1. Introduction
In last decades hybrid imaging, combining molecular and anatomical data in a unique, synergistic approach, has thoroughly changed the face of medical diagnostics [Citation1,Citation2]. In particular, positron emission computed tomography (PET/CT) has established itself as an essential tool in many oncological and non-oncological scenarios [Citation3], providing the opportunity of investigating in vivo physio-pathological processes at a cellular and molecular level [Citation4,Citation5]. Notably, in recent years some technological improvements have been introduced in PET imaging, such as novel iterative reconstruction algorithms, or time-of-flight (TOF) PET/CT scanners operating in fully-3D mode [Citation6]. Most importantly, the silicon photomultiplier (SiPM)-based detectors have been implemented instead of the ‘old-fashioned’ photomultiplier tubes (PMTs) [Citation7,Citation8], giving rise to the so-called digital PET/CT (dPET/CT). With respect to the PMT-equipped PET/CT, namely analogue PET/CT (aPET/CT), dPET/CT is characterized by higher sensitivity, spatial and temporal resolution, with a significantly greater detection rate of pathological lesions, also employing fast protocols [Citation9–15].
Traditional PET/CT devices have a standard axial field-of-view (SAFOV) ranging 15–30 cm, thus being capable to cover the ‘standard’ whole-body PET/CT scan length – from skull base to the proximal thigh -, by utilizing the step-and-shot (SS) technique or the more recently introduced continuous bed motion (CBM) [Citation16]. Worthy of note, SAFOV PET/CT detectors can collect a limited number of coincidence photons, with consequent suboptimal signal-to-noise ratio (SNR) and image quality. In order to overcome the aforementioned limitations, a novel type of PET/CT scanners, characterized by a long axial field-of-view (LAFOV), has been introduced.
2. The novel LAFOV PET/CT scanners
The main characteristic of the aforementioned novel scanners (LAOFV PET/CT, also known as total-body PET/CT/TB-PET/CT) is represented by the possibility to cover the entire PET/CT scan-length in a single bed position, thanks to their extended FOV [Citation17], ranging from 64 to 194 cm [Citation18–20], as schematized in . Notably, TB-PET/CT’s sensitivity is extremely high thanks to the numerous, highly performing SiMP-based detectors collecting a huge number of coincidence-photons, with consequent improvement of SNR that, in its turn, positively impacts on image quality. The aforementioned technical characteristics entail three major advantages when LAFOV scanners are employed: 1) the possibility to implement fast or ultra-fast protocols, thus reducing eventual movement artifacts and resulting particularly useful in case of severely debilitated subjects; 2) the possible administration of low or ultra-low radiopharmaceuticals’ activities, therefore favorably impacting on delivered radiation burden; 3) the feasibility of accurate PET dynamic studies including parametric imaging. as shown in .
Figure 1. An example of 18F-FDG Maximum Intensity Projection (MIP) images obtained by dynamic acquisition with a LAFOV PET/CT scanner (Biograph Vision Quadra, Siemens Healthineers) in a patient with metastatic melanoma and several lesions in the thoracic area (image courtesy of Prof. Antonia Dimitrakopoulou-Strauss).
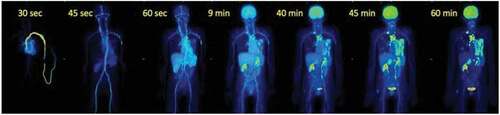
Table 1. Schematization of the main technical features of PET/CT scanners mentioned in the manuscript.
3. Applications in oncology
3.1. 18F-FDG
The majority of malignancies employs glycolysis as a preferential source to produce the energy needed for tumor growth and proliferation, therefore expressing glucose transporter (GLUT) to incorporate this substrate into the cell [Citation21]. This preferential metabolic pathway has determined the success and wide-spreading of 18F-fluorodeoxyglucose (18F-FDG), a radiolabeled analogue of glucose, as the most commonly utilized radiopharmaceutical in oncology.
Some preliminary studies were focused on TB-PET/CT’s applications for the 18F-FDG imaging of cancer patients with dedicated protocols. In 78 patients with hepatic tumors, Hu and coworkers carried out a standard 15-min TB-PET/CT scan (G15) and then reconstructed PET raw data by utilizing acquisition duration of 2 min (G2) [Citation22]. When comparing the diagnostic performance of standard (G15) and fast (G2) PET/CT scans, no significant differences were registered in the number of detected hepatic lesions among the two protocols employed, although three pathological lymph nodes were missed by G2. However, PET-based staging according to TNM classification resulted substantially concordant among the standard and the fast protocol.
TB-PET/CT scan at low or ultra-low dose represents a particularly relevant issue in pediatric patients [Citation23]. In a retrospective analysis including 100 oncological children who underwent a TB-PET/CT scan with 18F-FDG half-dose (i.e. 1.85 MBq/kg), Chen et al. firstly reconstructed PET images by utilizing the complete 600-second acquisition data (G600) and then utilizing 300-s, 180-s, 60-s, 40-s, and 20-s (G300-G20) data [Citation24]. Image quality was compared among the various reconstructed PET scans both visually (i.e. 5-point Likert scales) and quantitatively, by calculating several parameters (e.g. SUVmax, SUVmean, SNR, etc). Subjective qualitative score resulted concordant for G600, G300, and G180 and higher than that assigned to G60. Notably, all the lesions detected in the G600 resulted detectable in the G60 too, while only the 56% of the lesions were identified in the G20 scan. In light of the above, the authors suggested half-dose TB-PET/CT to be feasible in pediatric cancer patients, with reasonable diagnostic performance also when fast 60-s protocol is applied.
Dynamic PET data acquisition represents a cornerstone of parametric imaging, since it allows to assess radiopharmaceuticals’ biokinetics over time, an essential information not only for pharmacological studies but also for an accurate assessment of tumors’ biological behavior [Citation25]. Nevertheless, in spite of its high potential in oncology, dynamic PET/CT has not been fully explored yet, mainly because it is time-consuming and requires sophisticated algorithms of calculation [Citation26]. In this respect, recently introduced LAFOV PET/CT scanners hold the promise to be a game-changer due to their increased sensitivity. In this regard, it has to be mentioned the recently published study by Wang et al. [Citation27]. The authors performed a 60-min dynamic 18F-FDG TB-PET/CT in 30 patients with newly diagnosed non-small cell lung cancer (NSCLC) in order to investigate metabolic heterogeneity in primary tumor (PT) and metastatic lymph nodes (mLN) before therapy: quantitative parameters (e.g. Patlak-Ki, SUVmean, metabolic tumor volume/MTV, total lesion glycolysis/TLG, textural features) were calculated for PT and mLN; furthermore, next generation sequencing (NGS) was also carried out to determine tumor-associated molecular profile and then correlated with imaging results. According to dynamic PET data, patients were split into fast dynamic 18F-FDG metabolic group (F-DFM) and slow dynamic 18F-FDG metabolic group (S-DFM): subjects in the F-DFM group presented more homogenous 18F-FDG uptake than those in the S-DFM group and also showed higher infiltrations of T cells and macrophages, thus being potentially suitable to be treated with immunotherapeutic regimens. Of note, all the encouraging preliminary results obtained with 18F-FDG total-body PET/CT in oncology led to the recent publication of the first expert consensus document on this topic [Citation28].
3.2. PSMA-ligands
TB-PET/CT has been increasingly applied for the imaging with radiopharmaceuticals other than 18F-FDG in oncology. In particular, prostate specific membrane antigen (PSMA), a molecule overexpressed on cell membrane of prostate cancer (PC) and only minimally detectable in prostate normal tissue, has recently emerged as a valuable target for combining diagnosis and therapy into the ‘theranostic’ approach [Citation29]. In this regard, several PSMA-targeted radiolabeled ligands, such as 68Ga-PSMA-11 and 18F-PSMA-1007, have been introduced in clinical practice for the imaging of PC biochemical recurrence (BCR) [Citation30]. It has to be underlined that 68Ga-PSMA-11 PET/CT for PC BCR diagnosis is conventionally performed at 1 h post injection (p.i.), even though imaging at later time-points has been reported to be characterized by better tumor-to-background ratio (TBR) and lesions’ detectability [Citation31]. However, PET/CT image quality at late time-points may be hampered by the low count rate due to the relatively brief 68Ga half-life (i.e. 68 min). In this regard, Alberts and colleagues have recently investigated the potential of LAFOV PET/CT in a retrospective study performed on 10 patients submitted to 68Ga-PSMA-11 TB-PET/CT carried out at 1 h p.i. and then followed by an additional late image at 4 h p.i [Citation32]. PET images at 1 and 4 h were assessed both qualitatively and quantitatively by two experienced investigators: while image quality was scored as slightly better for standard 1-h scan, higher TBR and SNR were obtained at late 4-h imaging. In light of the foregoing,68Ga-PSMA-11 PET/CT acquisition at late time should be preferred for PC BCR diagnosis, when LAFOV devices are employed. Dynamic PET-CT imaging with 68Ga-PSMA-11 may be also be helpful as reported by Strauss et al. in a recent paper: the authors demonstrated a time window in the first 10 min where tumor uptake was high, but no bladder activity was measured, aiding accuracy in distinction of local recurrence. Kinetic modeling provided additional information for tumor characterization by tissue type [Citation33].
4. Applications in non-oncological fields
18F-FDG PET/CT is widely used for the diagnosis and monitoring of inflammation and infection, mainly thanks to the increased GLUT expression in activated inflammatory cells and infectious agents [Citation34]. In a prospective observational study, 30 patients (24 affected by autoimmune inflammatory arthritides/AIA and 6 with osteoarthritis/OA) underwent a 20-min TB-PET/CT scan starting 40 min after the i.v. administration of 18F-FDG at ultra-low dose (i.e. 78.1 ± 4.7) [Citation35]. TB-PET/CT provided an accurate assessment of the inflammatory involvement at joints of the entire patients’ body; furthermore, a concordance between 18F-FDG qualitative assessment and rheumatologic findings was registered for the 69.9% and 91.1% of the joints in AIA and OA cohorts, respectively. Notably, quantitative measures of 18F-FDG uptake in AIA subjects presented a moderate to strong correlation with rheumatologic data.
summarizes the main findings and the employed LAFOV scanners in the cited papers in oncological and non-oncological fields.
Table 2. Summary of the cited papers on the applications of TB-PET/CT in oncological and non-oncological fields.
5. Conclusions and future outlook
Technological improvement has always played a crucial role for diagnostic imaging development. In this perspective, LAFOV devices are moving the field forward, laying the foundation for a real revolution through the implementation of fast-scan or low-activity studies [Citation36].
Although preliminary data suggest that fast-scan or low-activity protocols result as accurate as the standard 15/20-min or full-activity scans for lesions’ detection, the majority of the studies carried out until now included relatively small cohorts of subjects and presented a retrospective design, thus being hampered by possible selection bias. Furthermore, it has still to be defined how much inter-individual heterogeneity in body mass index (BMI) might impact on TB-PET/CT protocols [Citation37]. However, it is clear that LAFOV scanners provide a higher sensitivity and allow low dose imaging. New reconstruction algorithms based on artificial intelligence and automatic segmentation of TB-PET/CT images will lead to a better and more standardized image evaluation, a prerequisite for the improvement of diagnosis and particularly for therapy monitoring. Standardized calculation of parametric images, like Patlak plot analysis, may facilitate the clinical use of dynamic TB-PET/CT together with shortened acquisition protocols. It is also open at the moment what is the optimal length for the scanners with the extended field of view. All these issues will be topics of larger prospective studies.
The ‘TB-PET/CT era’ is upcoming. Although we are not fully prepared for this revolution, the various nuclear medicine departments should definitely not miss the opportunity to lay hold of this powerful technology that, thanks to the ultra-high sensitivity and extended scan length, has been gaining an ever-increasing importance in oncology and non-oncological field. However, some issues have to be addressed, both on logistic and ethical sides. In regards to patients’ logistic management, if on the one hand TB-PET/CT still presents some of the typical limitations that affect SAFOV PET/CT, such as claustrophobia – that can be amplified by the extended field-of-view – and lack of access to injection sites during the scan, on the other hand the potentially increased patients’ output per day, allowed by the implementation of fast or very-fast protocols, might entail new logistic problems, such as the need of medical and para-medical dedicated personnel (physicians, nurses, radiology technician, etc.) and tracer’s availability.
Furthermore, LAFOV devices’ high economic impact might limit their wide-spreading and also rises ethical issues, since it paves the ground to relevant disparities in TB-PET/CT’s availability among countries. To the best of our knowledge, a TB-PET/CT’s cost-effectiveness analysis and an evaluation of its sustainability from the various healthcare systems have not been performed yet. In this regard, the sci-fi movie Elysium, set in a dystopian future where the dichotomy between rich and poor people has become irreconcilably deep, sounds as a sinister warning: while the poor are condemned to live in squalor on Earth, the rich escaped to the space-based colony Elysium, where they have a healthy, long life thanks to a device very similar to a TB-PET/CT, a magic ‘medicine-bed’ capable of diagnosing and healing any ailment. On this path, it is mandatory to put LAFOV PET/CT scanners under the spotlight in the international development debate, involving scholars from different disciplines (science, economy, politics, law, etc …) in the discussion, in order to find the most appropriate solution to minimize inequities and prevent the concretization of dystopian perspectives.
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewers disclosure
Peer reviewers on this manuscript have no relevant financial relationships or otherwise to disclose.
Acknowledgments
None
Additional information
Funding
References
- Cal-Gonzalez J, Rausch I, Shiyam Sundar LK, et al. Hybrid imaging: instrumentation and data processing. Front Phys. 2018;6:47.
- Filippi L, Biancone L, Petruzziello C, et al. Tc-99m HMPAO-labeled leukocyte scintigraphy with hybrid SPECT/CT detects perianal fistulas in crohn disease. Clin Nucl Med. 2006;31(9):541–542.
- Ell PJ, Kayani I, Groves AM. 18F-fluorodeoxyglucose PET/CT in cancer imaging. Clin Med. 2006;6(3):240–244.
- Hammes J, Bischof GN, Drzezga A. Molecular imaging in early diagnosis, differential diagnosis and follow-up of patients with neurodegenerative diseases. Clin Transl Imaging. 2017;5(5):465–471.
- Filippi L, Scopinaro F, Pelle G, et al. Molecular response assessed by 68Ga-DOTANOC and survival after 90Y microsphere therapy in patients with liver metastases from neuroendocrine tumours. Eur J Nucl Med Mol Imaging. 2016;43(3):432–440.
- Surti S. Update on Time-of-Flight PET Imaging. J Nucl Med. 2015;56(1):98–105.
- Fabbri A, Cencelli VO, Bennati P, et al. Dual isotope imaging with LaBr3: cecrystal and H8500 PSPMT. J Inst. 2013;8. C02022–C02022.
- Gundacker S, Heering A. The silicon photomultiplier: fundamentals and applications of a modern solid-state photon detector. Phys Med Biol. 2020;65(17):17TR01.
- Filippi L, Schillaci O. Digital PET and detection of recurrent prostate cancer: what have we gained, and what is still missing? Expert Rev Med Devices. 2021;18(11):1107–1110.
- Alberts I, Prenosil G, Sachpekidis C, et al., Digital versus analogue PET in [68Ga]Ga-PSMA-11 PET/CT for recurrent prostate cancer: a matched-pair comparison. Eur J Nucl Med Mol Imaging. 2020;47(3):614–623.
- Jakoby BW, Bercier Y, Conti M, et al. Physical and clinical performance of the mCT time-of-flight PET/CT scanner. Phys Med Biol. 2011;56(8):2375–2389.
- Rausch I, Cal-González J, Dapra D, et al. Performance evaluation of the Biograph mCT Flow PET/CT system according to the NEMA NU2-2012 standard. EJNMMI Phys. 2015;2(1):26.
- Carlier T, Ferrer L, Conti M, et al. From a PMT-based to a SiPM-based PET system: a study to define matched acquisition/reconstruction parameters and NEMA performance of the biograph vision 450. EJNMMI Physics. 2020;7(1):55.
- van Sluis J, de Jong J, Schaar J, et al. Performance characteristics of the digital biograph vision PET/CT system. J Nucl Med. 2019;60(7):1031–1036.
- Alberts I, Sachpekidis C, Prenosil G, et al. Digital PET/CT allows for shorter acquisition protocols or reduced radiopharmaceutical dose in [18F]-FDG PET/CT. Ann Nucl Med. 2021;35(4):485–492.
- Siman W, Kappadath SC. Comparison of step-and-shoot and continuous-bed-motion PET modes of acquisition for limited-view organ scans. J Nucl Med Technol. 2017;45(4):290–296.
- Katal S, Eibschutz LS, Saboury B, et al. Advantages and applications of total-body PET scanning. Diagnostics. 2022;12(2):426.
- Pantel AR, Viswanath V, Daube-Witherspoon ME, et al. PennPET explorer: human imaging on a whole-body imager. J Nucl Med. 2020;61(1):144–151.
- Prenosil GA, Sari H, Fürstner M, et al. Performance characteristics of the biograph vision quadra PET/CT system with a long axial field of view using the NEMA NU 2-2018 standard. J Nucl Med. 2022;63(3):476–484.
- Spencer BA, Berg E, Schmall JP, et al. Performance evaluation of the uEXPLORER total-body PET/CT scanner based on NEMA NU 2-2018 with additional tests to characterize PET scanners with a long axial field of view. J Nucl Med. 2021;62(6):861–870.
- Carvalho KC, Cunha IW, Rocha RM, et al. GLUT1 expression in malignant tumors and its use as an immunodiagnostic marker. Clinics. 2011;66(6):965–972.
- Hu Y, Liu G, Yu H, et al. Diagnostic performance of total-body 18F-FDG PET/CT with fast 2-min acquisition for liver tumours: comparison with conventional PET/CT. Eur J Nucl Med Mol Imaging. 2022;49(10):3538–3546.
- Mohammadi N, Akhlaghi P. Evaluation of radiation dose to pediatric models from whole body PET/CT imaging. J Applied Clin Med Phys. 2022;23(4). DOI:10.1002/acm2.13545.
- Chen W, Liu L, Li Y, et al. Evaluation of pediatric malignancies using total-body PET/CT with half-dose [18F]-FDG. Eur J Nucl Med Mol Imaging. 2022;49(12):4145–4155.
- Dimitrakopoulou-Strauss A, Pan L, Sachpekidis C. Parametric imaging with dynamic PET for oncological applications: protocols, interpretation, current applications and limitations for clinical use. Semin Nucl Med. 2022;52:312–329.
- Dimitrakopoulou-Strauss A, Pan L, Sachpekidis C. Kinetic modeling and parametric imaging with dynamic PET for oncological applications: general considerations, current clinical applications, and future perspectives. Eur J Nucl Med Mol Imaging. 2021;48(1):21–39.
- Wang D, Zhang X, Liu H, et al., Assessing dynamic metabolic heterogeneity in non-small cell lung cancer patients via ultra-high sensitivity total-body [18F]FDG PET/CT imaging: quantitative analysis of [18F]FDG uptake in primary tumors and metastatic lymph nodes. Eur J Nucl Med Mol Imaging. 2022;49(13): 4692–4704.
- Yu H, Gu Y, Fan W, et al. Expert consensus on oncological [18F]FDG total-body PET/CT imaging (version 1). Eur Radiol. 2022. DOI:10.1007/s00330-022-08960-8.
- Filippi L, Chiaravalloti A, Schillaci O, et al. The potential of PSMA-targeted alpha therapy in the management of prostate cancer. Expert Rev Anticancer Ther. 2020;20(10):823–829.
- Fendler WP, Bluemel C, Czernin J, et al. PET imaging in prostate cancer, future trends: PSMA ligands. Clin Transl Imaging. 2016;4(6):467–472.
- Alberts I, Sachpekidis C, Gourni E, et al. Dynamic patterns of [68Ga]Ga-PSMA-11 uptake in recurrent prostate cancer lesions. Eur J Nucl Med Mol Imaging. 2020;47(1):160–167.
- Alberts I, Prenosil G, Mingels C, et al. Feasibility of late acquisition [68Ga]Ga-PSMA-11 PET/CT using a long axial field-of-view PET/CT scanner for the diagnosis of recurrent prostate cancer—first clinical experiences. Eur J Nucl Med Mol Imaging. 2021;48(13):4456–4462.
- Strauss DS, Sachpekidis C, Kopka K, et al. Pharmacokinetic studies of [68 Ga]Ga-PSMA-11 in patients with biochemical recurrence of prostate cancer: detection, differences in temporal distribution and kinetic modelling by tissue type. Eur J Nucl Med Mol Imaging. 2021;48(13):4472–4482.
- Wahl RL, Dilsizian V, Palestro CJ. At Last, 18 F-FDG for Inflammation and Infection! J Nucl Med. 2021;62(8):1048–1049.
- Abdelhafez Y, Raychaudhuri SP, Mazza D, et al. Total-Body 18 F-FDG PET/CT in autoimmune inflammatory arthritis at ultra-low dose: initial observations. J Nucl Med. 2022;63(10):1579–1585.
- Slart RHJA, Tsoumpas C, Glaudemans AWJM, et al. Long axial field of view PET scanners: a road map to implementation and new possibilities. Eur J Nucl Med Mol Imaging. 2021;48(13):4236–4245.
- Xiao J, Yu H, Sui X, et al. Can the BMI-based dose regimen be used to reduce injection activity and to obtain a constant image quality in oncological patients by 18F-FDG total-body PET/CT imaging? Eur J Nucl Med Mol Imaging. 2021;49(1):269–278.
