Abstract
Health care costs incurred prior to the appropriate patient–provider transaction (i.e., transaction costs of access to health care) are potential barriers to accessing health care in low- and middle-income countries. This paper explores these transaction costs and their implications for health system governance through a cross-sectional survey of adult patients who received their first diagnosis of pulmonary tuberculosis (TB) at the three designated secondary health centres for TB care in Ebonyi State, Nigeria. The patients provided information on their care-seeking pathways and the associated costs prior to reaching the appropriate provider. Of the 452 patients, 84% first consulted an inappropriate provider. Only 33% of inappropriate consultations were with qualified providers (QP); the rest were with informal providers such as pharmacy providers (PPs; 57%) and traditional providers (TP; 10%). Notably, 62% of total transaction costs were incurred during the first visit to an inappropriate provider and the mean transaction costs incurred was highest with QPs (US$30.20) compared with PPs (US$14.40) and TPs (US$15.70). These suggest that interventions for reducing transaction costs should include effective decentralisation to integrate TB care with services at the primary health care level, community engagement to address information asymmetry, enforcing regulations to keep informal providers within legal limits and facilitating referral linkages among formal and informal providers to increase early contact with appropriate providers.
Introduction
One of the objectives of health systems globally is to provide universal access to quality health care without exposing patients to the risk of financial hardship (World Health Organization [WHO], Citation2010). However, growing evidence suggests that patients tend to incur substantial health care costs prior to the appropriate patient–provider transaction (Ukwaja, Alobu, Igwenyi, & Hopewell, Citation2013). These costs can be described as transaction costs of access to health care, and they include costs incurred while seeking inappropriate care.Footnote 1 Transaction costs, separate from the actual costs of diagnosis and treatment, constitute a potential barrier to accessing health care and typically arise when there is an asymmetry of health care information, poor coordination and weak regulation of health care markets (Jan, Pronyk, & Kim, Citation2008; Williamson, Citation1979), factors that tend to be prevalent in low- and middle-income countries (LMICs; Bloom, Standing, & Lloyd, Citation2008). Thus, reducing reliance on direct, out-of-pocket payments for the appropriate patient–provider transaction may do little to address the barriers to treatment faced by patients without more comprehensive strategies aimed at reducing inappropriate pre-diagnosis and pre-treatment costs. In this paper, we examine these costs using the concept of transaction costs to explore patient–provider transactions (Coase, Citation1960).
From the perspective of a patient, the transaction costs of access to health care refer to the costs incurred in obtaining health care that are not transferred to the appropriate health care provider (Wallis & North, Citation1986). These include the cost of information to determine what service is required and if, where and at what cost the service is available; the costs of finding a trustworthy and affordable provider; the cost of bargaining to reach an agreement with the provider; and the costs of monitoring to ensure they fulfil the agreement, and if not, the cost of legal action (Williamson, Citation1979). These costs may be incurred as patients move from one health provider to another, shopping around until they find the appropriate provider who can successfully diagnose and treat their illness. The extent of transaction costs in health systems depends on the level of institutional preconditions for the efficient functioning of health care markets – information, coordination and regulation (Leonard, Bloom, Hanson, O'Farrell, & Spicer, Citation2013). In communities with well-informed residents, low-cost transportation and communication, a well-organised and regulated health care market and reliable legal safeguards, most of the transaction costs of access to health care are avoided (Stiles, Mick, & Wise, Citation2001). In the absence of prior investments in these governance interventions, whether by a community, government or local health market, transaction costs can constitute a barrier of access to health care (Abimbola, Negin, Jan, & Martiniuk, Citation2014).
However, it is difficult to examine transaction costs empirically because most transaction costs do not exist in reality, ‘but in realities that have been avoided’ (Buckley & Chapman, Citation1997) as a result of the governance interventions already in place. Given the difficulty of measuring transaction costs that may constitute these barriers (Wang, Citation2007), in this study we estimate the transaction costs of access to health care among a sample of patients in Nigeria who had been diagnosed and were receiving treatment for tuberculosis (TB). The National Tuberculosis Control Programme (NTP) in Nigeria is based on the directly observed treatment, short-course strategy in which services are provided through selected secondary care facilities across the country where patients with suspected TB are diagnosed and treated (Federal Ministry of Health [FMOH], Citation2010). For patients to reach an NTP provider for appropriate care, the programme relies on self-referral or a referral from peripheral health providers without the capacity to diagnose and treat TB. Therefore, the transaction costs of access to TB care were computed by ascertaining the number, sequence and cost of visits to formal and informal health care providers by patients prior to their first visit to an NTP provider where they were diagnosed and treated.
The centralised delivery of TB services at the secondary level of care is a result of the how the health care system is organised in Nigeria. The responsibility for different levels of care is distributed among the three tiers of government: national, states and local governments. The state governments are responsible for secondary care, while the national government, in addition to providing tertiary care, also delivers vertical programmes such as the NTP. The responsibility for primary health care is shared by both sub-national (state and local) governments. However, which sub-national government takes primary responsibility for primary health care depends on the decision of each state government. Thus the provision of primary health care services is typically left to local government councils, where the technical capacity and financial resources to deliver primary health care are least available (Okorafor, Citation2010). The design of the NTP is such that patients ought to be diagnosed at secondary health care facilities and to receive treatment at peripheral primary health care facilities. However, weaknesses in the delivery of primary health care (due to lack of funding and human resources for health) make it necessary for a programme delivered by the national government such as the NTP to work through secondary care facilities. Providing services peripherally through primary health care facilities may lead to patients incurring less costs in order to access services (FMOH, Citation2010).
Although there are many studies in which the pathways of care for different conditions in LMICs have been examined, we are not aware of any study that specifically considered the associated transaction costs. This is perhaps because these studies are often of diseases that are self-limiting, present acutely, lead to early death or respond to commonly available remedies (Breiman et al., Citation2011; Burton et al., Citation2011; Grundy & Annear, Citation2010), such that they do not provide the opportunity to explore the details of complex care pathways. TB runs a chronic course and is difficult to treat; patients can present late and only respond to specific forms of therapy that must be sought from appropriate health providers to obtain treatment. Therefore, patients with TB tend to go through an elaborate care pathway, which lends well to transaction costs analysis. Previous studies of TB patients, for example, in rural Nepal (Ten Asbroek, Bijlsma, Malla, Shrestha, & Delnoij, Citation2008) and urban India (Kapoor, Raman, Sachdeva, & Satyanarayana, Citation2012) explored the details of care pathways but did not analyse the transaction costs incurred, whereas those in which pre-diagnosis costs of TB care were analysed, such as in urban Zambia (Needham, Godfrey-Faussett, & Foster, Citation1998) and Nicaragua (Macq, Solis, Ibarra, Martiny, & Dujardin, Citation2004), did not present detailed information on corresponding care pathways and so could only provide aggregate costs rather than at each step of the pathway. The aim of this paper is to use the concept of transaction costs to examine the costs associated with the care-seeking pathways of TB patients and their implications for access to health care and health system governance in Nigeria.
Methods
Data
The data used were obtained from a survey of 452 pulmonary TB patients sampled from three rural secondary care facilities in Ebonyi State, Nigeria (Ukwaja et al., Citation2013). A cross-sectional study of new pulmonary TB patients was conducted between January and September 2011 to assess the costs of TB to patients and their households from the onset of the TB illness, to diagnosis, to the end of the intensive phase of treatment. Only adult TB patients diagnosed based on sputum smear results with or without a chest X-ray and who were between the 5th and 11th weekly drug collection visits were included. Previously treated and extra-pulmonary TB patients and those with other co-morbidities except human immunodeficiency virus (HIV) were excluded as they may have markedly different care-seeking pathways from those with newly diagnosed pulmonary TB. The patients received treatment through community directly observed therapy short-course strategy.
Study setting
Ebonyi, one of Nigeria's 36 states, is located in southeast Nigeria with 73.6% of its population of 2.5 million living below the poverty line (National Bureau of Statistics, Citation2012) and 75% of its inhabitants living in rural areas (National Population Commission, Citation2009). The study was conducted in three rural hospitals (one public and two non-profit), one from each of the three senatorial districts of the state: Ebonyi North (non-profit hospital), Ebonyi Central (public hospital) and Ebonyi South (non-profit hospital) districts. Each study hospital is a centre for TB services, as part of the NTP, and together, they accounted for 70% of TB case notification in Ebonyi in 2009 (Ukwaja, Alobu, Ifebunandu, Osakwe, & Igwenyi, Citation2011). In 2011, the TB case detection rate in Nigeria was 40% (WHO, Citation2011). Non-profit providers are prominent in Ebonyi State because functioning public sector primary and secondary care facilities are often not available, partly because of resource challenges and because the public sector is unable to recruit and retain health workers in rural settings (Ukwaja et al., Citation2013). In Nigeria, households provide 74% of their total health expenditures and more than 95% of these occur through out-of-pocket payments (Soyibo, Olaniyan, & Lawanson, Citation2009). There is no risk-pooling mechanism in the financing of health care, as the National Health Insurance Scheme in Nigeria currently covers mainly federal government workers and their households, approximately 4% of the population (Onoka, Onwujekwe, Uzochukwu, & Ezumah, Citation2013). Although a national policy exempts patients with (or suspected to have) TB from paying for consultations, laboratory tests, TB drugs and admission, patients still incur part of these costs at the public hospital (consultation fees and meal charges if hospitalised) and the non-profit hospitals (consultation fees and admission and meal charges if hospitalised) where the study was conducted.
Data collection
A standardised questionnaire to estimate patient costs developed by the WHO's Stop-TB partnership was used for the survey (Mauch et al., Citation2011). The questions included a detailed list of expenses that might be incurred by TB patients during their pathway to care, i.e., from illness onset to a visit to any health provider(s), to diagnosis, to treatment. There were other questions that quantified the incomes of the patients and their households before the onset of TB symptoms, and the annual income of each patient's household was estimated from their mean monthly income (Mauch et al., Citation2011). The data were collected by two health workers. All of the patients were interviewed in their preferred language during their drug collection visit to the study hospitals, and each interview lasted an average of 30 minutes. Quality control was carried out by the respective district TB control officers charged with guiding and inspecting every step of the survey and was also carried out weekly by one of the investigators (KNU).
Variables
The variables included age, gender, residence, HIV status, smear status and walking distance to the nearest public facility. The questionnaire also included a closed-ended question about why people did not use formal public sector health services. The questionnaire also included questions about the types of initial health care provider visited after the onset of TB-related symptoms. This was classified as ‘NTP provider’ or ‘non-NTP provider’. Non-NTP providers were defined as health providers who were not part of the NTP, including qualified providers (QPs) such as public, for profit and non-profit health care providers; pharmacy providers (PPs) such as chemists and drug shops; and traditional providers (TPs) such as traditional healers and herbalists. In our study setting, PPs only provided drugs and advice typically in a shop and are not licenced to provide clinical care or perform diagnostic tests. QPs were public, for profit or non-profit primary health care providers licenced to generate revenue from consultations, admissions, diagnostic tests and drug sales.
Measuring transaction costs
To measure transaction costs of access to health care, we adopted a definition of transaction costs from the perspective of a consumer as costs incurred in the purchase of goods or services that are not transferred to the seller (Wallis & North, Citation1986). This is the difference between what the consumer spends and what the seller receives, or as described by Niehans (Citation1987), the ‘margins between the buying and selling price’ (p. 676). In this study, we estimated transaction costs of access to health care as the difference between total direct costs incurred by a patient in seeking care for symptoms of TB (i.e., what the customer – patient – spends) and the direct costs incurred in obtaining care from the appropriate provider of TB care (i.e., what the seller – NTP provider – receives). In effect, transaction costs of access to health care were computed as direct patient costs incurred while seeking care from non-NTP providers before their first contact with an NTP provider. The direct costs were the out-of-pocket payments for health services incurred in the pathway of care to access a TB service. These include user fees and the costs of obtaining a registration card, consultation, diagnostic tests, admission, travel, food and non-TB medication. These costs and data on income were captured in Nigerian Naira (N) and converted to the 2011 US$ rate (US$1 = N150).
Data analysis
The data were double entered, checked and analysed using Epi Info™ 3.4.1 (Dean et al., Citation2007). The normality of direct cost data distribution was assessed using a visual inspection of graphs. These were found to be normally distributed. The demographic profile of the patients was tabulated using simple descriptive statistics. The pathway of patients seeking health services from various providers until they reached an NTP provider was constructed using a flow diagram. The costs of navigating that pathway (transaction costs of access to health care) were also summarised as the means (± standard deviation). Group means were compared using the analysis of variance. Multiple linear regression models were constructed with the number of pre-NTP visits and transaction costs as outcome variables. In addition, multivariable logistic regression analysis was performed with choice of provider for first visit (NTP vs. non-NTP provider) as the outcome variable. All variables of clinical importance and those with bivariate P < 0.25 were selected as the explanatory variables. All P values were bidirectional, and a P value of less than 0.05 was set as statistically significant.
Ethical issues
Written informed consent was sought and obtained from all study participants. There was a request to keep the costs of care obtained at NTP facilities confidential; therefore, we did not disaggregate and analyse diagnosis and treatment costs according to the NTP clinic where patients obtained care. The research protocol was approved by the Ebonyi State University Teaching Hospital Health Research and Ethics Committee.
Results
There were in total 452 patients enrolled, with a median age of 30 years, most of whom were males (55%), rural residents (79%), HIV negative (71%) and had smear-positive TB (80%; ). The median monthly household income of the patients was US$133.3 (mean US$167.6) with an interquartile range of US$100–US$200. There were 55.3% of the patients residing in Ebonyi North, 26.5% in Ebonyi Central and 18.1% in Ebonyi South. The patients obtained TB care in their respective senatorial districts such that 73.5% of patients obtained TB care from a non-profit NTP provider and 26.5% obtained TB care from a public NTP provider. The reason patients gave as most important for their first preference for health care provider not being a qualified public sector provider were: long waiting time at health facility during visits (26.3%), distance from home to facility (23.0%), high cost (19.9%), belief system with a preference for alternative medicine (17.9%), mistrust of the public sector health service provision (11.5%) and lack of health facility (1.3%).
Table 1. Demographic characteristics, number of pre-NTP visits and transaction costs of access to TB care in Ebonyi State, Nigeria, 2011.
The total direct costs of TB care per patient in the population were US$110.80, of which US$26.10 were transaction costs and US$84.70 were diagnosis and treatment costs, i.e., 24% of direct costs of TB care were due to transaction costs. There were a total of 596 consultations prior to visiting an NTP provider, out of which 57% were with PPs, 33% with qualified non-NTP providers and 10% with TPs.
Approximately 16% of the patients (72 of the 452) reported consulting an NTP provider first, whereas 84% consulted a non-NTP provider first, 36 (8%) a TP, 284 (63%) a PP and 60 (13%) a QP (). Transaction costs per patient (including costs incurred at subsequent pre-NTP visits) were highest for those whose first pre-NTP visit was to a QP (US$79.80 over an average of 2.2 visits), compared with those who first contacted a PP (US$22.10 over an average of 1.4 visits) or a TP (US$20.20 over an average of 1.7 visits; ). Likewise, the average transaction cost incurred per pre-NTP visit was highest for QPs (US$30.20), double that of PPs (US$14.40) and TPs (US$15.70). In all, approximately 52% of patients sought medical care from one provider before an NTP provider, 17% sought care from two providers, 13% from three and 1% from four providers before an NTP provider (). The amount of transaction costs incurred increased with the number of providers visited before an NTP provider, such that those who saw one incurred an average of US$16, two incurred US$26.70, three incurred US$85.40 and four incurred US$134 per patient (P < 0.001).
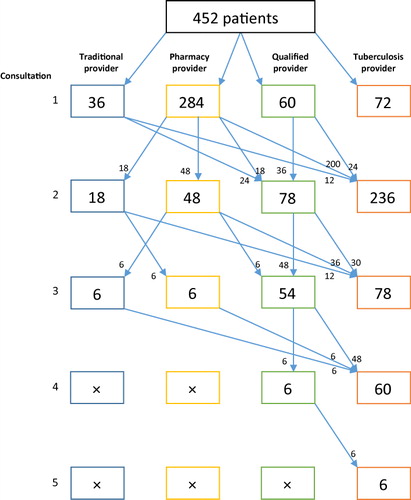
In the study population, 51% of total transaction costs of access to TB care (US$11,799) were incurred at QPs, whereas the other half was incurred at informal providers, 41% at PPs and 8% at TPs. Most (62%) of the transaction costs were incurred at the first pre-NTP visit, such that if all patients were referred to an NTP provider after the first contact with a non-NTP provider, only 38% of the transaction costs would be saved. displays the 14 different trajectories that patients in the sample followed to access appropriate TB care and the associated costs.
Table 2. The trajectories patients followed to reach tuberculosis service and associated transaction costs and costs of diagnosis and treatment in Ebonyi State, Nigeria, 2011.
The percentage of patients transferred to an NTP provider after a first consultation with a non-NTP provider was highest for those whose first consultation was with a PP (70%) compared with a TP (33%) and a QP (40%). The rate of transfer increased in those whose second consultation was with either a PP (75%) or a TP (67%) but remained approximately 40% when the second consultation was with a QP. In addition, only patients whose first visit was to a QP had up to four visits prior to seeing an NTP provider, and none of those who first consulted a QP went back to consult an informal (traditional or pharmacy) provider. None of those whose first visit was to a TP returned to a TP for a subsequent consultation. Among the 14 paths patients followed on their way to TB care, those with trajectories involving QPs incurred higher transaction costs per patient compared with others (see and ).
In multiple linear regression analysis, the independent predictors of higher number of pre-NTP visits (Model 1; ) were longer walking distance to the nearest public facility (P < 0.014); older age (P < 0.001); female gender (P < 0.001); HIV-positive status (P < 0.001); and first visit to a TP (P < 0.001) or a QP (P < 0.001), but not to a PP (P = 0.081). In addition, the independent predictors of higher transaction costs of access to TB care (Model 2; ) were a higher number of pre-NTP visits (P < 0.001); longer walking distance to the nearest public facility (P < 0.001); urban residence (P < 0.001); female gender (P = 0.003); HIV-negative status (P < 0.001); residence in districts with a non-profit NTP provider (i.e., Ebonyi North and South; P = 0.018); and first visit to a TP (P < 0.001), a PP (P < 0.001) and a QP (P < 0.001; ). Inspection of the graphs of the residuals suggests that the data for number of pre-NTP visits and for transaction costs met the assumptions for multiple linear regression analysis, and the correlation coefficients (R2) were 0.50 and 0.83, respectively, which indicate that the regression models are a good fit (Woodward, Citation2005).
Table 3. Multivariable linear regression analysis of factors associated with high number of pre-NTP visits and high transaction costs of access to TB care in Ebonyi State, Nigeria, 2011.
In the multivariable logistic regression analysis to determine the independent predictors of choice between an NTP and a non-NTP provider as provider choice of first visit (), higher household income (adjusted odds ratio [aOR] 1.01; 95% confidence interval [CI] 1.01–1.02); older age (aOR 1.05; 95% CI 1.02–1.07); and female gender (aOR 2.6; 95% CI 1.6–5.2) were associated with visiting an NTP provider first for consultation; while HIV-positive status (aOR 3.6; 95% CI 1.1–11.7) and smear-negative TB status (aOR 0.1; 95% CI 0.04–0.3) were associated with visiting a non-NTP provider first for consultation.
Table 4. Multivariable logistic regression analysis of factors associated with choice of NTP provider at first visit among TB patients, Ebonyi State, Nigeria, 2011.
Discussion
This study demonstrates that transaction costs are a potential financial barrier of access to the diagnosis and treatment of TB in Nigeria in settings where the TB case detection rate was only 40% (WHO, Citation2011). This is important because this study was conducted among the rural poor in one of the poor states in Nigeria, where three out of every four people live below the poverty line and for whom every additional cost is an important potential barrier to accessing services. This study illustrates that transaction costs account for up to 24% of the total direct costs of TB care and, at an average of US$26.10, are approximately 20% of the median monthly household income (US$133.30) in this population of TB patients among whom a higher number of pre-NTP visits is associated with incurring higher transaction costs. However, while patients from higher income households tend to visit an NTP provider for their first consultation (higher income households may have more information about the NTP), household income is neither associated with the number of pre-NTP visits nor with the extent of transaction costs. Perhaps reflecting complexities in the effect of gender on access to household resources, being female is associated with fewer pre-NTP visits and the choice of an NTP provider for first consultation, but also with incurring higher transaction costs. Living at a longer distance from a qualified public provider is associated with higher number of pre-NTP visits and higher transaction costs, but not with the choice between NTP and non-NTP provider for first consultation. In addition, patients with smear-negative TB and those who are HIV positive tend to visit a non-NTP provider for their first consultation, possibly because their symptoms tend to be less suggestive of TB.
As in many other studies of health care-seeking behaviour conducted in LMICs (Sudhinaraset, Ingram, Lofthouse, & Montagu, Citation2013), the majority (62.8%) of patients first went to a PP to obtain care at lower costs, an average of US$14.40 compared with US$15.70 from TPs and US$30.20 from QPs. In Nigeria, as in other LMICs, PPs are often the first line of care and are therefore the de facto providers of primary health care. In many communities, they tend to be more trusted, have been around much longer, are more readily available, less costly and have closer relations with the community than QPs (Abimbola, Citation2011; Brieger, Osamor, Salami, Oladepo, & Otusanya, Citation2004). These PPs are mostly patent medicine vendors with drug shops operating outside regulatory provisions that allow them to sell only common drugs such as pain-relieving medicine and cough syrups in pre-packaged forms and not, for example, antibiotics (Brieger et al., Citation2004). For the rural poor, seeking care from informal health providers is often a strategy devised to cut costs, but by which they may end up incurring higher costs due to opportunism in the poorly regulated rural health market (Bloom et al., Citation2011). Financial access to care and the general quality of health services are therefore important determinants of transaction costs. More than 50% of all transaction costs were incurred during visits to QPs, although these visits accounted for only 33% of all pre-NTP visits. This is perhaps because unlike pharmacy and TPs, patients often have to pay consultation fees to see a QP, in addition to the cost of drugs, admission, and the laboratory, radiological and other diagnostic tests peculiar to QPs.
The findings of this study show – as identified by Williamson (Citation1979) – that non-modifiable characteristics of transactions such as the peculiarities of TB diagnosis contribute to the extent of transaction costs, alongside the modifiable institutional determinants of transaction costs. The findings are also in keeping with the results of previous studies in LMICs in which the care pathways of TB patients were examined. A study in urban Zambia (Needham et al., Citation1998) demonstrated that pre-diagnosis costs could create barriers to prompt diagnosis, potentially leading to continuing transmission of the infection. A study in urban India (Kapoor et al., Citation2012) revealed that informal providers were the first point of contact and the source of clinical advice for two-thirds of patients, similar to the 71% whose first point of contact was an informal provider in rural Nigeria, and the rest sought health care from QPs directly, whether or not they provided TB services. Studies in urban India and in Nicaragua (Macq et al., Citation2004) also found that most patients sought care from more than two providers before being diagnosed with TB. In rural Nepal (Ten Asbroek et al., Citation2008), a qualitative study of patient pathways found 26 different patient pathways (compared with 14 in rural Nigeria), which, as in rural Nigeria, often started with a PP and proceeded through intricate routes until they reached facilities where TB was diagnosed and treated.
The study provides possible guidance to policy-makers regarding the use of various types of health services in Nigeria. Though 18% of respondents preferred TPs to QPs, only 8% of patients had their first consultation with a TP. In addition, none of those who had their first contact with a TP subsequently returned to a TP, suggesting that community members recognise some limitations of TPs. Furthermore, patients who had their first consultation with a QP had the highest number of subsequent consultations, all with QPs, before attaining appropriate care. This suggests that QPs may be serving a filtering function, performing diagnostic tests to separate patients who have TB from those who may not, with the possibility that significant financial interests may be involved in this source of transaction costs. However, more than 70% of those whose first visit was to a PP had an immediate subsequent visit to an appropriate NTP provider, suggesting a relatively strong referral link. Given that the majority of transaction costs were incurred at the first visit to a health provider, governance interventions to reduce transaction costs of access to TB care in this population would aim to prevent this first visit to a non-NTP provider, reduce the cost of the ineffective care obtained from non-NTP providers or provide non-NTP providers with information and incentives to refer TB patients immediately to NTP providers at no cost to the patient. While it may be unrealistic to expect that patients would directly go to a centralised NTP provider, this study shows that anything short of going directly to an NTP provider implies high transaction costs. This suggests a need to strengthen primary health care services such that TB services will be effectively decentralised to the primary health care level.
Interventions may be at three levels of governance: constitutional (governments), collective (the communities) and operational (health system actors in the local health market; Abimbola et al., Citation2014). At the operational level, NTP providers in communities in Ebonyi may give incentives to non-NTP providers to ensure early and immediate referral when patients present with symptoms suggestive of TB (Oladepo & Lucas, Citation2013). At the collective level, communities in Ebonyi may be supported to monitor and enforce appropriate health service provision to ensure quality, promote cost-reducing referral practices, disseminate information about available health services and prevent opportunistic behaviour among providers (Bloom et al., Citation2011; Oladepo & Lucas, Citation2013). At the constitutional level, the national government may co-locate the NTP with more QPs in order to reduce the high transaction costs incurred at QPs, or reorganise health services so that responsibility for primary health care is with a more capable tier of government such as the national government itself or Ebonyi State Government or strengthen the capacity of local governments in Ebonyi to deliver primary health care services. This will ensure the provision of primary health care in rural Ebonyi such that a programme like the NTP will be able to operate within health facilities that are closer to the people. Governments may also establish financing mechanisms that reduce the cost of care in order improve financial access to care and allow patients to seek appropriate care early. The Government of Ebonyi State may enforce regulations that limit the activities of informal providers such that PPs, for example, are only able to dispense over-the-counter drugs (Bloom et al., Citation2011). Interventions to reduce transaction costs may also include those without specific application to the health system, for example, government initiatives to build better rural road networks, ensure that the population is literate and educated, fund low-cost transportation and communication and support legal protection of contracts for the rural poor (Altmann, Citation2011).
There may be recall bias in our study given that the information on care pathways was collected retrospectively. The study would have benefited from a qualitative component in which information could be obtained on why people made their choices about the first and successive places where they sought health care. Such data should be included in future studies exploring transaction costs of health care in LMICs. In addition, because we only obtained information from patients who found their way to TB treatment, we have no direct information on how transaction costs constituted barriers to those who could not attain appropriate TB care. Further, because of the retrospective study design, we were not able to obtain data on successive time delays and associated indirect costs at each stage of the care-seeking pathway. While our focus in this study is direct costs, future studies should include indirect costs as they too can constitute a major barrier of access to health care and because data on them can further deepen the understanding of barriers of access to health care. We also do not know the extent to which the patient trajectories in our sample are representative of those who did not attain appropriate care due to transaction costs. However, the patients in our study were representative of Ebonyi State and Nigeria with respect to rural residence and the prevalence of HIV–TB co-infection, reducing concerns that the enrolled sample was systematically different than the population as a whole. It was observed that 79% of our sample reside in rural areas, compared with 75% in the entire Ebonyi State, and that 29% of our sample, compared with 25% of TB patients in Nigeria, are co-infected with HIV (WHO, Citation2011).
The success of governance interventions to reduce the transaction costs of access to health care depends on the costs of implementing them relative to the transaction costs incurred in the absence of such interventions. The motivation of health system actors to intervene depends on whether they foresee such net benefits from an intervention (Varughese & Ostrom, Citation2001). It is therefore important for health system actors at the operational, collective and constitutional levels of governance to realise the transaction costs of access to health care being incurred by patients due to the absence of governance interventions. Further research should explore the costs of alternative interventions to inform the choice of strategies for reducing transaction costs of access to health care. The transaction costs of access to health care can also be an outcome measure in comparative studies of health system governance. Future theory-based evaluations of health system governance in LMICs should explore how and under what circumstances health system actors are able to minimise transaction costs of access to health care. For example, how would transaction costs vary with availability of information on the appropriate health providers in a community? Would people consult a health care provider that incorporates different services (vertical integration) instead of repeatedly initiating and negotiating different patient–provider relationships along the referral pathway? How would care-seeking behaviour differ if expenses were not being paid out of pocket, or if informal providers were effectively regulated? Would patients prefer to consult formal (rather than informal) providers if formal legal redress was as accessible as informal arbitration in case of malpractice? We consider this study an initial step in the process of exploring health system governance in LMICs along these dimensions informed by the concept of transaction costs.
Conclusion
In summary, this study highlights the costs incurred by patients before reaching an appropriate health provider where they were diagnosed and treated for TB, as established by the NTP. Although the NTP is based on a treatment model that has been proven to be efficacious internationally, its success in Nigeria is tempered by the high transaction costs that patients face when accessing care due to weaknesses in the delivery of primary health care in Nigeria. The study also provides a template for analysing the transaction costs of gaining access to the care of other chronic diseases in which patients potentially experience similarly intricate and costly care-seeking pathways. The concept of transaction costs can be used to examine the comparative costs of different models of health services organisation. High transaction costs can be attributed to a failure of governance and can explain why otherwise effective interventions are not successfully implemented, particularly in LMICs. The concept of transaction costs presents unique insights into the study of health system governance in LMICs, as it draws attention to otherwise ignored implications of weak health system governance, to alternative modes of governing relations within the health care market and to strategies for reducing transaction costs for patients.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
Notes
1. Transactions occur when a good or service is transferred across a technologically separable interface (for example, among health care providers, within health care organisations and between patient and health care provider), and transaction costs are costs associated with search, negotiation and enforcement of contracts in order to facilitate a transaction (Williamson, Citation1979). In health systems, transaction costs may be incurred by health care providers and organisations (in providing health care) or by patients (in accessing health care); this paper focuses on the latter. See Tyagi (Citation2004) and Kim and Li (Citation2009) for similar applications of the concept of transaction costs to consumer–producer transactions (similar to patient–provider transactions in health care markets). For previous applications to transactions among or between health care providers, see Ashton (Citation1998) and Zinn et al. (Citation2003), and within or by health care organisations, see Stiles et al. (Citation2001) and Jan et al. (Citation2008).
References
- Abimbola, S. (2011). Health systems in an interconnected world: A view from Nigeria. MEDICC Review, 13(3), 43–45. doi:10.1590/S1555-79602011000300010
- Abimbola, S., Negin, J., Jan, S., & Martiniuk, A. (2014). Towards people-centred health systems: A multi-level framework for analysing primary health care governance in low- and middle-income countries. Health Policy and Planning, 29(Suppl. 2), ii29–ii39. doi:10.1093/heapol/czu069
- Altmann, M. P. (2011). Contextual development economics: A holistic approach to the understanding of economic activity in low-income countries. New York, NY: Springer.
- Ashton, T. (1998). Contracting for health services in New Zealand: A transaction cost analysis. Social Science & Medicine, 46, 357–367. doi:10.1016/S0277-9536(97)00164-0
- Bloom, G., Standing, H., & Lloyd, R. (2008). Markets, information asymmetry and health care: Towards new social contracts. Social Science & Medicine, 66, 2076–2087. doi:10.1016/j.socscimed.2008.01.034
- Bloom, G., Standing, H., Lucas, H., Bhuiya, A., Oladepo, O., & Peters, D. H. (2011). Making health markets work better for poor people: The case of informal providers. Health Policy and Planning, 26(Suppl. 1), i45–i52. doi:10.1093/heapol/czr025
- Breiman, R. F., Olack, B., Shultz, A., Roder, S., Kimani, K., Feikin, D. R., & Burke, H. (2011). Healthcare-use for major infectious disease syndromes in an informal settlement in Nairobi, Kenya. Journal of Health, Population and Nutrition, 29, 123–133. doi:10.3329/jhpn.v29i2.7854
- Brieger, W. R., Osamor, P. E., Salami, K. K., Oladepo, O., & Otusanya, S. A. (2004). Interactions between patent medicine vendors and customers in urban and rural Nigeria. Health Policy and Planning, 19, 177–182. doi:10.1093/heapol/czh021
- Buckley, P. J., & Chapman, M. K. (1997). The perception and measurement of transaction costs. Cambridge Journal of Economics, 21, 127–145. doi:10.1093/oxfordjournals.cje.a013663
- Burton, D. C., Flannery, B., Onyango, B., Larson, C., Alaii, J., Zhang, X., … Feikin, D. R. (2011). Healthcare-seeking behaviour for common infectious disease-related illnesses in rural Kenya: A community-based house-to-house survey. Journal of Health, Population and Nutrition, 29, 61–70. doi:10.3329/jhpn.v29i1.7567
- Coase, R. H. (1960). The problem of social costs. Journal of Law and Economics, 3, 1–44. doi:10.2307/724810
- Dean, A. G., Arner, T. G., Sunki, G. G., Friedman, R., Lantinga, M., Sangam, S., … Fuller, G. (2007). Epi Info™ (3.4.1). A database and statistics program for public health professionals. Atlanta, GA: Centers for Disease Control and Prevention (CDC).
- Federal Ministry of Health (FMOH). (2010). National tuberculosis and leprosy control programme: Workers manual. 5th ed. Abuja: Author.
- Grundy, J., & Annear, P. (2010). Health-seeking behaviour studies: A literature review of study design and methods with a focus on Cambodia (Working Paper Series Number 7). Retrieved from http://ni.unimelb.edu.au/hphf-hub/publications/working-papers/7
- Jan, S., Pronyk, P., & Kim, J. (2008). Accounting for institutional change in health economic evaluation: A program to tackle HIV/AIDS and gender violence in Southern Africa. Social Science & Medicine, 66, 922–932. doi:10.1016/j.socscimed.2007.11.010
- Kapoor, S. K., Raman, A. V., Sachdeva, K. S., & Satyanarayana, S. (2012). How did the TB patients reach DOTS services in Delhi? A study of patient treatment seeking behavior. PLoS ONE, 7, e42458. doi:10.1371/journal.pone.0042458
- Kim, Y. G., & Li, G. (2009). Customer satisfaction with and loyalty towards online travel products: A transaction cost economics perspective. Tourism Economics, 15, 825–846. doi:10.5367/000000009789955125
- Leonard, D. K., Bloom, G., Hanson, K., O'Farrell, J., & Spicer, N. (2013). Institutional solutions to the asymmetric information problem in health and development services for the poor. World Development, 48, 71–87. doi:10.1016/j.worlddev.2013.04.003
- Macq, J., Solis, A., Ibarra, M., Martiny, P., & Dujardin, B. (2004). The cost of medical care and people's health-seeking behaviour before being suspected of tuberculosis in three local health systems, Nicaragua. International Journal of Tuberculosis and Lung Disease, 8, 1330–1336.
- Mauch, V., Woods, N., Kirubi, B., Kipruto, H., Sitienei, J., & Klinkenberg, E. (2011). Assessing access barriers to tuberculosis care with the ‘tool to estimate patients’ costs’: Pilot results from two districts in Kenya. BMC Public Health, 11, 43. doi:10.1186/1471-2458-11-43
- National Bureau of Statistics. (2012). The Nigeria poverty profile: 2010 report. Abuja: Author. Retrieved from http://resourcedat.com/resources/The-Nigerian-Poverty-Profile1.pdf
- National Population Commission. (2009). The 2006 population and housing census of the Federal Republic of Nigeria. Priority tables (volume I). Abuja: Author. Retrieved from http://www.ibenaija.org/uploads/1/0/1/2/10128027/priority_tables_volume_i-update.pdf
- Needham, D. M., Godfrey-Faussett, P., & Foster, S. D. (1998). Barriers to tuberculosis control in urban Zambia: The economic impact and burden on patients prior to diagnosis. International Journal of Tuberculosis and Lung Disease, 2, 811–817.
- Niehans, J. (1987). Transaction costs. In J. Eatwell, M. Milgate, & P. Newman (Eds.), The New Palgrave Dictionary of Economics (vol. 4, p. 676). London: Macmillan.
- Okorafor, O. A. (2010). Primary healthcare spending: Striving for equity under fiscal federalism. Cape Town: UCT Press.
- Oladepo, O., & Lucas, H. (2013). Improving the performance of patent medicine vendors in Nigeria. In G. Bloom, B. Kanjilal, H. Lucas, & D. H. Peters (Eds.), Transforming health markets in Asia and Africa: Improving quality and access for the poor (pp. 103–114). London and New York, NY: Routledge.
- Onoka, C. A., Onwujekwe, O. E., Uzochukwu, B. S., & Ezumah, N. N. (2013). Promoting universal financial protection: Constraints and enabling factors in scaling-up coverage with social health insurance in Nigeria. Health Research Policy and Systems, 11, 20. doi:10.1186/1478-4505-11-20
- Soyibo, A., Olaniyan, O., & Lawanson, A. O. (2009). National health accounts of Nigeria, 2003–2005. Incorporating sub-national health accounts of states. Volume 1: Main report. Abuja: Federal Ministry of Health. Retrieved from http://www.who.int/nha/country/nga/nigeria_nha_2003-2005_report.pdf
- Stiles, R. A., Mick, S. S., & Wise, C. G. (2001). The logic of transaction cost economics in health care organization theory. Health Care Management Review, 26(2), 85–92. doi:10.1097/00004010-200104000-00010
- Sudhinaraset, M., Ingram, M., Lofthouse, H. K., & Montagu, D. (2013). What is the role of informal healthcare providers in developing countries? A systematic review. PLoS ONE, 8, e54978. doi:10.1371/journal.pone.0054978
- Ten Asbroek, A. H., Bijlsma, M. W., Malla, P., Shrestha, B., & Delnoij, D. M. (2008). The road to tuberculosis treatment in rural Nepal: A qualitative assessment of 26 journeys. BMC Health Services Research, 8, 7. doi:10.1186/1472-6963-8-7
- Tyagi, R. K. (2004). Technological advances, transaction costs, and consumer welfare. Marketing Science, 23, 335–344. doi:10.1287/mksc.1030.0038
- Ukwaja, K., Alobu, I., Ifebunandu, N., Osakwe, C., & Igwenyi, C. (2011). From DOTS to the stop TB strategy: DOTS coverage and trend of tuberculosis notification in Ebonyi, Southeastern Nigeria, 1998–2009. Pan African Medical Journal, 9, 12. doi:10.4314/pamj.v9i1.71187
- Ukwaja, K. N., Alobu, I., Igwenyi, C., & Hopewell, P. C. (2013). The high cost of free tuberculosis services: Patient and household costs associated with tuberculosis care in Ebonyi State, Nigeria. PLoS ONE, 8, e73134. doi:10.1371/journal.pone.0073134
- Varughese, G., & Ostrom, E. (2001). The contested role of heterogeneity in collective action: Some evidence from community forestry in Nepal. World Development, 29, 747–765. doi:10.1016/s0305-750x(01)00012-2
- Wallis, J. J., & North, D. C. (1986). Measuring the transaction sector in the American economy 1870–1970. In S. L. Engerman & R. E. Gallman (Eds.), Long-term factors in American economic growth (pp. 95–161). Chicago, IL: University of Chicago Press.
- Wang, N. (2007). Measuring transaction costs: Diverging approaches, contending practices. Division of Labor & Transaction Costs, 2, 111–146. doi:10.1142/S0219871107000324
- Williamson, O. E. (1979). Transaction cost economics: The governance of contractual relations. Journal of Law and Economics, 22, 233–261. doi:10.2307/725118
- Woodward, M. (2005). Epidemiology: Study design and data analysis. 2nd ed. Boca Raton, FL: Chapman & Hall/CRC Press.
- World Health Organization (WHO). (2010). Health systems financing: The path to universal coverage. 2010 world health report. Geneva: Author. Retrieved from http://whqlibdoc.who.int/whr/2010/9789241564021_eng.pdf
- WHO. (2011). Global tuberculosis control: WHO report 2011. Geneva: Author. Retrieved from http://whqlibdoc.who.int/publications/2011/9789241564380_eng.pdf
- Zinn, J. S., Mor, V., Intrator, O., Feng, Z., Angelelli, J., & Davis, J. A. (2003). The impact of the prospective payment system for skilled nursing facilities on therapy service provision: A transaction cost approach. Health Services Research, 38, 1467–1485. doi:10.1111/j.1475-6773.2003.00188.x
