ABSTRACT
Background
This study evaluated treatment patterns for long bone fractures and factors that contribute to use of intramedullary nails (IMN).
Methods
Patients from IBM MarketScan® Research Commercial and Medicare Databases with femoral/tibial/humeral fractures during inpatient admission between January 2016-July 2019 were identified. Patients were categorized by treatment (i.e., non-surgical/internal fixation [extramedullary internal fixation/plating]/IMN/external fixation). Four-year rates of IMN were reported by fracture type. Logistic regression evaluated factors contributing to IMN use.
Results
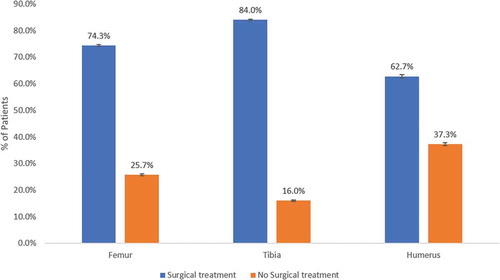
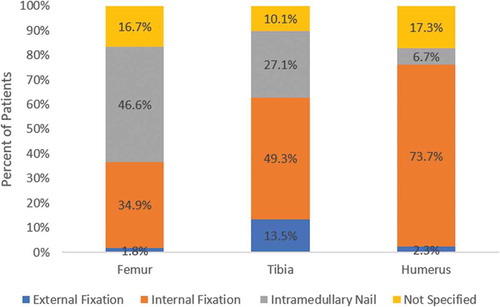
14,961 femoral, 14,101 tibial, and 7,059 humeral fracture patients were identified (mean[SD] age was 45.3[18.9], 42.0[16.3], and 39.8[21.6] years and % female 50.8%, 47.7%, and 55.3%, respectively). Mean(SD) lengths of stay were 6.7(9.2), 5.9(7.0), and 5.8(10.3) days, rates of surgical treatment were 74.3%, 84.0%, and 62.7%, and rates of IMN among surgical patients were 46.6%, 27.1%, and 6.7% for femoral, tibial, and humeral fractures, respectively. IMN was the predominant treatment for femoral fractures over the past 4 years. Factors contributing to IMN use included open/closed diaphyseal fractures, pathological fractures, diagnoses of cancer or AIDS/HIV, and alcohol abuse.
Conclusions
IMN was the predominant treatment for femoral fractures and use slightly increased for tibial/humeral fractures. Open/closed diaphyseal fractures, pathological fractures, cancer or AIDS/HIV, and alcohol abuse contributed to IMN use.
1. Introduction
Long bones, including the femur, tibia, and humerus, are the most commonly fractured bones in the human body [Citation1]. A broken hip or femur is one of the most serious fall injuries and is associated with disability and premature death [Citation2]. Each year over 300,000 older people are hospitalized for femur fractures in the US [Citation3]. Tibia fractures are common but unanticipated trauma results in painful and prolonged recovery, often associated with complications [Citation1,Citation4]. Tibia and fibula fractures annually result in 77,000 hospitalizations [Citation4]. The incidence of humeral fractures has been increasing with the aging population resulting in a large socioeconomical burden [Citation5].
Current methods used for the surgical treatment of long bone fractures include plate fixation, external fixation, and intramedullary nailing [Citation6]. Despite a lack of consensus regarding the best treatment method for fractures of the femur, tibia, and humerus, open reduction and internal fixation (ORIF) is a popular treatment option [Citation7]. In ORIF, the broken bone is surgically reduced or put back into place. Once the bone is reduced, an internal fixation device (e.g., screw, plate, rod, or pin) is placed on and/or inside the bone to ensure that the bone is stabilized for optimal healing.
Outcomes and complication rates following the treatment of long-bone fractures are not well established and depend on multiple factors such as fracture type, patient comorbidities, and surgical approach. A better understanding of the utilization of surgical treatment method by fracture anatomy and patient presentation would be helpful to benchmark current patterns of care for healthcare payers, clinicians, manufacturers, and patients. This study used administrative claims data to (1) evaluate the treatment patterns for long bone fractures (i.e., fractures of the femur, tibia and humerus); and (2) to determine the factors contributing to the use of IMN versus other internal fixation devices.
2. Methods
2.1. Data source
This study used U.S. administrative claims data from the IBM MarketScan® Commercial and Medicare Research Databases. Data included in the databases are enrollment information, demographics, inpatient and outpatient medical, and outpatient pharmacy claims. The data are collected from more than 300 large self-insured U.S. employers and over 25 U.S. health plans. Commercial data represents individuals <65 years of age (primary insured, spouse, or dependent). Demographic information includes age, gender, geographic region of the U.S., health insurance payer type, employment status, monthly enrollment status, and whether the health plan contains a mental health carve-out (i.e., mental health-related charges not covered). International Classification of Diseases, 9th and 10th Revision, Clinical Modification (ICD-9-CM and ICD-10-CM) diagnosis and procedure codes are included in the various inpatient and outpatient healthcare settings. Additional information available includes length of stay, date and duration of services, provider types, place of services, plan payments, patient deductibles, co-pay amounts, national drug codes (NDCs), therapeutic classes; dispensing dates; quantities and days supplied, and plan- and patient-paid amounts.
2.2. Patient population
Patients <65 years old diagnosed with femoral, tibial, or humeral fractures during a hospitalization between January 2016 and July 2019 were included in the study. The date of hospitalization for the fracture was considered the index date. Patients were also required to have continuous health insurance enrollment during the six months prior to the index hospitalization; this was considered the baseline period. Patients were excluded if they had evidence of any long bone fractures during the baseline period, had an amputation during the index hospitalization, or had fractures in multiple bones during the index hospitalization (polytrauma).
2.3. Outcome measures
Patients were categorized into three groups based on long bone fracture type: femur, tibia, and humerus. Patient baseline characteristics that were evaluated included age, sex, geographic region (Census region), and insurance plan type (preferred provider organization [PPO], Consumer Directed Health Plan [CDHP] or health maintenance organization [HMO]). Clinical characteristics that were evaluated included 32 comorbidities (i.e., presence of osteoporosis and 31 comorbidities from Elixhauser Comorbidity measure [Citation8]), the nature of the fracture (i.e., open, closed diaphyseal, displaced, comminuted, condylar, tuberosity, and proximal or distal), the functional comorbidity index score (range from 0 to 4+), and the injury severity score. The mean hospital length of stay (LOS) was also evaluated for each long bone fracture type.
Within each long bone fracture type, patients were categorized based on the treatment that they received. The proportions of patients receiving surgical versus non-surgical treatment were presented, along with the proportions of patients receiving IMN by long bone fracture type. Rates of utilization for IMN were reported over the 4 years for the three fracture types. The factors contributing to the use of IMN versus other internal fixation devices were also evaluated by long bone fracture type.
2.4. Statistical analyses
All study variables were analyzed descriptively. Frequency counts and proportions were provided for dichotomous and polychotomous variables. Means and standard deviations were provided for continuous variables. SAS version 9.4 was used for all statistical analyses. Logistic regression was conducted to determine the factors associated with treatment with IMN versus other internal fixation devices.
3. Results
3.1. Baseline demographic and clinical characteristics
A total of 14,961patients with femoral fractures, 14,101 patients with tibial fractures, and 7,059 patients with humeral factors were identified. Mean (SD) age was 45.3 (18.9), 42.0 (16.3), and 39.8 (21.6) years and 50.8%, 47.7%, and 55.3% of patients were female for femoral, tibial, and humeral fractures, respectively. Patients most commonly had preferred provider organization (PPO) health insurance plans and resided in the South or North Central regions of the US. Approximately one-quarter of patients had hypertension and 8.8%-12.0% had diabetes. Patients with tibial and humeral fractures less commonly had osteoarthritis, had somewhat less functional comorbidity, and more commonly had upper end and lower end fractures. The proportion of patients with displaced fractures ranged from 66.3%-81.9% and the proportion of patients with comminuted fractures ranged from 13.2%-22.1%. Over half of patients with tibial fractures had diaphyseal fractures and nearly one of five had open fractures, whereas one-third patients with femoral or humeral fractures had diaphyseal fractures and less than one in ten had open fractures ().
Table 1. Baseline demographic and clinical characteristics of patients with long bone fractures by fracture type.
3.2. Length of Stay and surgical treatment type for long bone fractures
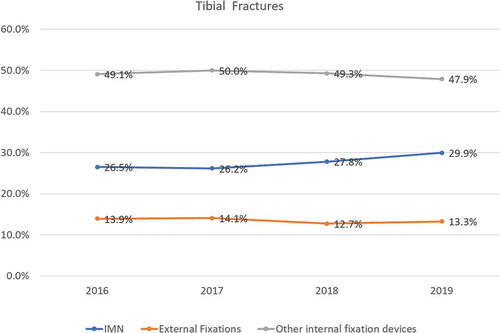
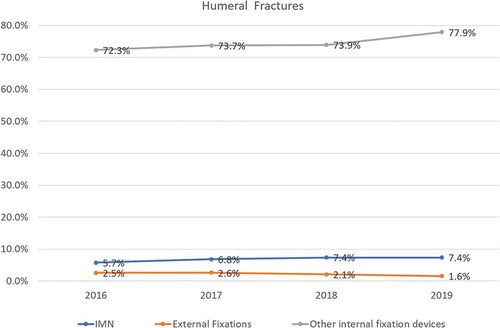
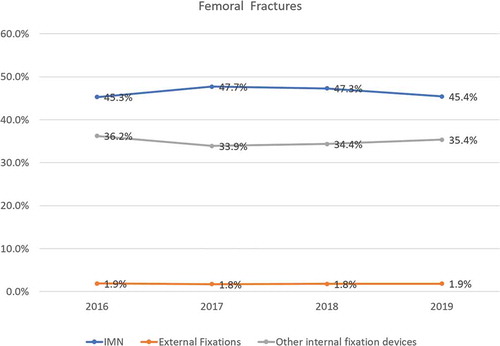
Mean (SD) lengths of stay among patients with fractures were 6.7 (9.2) days for femoral fractures, 5.9 (7.0) days for tibial fractures, and 5.8 (10.3) days for humeral fractures. Rates of surgical versus non-surgical treatment were 74.3% for femoral fractures, 84.0% for tibial fractures, and 62.7% for humeral fractures (). Among patients with surgical treatment, internal fixation was performed for 34.9% of femoral fractures, 49.3% of tibial fractures, and 73.7% of humeral fractures. Rates of external fixation among patients with surgical treatment were 1.8% for femoral fractures, 13.5% for tibial fractures, and 2.3% for humeral fractures. Rates of IMN among patients with surgical treatment were 46.6% for femoral fractures, 27.1% for tibial fractures, and 6.7% for humeral fractures (). Over the past 4 years, rates of utilization of IMN have been stable for femoral fractures and have increased slightly for tibial and humeral fractures; utilization of other internal fixation devices is still predominant in tibial and humeral fractures (–).
Figure 3. Rates of treatment type by year among patients with surgical treatment for femoral fractures.
3.3. Factors contributing to the use of imn versus other internal fixation devices
Factors contributing to the use of IMN for femoral fractures included higher injury severity score, PPO vs. HMO health insurance, presence of osteoporosis or metastatic cancer, open or closed diaphyseal fracture, pertrochanteric fracture, pathological fracture, displaced fracture, comminuted fracture, absence of proximal or distal fracture, absence of neck fracture, and absence of condylar fracture (). Presence of AIDS/HIV, absence of rheumatoid arthritis, open or closed diaphyseal fracture, pathological fracture, comminuted fracture, absence of condylar fracture, and absence of tuberosity fracture were factors contributing to the use of tibial IMN (). South vs. West region, HMO vs. PPO health insurance, presence of lymphoma, metastatic cancer, or alcohol abuse, pathological fracture, closed diaphyseal fracture, absence of surgical neck fracture, absence of condylar fracture, absence of tuberosity fracture, and absence of lower end fracture were predictive of humeral IMN ().
Table 2. Significant factors associated with treatment of intramedullary nailing (IMN) versus other internal fixation device for femoral fractures.
Table 3. Significant factors associated with receipt of intramedullary nailing (IMN) versus other internal fixation device for tibial fractures.
Table 4. Significant factors associated with receipt of intramedullary nailing (IMN) versus other internal fixation device for humeral fractures.
4. Discussion
This study of patients diagnosed with femoral, tibial, or humeral fractures during an inpatient admission showed that surgical treatment of long bone fractures was common. IMN has been used to treat fractures of long bones of the body for more than 80 years [Citation9,Citation10]. Our study findings showed that, over the past 4 years, IMN was the predominant treatment option for femoral fractures. Utilization of other internal fixation devices was still predominant in tibial and humeral fractures.
Rates of utilization of IMN have been stable for femoral fractures and have increased slightly for tibial and humeral fractures. This increasing trend in utilization is consistent with previous studies published in the medical literature. A retrospective review of US Veterans Affairs Surgical Quality Improvement Program (VASQIP) data found that use of intramedullary nails in Veterans Affairs facilities increased from 1998 through 2005 and varied by geographic region [Citation11]. An analysis of a national database of Medicare patients with intertrochanteric femur fractures found a significant increase in the percentage of IMN compared to sliding hip screw, from 46.9% IMN in 2005 to 79.1% in 2011 [Citation12].
The reasons for the utilization of IMN in femoral, tibial, and humeral fractures are multifactorial. Factors contributing to the use of IMN in the current study included diaphyseal fractures, pathological fractures, and pertrochanteric fractures, diagnoses of cancer or AIDS/HIV, and alcohol abuse. A previous study evaluating surgeon and hospital characteristics associated with the use of IMN compared with plate-and-screw devices among Medicare patients with intertrochanteric hip fractures provides some additional insights [Citation13]. Surgeon factors that were found to be associated with IMN use included younger surgeon age (<45 years), an osteopathy degree, and operating at more than one hospital. Hospital factors that were found to be associated with IMN use included a higher volume of hip fracture surgeries, teaching hospital status, and having resident assistance during surgery.
Surgical treatment of long bone fractures was especially common in patients with tibial fractures (84.0%). Patients with tibial fractures were more commonly male and were more likely to have no functional comorbidity. The complexity of treating tibial fracture patients that has been documented in the literature [Citation1,Citation4,Citation14,Citation15] was affirmed in this study as findings showed that nearly one in five patients with tibial fractures in the dataset had open fractures and over half had diaphyseal fractures. Use of IMN in patients with tibial fractures was more likely in patients with a diagnosis of AIDS/HIV and in patients without rheumatoid arthritis. Open or closed diaphyseal, pathological, or comminuted tibial fractures were factors contributing to the use of IMN. Use of IMN was less likely in patients with condylar and tuberosity tibial fractures. The strongest predictors of use of IMN with tibial fractures in this study were open or closed diaphyseal fractures.
Consistent with the literature [Citation16], our study findings showed that patients with femoral fractures were older and had greater comorbidity compared to patients with fractures of the tibia or humerus. Three-quarters of patients with femoral fracture were treated surgically. These patients had a longer LOS and IMN was used in nearly half of patients with femoral fracture who were treated surgically. Higher injury severity score, PPO vs. HMO health insurance, presence of osteoporosis or metastatic cancer, open or closed diaphyseal fracture, pertrochanteric fracture, pathological fracture, displaced fracture, comminuted fracture, absence of proximal or distal fracture, absence of neck fracture, and absence of condylar fracture were factors contributing to the use of IMN for femoral fracture. Open and closed diaphyseal fracture, pertrochanteric fracture, and pathological fracture were the strongest predictors of IMN use for femoral fractures in this study.
Nearly two-thirds of patients with fractures of the humerus were treated surgically, however IMN was not as common of a treatment approach (6.7%). Factors contributing to the use of IMN were South vs. West region, HMO vs. PPO health insurance, presence of lymphoma, metastatic cancer, or alcohol abuse, pathological fracture, closed diaphyseal fracture, absence of surgical neck fracture, absence of condylar fracture, absence of tuberosity fracture, and absence of lower end fracture. Pathological fractures and diagnoses of lymphoma or metastatic cancer were the strongest predictors of IMN use for humeral fractures.
Administrative claims data enable the assessment and monitoring of disease and treatment patterns in large samples of patients being treated in the ‘real-world’ [Citation17,Citation18]. These health services utilization data reflect payments received for healthcare services and commodities. A better understanding of the interactions that patients with long bone fractures have with the healthcare system can be helpful in improving patient quality of care [Citation19,Citation20]. The benchmarking of care of patients with long bone fractures provides a first step toward the goals of the Triple Aim of simultaneously improving the experience of care, improving the health of populations, and reducing per capita costs of healthcare [Citation21]. This information could be used to identify and prioritize healthcare improvement goals and to track progress toward those goals.
Understanding the factors contributing to the use of IMN is also helpful in improving our understanding of the rationale physicians use in deciding upon utilizing this treatment approach. Future administrative claims database studies might include measures that serve as proxies of clinical outcomes or complications. Such efforts could assist with identifying which patient populations might best be targeted for IMN, and what specific interventions might be optimal for implementing IMN for the various patient subgroups.
A limitation of this study is the use of data from administrative claims. Administrative claims data are collected for the reimbursement of healthcare goods and services, and not specifically for research. Potential problems with using administrative data for research include the risk of clerical inaccuracies, recording bias secondary to financial incentives, temporal changes in billing codes, and a lack of clinically-relevant variables and orthopedic-specific outcomes (e.g., information regarding the severity of fractures and fracture classification was not available) [Citation18,Citation22]. The inferences that can be made from administrative claims data are limited and temporal relations cannot be made. Validation studies confirming the long bone fracture practice patterns observed in this administrative claims study could be conducted through the use of medical charts or electronic health records (EHRs).
It is important to note that the patients included in this study were restricted to those with an inpatient admission. Therefore, this study did not account for patients who did not present to the hospital (e.g., presented to their physician’s office) or patients who presented to the emergency department but were not admitted and were discharged home. In an effort to homogenize the patient population evaluated in this study and optimize the integrity of analyses, patients were excluded if they had evidence of any long bone fractures during the baseline period, had an amputation during the index hospitalization, or had fractures in multiple bones during the index hospitalization (polytrauma). These restrictions limit the generalizability of findings to patients who did not have these events. As this dataset is for patients in US health plans, the findings may not be generalizable to patients in other countries or in US patients with other types of healthcare coverage. For example, the lengths of hospital stay observed in this study may vary across different US settings of care and are likely lower than what would be observed in most other countries. Also, there may be an under-estimation of surgical procedures when patients do not seek care (or are denied access). To that end, these data reflect estimated resource use of those who sought care and were covered by one of the many plans in the database
5. Conclusions
A significant proportion of long bone fractures require surgical repair. Study findings showed that, over the past 4 years, IMN was the predominant treatment option for femoral fractures. Utilization of other internal fixation devices was still predominant in tibial and humeral fractures, however rates of IMN utilization have increased slightly over the past 4 years. Factors contributing to the use of IMN included open or closed diaphyseal fractures, pathological fractures, and pertrochanteric fractures, diagnoses of cancer or AIDS/HIV, and alcohol abuse.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Declaration of interest
A Chitnis, C Sparks, Y Grebenyuk, M Vanderkarr, and C Holy are employees of JnJ; and A Chitnis, C Sparks, Y Grebenyuk, M Vanderkarr, and C Holy own stocks in the company. B Ray was a contractor with JnJ at the time of the study. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Additional information
Funding
References
- Antonova E, Le TK, Burge R, et al. Tibia shaft fractures: costly burden of nonunions. BMC Musculoskelet Disord. 2013 Jan;26(14):42.
- Marks R. Hip fracture epidemiological trends, outcomes, and risk factors, 1970-2009. Int J Gen Med. 2010;3:1–17.
- HCUPnet. Healthcare cost and utilization project (HCUP) Rockville, MD. 2012.. Available from[cited 2019]: http://hcupnet.ahrq.gov
- Miller NC, Askew AE. Tibia fractures. An overview of evaluation and treatment. Orthop Nurs. 2007 Jul-Aug;26(4):216–23;quiz 224–5.
- Kim SH, Szabo RM, Marder RA. Epidemiology of humerus fractures in the United States: nationwide emergency department sample, 2008. Arthritis Care Res (Hoboken). 2012 Mar;64(3):407–414.
- Jordan RW, Saithna A. Defining the role of intramedullary nailing for fractures of the distal radius: a systematic review. Bone Joint J. 2015 Oct;97-B(10):1370–1376.
- Rasouli MR, Viola J, Maltenfort MG, et al. Hardware removal due to infection after open reduction and internal fixation: trends and predictors. Arch Bone Jt Surg. 2015 Jul;3(3):184–192.
- Menendez ME, Neuhaus V, van Dijk CN, et al. The Elixhauser comorbidity method outperforms the Charlson index in predicting inpatient death after orthopaedic surgery. Clin Orthop Relat Res. 2014 Sep;472(9):2878–2886.
- Born CT, Pidgeon T, Taglang G. 75 years of contemporary intramedullary nailing. J Orthop Trauma. 2014;28:S1–S2.
- Vecsei V, Hajdu S, Negrin L. Intramedullary nailing in fracture treatment: history, science and Küntscher’s revolutionary influence in Vienna, Austria. Injury. 2011 Sept 01;42(Suppl 4):S1–5.
- Radcliff TA, Regan E, Cowper Ripley DC, et al. Increased use of intramedullary nails for intertrochanteric proximal femoral fractures in veterans affairs hospitals: a comparative effectiveness study. J Bone Joint Surg Am. 2012 May 2;94(9):833–840.
- Werner BC, Fashandi AH, Gwathmey FW, et al. Trends in the management of intertrochanteric femur fractures in the United States 2005-2011. Hip Int. 2015 May-Jun;25(3):270–276.
- Forte ML, Virnig BA, Eberly LE, et al. Provider factors associated with intramedullary nail use for intertrochanteric hip fractures. J Bone Joint Surg Am. 2010 May;92(5):1105–1114.
- Krieg JC. Proximal tibial fractures: current treatment, results, and problems. Injury. 2003 Aug;34(Suppl 1):A2–10.
- Henkelmann R, Frosch K-H, Glaab R, et al. Infection following fractures of the proximal tibia – a systematic review of incidence and outcome. BMC Musculoskelet Disord. 2017 Nov 21;18(1):481.
- Mavrogenis AF, Panagopoulos GN, Megaloikonomos PD, et al. Complications after hip nailing for fractures. Orthopedics. 2016 Jan-Feb;39(1):e108–16.
- Cadarette SM, Wong L. An introduction to health care administrative data. Can J Hosp Pharm. 2015 May-Jun;68(3):232–237.
- Patel AA, Singh K, Nunley RM, et al. Administrative databases in orthopaedic research: pearls and pitfalls of big data. J Am Acad Orthop Surg. 2016 Mar;24(3):172–179. .
- Auerbach A. Healthcare quality measurement in orthopaedic surgery: current state of the art. Clin Orthop Relat Res. 2009;467(10):2542–2547.
- Mauffrey C, Mavrogenis AF. Quality, cost and outcomes measures in orthopaedic healthcare. Int Orthop. 2017 Sept 01;41(9):1705–1708.
- Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008 May-Jun;27(3):759–769.
- Bohl DD, Singh K, Grauer JN. Nationwide databases in orthopaedic surgery research. J Am Acad Orthop Surg. 2016 Oct;24(10):673–682.