ABSTRACT
Introduction
Inhalation of herbs and other compounds has a long history but habits for medical treatment are intertwined with rituals to obtain hallucinatory effects and pleasurable sensations. Several examples of inhaled herbs, and the diseases they were used for, based on early translations of ancient manuscripts related to inhalation were found to be speculative and inconsistent with each other in literature. They needed to be reconsidered and verified with the original sources of information.
Areas covered
Examples of ancient inhalation and the development of early dry powder inhalers up to and including the first half of the twentieth century. Databases used for literature about historic events, ancient habits, and ancient science, included SmartCat, JSTOR, and ANDAT; various facts were verified via personal communication with historians and custodians of historic manuscripts and artifacts.
Expert opinion
Inhalation does not necessarily require active creation of inhalable aerosols, smokes or fumes. Inhaling ‘healthy air’ with volatile and gaseous components, or fine aerosols in pine forests, on volcano slopes and at the seaside must be considered as inhalation therapy too. From this viewpoint, inhalation therapy may have been much more common and widespread and have a longer history than is currently known from written evidence.
1. General introduction
Several manuscripts are known in which the history of pulmonary drug delivery in general and that of dry powder inhalation more specifically have been addressed [Citation1–16]. Therefore, a repetition of historical facts does not seem necessary. However, by comparison of these previous manuscripts with each other, it occurred that there are inconsistencies in the details given, as well as some incorrect interpretations of the facts, particularly regarding some most ancient examples of inhalation. We believe that this is partly the result of referring to each other instead of to the original sources, which is understandable because the original information is often difficult, if not impossible, to gain access to. Inaccuracies in older manuscripts may also be the result of new information, as for instance from improved translations, which has become available since they were published, or from more scientific interpretations of ancient manuscripts and artifacts. This, for instance, is the case for the Papyrus Ebers, a frequently cited ancient document about inhalation from about 1500 BCE. In Paragraph 2.2 it is explained why previously published information about this papyrus has to be reconsidered and there are a few more examples of ancient inhalation in this review manuscript for which new, or additional information has been found.
To be different from other previous reviews, the past of dry powder inhalation has been written in the context of societal, technical and scientific developments and innovations that are known to have been of great influence on dry powder inhaler (DPI) development. These events are presented in two different parts, covering two different time periods, this first part addressing the ancient history and some precursors to modern DPIs. Frequently, innovations require a facilitating development that is not directly related to the invention itself. We divided these developments in drivers, those making improvements in pulmonary drug delivery desired or necessary, and enablers, those making such improvements possible. To our knowledge, such a link between various events and developments has never been made before for the history of inhalation technology. A striking example, although not yet for inhalation, is the vaccine development to curb the SARS CoV-2 pandemic that started in December 2020. The necessity to scale down the catastrophic spread and the effects of this deadly disease (as driver) pushed the development for vaccines to an unprecedented speed and this was possible thanks to a series of landmark experiments (the enablers) since the 1960s [Citation17]. They include the discovery of messenger RNA (mRNA) in 1961, the development of liposomes in 1965, their use for drug (1971) and vaccine (1974) delivery, the combination of mRNA and liposomes (1977) and several more successive steps as reviewed by Salmin et al. [Citation18]. Also, effective nebulization at home became first possible after completion of the household electrification in the beginning of the 20th century [Citation19]. Similarly, the mass production of easy to use, robust and portable DPIs required the invention and cheap production of suitable plastics first, and a lot more as will be discussed in Part 2 of the modern history and the present of DPIs [Citation20]. In fact, many drug, vaccine and inhaler ‘inventions’ were not really new when they could successfully be introduced to the market. Instead, they were improvements, or applications of already existing concepts, principles, and ideas that could be realized first when the enablers made it possible. Therefore, in many cases, it is better not to use the fashionable term ‘technology driven,’ but to speak of ‘technology enabled’ developments.
2. Ancient history of pulmonary drug therapy relevant to dry powder inhalation
In the early history, pulmonary therapy is intertwined with habits and rituals to obtain hallucinatory effects and pleasurable sensations. Many herbs used for combustion, smoking, or heating to release their volatile components are not only known for their therapeutic value, but also for their psychiatric effects, often leading to an addiction [Citation21–24]. Well-known examples are Ephedra sinica containing epinephrine, the nightshade species Datura stramonium (thorn apple) and Hyoscyamus Niger (black henbane or stinking nightshade) both with atropine, Papaver somniferum for opium containing noscapine and morphine, Cannabis sativa with tetrahydrocannabinol (THC) and cannabidiol (CBD), and Nicotiana tabacum (tobacco) with nicotine. Columbus already observed in 1492 that growing and smoking tobacco by native Americans was variably practiced for the treatment of ills and for its pleasurable effects [Citation25]. The rapidly increasing popularity of the asthma cigarette (e.g. with stramonium, lobelia, tobacco, and potash) among patients with asthma in the late 1800s coincided precisely with a growing interest in smoking cigarettes with cannabis and opium for both recreational and medical purposes [Citation26]. Examples like these mark the very thin line between medical and recreational inhalation. It may, therefore, be questioned whether all examples of inhaling vapors, fumes, and smokes from the past should be considered significant examples for the evolution of pulmonary therapy. On the other hand, the beneficial effects from inhaling salt air at the seaside or in salt mines, or those from inhaling the wholesome volatile organic compounds (e.g. limonene and pinene) in pine forests is often disregarded in recent historical reviews [Citation27.Citation28]. Greek soldiers with tuberculosis of the lungs were sent to the pine forests of Libya to inhale these volatile compounds for recovery around 1000 BCE [Citation29]. Also, the Greek/Roman physician Claudius (Clarissimus) Galenus (129 to approx. 200 CE), in the English literature mostly referred to as Galen (of Pergamon), recommended his patients to breathe the sulfuric vapors arising from cracks in the slopes of the Vesuvius, or make a sea voyage for the treatment of tuberculosis [Citation30,Citation31]. The difference with other examples given in literature is that these patients did not create the salutary air themselves, as for instance by combustion or heating of plant materials. Instead, they went to a place where it is naturally present. It may be expected that much older peoples and tribes have recognized the potential health benefits of inhaling certain airborne biogenic substances too, but for the prehistoric period it is difficult to find evidence for habits that did not leave artifacts to be found. From this viewpoint, the inhalation therapy is probably considerably older and much more widespread than any of the milestones mentioned in previously written manuscripts. Frequently, the third millennium BCE is considered the earliest date giving proof of pulmonary drug delivery in the form of written documentation. In the paragraphs 2.1 to 2.4 the current knowledge about some frequently mentioned examples is presented and discussed.
2.1. Huang Ti and the ancient book of medicine NeI Ching
The traditional Chinese medicine yielding temporary relief for shortness of breath, chest tightness, and wheezing is Ma-huang. It is derived from the plant Ephedra sinica having a high ephedrine content [Citation32,Citation33]. The use of Ma-huang for inhalation may have been described for the first time in what is known as the oldest known Chinese book on internal medicine, Nei Ching, in which also symptoms that indicate asthma are mentioned [Citation3]. Often Huang-Ti, also known as Huang-Di, or the Yellow Emperor of China, is mentioned as the author of Nei Ching and Stein and Thiel referred to about 1000 BCE for this book [Citation5]. However, according to modern views its author is unknown, its age is uncertain and its text is partly unauthentic.
Nei Ching (also Nei Jing or Neijing) has two separate books [Citation34,Citation35]: Su Wen (or Suwen), dealing mostly with physiology and pathology, and Ling Shu (or Lingshu) about anatomy and acupuncture therapy [Citation36]. The Yellow Emperor, Huang Ti (or Huang Di), who according to the historian Ssu ma-Ch’ien, or Ssu ma-Kuang was the first ruler of the Chinese empire and the founder of the Chinese civilization, supposedly lived from 2697 to 2597 BCE [Citation37]. Genealogies of the Chinese Dynasties list Huang Ti as the third of China’s first five rulers of the ‘Legendary Period’ from approx [Citation38]. 2850 to 2200 BCE, but modern historiography tends to consider him as an imaginary being, rather than an actual personality. Although there remains controversy about his actual existence in the past, it is currently generally accepted that Huang Ti is not the author of Nei Ching, even among those who believed in his existence [Citation34]. According to Ssu-ma-Kuang (living from 1019 to 1086 CE), who was a leading conservative statesman himself and a great Chinese historian [Citation39], an emperor would not have the time to write such a book. Ssu-ma-Kuang believed that the book Nei Ching was written in the period between the Chou (10th century till 256 BCE) and the Han dynasty (202 BCE-220 CE) by someone who antedated his writing to enhance its importance. According to others [Citation36,Citation40], there is sufficient historical evidence that Nei Ching is probably written about 1000 BCE, which agrees with the date mentioned by Stein and Thiel [Citation5]. However, Veith [Citation34] mentions that the Jesuit missionary and medical doctor Léon Wieger (1856–1933 CE) refined this date to the Han Dynasty based on the style of writing for a major text part of Su Wen, although he acknowledged that its contents may be older. Another part he dated to being older than Lao-tze (also Laozi), a Chinese philosopher, whose precise identity and period of living are uncertain. The latter is positioned somewhere in the period between the 6th and 4th century BCE, but most likely he is imaginary too, similarly as Huang-Ti [Citation41]. Nei Ching Su Wen in its present form is known from Wang Ping who lived in the Tang dynasty (609–907 CE). He claimed to be the first to discover the manuscript that he commented and expanded to 24 books, sub-divided in 81 chapters. Also, later revisions are known (1068–1078 CE) as a result of which little of the authentic text remains [Citation34].
2.2. The Papyrus Ebers
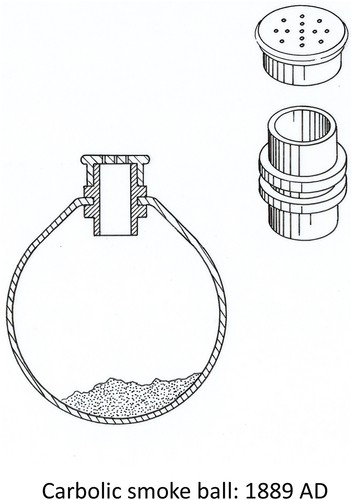
Combusting, smoking, or heating plant material are also known from Egypt, India, the Americas and various Arabic and Islamic countries. Many manuscripts mention the Papyrus Ebers that was found in Egypt and is dated approximately 1500 BCE. The papyrus gives a clear reference to ‘swallowing the smoke’ through a reed sticking through the bottom of a container placed over the medicine (e.g. leaves) on a stone that has been heated in a fire (see ). This might be the oldest known description of an inhaler device, but the plants and diseases mentioned in some reviews cannot be confirmed.
Figure 1. Ancient Egyptian technique for inhaling volatile vapors released by therapeutic herbs put on a hot stone as described in the Papyrus Ebers (1500 BCE). The stone is heated in a fire and the vapors are collected in a jar placed over the herbs having a hole in the bottom through which a reed sticks for inhaling the vapors.
The Papyrus Ebers is one of several medical papyri from Egypt, dating from the second millennium BCE of which eight are presented and discussed by Metwaly et al. [Citation39]. It is referred to in various manuscripts about the history of pulmonary therapy [Citation2,Citation3,Citation5,Citation7,Citation26,Citation42]. However, part of the information regarding its age, find and contents in these references is incorrect. This may have its origin in the first translation of the papyrus by Ebbell, which is currently no longer considered representative [Citation40]. The information given hereafter is received from personal correspondence (January 2022) with Dr. Almuth Märker, custodian of the Papyri and Ostraca collection (University Library, Leipzig), and Dr. Lutz Popko, Academy of Sciences and Humanities in Leipzig who, in collaboration with others, published a new scientific translation of the Papyrus Ebers in 2021 [Citation41]. They kindly shared their up-to-the-minute-knowledge about the papyrus that was discovered in the nineteenth century in Upper Egypt by Georg Ebers, Egyptologist, and professor at the Leipzig University. Ebers purchased the papyrus in 1873, possibly from an antiquarian after which it came in the possession of the University Library of Leipzig. According to Ebers’ notes, a tomb in el-Assassif, a necropolis near Luxor, was mentioned to him as the find spot. Recent C14 analysis (in 2014), the form of writing known from the final decades of the 16th century and a reference to the reign of Amenhotep (from the 18th Dynasty) confirm that the papyrus dates back to approximately 1500 BCE. It has been mentioned in literature that some text parts are much older, dating back 3000–2500 BCE [Citation42], but that is considered very unlikely by the experts, although the text itself may be a collection of older recipes indeed. The author of the 18.63 m long manuscript having originally 108 columns is unknown. The papyrus is a textbook of contemporary knowledge of medicine for doctors and contains prescriptions of recipes for ‘inhalation’ from which various specific ingredients and diseases have been interpreted. For instance, black henbane has been mentioned in most references [Citation43], but in reality, the plants mentioned in connection with inhalation (in the columns 54 and 55 of the papyrus) cannot be identified. In fact, most of the components for the remedies cannot be translated into currently known ingredients, which makes it difficult to reproduce ancient Egyptian prescriptions. Moreover, black henbane (Hyoscyamus Niger) is native to North Africa, but Hyoscynamus muticus (Egyptian henbane) is regionally much more common in Northern Africa and both have the same properties and ingredients [Citation44]. Hence, the use of black henbane is not very likely. Diseases can neither be concluded from the inhalation prescriptions which belong to a group of recipes against coughing of which neither the cause, nor the kind is specified and any interpretation toward a specific disease is speculative. Nevertheless, the most relevant passage about ‘inhalation,’ which word is not really known in the ancient Egyptian language, has recently been translated into: ‘Take seven stones and heat them in a fire. Take one of them from the fire and put some of this [i.e. the afore described] medicine on it. Cover the stone with a new jar of which the bottom is perforated and stick a reed through the perforation. Take the reed in the mouth and swallow the smoke. Do the same with the other stones. Next, some greasy food has to be eaten’ (recipe no. Eb 325). This is an English interpretation of the original translation into German.
At the end of the Second World War the Ebers papyrus was evacuated and briefly stored in Schloss Rochlitz in the neighborhood of Leipzig. In this period, the papyrus was seriously desecrated. Seventeen columns were lost and another seven were severely damaged. Fortunately, a perfect facsimile was prepared already in 1875 thanks to which its whole contents is still available. There are more ancient Egyptian papyri known than only the eight presented by Metwaly et al. [Citation44] that describe treatments for fumigation (combustion of therapeutic substances). Some recipes mentioned in these papyri are for treatment of particular body parts.
2.3. Ayurveda, the Indian tradition of medicine
The ancient history of Hinduism in India has been captured from oral tradition in four different Veda’s, written in Vedic Sanskrit: Rigveda, Atharvaveda, Yajurveda, and Samaveda. These Veda’s are collections of sacred books that consist of various types of subsidiary and supplementary compendia, such as Samhitas and Brahmanas. One of the subsidiary parts of Atharvaveda, an amalgam of religion, magic, and empiric elements [Citation45], is Ayurveda about the ancient Indian conception of medicine and lifestyle [Citation46]. The name Ayurveda is a combination of the words Ayur, that has several different translations relating to life, and Veda meaning knowledge or science. Ayurveda is also the name of the traditional Indian medicine. Two main sets of texts form the foundation of Ayurveda: Charaka Samhita and Susruta Samhita. Charaka (Caraka or Charak) was a physician and Susruta a surgeon. According to Panda and Doddanagali, the symptoms of bronchial asthma (Tamaka Swasa) and its treatment with polyherbal combinations are described in Charaka Samhita, but they did not refer to a route of administration [Citation47]. Although the mentioning of their names in relation to both Samhitas suggests that Charaka and Susruta are the authors, they are currently more seen as revisers of older texts to which they have contributed by rewriting them in light of new knowledge. This could well be knowledge from elsewhere as there was an immense exchange in thinking and knowledge across the ancient world (Greece, China, Mesopotamia, and India) between the 7th and 1st century BCE [Citation45]. For both presently available Charaka and Susruta Samhitas, at least three authors from three different periods are considered responsible [Citation48–50]. Agnivesha is reputedly the author of the oldest concept of Charaka Samhita, named Agnivesha Tantra, which at present is no longer available. Agnivesha was a pupil of Atreya, who is believed to have lived before 500 BCE, but both characters, referred to with the title of ‘rishi,’ ‘seer’ or ‘sage,’ are largely legendary. Rishi (Sanskrit) is a Vedic poet, Seer (Sanskrit) is an authoritative person who divines the future and Sage (Sanskrit) is a wise man or spiritual teacher. Agnivesha Tantra may have been revised and supplemented in 200 BCE by Charaka and in 400 CE by Dridhabala [Citation48–50]. Although most references agree with the involvement of these three compilers, there is no consensus in literature about aforementioned dates. According to Raju [Citation45], Charaka is a contemporary of Susruta whom he placed somewhere in the period between 800 and 600 BCE. Meulenbeld in his comprehensive authoritative work concluded for Chakara that he cannot have lived later than 150–200 CE and not much earlier than 100 BCE [Citation51]. This is in fair agreement with 200 BCE [Citation48], 2nd century BCE [Citation49] and 1st century CE [Citation50] mentioned by others and this seems to exclude him from being a contemporary of Susruta. Hence, the uncertainty about the timeline and the authorship of substantial text parts of Charaka Samhita makes it impossible to give a precise date for an early reference to inhalation in this compendium.
2.4. Ancient Greek-Roman medicine
Hippocrates of Kos (approx. 460–370 BCE) developed his innovating, and at the time unorthodox medical theories in the Golden Age of the Greek cities. Hippocrates was the first to see natural causes for diseases instead of supernatural powers [Citation52]. In the translation of part of his work and that of and Claudius Galenus by Redman Coxe [Citation53], Hippocrates is quoted with: ‘Some diseases arise from the air we breathe. Whenever in the same place many persons are attacked with the same disease at the same time, we must attribute this to the same common course, which is the air.’ Hippocrates also used physical symptoms to diagnose a disease and refined the humoral theory, developed in the 6th century by Alcmaeon of Croton. This theory, possibly having roots in ancient Egypt or Mesopotamia and as applied to medicine by Hippocrates, suggests that the vital body fluids (humors) are blood, phlegm, yellow bile, and black bile, which all have to be in good balance with each other. An excess or deficiency of any of these humors is indicative of an illness that needs to be treated. Hippocrates’ approach of medical science has long been leading in the Greek-Roman medical practice but was also important in the ancient Islamic medical tradition, flourishing in the 8th to 14th century CE. A reference to Hippocrates’ work is often a reference to Corpus Hippocraticum, but this collection of manuscripts is written in different ionic dialects of which some contradict each other, suggesting that it is rather an assembly of manuscripts from different authors. Famous Greek and Roman physicians who worked in the tradition of Hippocrates are Pedanius Dioscorides (Greek-Roman: approx. 40–90 CE), Arataeus of Cappadocia (Greek: 2nd century CE), Claudius (Clarissimus) Galenus (Greek-Roman: approx. 130–200 CE), Caelius Aurelianus (Roman: 5th century CE) and Paulus Aegineta (or Paul of Aegina, Byzanthine Greek: approx. 625–690 CE). They are known for prescribing the inhalation of fumes and vapors from the combustion of plant and other organic materials, or that of sea air or sulfuric gases from volcanic activity in the treatment of breathing difficulties due to respiratory diseases. Particularly, Hippocrates is mentioned as being one of the first having recommended the use of a container and a reed to assist the inhalation of vapors and fumes arising from combustion [Citation2]. Unfortunately, no evidence for that can be found in the translation of part of his work by Redman Coxe [Citation53].
2.5. Smoking as a manner of ‘controlled inhalation’
All aforementioned examples are about inhaling vapors, smokes, or gases that move freely into and with the air around, and preferably toward the patient, unless a reed is used for inhalation from a small container in which the vapor or smoke is generated. Smoking with a pipe in which plant material or any other substance is combusted is another, and generally more efficient way to inhale the thereby created smoke. Considering that smoke is an aerosol of very small incompletely burned particles and that smoking pipes are developed specifically for creating and administering such aerosols, one could argue that smoking pipe approaches using a dry powder inhaler. At least with a pipe, there can be much greater consistency of the delivered dose than with combustion of herbs in the free air. Generally, smoking is associated with tobacco and with the Americas where tobacco is a native plant. With a few exceptions (in Australia), nearly all sixty species of Nicotiana come from the Americas [Citation25]. The smoking of tobacco is usually for obtaining a pleasurable sensation. The plant, however, has already in ancient times been mixed with various therapeutic herbs and substances for the treatment of a great variety of different diseases, including asthma, either for smoking, sniffing, rubbing, or other ways of application. For instance, Stein and Thiel mentioned that Central and South American native people are likely to have smoked tobacco with Datura leaves as a therapeutic remedy for the treatment of asthma and with Cannabis as a sedative [Citation5]. There has also been found evidence for the smoking of tobacco with Rhus glabra in North America (central Washington State) in an approximately 1400-year-old pipe [Citation54]. Rhus glabra was a widely used plant among native people in North America because of its antimicrobial activity [Citation55]. After its introduction to Europe in the 16th century, tobacco was considered a botanical medicine and a universal remedy against more than 65 different ailments for more than 300 years [Citation56]. Tobacco initially was smoked, sniffed and chewed upon, but after mass production machines for cigarettes were developed in the second half of the 19th century, smoking became the preferred manner of use in most countries. Tobacco in therapeutic cigarettes for relief of asthma and catarrh was mixed with stramonium leaves and became very popular in the late 1800s in Europe, the US, and China, even among physicians. The smoking of therapeutic cigarettes lasted into the fifties of the 20th century before it was recognized that the cigarette is the deadliest artifact in the history of human civilization [Citation57]. Smoking is not limited to tobacco, however, and the use of tobacco is not limited to smoking. Evidence for smoking of plants of the Cannabis genus in wooden braziers has been found on a cemetery in Central Asia dated approximately 500 BCE [Citation58]. Ren et al. also referred to similar discoveries in western China and concluded that the smoking of Cannabis is historically for ritual purpose and very little is known about its use for psychoactive effects. Cannabis and opium were smoked in Asia and Egypt, whereas the Vikings in Europe (approx. 800 to 1100 CE) used Angelica archangelica (angelikarot) in their pipes.
2.6. Medical recognitions and achievements stimulating inhalation
Relevant to the history of pulmonary therapy are also various medical recognitions and achievements. To understand the rationale for inhaled therapeutic substances, the existence of the lungs, and their function must be understood in relation to other bodily functions. Two important quotes of Claudius Galenus, Greek-Roman physician (approx. 130–200 CE), in the translation of Redman Coxe, witness the high level of understanding of anatomy and medicines among Greek physicians briefly after the beginning of the era [Citation53]. This translation reveals that Galenus knew that ‘The largest elephant and the smallest bird that breathe have a similarly constructed heart and lungs.’ Galenus also reasoned: ‘The use, or benefit of respiration, or rather the air in inspiration depends not only on its actual substance, but rather on some quality connected with it.’ According to his understanding, ‘inspiration has the intention of ventilating the blood and cooling it.’ With this understanding and some knowledge of the symptoms that accompany diseases affecting the airways plus the reasoning of Hippocrates about the cause for some diseases from the inhaled air, it should not even be surprising that these early Greek physicians suggested the inhalation of therapeutic substances (gases, vapors, fumes, or powders) as best remedy to cure these airway diseases. In this light, the recognition of John Stern (1764) ‘that the windpipe is the only possible way of applying medicines directly to the lungs’ is no more than a rediscovery of more than 1500 years old knowledge [Citation3]. It is known that Hippocrates and Galenus did indeed recognize the symptoms of asthma, tuberculosis (phthisis), empyema, and catarrh already [Citation53]. Most likely, they did not understand the working mechanisms of the therapeutic substances they recommended for inhalation. They must have been selected on empirical knowledge, but they were well aware of the concept of contagion and understood the importance of a good hygiene [Citation52].
From the Middle Ages, there is very limited information. In the period between 700 and 1100 CE most remedies for ailments were not written down but passed on orally from person to person as most people were illiterate and had no use for medical books [Citation59]. Much of the medical knowledge from the Greek and Roman civilizations was lost after the fall of the Western Roman Empire in 476 CE and the large European population migration in the 4th to 6th century. The period from approximately 1100 CE on can be marked for a change in the situation when the Crusades initiated trade and the exchange of ideas between Europe and Islamic countries. Previously lost Greek and Roman medical texts returned to Europe, enriched by the experiences and knowledge of Islamic (Persian and/or Syrian) physicians, such as al-Razi, Yuhanna ibn Bukhtishu, and ibn Sina [Citation60,Citation61]. Another person to be mentioned in this respect is Maimonides (1138–1204 CE), born in Spain as Moshe ben Maimon. Maimonides lived and worked in Spain and Egypt, in the latter place as physician of the sultan of Egypt, and is known (amongst many other achievements) for his book ‘A Treatise on Asthma’ [Citation62]. In many manuscripts, Maimonides is mentioned for advocating the inhalation of herbs in the treatment of asthma [Citation2,Citation3,Citation7,Citation26,Citation63], but in reviews specifically about his life and work, such a reference lacks [Citation62,Citation64,Citation65]. Nevertheless, Maimonides’ knowledge of how to treat asthma seems undisputed. He understood the relationship between lifestyle, environmental conditions and asthma severity and recognized that the great heterogeneity of the patients required therapy on individual basis.
3. Precursors to modern dry powder inhalers
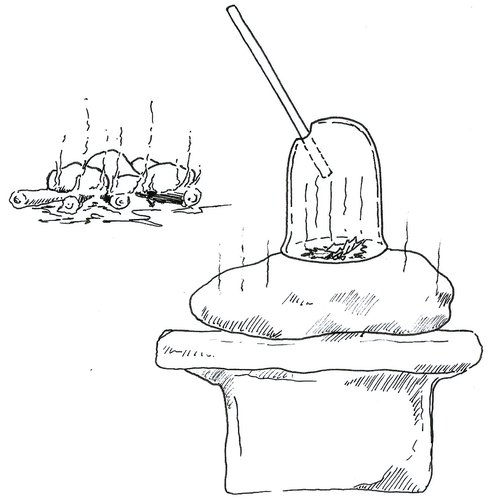
In contrast with nebulizers, the past of modern dry powder inhalation is relatively short. It started first in the second half of the 20th century, with the exception of a few earlier inventions and inhalation habits that are mostly mentioned because they are illustrative for the desire to deliver powdered herbs, minerals, or other substances to the airways from early times onwards. They show the great interest in having access to delivery means for therapeutic (or hallucinogenic) substances to the respiratory tract. Proof for the delivery of powdered herbs and other substances to the respiratory tract can be found in South America where snuff trays dating back to at least 400–700 CE have been found [Citation66]. The hallucinogenic substance was carried in a cane or bone box, or leather pouch, pulverized in a miniature mortar before use and the pulverized material was transferred to the snuff-tray before it was inhaled deeply through the nose (). Also from other cultures comparable inhalation equipment is known, but for ages very few innovative developments in equipment for the inhalation of powdered material were reported. One of the first known inventions is a small and portable DPI presented by Ira Warren in Boston in 1852 [Citation5]. This inhaler consists of two tubular glass parts in a coaxial arrangement as shown in ). The arrangement allows the inner part to be wiggled and twirled by hand during inhalation. The inner tube is open at its rear end for inserting the inhalation powder and has a convex front with a diameter being slightly larger than the inner diameter of the tube itself. There are small holes in the convex front through which the powder can be discharged into the air stream during inhalation. The outer tube has the mouthpiece through which the aerosol is inhaled. Twelve years later, the first known patent application for a DPI was filed in London by A.E. Newton in 1864 [Citation3]. The description in this patent no 1161 is that of a bin with a rounded bottom in a wooden cabinet with a hinging roof-shaped lid (): cabinet and bin shown separately). Through the bin is a horizontal shaft that has hair strings or feathers in order to brush medicinal powder from the bottom of the bin into the air when the shaft is rotated using a handle sticking outside the cabinet [Citation67]. The rotation of the feathers also starts the air in the bin to whirl and to create an aerosol. Holes made in the cabinet allow for the admission of air to its interior. The patient sits with his or her face pressed against an opening in the roof-shaped lid of the cabinet in order to inhale the aerosol. Between the bin and the opening is a mesh to refine the powder.
Figure 2. Wooden tray with condor head for the inhalation of hallucinogenic and therapeutic powdered herbs using a hollow bone as reed, San Pedro, Colombia, 700–950 CE.
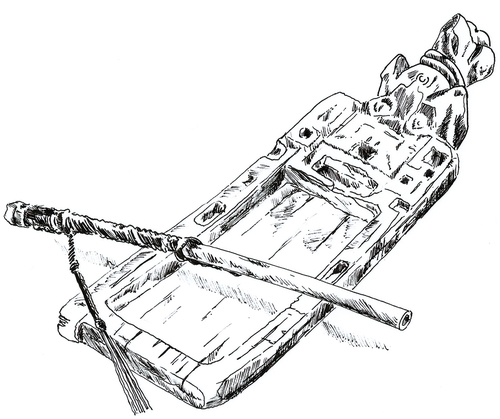
Figure 3. Inhaler Ira Warren (A: 1852 CE) and inhaler A.E. Newton (B: 1864 CE), see text for the explanations.
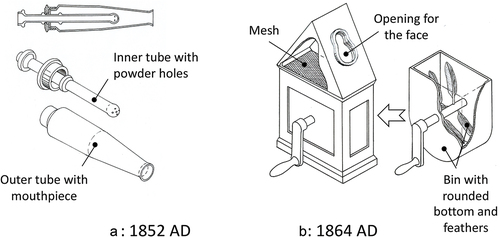
Both previously mentioned inventions were very ineffective in dispersion, vulnerable (Ira Warren concept), too large to be portable (Newton concept), and showed very low consistency of delivered dose. It is therefore not surprising that in his book entitled ‘The inhalation treatment of diseases of the organs of respiration: including consumption,’ Hassall discriminated between six different kinds of apparatus being employed for the delivery of therapeutic substances to the lungs, versus only one for the inhalation of powders mentioned as last [Citation68]. Although he depicted and described many different constructions for the generation of sprays and vapors, Hassall gave no example for the delivery of powdered medication in his book [Citation68]. He concluded that the construction of a suitable inhalation chamber for ‘substances in aeriform condition’ was (to his best knowledge) not yet accomplished in a satisfactory and scientific manner. Moreover, he commented that many of the wet aerosol generators were quite useless too, obsolete and often unimportant modifications of each other. Briefly, after Hassall published his view on inhalation technique, Frederick Roe invented the Carbolic Smoke Ball in 1889 [Citation5]. This device is, basically, a rubber squeeze ball containing the medicinal powder, which in the formulation of Roe contains powdered glycyrrhiza and hellebore (both perennial plants) and carbolic acid, also known as phenol, an aromatic (solid and volatile) alcohol. The squeeze ball is attached to an ebonite (vulcanized rubber, also incorrectly named vulcanite which is a telluric mineral) tube-like part in its opening, which has a double function by being the mouthpiece and the holder of a gauze for refining the powder aerosol, see . The Roe invention is mostly not remembered as inhaler, but some may recognize it as the basic design of an insect, or bulb duster for the aerosolization of insecticides like the currently forbidden dichlorodiphenyltrichloroethane (DDT). Lawyers may also have better knowledge of this inhaler because the Carbolic Smoke Ball Company was involved in a legal case from the English Court of Appeal [Citation69]. The market presentation in 1891 of the Carbolic Smoke Ball that was meant to cure influenza and a number of cold-associated complications, was invigorated with a special offer. In advertisements in various papers, it was announced that any person contracting the infectious influenza or any disease caused by taking cold after having used the ball three times daily for two weeks according to the printed instructions would receive a reward of £100, – from the Company. Mrs Louisa Elizabeth Carlill from London read the advertisement and bought one of the balls, which she used for nearly two months as prescribed. Nevertheless, she contracted influenza and in response to the advertisements, she contacted the Company to claim her reward. However, instead of reacting as promised, the Company asked Mrs Carlill to come to their office and use the ball for three more weeks to check whether she had used it correctly. Mrs Carlill denied this request and decided to sue the company for denying to pay her the reward. The judges decided to her advantage and condemned the company, who claimed in court that the reward was meant as a joke, but they had difficulties motivating their decision as the contract law at the time did not foresee situations as between Mrs Carlill and the Company. The case is known for the great inventiveness of the judges (particularly Lord Justice Lindley and Bowden) in extrapolating the basic principles of contract law and it is still often the first legal case of a unilateral contract that students in the law of contract are confronted with.
The first DPI having some commercial success on the market was the Abbott Aerohalor (1948) (). It was developed in the 1940s by Mack Fields, who worked for Abbott Laboratories, for the delivery of penicillin to the lungs [Citation5]. The Aerohalor had several characteristics of currently used inhalers, like being disposable and using disposable cartridges. It was also the first inhaler delivering active ingredients with proven effect against the diseases for which it was used. On the basis of these characteristics, the Aerohalor could be considered the first modern DPI. Its invention did not bring a breakthrough comparable with that of the Fisons Spinhaler at the end of the 1960s, more than 20 years later, however. This breakthrough required first the development of several prerequisites for their large-scale production, such as suitable plastics, pharmaceutical-grade lactose, effective jet mills, high-speed capsule filling machines, etc., as will be discussed in part 2. For these reasons, we decided to appoint the Spinhaler as the first modern DPI.
Figure 5. Aerohalor (Abbott laboratories, 1948) with sifter cartridges for isoprenaline sulfate (brand name Norisodrine) and penicillin, invented by Mack Fields.
When the Aerohalor became available, there must have been a burning interest in a simple and easy to use technique for delivering penicillin and other antibiotics, like Streptomycin, to the lungs after clinical studies had shown that this is highly effective in the treatment of respiratory diseases, but certainly ‘not an office procedure’ [Citation70]. To obtain a good result, Farber and Ross requested their patients to inhale at least four or five times a day for several days. They emphasized the need for using an appropriate nebulizer, giving careful instructions as well as attention to details that made nebulization a hospital procedure and almost a day-time job for the patients and the hospital staff [Citation70]. The Aerohalor of Abbott was a simple plastic inhalation device making use of interchangeable sifter cartridges carrying a dose of the drug mixed with lactose [Citation1]. These cartridges had an opening to the aerosol chamber in which a fine mesh was placed. The air inlet was a curved channel in which a steel ball rolled upwards during inhalation to collide with the sifter cartridge and release some powder from it through the mesh into the inhaled air stream. The mouthpiece could be interchanged with nosepiece to target the desired site of deposition. Until 1950, penicillin was not made available for civilians; its application was reserved for military use only.
4. Conclusions
Inhalation of therapeutic and hallucinogenic gases, vapors, smokes, and aerosols is likely to have a much longer history than can be concluded from written evidence or excavated artifacts referring to inhalation. Administration of therapeutic substances via the pulmonary route does not per se require specific tools for their preparation or use. Beneficial airborne substances to health may naturally be present in certain areas, such as the seaside, around volcanoes and in pine forests. First from the nineteenth century, the first attempts to create powdered aerosols for inhalation are known. They were not very successful because of a lack of effective drugs and a very limited control of the aerosol properties and the delivered dose to the patient. Therefore, they are rather precursors to modern DPIs, showing the interest in dry powder inhalation, than full-fledged pulmonary drug administration devices, which may also be blamed on a lack of good production equipment and suitable materials for large-scale production, as will be explained in Part 2.
5. Expert opinion
Any expert opinion about the past is arguable, as the past remains largely unknown whereas it has no future to predict. Commenting on the past cannot change its course for the better, nor for the worse, as it is a fait accompli. It may be possible to mention some periods and places where and when ancient people inhaled certain vapors, gases or aerosols, but any speculation about the extent to which this habit was spread and the reasons why it was exercised is neither provable nor refutable. Was it for hallucinatory effects and practiced by magicians and shamans primarily? Or was it therapeutic treatment prescribed or recommended by contemporary medical scientists? For both possibilities, certain arguments and indications can be given depending on the find and the period of the event, but for several historic examples the main reason remains unclear. We often know where, and how people lived in the past and partly what they did, but the reasons for their behavior remain often speculative due to the lack of written evidence. The two most drastic turning points in human history may be good examples of ignorance about human motivation in the past: the Neolithic, or first Agricultural Revolution and the (first) Industrial Revolution (IR). In both cases the standard of living decreased initially and yet this was endured and the revolutions were continued to turn first much later for the better when the population growth reached to the extent for which the situations before the revolutions would have been no longer tenable. The IR may have been profitable for the entrepreneurs right from the start, but for their employees it was a dramatic deterioration of the standard of living. Also, the presumed superiority of agriculture in its early ages of the Neolithic Revolution may be questioned [Citation71] and it is still poorly understood what drove people to get involved when for most of them only the negative aspects of these revolutions were to be recognized. The IR took place in a relatively short period between approximately 1760 and 1870 and this period is intertwined with outbreaks of infectious diseases being contagious through the lungs and a high prevalence of lung diseases like asthma, COPD and silicosis. This shows the strong connection of the IR with pulmonary diseases. The IR could also be considered as an urban revolution, although this term was first introduced in the 20th century [Citation72], as people moved en masse from rural areas to cities in order to become employees of the rapidly expanding industry. In England, where the IR began, small cities like Manchester grew from 10.000 inhabitants in 1801 to 2.3 million in 1891 and became completely overcrowded. Due to this population explosion and impotent city administrations (at least before 1835), social infrastructures collapsed and the provision of sufficient food, appropriate housing and medical care started to fail. The working class, living in slums, also suffered from insufficient hygiene. People lived and worked closely together in damp, dark and unheated houses and inhaled heavily polluted air. In addition, there was insufficient knowledge of how contagious diseases are spread and how to protect oneself against infection. This all resulted repeatedly in heavy outbreaks of smallpox, cholera, typhoid, typhus and particularly tuberculosis (TB), the latter in the Middle Ages also referred to as phthisis and ‘white plague’ and in 1800s as ‘consumption.’ In 1838 up to one third of the British working class died of TB against up to one sixth in the upper class [Citation31]. The situation stimulated research into a better understanding of the requirements for prevention and treatment of these illnesses. It resulted, for instance, in the mid-nineteenth century in a Sanitary Reform Movement in the UK drawing attention to the connection between pauperism, unsanitary conditions and disease. In line with that, the period of the IR was the era in which significant advancements in the medical field were made such as an improved understanding of the course of diseases like tuberculosis [Citation31,Citation73]. Industrial manufacturing made fast and cheap production of medical instruments (e.g. scalpels, clamps, microscope lenses, test tubes, glassware, etc.) possible. In addition, and from 1760 on, various new pulmonary delivery devices, mainly for wet aerosols, and therapeutic entities were developed and identified [Citation5]. In contrast, dry powder inhaler technique did not directly profit from the technological advancements made during the IR. None of the aforementioned DPI examples from the 19th century meets the criteria for modern DPI technology, such as being effective, mass-produced and cheap, and delivering accurately metered single doses. This required several additional developments first to be made in the 20th century. These would not have been possible without the IR, however, which created the industrial design and manufacturing climate and standards for the introduction of electricity as power source, the development of new materials (e.g. Bessemer steel and plastics) and integrated production lines. These developments are discussed in part 2.
As many diseases enter the body via the lungs and/or manifest (primarily) in the lungs, most diseases of the IR were potentially a point of departure for the development of inhaled drugs and pulmonary drug delivery systems. Already at the end of the 17th century TB was recognized as an example of such a disease [Citation31]. In 1854, the sanatorium cure for TB-patients was introduced by Hermann Brenner and in 1865, the infectious nature of TB was demonstrated by J-A Villemin [Citation31]. However, the perception of the cause and spreading of TB took first a dramatic turn when Robert Koch irrefutably demonstrated in 1882 that the disease is caused by bacteria. Koch is considered the founder of the bacteriology, although the credit should actually be given to Aloys Pollender who already observed in 1845 ‘plants’ in the blood of animals that died of anthrax [Citation74,Citation75]. Other pathogenic bacteria were discovered shortly after and the knowing of their existence ended the humoral theory at the favor of a new germ theory [Citation76]. This is an important change in thinking as it gradually put an end to the treatment of pulmonary diseases with ‘antiseptic aerosol therapy.’ Instead of having to inhale ineffective and hazardous compounds like turpentine, petroleum, picric acid, tar, iodine, sulfuric acid, and phenol, also called carbolic acid [Citation30], effective antibiotics became available after Alexander Fleming (1928) discovered penicillin and the existence of the fungus producing this β-lactam compound [Citation77]. Briefly, before that, Dmitri Ivanovsky (1892) and Martinus Beijerinck (1898) reported independently of each other that tobacco mosaic disease is caused by a pathogen smaller than bacteria, being a virus [Citation78]. The finding that bacteria, fungi, and viruses can be responsible for the transmission of infectious diseases via aerosols proved the right of Hippocrates’s hypothesis from more than 2000 years ago that ‘some diseases arise from the air that we breathe.’ The new recognitions enabled goal-oriented searches for suitable approaches and medicines for neutralizing virulence factors and eradicating the pathogens, respectively [Citation79]. In the 20th century the use of antimicrobial substances for many applications and in many places became so excessive, unnecessary, or inadequately, also regarding inhalation, that it caused resistance development of the microorganisms against these substances, particularly since the 1960s [Citation80]. A striking example is the resistance of Mycobacterium tuberculosis (Mtb) strains against a great number of anti-Mtb drugs, which is not only evolutional, but also intrinsic due to a thick waxy, hydrophobic cell envelope and the presence of drug degrading and modifying enzymes [Citation81]. Therefore, new antibiotics will be necessary and their administration against infectious diseases via the respiratory tract instead of via injection, might establish a more effective and endurable use, as this yields much higher drug concentrations at the site of action and considerably lower systemic exposure and, thus, less severe adverse side effects [Citation82].
Article highlights
The practice of inhaling therapeutic vapors and gasses may be considerably older than can be concluded from written manuscripts and excavated artefacts.
The uncertainty and ignorance about the origin and contents of ancient manuscripts should not result in speculations about herbs used and diseases treated, nor in the mentioning of specific dates.
The period of the Industrial Revolution induced a turning point in the inhalation therapy too.
The development of effective dry powder inhalers in the 20th century required completion of several preceding technological developments.
The health risks of inhaling therapeutic smoke were first widely recognized in the second half of the twentieth century.
The discovery of micro-organisms as cause for infectious diseases replaced the humoral theory by the germ theory. This opened the way for inhaling antibiotics and improve the treatment of infectious (lung) diseases.
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Acknowledgments
The authors thank Dr. Almuth Märker, Universitätsbibliothek Leipzig in Germany, custodian of the Papyri and Ostraca collection and Dr. Lutz Popko, Academy of Sciences and Humanities in Leipzig for their valuable contribution and interesting discussions about the Papyrus Ebers. They are also thankful for the written information received from Museo Chileno de Arte Precolombino, Santiago, Chile.
Additional information
Funding
References
- Rau JL. The inhalation of drugs: advantages and problems. Resp Care. 2005;50(3):367–382. •• One of the first critical (comparative) evaluations regarding the efficacy of pulmonary drug delivery devices.
- Anderson PJ. History of aerosol therapy: liquid nebulization to MDIs to DPIs. Resp Care. 2005;50(9):1139–1150.
- Sanders M. Inhalation therapy: an historical review. Prim Care Resp J. 2007;16(2):71–81.
- Sehata M. History of inhalation iherapy. Internet J Health. 2008;9(1):1–9.
- Stein WS, Thiel CG. The history of therapeutic aerosols: a chronical review. J Aerosol Med Pulm Drug Deliv. 2017;30(1):20–41.
- Rudén J. Powder mechanics and dispersion properties of adhesive mixtures for dry powder inhalers, conceptualized as a blend state model [Thesis]. Sweden: University of Uppsala, Dept Pharm Bioscience, 2021, pp 16–21.
- Rospond B, Krakowska A, Muszyńska B, et al. The history, current state and perspectives of aerosol therapy. Acta Pharm. 2022;72(2):225–243.
- Prime D, Atkins PJ, Slater A, et al. Review of dry powder inhalers. Adv Drug Deliv Rev. 1997;26(1):51–58.
- Newman SP, Busse WW. Evolution of dry powder inhaler design, formulation, and performance. Resp Med. 2002;96(5):293–304.
- Atkins PJ. Dry powder inhalers: an overview. Resp Care. 2005;50(10):1304–1312.
- Young PM, Traini D, Coates M, et al. Dry powder inhalers: challenges and goals for next generation therapies. Pharm Tech Europe. 2007;19(4):1–17.
- Reddy SC. Past and present trends of dry powder inhaler devices: a review. J Drug Deliv Therapeutics. 2014;4(1):97–107.
- Berkenfeld K, Lamprecht A, McConville, et al. Devices for dry powder drug delivery to the lung. AAPS PharmSciTech. 2015;16(3):479–490.
- de Boer AH, Hagedoorn P, Hoppentocht M, et al. Dry powder inhalation: past, present and future. Exp Opion Drug Deliv. 2017;14(4):499–512.
- Metha PP. Dry powder inhalers: upcoming platform technologies for formulation development. Ther Deliv. 2019;10(9):551–554.
- Xiroudaki S, Schoubben A, Giovagnoli S, et al. Dry powder inhalers in the digitalization era: current status and future perspectives. Pharmaceutics. 2021;13(9):1455.
- Dolgin E. The tangled history of mRNA vaccines. Nature. 2021;597(7876):318–324.
- Sahin U, Karikó K, Türeci Ö. mRNA-based therapeutics – developing a new class of drugs. Nat Rev Drug Discov. 2014;13(10):759–780.
- Lagendijk VC. Electrifying Europe: the power of Europe in the construction of electricity networks. Thesis Techn. The Netherlands: University Eindhoven, 2008, pp. 15–104.
- Chalmin P. The history of plastics: from the capitol to the Tarpeian rock. Open Edition J. 2019;19:6–11.
- Maglione M, Miotto K, Iguchi M, et al. Psychiatric effects of Ephedra use: an analysis of food and drug administration reports of adverse events. Am J Psychiatry. 2005;162(1):189–191.
- Miller SC. Psychiatric effects of Ephedra: addiction. Am J Psychiatry. 2005;162(11):2198.
- Sheik Ali B, Sathiswara B. Atropine induced psychosis: a report of two cases. Int J Health Sci Res. 2017;7(12):325–327.
- Picciotto MR, Kenny PJ. Mechanisms of nicotine addiction. Cold Spring Harb Perspect Med. 2021;11(5):a039610.
- Charlton A. Medicinal uses of tobacco in history. J R Soc Med. 2004;97(6):292–296.
- Jackson M. “Devine Stramonium”: the rise and fall of smoking for asthma. Med Hist. 2010;54(2):171–194.
- Wasik AA, Tuuminen T. Salt therapy as a complementary method for the treatment of respiratory tract diseases, with a focus on mold-related illness. Altern Ther Health Med. 2021;27(S1):223–239.
- Antonelli M, Donelli D, Barbieri G, et al. Forest volatile organic compounds and their effects on human health: a state-of-the-art review. Int J Environ Res Public Health. 2020;17(18): 6506.
- Miller WF. Aerosol therapy in acute and chronic respiratory disease. Arch Intern Med. 1973;131(1):148–155.
- Dessanges J-F. A history of nebulization. J Aerosol Med. 2001;14(1):65–71.
- Barberis I, Bragazzi NL, Galluzzo L, et al. The history of tuberculosis: from the first historical records to the isolation of Koch’s bacillus. J Prev Med Hyg. 2017;58(1):E9–12.
- Lee MK, Cheng BW, Che CT, et al. Cytotoxicity assessment of Ma-Huang (Ephedra) under different conditions of preparation. Toxicol Sci. 2000;56(2):424–430.
- Jiao, Jao J, Wu J, et al. Ma Huang Tang ameliorates bronchial asthma symptoms through the TLR9 pathway. Pharm Biol. 2018;56(1):580–593.
- Veith I. The yellow emperor’s classic of internal medicine. Berkeley and Los Angeles: University of California Press; 1966.
- ItsHaky B. Huang Di Nei Jing Ling Shu; The ancient classic on needle therapy; the complete Chinese text with an annotated English translation. J Altem Complement Integr Med. 2017;3:20.
- Kan LB. Introduction to Chinese medical literature. Bull Med Libr Assoc. 1965;53(1):60–67.
- Watson B. Ssu-ma Ch’ien Grand historian of China. New York: Columbia University Press; 1963.
- Chi-min W. China’s contribution to medicine in the past. Annals of Medical History. 1926;VIII:192–201.
- Metwaly AM. Traditional ancient Egyptian medicine: a review. Saudi J Biological Sci. 2021;28(10):5823–5832.
- Ebbel B. The Papyrus Ebers, the greatest Egyptian medical document. Copenhagen: Levin & Munksgaard; 1937.
- Popko L, Schneider UJ, Scholl R, et al. Papyrus Ebers: Die grösste Schriftrolle zur altägyptischen Heilkunst. Darmstadt: WBG; 2021. • Very interesting renewed translation of the Papyrus Ebers with annotations (in German).
- Cohen SG. Asthma in antiquity: the Ebers Papyrus. Allergy Proc. 1992;13(3):147–154.
- Karamanou M, Androutsos G. Aretaeus of Cappadocia and the first clinical description of asthma, letter to the editor. Am J Respir Crit Care Med. 2011;184(12):1420–1421.
- Alizadeh A, Moshiri M, Alizadeh J, et al. Black henbane and its toxicity – a descriptive review. Avicenna J Phytomed. 2014;4(5):297–311.
- Raju VK. Susruta of ancient India. Indian J Ophthalmol. 2003;51(2):119–122.
- Loukas M, Lanteri A, Ferrauiola J, et al. Anatomy in ancient India: a focus on the Susruta Samhita. J Anat. 2010;217(6):646–650.
- Panda AK, Doddanagali SR. Clinical efficacy of herbal Padmapatradi yoga in bronchial asthma (Tamaka Swasa). J Ayurveda Integrative Med. 2011;2(2):85–90.
- Patwardhan K. The history of the discovery of blood circulation: unrecognized contributions of ayurveda masters. Adv Physiol Educ. 2012;36(2):77–82.
- Bhavana KR, Shreevathsa S. Medical geography in Charaka Samhita. AYU Int Q J Res Ayurveda. 2014;35(4):371–377.
- Mukherjee PK, Harwansh RK, Bahadur S, et al. Development of ayurveda - tradition to trend. J Ethnopharmacol. 2017;197:10–24.
- Meulenbeld GJ. A history of Indian medical literature, part 1A, Vol 1. Brill/Schöningh Verlag: Paderborn; 2002.
- Pappas G, Kiriaze IJ, Falagas ME, et al. Insights into infectious disease in the era of Hippocrates. Int J Infect Disease. 2008;12(4):347–350.
- Redman Coxe J. The writings of Hippocrates and Galen, epitomised from the original latin translations. Philadelphia: Lindsay and Blakiston; 1846. •• Highly interesting commentary on translated medical treatises written by Hippocrates (of Kos) and Claudius Galenus to those admiring ancient Greek medical knowledge.
- Brownstein, Brownstein KJ, Tushingham S, et al. An ancient residue metabolomics-based method to distinguish use of closely related plant species in ancient pipes. Front Mol Biosci. 2020;7:133.
- Saxena G, McCutcheon AR, Farmer S, et al. Antimicrobial constituents of Rhus glabra. J Ethnopharmacol. 1994;43(2):95–99.
- Sanchez-Ramos JR. The rise and fall of tobacco as a botanical medicine. J Herbal Med. 2020;22:100374.
- Proctor RN. The history of the discovery of the cigarette-lung cancer link: evidentiary traditions, corporate denial, global toll. Tob Control. 2012;21(2):87–91.
- Ren M, Tang Z, Wu X, et al. The origins of cannabis smoking: chemical residue evidence from the first millennium BCE in the Pamirs. Sci Adv. 2019;5(6):eaaw1391.
- Amr SS, Tbakhi A. Abu Bakr Muhammad Ibn Zakariya Al Razi (Rhazes): philosopher, physician and alchemist. Ann Saudi Med. 2007;27(4):305–307.
- McCall T. Medical knowledge in the early medieval period. British Library. 2021. [cited Dec 2021]. Available from: https://www.bl.uk/medieval-english-french-manuscripts/articles/medical-knowledge-in-the-early-medieval-period?
- Wishah G. Ibn Sina’s role in scientific discoveries. Asian J Humanities Social Studies. 2018;6(6):193–200.
- Gea J. Maimonides, the respiratory system and personalized medicine. Open Respir Arch. 2019;1(1–2):3–4.
- Cohen SG. Food allergens: landmarks along a historic trail. J Allergy Clin Immunol. 2008;121(6):1521–1524.
- Zaikon SJ. Maimonides 1135-1204. Q Bull Northwest Univ Med Sch. 1959;33(1):71–76.
- Beyar R, Skorecki K, Blazer S. The Maimonides heritage: discovery and propagation of medical knowledge. Rambam Maimonides Med J. 2018;9(3):e0017.
- Miller MJ, Albarracin-Jordan J, Moore C, et al. Chemical evidence for the use of multiple psychotropic plants in a 1,000-year-old ritual bundle from South America. PNAS. 2019;116(23):11207–11212.
- Newton AV. Inhaling apparatus. English patent 1161. 1964
- Hassall AH. The inhalation treatment of diseases of the organs of respiration: including consumption. London: Longmans, Green, and Co; 1885.
- McGinnis JD, Carlill V. Carbolic smoke ball company: influenza, quackery, and the unilateral contract. Can Bull Med Hist. 1988;5:121–141, CBMH/BCHM
- Farber JE, Ross J. The use of aerosol Penicillin and Streptomycin in bronchopulmonary infections. Calif Med. 1950;73(3):214–217.
- Svizzero S. Persistent controversies about the Neolithic revolution. J Hs Arch & Anthropol Sci. 2017;1(2):53–56. •• Critical evaluation of the debates about the presumed superiority of farming over foraging and the origin and spread of the Neolithic revolutions.
- Smith ME. Gordon childe and the Urban revolution: a historical perspective on a revolution in urban studies. Trp. 2009;80(1):3–29.
- McFadden ER. A century of asthma. Am J Respir Crit Care Med. 2004;170(3):215–221.
- Blevins SM, Bronze MS. Robert Koch and the ‘golden age’ of bacteriology. Int J Infect Diseases. 2010;14(9):e744–e51.
- Münch R. Robert Koch. Microbes Infect. 2003;5(1):69–74.
- Williams DW. The germs-theory. Br Med J. 1871 April;8(536):368.
- Gaynes R. The discovery of Penicillin – new insights after more than 75 years of clinical use. Emerging Infect Dis. 2017;23(5):849–853.
- Zaitlin M. The discovery of the causal agent of the tobacco Mosaic disease. In: Kung SD, Yang SF, editors. Discoveries in plant biology. Hong Kong: World Publishing Co. Ltd; 1998. p. 105–110.
- Pirofski L-A, Casadevall A. What is infectiveness and how is it involved in infection and immunity? BMC Immunol. 2015;16(1):13.
- Davies J, Davies D. Origins and evolution of antibiotic resistance. Microbiol Mol Biol Rev. 2010;74(3):417–433.
- Gygli SM, Borrell S, Trauner A, et al. Antimicrobial resistance in Mycobacterium tuberculosis: mechanistic and evolutionary perspectives. FEMS Microbiol Rev. 2017;41(3): 354–373.
- Traini D, Young PM. Drug delivery for tuberculosis: is inhaled therapy the key to success? Ther Deliv. 2017;8(10):819–821.