1. Background
Parkinson’s disease (PD) commonly affects both visual and cognitive functions, which is complicated by the fact that these functions are inter-related (termed visuo-cognition). Visuo-cognitive deficits range from impairments in basic visual functions (i.e. acuity and contrast sensitivity) to higher levels of visual attention and perception. Studies have shown that people with PD are more likely to experience visual impairments, and these impairments are associated with an increased risk of hip fracture, depression, anxiety, dementia, and hallucinations [Citation1]. Furthermore, visuo-cognitive dysfunction is associated with freezing of gait in PD, which is one of the most common reasons for falls and dependency in this population [Citation2].
Accurate and timely diagnosis of visuo-cognitive impairments is important in PD, as early intervention could prevent loss of independence and reduce falls risk. In practice, visuo-cognitive function is assessed using pen and paper outcome measures or eye charts, which can be subjective (based on expert rating), time-consuming and only examine global function. Visuo-cognitive function is rarely considered for rehabilitation in PD, with limited studies using eye movement exercises, pen and paper tasks, or inter-active games to improve visuo-cognitive performance. There is a need for a more objective technological approach that can comprehensively assess and provide rehabilitation for visuo-cognitive deficits in PD.
Here, we present the package of visuo-cognitive tools offered by Senaptec Ltd., a company who have developed a series of digital technologies that can be deployed with healthy and clinical populations to assess and rehabilitate visuo-cognitive function (https://senaptec.com/). We discuss how this technology may offer a solution to address the need for faster diagnosis of, and targeted intervention for, visuo-cognitive deficits in PD.
1. Senaptec visuo-cognitive technology
1.1. Using the senaptec sensory station
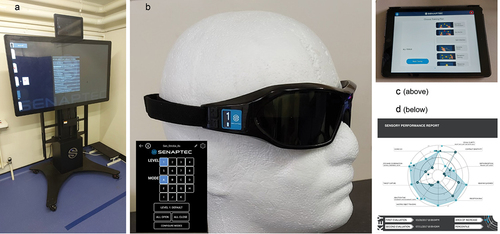
The Senaptec Sensory Station (SSS) is a computerized tool designed to evaluate and train visuo-cognitive function [Citation3–5]. It is an interactive touch screen device consisting of a computer that controls two LCD monitors mounted on a height adjustable pedestal (). The station runs on an Android operating system and uses cloud-based technology to manage data and create user profiles and progress reports for each individual.
Figure 1. a. Senaptec Sensory Station; b. Senaptec Strobe Glasses operated via buttons at side of glasses or remotely via a mobile application; c. Senaptec Application; d. Radar chart.
There are a variety of visuo-cognitive impairments in PD that require a comprehensive assessment battery, which the SSS has the potential to provide. The SSS assessment includes demographic information, as well as vision correction and medical history. Individuals complete a battery of 10 computerized tasks that are administered with video instructions. The interactive task battery includes measures such as acuity, contrast sensitivity and depth perception, as well as tasks that rely on visuo-cognitive and motor function such as reaction time, perception span, and multiple-object tracking. Tasks are performed at close range (2 feet) on the main screen or via a smartphone interface for training at a distance (10 feet). The visuo-cognitive assessments in the SSS have been validated against reference measures in healthy populations [Citation3]. Additionally, test–retest reliability on the SSS has been demonstrated in healthy individuals, with no significant differences between repeated assessments [Citation6].
1.2. Intervention with senaptec technology
1.2.1. Strobe/quad strobe glasses
People with PD (and older adults) become increasingly reliant on visuo-cognition for mobility, which may require sensory reweighting training to overcome functional problems and improve performance. Stroboscopic visual perturbation has been shown to be a valid assessment method for sensory dependence and reweighting [Citation7]. In addition to offering the SSS, Senaptec produce glasses which have liquid crystal lens technology that allows the lenses to strobe between clear and opaque (). These glasses block visual information intermittently during fully mobile tasks and have been used in a variety of sporting and clinical contexts as a means of training visuo-cognitive abilities and improving motor performance.
The strobe frequency and pattern () can be controlled from the side of the glasses (using two buttons) or remotely using the accompanying mobile application (), so a patient or clinician can control the visual input received during tasks and allow progressions to be made during rehabilitation. The lens mode settings can be customized according to which aspects of vision are being trained. For example, one lens can remain strobing, while the other lens remains opaque, which allows targeted training of a non-dominant eye or peripheral vision. The Quad Strobe lenses are divided into four segments which allow different regions of the lens to be activated (or occluded). This modification may be of particular use in conditions such as stroke or multiple sclerosis where visual field deficits are more common.
Table 1. Strobe levels, settings.
1.2.2. Senaptec application
Home-based and patient-centered rehabilitations that can be undertaken by patients without clinicians needing to be present are needed for PD. The ‘Senaptec App’ is a portable training extension of the SSS assessment/rehabilitation, which can be used on a tablet within any environment and works on both Android and iOS platforms ().
The Senaptec App uses algorithms to automatically increase the difficulty of the training in line with subject performance, which reduces the need for clinical input into rehabilitation progression. The data and algorithm are synchronized with an onlline hub, which is a secure cloud-based technology to manage the data and provide results during the rehabilitation program. This can be remotely accessed by clinicians to monitor adherence and progression. The App includes 15 training modules aimed at targeting different aspects of visuo-cognitive and visuo-motor function, such as eye-hand co-ordination, depth perception, and multiple-object tracking.
1.3. Senaptec solution outcomes/reports
The Sensory Performance report is presented on a radar chart that provides a simple summary of overall performance (). The further the score from the center of the chart, the better the performance in that area of sensory function. The summary provides a percentile ranking to show specific patient strengths and areas for improvement. The report is available immediately upon completion of the evaluation, and raw data can be downloaded for further analysis or research, with the specific metrics for the assessments (e.g. LogMar scores).
1.4. Use of Senaptec solutions for clinical assessment and intervention
The Senaptec solutions have been used with healthy young individuals and more recently, within clinical populations for assessment and rehabilitation of visuo-cognitive function. Studies on healthy individuals have shown that visuo-cognitive outcomes can predict real-world task performance, such as goal scoring ability in hockey players [Citation4] and collision avoidance in football players [Citation8]. Additionally, the use of Strobe Glasses as an intervention/training tool has been shown to improve eye-hand co-ordination, sensory weighting, and attentional capabilities in healthy populations [Citation7,Citation9,Citation10].
In terms of clinical populations, assessment using the SSS has highlighted visuo-cognitive deficits following neurological injury, specifically concussion in sport and military populations [Citation11,Citation12], with links to subsequent mobility impairment [Citation13]. SSS outcomes have been found to improve with stroboscopic visual training in those with concussion, with modifications in underlying brain activity [Citation14]. As a result, the SSS is often used as a baseline measure of visuo-cognitive performance prior to neurological injury [Citation11]. Older adults and those with neurological diseases have also benefited from stroboscopic visual training. For example, older adults and people with multiple sclerosis have been shown to benefit even within a single session of rehabilitation [Citation15,Citation16]. Stroboscopic visual training has also been found to be useful for musculoskeletal injuries, such as anterior cruciate ligament injury, with balance improvements resulting from sensory perturbation during rehabilitation [Citation17]. These clinical applications demonstrate that technologies such as the Senaptec solution show promise for use within a variety of settings and within a range of populations in the future, including PD.
2. Future work
In 2020, Senaptec Ltd. and Northumbria University formed a collaboration to develop a clinical study to examine the feasibility and initial efficacy of using the Senaptec solutions in individuals with PD. The study is currently underway and involves 40 people with PD undergoing either standard care or the Senaptec technological visuo-cognitive training (TVT) over a 4-week period [Citation18]. All participants are assessed using the SSS pre- and post-intervention, and those in the TVT arm use the strobe glasses and Senaptec App for home-based rehabilitation twice per week with a physiotherapist. The clinical study will take 36 months to complete, with subjects recruited from the Northumbria Healthcare NHS Foundation Trust and the Gateshead Health NHS Foundation Trust. If the findings demonstrate that the Senaptec solutions are useful for visuo-cognitive assessments and rehabilitation in PD, this would support their use as a potential means of objectively and comprehensively providing visuo-cognitive care for patients in a variety of settings.
Longer term randomized trials are needed to determine whether use of this platform leads to a sustained improvement in visuo-cognitive outcomes in both healthy individuals and those with neurological diseases. In PD specifically, studies should explore the role of Senaptec technology in those with freezing of gait. Further work is also required to determine the feasibility of integrating these Senaptec tools into existing health-care practices, taking into account costs, user-acceptability and current clinical practices.
Beyond the scope of the ongoing study, we envisage that the Senaptec solutions could be useful for disease progression monitoring and may aid in early diagnostics of PD. Other areas of potential use would be drug development pipelines, where response to medication or deep brain stimulation may be objectively measured. These applications would greatly improve the care of people with PD.
3. Summary
The technical feasibility of the Senaptec solutions for visuo-cognitive assessment and rehabilitation has been established in healthy and clinical populations. Work is underway to assess the use of these solutions with PD, which may prove to provide a time-efficient and user-friendly tool that can be used by non-experts (even patients) to diagnose and rehabilitate visuo-cognitive impairment.
Declaration of interest
Julia Das is funded by a Northumbria University PhD studentship in collaboration with Senaptec Ltd (Beaverton, Oregon, USA) as well as a Movement Disorder Research Grant from the British Geriatric Society. Samuel Stuart is funded in part by a Parkinson’s Foundation post-doctoral fellowship for basic scientists (PF-PDF-1898) and a clinical research award (PF-CRA-2073). The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewers disclosure
Peer reviewers on this manuscript have no relevant financial relationships or otherwise to disclose.
Additional information
Funding
References
- Hamedani AG, Abraham DS, Maguire MG, et al. Visual impairment is more common in Parkinson’s disease and is a risk factor for poor health outcomes. Mov Disord. 2020;35(9):1542–1549.
- Peterson DS, King LA, Cohen RG, et al. Cognitive contributions to freezing of gait in Parkinson disease: implications for physical rehabilitation,” (in eng). Phys Ther. 2016 May;96(5):659–670.
- Wang L, Krasich K, Bel-Bahar T, et al. Mapping the structure of perceptual and visual-motor abilities in healthy young adults,” (in eng). Acta Psychol (Amst). 2015May;157:74–84.
- Poltavski D, Biberdorf D. The role of visual perception measures used in sports vision programmes in predicting actual game performance in Division I collegiate hockey players,” (in eng). J Sports Sci. 2015;33(6):597–608.
- Erickson GB. Review: visual performance assessments for sport. Optometry Vision Sci. 2021;98(7):672–680. DOI:10.1097/OPX.0000000000001731.
- Erickson GB, et al. Reliability of a computer-based system for measuring visual performance skills. Optomet-J Am Optomet Assoc. 2011;82(9):528–542.
- Kim KM, Kim JS, Oh J, et al. Stroboscopic vision as a dynamic sensory reweighting alternative to the sensory organization Test,” (in eng). J Sport Rehabil. 2020 May 29; 1–7. DOI:10.1123/jsr.2019-0466.
- Harpham JA, Mihalik JP, Littleton AC, et al. The effect of visual and sensory performance on head impact biomechanics in college football players,” (in eng). Ann Biomed Eng. 2014 Jan;42(1):1–10.
- Ellison P, et al. The effect of stroboscopic visual training on eye–hand coordination. Sport Sci Health. 2020;16(3):401–410.
- Ballester R, Huertas F, Uji M, et al. Stroboscopic vision and sustained attention during coincidence-anticipation. Sci Rep. 2017;7(1):1–7.
- Fraser MA, Kilchrist LM, Kuo M. Concussion baseline retesting is necessary when initial scores are low. Clin J Sport Med. 2022;32(1):e40–e51.
- DeCicco JP, et al. The relationship between neurovascular coupling, vision and sensory performance, and concussion history in special operations forces combat soldiers. Clin Neuropsychol. 2020;34(6):1215–1225.
- Avedesian JM, Covassin T, Baez S, et al. Relationship between cognitive performance and lower extremity biomechanics: implications for sports-related concussion. Orthop J Sports Med. 2021;9(8):23259671211032246.
- Poltavski DV, Biberdorf DH, Praus Poltavski CA. Which comes first in sports vision training: the software or the hardware update? Utility of electrophysiological measures in monitoring specialized visual training in youth athletes. Front Hum Neurosci. 2021;566:732303. DOI:10.3389/fnhum.2021.732303.
- Shalmoni N, Kalron A. The immediate effect of stroboscopic visual training on information-processing time in people with multiple sclerosis: an exploratory study. J Neural transm. 2020;127(8):1125–1131.
- Chen Y-C, Chou Y-C, Hwang I-S. Reliance on visual input for balance skill transfer in older adults: EEG connectome analysis using minimal spanning tree. Front Aging Neurosci. 2021;13:632553.
- Wohl TR, Criss CR, Grooms DR. Visual perturbation to enhance return to sport rehabilitation after anterior cruciate ligament injury: a clinical commentary. Int J Sports Phys Ther. 2021;16(2):552.
- Das J, et al. Exploring the feasibility of technological visuo-cognitive training in Parkinson’s: study protocol for a pilot randomised controlled trial,” (in eng). PLoS One. 2022;17(10):e0275738.
