represented by yellow color (a). Firstly, liposomes pass through the leaky blood vessels, potentially by EPR effect (b). The big red circle is showing region of applied hyperthermia. Hyperthermia increases the vessel pore size and liposomal extravasation is increased too(c). Drug is probably released in tumor interstitium, in addition vasculature (d) and cell membrane permeability may also be increased, adapted from [Citation42].
![Figure 1. Mechanism of action of thermosensitive liposomes under hyperthermia. The green lining is showing lipid shell whereas drug is represented by yellow color (a). Firstly, liposomes pass through the leaky blood vessels, potentially by EPR effect (b). The big red circle is showing region of applied hyperthermia. Hyperthermia increases the vessel pore size and liposomal extravasation is increased too(c). Drug is probably released in tumor interstitium, in addition vasculature (d) and cell membrane permeability may also be increased, adapted from [Citation42].](/cms/asset/d3492b0e-5a16-4d4e-9029-94ba1c182fab/iedd_a_2099834_f0001_oc.jpg)
Article highlights
Appraisal of the pre-clinical data supporting triggered drug release from carriers
Description of heat producing modalities and their comparison
Appraisal of pre-clinical studies on hyperthermia induced drug release
Listing and appraisal of clinical trials of hyperthermia triggered drug release from liposomes
This box summarizes key points contained in the article.
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewer disclosures
A reviewer on this manuscript has disclosed that they are a co-founder of Thermosome, a biotech start-up focused on developing temperature-sensitive liposomes for clinical use based on the synthetic phospholipid DPPG2. Peer reviewers on this manuscript have no other relevant financial relationships or otherwise to disclose.
Supplemental Material
Download MS Word (36.7 KB)EODD-2022–0049.R1_Supplementary_Table_3_preclinical_data.docx
Download MS Word (30.5 KB)EODD-2022–0049.R1_Supplementary_Table_1_s.docx
Download MS Word (19.5 KB)Supplementary material
Supplemental data for this article can be accessed here
Additional information
Funding
References
- Cao D, Hou M, Guan YS, et al. Expression of HIF-1alpha and VEGF in colorectal cancer: association with clinical outcomes and prognostic implications. BMC Cancer [Internet]. 2009 Dec 10 [cited 2021 Jul 31]. 9(1): 432. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2797529/
- Determination of doxorubicin levels in whole tumor and tumor nuclei in murine breast cancer tumors. PubMed [Internet]. [cited 2021 Jul 31]. Available from: https://pubmed.ncbi.nlm.nih.gov/16203786/
- Zhao J, Salmon H, Sarntinoranont M. Effect of heterogeneous vasculature on interstitial transport within a solid tumor. Microvasc Res. 2007 May;73(3):224–236.
- Simonsen TG, Gaustad JV, Leinaas MN, et al. High interstitial fluid pressure is associated with tumor-line specific vascular abnormalities in human melanoma xenografts. PLoS One [Internet]. 2012 Jun 29 [cited 2021 Jul 31];7(6):e40006. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3386940/
- Heldin CH, Rubin K, Pietras K, et al. High interstitial fluid pressure - an obstacle in cancer therapy. Nat Rev Cancer. 2004 Oct;4(10):806–813.
- Skeel RT, and Khleif SN. Handbook of cancer chemotherapy. Hagerstown, MD, USA: Lippincott Williams & Wilkins; 2011. p. 896.
- Kumari P, Ghosh B, Biswas S. Nanocarriers for cancer-targeted drug delivery. J Drug Target. 2016;24(3):179–191.
- Golombek SK, May JN, Theek B, et al. Tumor targeting via EPR: strategies to enhance patient responses. Adv Drug Deliv Rev [Internet]. 2018 May [cited 2021 Jul 31];130:17–38. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6130746/
- Iyer AK, Khaled G, Fang J, et al. Exploiting the enhanced permeability and retention effect for tumor targeting. Drug Discov Today. 2006 Sep;11(17–18):812–818.
- Polymeric drugs for efficient tumor-targeted drug delivery based on EPR-effect. PubMed [Internet]. [cited 2021 Jul 31]. Available from: https://pubmed.ncbi.nlm.nih.gov/19070661/
- Maeda H. SMANCS and polymer-conjugated macromolecular drugs: advantages in cancer chemotherapy. Adv Drug Deliv Rev. 2001 Mar 1;46(1–3):169–185.
- Hollis CP, Weiss HL, Leggas M, et al. Biodistribution and bioimaging studies of hybrid paclitaxel nanocrystals: lessons learned of the EPR effect and image-guided drug delivery. J Control Release. 2013 Nov 28;172(1):12–21.
- Torrice M. Does nanomedicine have a delivery problem? ACS Cent Sci. 2016 Jul 27;2(7):434–437.
- The entry of nanoparticles into solid tumours. Nature Materials [Internet]. [cited 2021 Jul 31]. Available from: https://www.nature.com/articles/s41563-019-0566-2
- Kawai M, Higuchi H, Takeda M, et al. Dynamics of different-sized solid-state nanocrystals as tracers for a drug-delivery system in the interstitium of a human tumor xenograft. Breast Cancer Res. 2009;11(4):R43.
- Dromi S, Frenkel V, Luk A, et al. Pulsed-high intensity focused ultrasound and low temperature-sensitive liposomes for enhanced targeted drug delivery and antitumor effect. Clin Cancer Res. 2007 May 1;13(9):2722–2727.
- Seynhaeve ALB, Dicheva BM, Hoving S, et al. Intact doxil is taken up intracellularly and released doxorubicin sequesters in the lysosome: evaluated by in vitro / in vivo live cell imaging. J Control Release. 2013 Nov 28;172(1):330–340.
- Yoo J, Park C, Yi G, et al. Active targeting strategies using biological ligands for nanoparticle drug delivery systems. Cancers (Basel) [Internet]. 2019 May 8 [cited 2021 Apr 28];11(5). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6562917/.
- Estanqueiro M, Amaral M, and Conceição J, et al. Evolution of liposomal carriers intended to anticancer drug delivery: an overview. International Journal of Current Pharmaceutical Research. 2015;6(4): 3–10. ISSN: .
- Schroeder A, Honen R, Turjeman K, et al. Ultrasound triggered release of cisplatin from liposomes in murine tumors. J Control Release. 2009 Jul 1;137(1):63–68.
- Hong CW, Libutti SK, Wood BJ. Liposomal doxorubicin plus radiofrequency ablation for complete necrosis of a hepatocellular carcinoma. Curr Oncol. 2013 Jun;20(3):e274–277.
- Koning GA, Eggermont AMM, Lindner LH, et al. Hyperthermia and thermosensitive liposomes for improved delivery of chemotherapeutic drugs to solid tumors. Pharm Res. 2010 Aug;27(8):1750–1754.
- Issels RD, Lindner LH, Verweij J, et al. Neo-adjuvant chemotherapy alone or with regional hyperthermia for localised high-risk soft-tissue sarcoma: a randomised phase 3 multicentre study. Lancet Oncol. 2010 Jun;11(6):561–570.
- Zhu L, Altman MB, Laszlo A, et al. Ultrasound hyperthermia technology for radiosensitization. Ultrasound Med Biol. 2019 May;45(5):1025–1043.
- Wessalowski R, Schneider DT, Mils O, et al. Regional deep hyperthermia for salvage treatment of children and adolescents with refractory or recurrent non-testicular malignant germ-cell tumours: an open-label, non-randomised, single-institution, phase 2 study. Lancet Oncol. 2013 Aug;14(9):843–852.
- Overcoming limitations in nanoparticle drug delivery: triggered, intravascular release to improve drug penetration into tumors. Cancer Research [Internet]. [cited 2021 Aug 1]. Available from: https://cancerres.aacrjournals.org/content/72/21/5566
- Nanoparticle delivery of cancer drugs. Annual Review of Medicine [Internet]. [cited 2021 Aug 1]. Available from: https://www.annualreviews.org/doi/abs/10.1146/annurev-med-040210-162544
- Hyperthermia enables tumor-specific nanoparticle delivery: effect of particle size. Cancer Research [Internet]. [cited 2021 Aug 1]. Available from: https://cancerres.aacrjournals.org/content/60/16/4440.short
- Yu M, Guo F, Tan F, et al. Dual-targeting nanocarrier system based on thermosensitive liposomes and gold nanorods for cancer thermo-chemotherapy. J Control Release. 2015;215:91–100.
- Valle SJ, Alzahrani NA, Liauw W, et al. Hyperthermic Intraperitoneal Chemotherapy (HIPEC) methodology, drugs and bidirectional chemotherapy. Indian J Surg Oncol [Internet]. 2016 Jun [cited 2022 Apr 21];7(2):152–9. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4818620/
- Efficacy of liposomes and hyperthermia in a human tumor xenograft model: importance of triggered drug release. PubMed [Internet]. [cited 2021 Aug 1]. Available from: https://pubmed.ncbi.nlm.nih.gov/11156395/
- Funaki K, Fukunishi H, Funaki T, et al. Magnetic resonance-guided focused ultrasound surgery for uterine fibroids: relationship between the therapeutic effects and signal intensity of preexisting T2-weighted magnetic resonance images. Am J Obstet Gynecol. 2007 Feb;196(2):184.e1–6.
- Schmid FA, Schindele D, Mortezavi A, et al. Prospective multicentre study using high intensity focused ultrasound (HIFU) for the focal treatment of prostate cancer: safety outcomes and complications. Urol Oncol. 2020 Apr;38(4):225–230.
- MR-guided focused ultrasound thalamotomy for essential tremor: a proof-of-concept study. The Lancet Neurology [Internet]. [cited 2021 Aug 1]. Available from: https://www.thelancet.com/journals/lancet/article/PIIS1474-4422(13)700486/fulltext)700486/fulltext
- High-intensity focused ultrasound in the treatment of solid tumours. Nature Reviews Cancer [Internet]. [cited 2021 Aug 1]. Available from: https://www.nature.com/articles/nrc1591
- Frenkel V, Li KCP. Potential role of pulsed-high intensity focused ultrasound in gene therapy. Future Oncol. 2006 2;Feb(1):111–119.
- Staruch R, Chopra R, Hynynen K. Localised drug release using MRI-controlled focused ultrasound hyperthermia. Int J Hyperthermia. 2011;27(2):156–171.
- Henderson TA, Morries LD. Near-infrared photonic energy penetration: can infrared phototherapy effectively reach the human brain?. Neuropsychiatr Dis Treat [Internet]. 2015 Aug 21 [cited 2021 Aug 1];11:2191–2208. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4552256/
- Remote triggered release of doxorubicin in tumors by synergistic application of thermosensitive liposomes and gold nanorods. ACS Nano [Internet]. [cited 2021 Aug 1]. Available from: https://pubs.acs.org/doi/10.1021/nn201010q
- Immunotargeted nanoshells for integrated cancer imaging and therapy. Nano Letters [Internet]. [cited 2021 Aug 1]. Available from: https://pubs.acs.org/doi/10.1021/nl050127s
- Feasibility study of particle-assisted laser ablation of brain tumors in orthotopic canine model. Cancer Research [Internet]. [cited 2021 Aug 1]. Available from: https://cancerres.aacrjournals.org/content/69/4/1659
- Computationally guided photothermal tumor therapy using long-circulating gold nanorod antennas. PubMed [Internet]. [cited 2021 Aug 1]. Available from: https://pubmed.ncbi.nlm.nih.gov/19366797/
- Chen J, Glaus C, Laforest R, et al. Gold nanocages as photothermal transducers for cancer treatment. Small [Internet]. 2010 Apr 9 [cited 2021 Aug 1];6(7):811–817. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3035053/
- Gene silencing by gold nanoshell-mediated delivery and laser-triggered release of antisense oligonucleotide and siRNA. ACS Nano [Internet]. [cited 2021 Aug 1]. Available from: https://pubs.acs.org/doi/10.1021/nn301135w
- Remote control of ion channels and neurons through magnetic-field heating of nanoparticles. Nature Nanotechnology [Internet]. [cited 2021 Aug 1]. Available from: https://www.nature.com/articles/nnano.2010.125
- Liu X, He Z, Chen Y, et al. Dual drug delivery system of photothermal-sensitive carboxymethyl chitosan nanosphere for photothermal-chemotherapy. Int J Biol Macromol [Internet]. 2020 Nov 15 [cited 2022 Apr 20];163:156–166. Available from: https://www.sciencedirect.com/science/article/pii/S0141813020336448
- Raza A, Hayat U, Rasheed T, et al., “Smart” materials-based near-infrared light-responsive drug delivery systems for cancer treatment: a review. J Mater Res Technol [Internet]. 2019 Jan 1 [cited 2022 Apr 20];8(1):1497–1509. Available from: https://www.sciencedirect.com/science/article/pii/S2238785417307251
- Sasaki A, Kai S, Iwashita Y, et al. Microsatellite distribution and indication for locoregional therapy in small hepatocellular carcinoma. Cancer. 2005 Jan 15;103(2):299–306.
- Swenson CE, Haemmerich D, Maul DH, et al. Increased duration of heating boosts local drug deposition during radiofrequency ablation in combination with thermally sensitive liposomes (ThermoDox) in a porcine model. PLoS One. 2015;10(10):e0139752.
- Principles of and advances in percutaneous ablation. PubMed [Internet]. [cited 2021 Aug 1]. Available from: https://pubmed.ncbi.nlm.nih.gov/21273519/
- Microwave-triggered smart drug release from liposomes co-encapsulating doxorubicin and salt for local combined hyperthermia and chemotherapy of cancer. Bioconjugate Chemistry [Internet]. [cited 2021 Aug 1]. Available from: https://pubs.acs.org/doi/10.1021/acs.bioconjchem.6b00603
- Simon CJ, Dupuy DE, Mayo-Smith WW. Microwave ablation: principles and applications. Radiographics. 2005 Oct;25(Suppl 1):S69–83.
- Dewhirst M. Pilot study of external hyperthermia and intravesical mitomycin-C to treat recurrent bladder cancer after resection and standard adjuvant therapy [Internet]. clinicaltrials.gov; Report No.: NCT00734994; 2015 Jun [cited 2022 Apr 27]. Available from: https://clinicaltrials.gov/ct2/show/NCT00734994
- Synthesis of carbon nanotubes by microwave heating: influence of diameter of catalytic Ni nanoparticles on diameter of CNTs. Journal of Materials Chemistry [Internet]. [cited 2021 Aug 1]. Available from: https://pubs.rsc.org/en/content/articlelanding/2014/ta/c3ta13297h
- Yoo JW, Doshi N, Mitragotri S. Adaptive micro and nanoparticles: temporal control over carrier properties to facilitate drug delivery. Adv Drug Deliv Rev [Internet]. 2011 Nov 1 [cited 2021 Aug 1];63(14):1247–1256. Available from: https://www.sciencedirect.com/science/article/pii/S0169409X11000780
- Comparison of procedure costs of various percutaneous tumor ablation modalities. PubMed [Internet]. [cited 2021 Aug 1]. Available from: https://pubmed.ncbi.nlm.nih.gov/25174139/
- Zagar TM, Vujaskovic Z, Formenti S, et al. Two phase I dose-escalation/pharmacokinetics studies of low temperature liposomal doxorubicin (LTLD) and mild local hyperthermia in heavily pretreated patients with local regionally recurrent breast cancer. Int J Hyperthermia. 2014 Aug;30(5):285–294.
- Co-delivery of doxorubicin and SATB1 shRNA by thermosensitive magnetic cationic liposomes for gastric cancer therapy. [Internet]. [cited 2021 Aug 2]. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0092924
- Dou YN, Weersink RA, Foltz WD, et al. Custom-designed laser-based heating apparatus for triggered release of cisplatin from thermosensitive liposomes with magnetic resonance image guidance. J Vis Exp. 2015 Dec;13(106):e53055.
- Kono K. Thermosensitive polymer-modified liposomes. Adv Drug Deliv Rev [Internet]. 2001 Dec 31 [cited 2022 Apr 19];53(3):307–319. Available from: https://www.sciencedirect.com/science/article/pii/S0169409X01002046
- Kokuryo D, Nakashima S, Ozaki F, et al. Evaluation of thermo-triggered drug release in intramuscular-transplanted tumors using thermosensitive polymer-modified liposomes and MRI. Nanomedicine. 2015 Jan;11(1):229–238.
- Lu T, Lokerse WJM, Seynhaeve ALB, et al. Formulation and optimization of idarubicin thermosensitive liposomes provides ultrafast triggered release at mild hyperthermia and improves tumor response. J Control Release.2015 Dec 28;220(Pt A):425–437.
- Dos Santos N, Mayer LD, Abraham SA, et al. Improved retention of idarubicin after intravenous injection obtained for cholesterol-free liposomes. Biochim Biophys Acta. 2002 Apr 12;1561(2):188–201.
- Lin W, Xie X, Yang Y, et al. Thermosensitive magnetic liposomes with doxorubicin cell-penetrating peptides conjugate for enhanced and targeted cancer therapy. Drug Deliv. 2016 Nov;23(9):3436–3443.
- Santos MA, Goertz DE, Hynynen K. Focused ultrasound hyperthermia mediated drug delivery using thermosensitive liposomes and visualized with in vivo two-photon microscopy. Theranostics. 2017;7(10):2718–2731.
- Centelles MN, Wright M, So PW, et al. Image-guided thermosensitive liposomes for focused ultrasound drug delivery: using NIRF-labelled lipids and topotecan to visualise the effects of hyperthermia in tumours. J Control Release. 2018 Jun;28(280):87–98.
- van Elk M, van den Dikkenberg JB, Storm G, et al. Preclinical evaluation of thermosensitive poly(N-(2-hydroxypropyl) methacrylamide mono/dilactate)-grafted liposomes for cancer thermochemotherapy. Int J Pharm. 2018 Oct 25;550(1–2):190–199.
- Lyu Y, Xiao Q, Yin L, et al., Potent delivery of an MMP inhibitor to the tumor microenvironment with thermosensitive liposomes for the suppression of metastasis and angiogenesis. Sig Transduct Target Ther [Internet]. 2019 Aug 9 [cited 2021 Aug 2];4(1):1–9. Available from: https://www.nature.com/articles/s41392-019-0054-9
- Wood BJ, Poon RT, Locklin JK, et al. Phase I study of heat-deployed liposomal doxorubicin during radiofrequency ablation for hepatic malignancies. J Vasc Interv Radiol. 2012 Feb;23(2):248–255.e7.
- Tak WY, Lin SM, Wang Y, et al. Phase III HEAT study adding lyso-thermosensitive liposomal doxorubicin to radiofrequency ablation in patients with unresectable hepatocellular carcinoma lesions. Clin Cancer Res. 2018 Jan 1;24(1):73–83.
- Gasselhuber A, Dreher MR, Partanen A, et al. Targeted drug delivery by high intensity focused ultrasound mediated hyperthermia combined with temperature-sensitive liposomes: computational modelling and preliminary in vivovalidation. Int J Hyperthermia. 2012;28(4):337–348.
- Celsion Reports Unanimous Independent Data Monitoring Committee Recommendation to Continue the Phase III OPTIMA Study of ThermoDox® in Primary Liver Cancer [Internet]. [cited 2021 Aug 2]. Available from: https://finance.yahoo.com/news/celsion-reports-unanimous-independent-data-130000797.html
- Celsion Corporation Reports Second Quarter 2019 Financial Results and Provides Business Update. Celsion Corporation [Internet]. [cited 2021 Aug 2]. Available from: https://investor.celsion.com/news-releases/news-release-details/celsion-corporation-reports-second-quarter-2019-financial
- Phase 3 OPTIMA Trial in HCC to Continue to Follow Patients for OS [Internet]. OncLive. [cited 2022 Jan 14]. Available from: https://www.onclive.com/view/phase-3-optima-trial-in-hcc-to-continue-to-follow-patients-for-os
- Lyon PC, Griffiths LF, Lee J, et al. Clinical trial protocol for TARDOX: a phase I study to investigate the feasibility of targeted release of lyso-thermosensitive liposomal doxorubicin (ThermoDox®) using focused ultrasound in patients with liver tumours. J Ther Ultrasound. 2017;5(1):28.
- Lyon PC, Gray MD, Mannaris C, et al. Safety and feasibility of ultrasound-triggered targeted drug delivery of doxorubicin from thermosensitive liposomes in liver tumours (TARDOX): a single-centre, open-label, phase 1 trial. Lancet Oncol [Internet]. 2018 Aug 1 [cited 2021 May 15];19(8):1027–1039. Available from: https://www.thelancet.com/journals/lanonc/article/PIIS1470-2045(18)30332-2/abstract
- Gabizon A, Shmeeda H, Barenholz Y. Pharmacokinetics of pegylated liposomal Doxorubicin: review of animal and human studies. Clin Pharmacokinet. 2003;42(5):419–436.
- Bi H, Xue J, Jiang H, et al. Current developments in drug delivery with thermosensitive liposomes. Asian J Pharm Sci [Internet]. 2019 Jul 1 [cited 2021 Aug 2];14(4):365–379. Available from: https://www.sciencedirect.com/science/article/pii/S1818087617307419