ABSTRACT
Chronic conditions are an increasing problem in Low- and Middle-Income Countries (LMICs) yet, the challenges faced by low-income populations with these conditions in such countries are not well understood. Based on in-depth interviews with people affected by chronic conditions and their family members, this paper describes the experience of patients suffering from diabetes or hypertension in rural communities of Mozambique, Nepal, and Peru. We analysed our data using the concepts of disruption and adaptive strategies, finding that despite being very different countries, the implications in daily lives, interpersonal relationships, and family dynamics are similar, and that oftentimes such impact is defined along gender lines. We show that adjustments to living with a chronic disease are not always easy, particularly when they imply changes and reconfiguration of roles and responsibilities for which neither the individual nor their families are prepared. The study adds to the literature on the disruptive effects of chronic conditions and stresses the importance of contextualising disruptive experiences among disadvantaged populations within weak health systems. Our findings highlight the relevance of understanding the challenges of developing adaptive solutions to chronic care in resource-scarce contexts.
Introduction
Chronic conditions are health problems that persist over time and require ongoing management with no cure or resolution (Bentzen, Citation2003; WHO, Citation2002). They cover a wide range of health issues including non-communicable diseases, HIV/AIDS, and mental disorders, as well as disabilities and impairments (Nolte & McKee, Citation2008; WHO, Citation2002). Furthermore, they require follow-up treatment and rehabilitation (Barros, Cesar, Carandina, & Torre, Citation2006) and are characterised by periods of improvement and acute episodes of worsening health demanding a complex response over an extended time period (Barros et al., Citation2006). Strong health systems and social support are key elements for managing chronic conditions, but when thinking about tailored responses at the Primary Health Care (PHC) level it is also necessary to understand the individual and social implications for those affected by chronic diseases.
Chronic conditions have been studied from sociological perspectives since the 1970s. The concept of disruption was developed in the 1980s to understand the experience of living with a chronic condition (Bury, Citation1982). This extensively used concept has enabled a more nuanced understanding of the challenges of having a chronic debilitating illness, coping processes, management strategies, and adjustment processes (Williams, Citation2000). When a chronic illness is diagnosed or when symptoms appear, people’s concept of self and their biography changes causing ‘biographical disruption’ (Bury, Citation1982). Biographical disruption is the cognitive process people undergo when their expectations about the course of their lives change suddenly (Becker, Citation1994); it brings a feeling of having lost control over parts of one’s life (Mattingly & Garro, Citation2000). Disruption also occurs in people’s everyday actions (Becker, Citation1994): everyday routines and activities are altered, and strategies have to be developed to reconcile the requirements of chronic management with leading a full or ‘normal’ life (Burridge et al., Citation2016; Bury, Citation1982; Campbell et al., Citation2003; Charmaz, Citation1994; Robinson, Citation1993). Adaptive behaviours enable patients to cope with the pain or distress of living with a chronic illness and to the need to adjust to the long-lasting course of their condition (Büssing, Ostermann, Neugebauer, & Heusser, Citation2010).
Bury (Citation1982) explains that chronic conditions also disrupt the capacity to ‘mobilize resources’ since chronically ill individuals can no longer participate in relationships that are emotionally important, but also resolve material and practical affairs. In many instances, chronically ill people are no longer able to reciprocate for the help they receive (Bury, Citation1982). It is important to be careful not to generalise findings across all chronic conditions since there are clinical and contextual specificities which frame the experiences.
One limitation of the literature on disruption and chronicity is the lack of attention to structural aspects that frame the experience of chronicity, as most studies have focused on individual’s personal experiences (Bury, Citation1991). Furthermore, it is important to assess the relevance of the concept of disruption outside of Western contexts (Williams, Citation2000). Studies on disruption in High Income Countries (HIC) have set the theoretical foundations of the discussion (Becker, Citation1994; Burridge et al., Citation2016; Bury, Citation1982; Campbell et al., Citation2003; Charmaz, Citation1994; Robinson, Citation1993) while studies from LMIC settings (Eshun-Wilson, Rohwer, Hendricks, Oliver, & Garner, Citation2019; Hondras, Hartvigsen, Myburgh, & Johannessen, Citation2016; Mairami, Warren, Allotey, Mak, & Reidpath, Citation2018; Wouters & Wet, Citation2016) appear to point to the role of socioeconomic status and everyday scarcity in people’s experiences and the relevance of exploring the social and cultural context to better understand its implications and meaning (Pound, Gompertz, & Ebrahim, Citation1998).
In this paper, we describe the impact of chronic conditions and chronic care management in the lives of both individuals and families from three LMICs and discuss the relevance of the literature on disruption in non-Western contexts among disadvantaged groups.
Methods
This study aimed to explore the experience of vulnerable groups living in Mozambique, Nepal, and Peru who access PHC services when affected by a chronic condition. In-depth interviews were carried out in rural and semi-rural communities in the three countries with individuals affected by diabetes or hypertension and their caregivers and/or heads of household. The interview guides covered four topics: (1) Lay understandings of disease, (2) Experiences at PHC facilities (with emphasis on the diagnosis and follow-up of the condition), (3) Impact on self and family, and (4) Caregiving activities and impact of caregiving. In all countries, participants answered a short questionnaire to collect basic socio-demographic information. In this paper, we focus on Topic 3: Impact on self and family. The specific questions and probes asked are shown in .
Table 1. Questions and probes to patients and caregivers/heads of household.
To ensure comparability of the data collected in the three countries, the protocol and instruments were prepared in English with the participation of the three research teams and with the support of senior researchers. The methodological guide and data collection tools were translated and adapted to the particular context of each country and used to train local fieldworkers. During the analysis process, the three research teams used the same codebook and discussed concerns. offers contextual demographic information for each country.
Table 2. General information of Mozambique, Nepal and Peru.
Recruitment strategy
Data collection was undertaken in 2017. In Mozambique, patients and caregivers were recruited at health facilities followed by a snowball sampling. In Nepal, patients were recruited with the support of one local male health worker who invited participants for interviews. In most cases, the recruiters were involved in community activities and known by community members. Caregivers and head of households were contacted through the interviewed patients and were invited to participate at their homes. In Peru, fieldworkers recruited patients in public spaces, asking if anybody knew somebody affected by diabetes or hypertension. After recruiting three participants, a snowball sampling methodology was used with support of local health workers. Caregivers were invited to participate at the patient’s home just before beginning the interview with the patient. In all three countries, interviews with patients and caregivers were conducted separately. There was one case in Mozambique and one case in Peru where both participants were together, however the interviews were done one after the other and thus were not dyadic interviews.
Settings
In Mozambique, one community was located in the rural area of the Maputo province, where the main livelihoods are in the agricultural sector (Instituto Nacional de Estatística, Citation2015). The second community was peri-urban and close to the peripheral belt of the capital and largest city in the country where the main economic activity is in the informal commerce sector. The rural health facility was staffed by two doctors and several health workers, serving a total population of 21,723 people. The peri-urban community had a health facility with three doctors and around 80 other cadres of health workers serving a population of 60,000.
Both communities in Nepal were located in Province No.1 in the Eastern Development Region. One is situated in a fast-growing town in the Sunsari district and the other in a rural area in the Jhapa district where 59% of the land is used for agricultural purposes (Rimal, Citation2013) and 80% of the population works in agriculture, specifically in paddy farming. Each community has a population of 20,000 served by a PHC staffed with one medical officer and eight health workers.
For the Peruvian component of the study, both communities were located in a rural area of the Piura Region at the northern part of the country where 54% of people work in agriculture (INEI, Citation2017). Each community was served by a PHC facility staffed by four and three health workers respectively for a population of approximately 1000 people each.
Research teams in all countries had previous experience in qualitative data collection. In Mozambique, interviews were conducted in Portuguese and Xangane, the predominant local language in the southern region of the country. In Nepal, data collection was mostly conducted in Nepali. In a few cases, women from the communities fluent in other local languages assisted the research team. In Peru, all data were collected in Spanish.
Data analysis
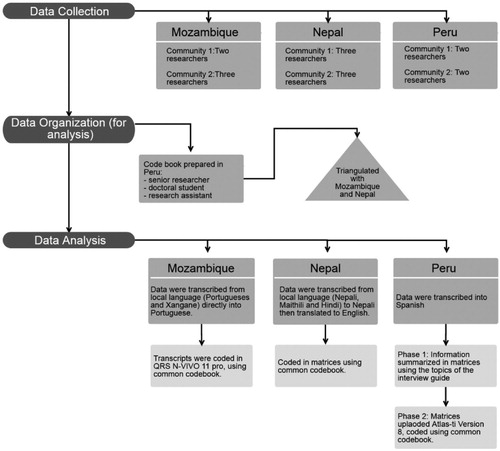
A qualitative content analysis was conducted, which allowed for a subjective interpretation of the data through a systematic classification process of coding and the identification of themes or patterns (Hsieh & Shannon, Citation2005). The analysis began by coding the data using predefined themes, with flexibility to allow emergent themes in the process (Azungah, Citation2018). Data across the three countries were analysed using a common thematic codebook developed from the major themes in the interview guide (). New codes were created after the initial review of the data while others were merged. The final version of the codebook was prepared by a senior researcher, a doctoral student, and a research assistant in Peru, and triangulated with input from the Nepalese and Mozambican teams.
In Mozambique, interviews were transcribed from the local language into Portuguese and coded using QRS N-VIVO 11 pro. In Nepal, interviews were transcribed in Nepali, then translated into English and coded manually in matrices. In Peru, all interviews were transcribed in Spanish and analysed in two phases. In Phase 1, the information from the audio recording was summarised in matrices by fieldworkers, using the topics of the interview guide. Matrices were then reviewed both by the study coordinator and the research assistant. In Phase 2, the matrices were uploaded into Atlas-ti Version 8 and coded using the common codebook.
In this manuscript, we draw from the data from the following two codes: (1) impact of living with a chronic condition at the individual level and (2) impact of living with a chronic condition at the family level. Data were assembled and analysed using a comparative conceptual lens drawn from the literature on disruption. The senior qualitative researcher from Peru reviewed the information (interview excerpts) from the three countries and identified common themes that we present in the results section of this paper.
All participants provided written or verbal consent prior to collecting the data. All interviews were digitally recorded and transcribed. The study was approved by the Cantonal Commission for Research Ethics (IRB No. 2016-01242), and by the IRBs of each local institution.
Results
A total of 63 interviews were conducted (59.5% female), with 16 people with diabetes and 20 with hypertension. Fifteen interviews were done with caregivers and 12 with heads of households as shown in .
Table 3. Participants by type of informant, gender, and country.
The interviews highlight the changes introduced in their everyday activities, their relations with their loved ones and in their sense of self-worth. The latter is usually associated with their capacity to perform their responsibilities within the household and family.
Chronic conditions and physical activity
Diabetes and hypertension are commonly referred to as ‘silent diseases’ because their symptoms are only detectable with clinical testing. Although we did not perform any measurement of blood glucose or blood pressure, all respondents expressed that having diabetes or hypertension meant they were constantly unwell. They expressed feeling weak, tired, lethargic or sleepy. Others said they suffered from headaches or were frequently worried. This association between worry and headaches was more common in the case of Nepal, where stress (‘Tanab’ or ‘Chinita’) was also referred to as ‘pressure in the brain.’
Besides weakness and headaches, participants also mentioned pain in their limbs (‘dolor de huesos’ in Peru or ‘saririk’ and ‘dukhai’ in Nepal) or difficulties in breathing which resulted in reduced physical activity:
I can’t do heavy things, work for a long time with energy, it takes time to iron, cook with energy (…). The diagnosis of tension [hypertension] has changed my life, it harmed me because I can’t do everything I did before (…) I can’t run, I can’t walk long distances under the sun. (Female-hypertension-Mozambique. Age 43)
Not being able to walk, work, or participate in activities that demanded physical strength was a source of frustration for different reasons. Having a chronic condition implied not being able to share the workload with other family members. This was particularly hard when they could not participate in agricultural activities that are essential for survival. Having a chronic condition also meant not being able to fulfil their duties as wives, husbands or other family roles. In Peru, a male-caregiver explained that because of his wife’s diabetes he often had to take care of the household tasks. Another woman affected by hypertension in Peru, lamented her inability to cook or do other domestic chores due to the discomfort resulting from her condition. Some of the interviewees expressed grief for not being able to do what they used to do. They were concerned about the impact of such limitations on others’ workload or in their own responsibilities towards others: ‘It hurts me not to go to the farm because it helped me take care of the children, now I have nothing to give them’ (Female-hypertension-Mozambique. Age 54). Although not explored in depth, the physical health limitations caused by chronic conditions among women meant a disruption in their gendered roles.
For the interviewees who had an income-generating occupation, having a chronic condition meant that their capacity to contribute to the family economy was reduced or that they had to overcome the physical discomfort and continue working:
[Before having the disease] I was helping at home to have something to eat. It was difficult and it is still difficult because the head of the family has not been working for a long time. Now I have to make an effort to help, I make badjias (local food). I feel that my body is not good, but I have no alternative, I also need the money to be able to buy pills. (Female-diabetes-Mozambique. Age 52)
Caregivers’ capacity to assign time to work was also affected since they had to allocate time to care for their relative: ‘We have to give extra time for his care by missing our work’ (Male-Caregiver-diabetes-Nepal. Age 46); ‘I used to work as a tailor but since he has become ill I don’t do that anymore’ (Female-Caregiver-hypertension-Nepal. Age 44). In Peru, family members had to make arrangements for taking their parent to their appointments since most received follow-up care in secondary level facilities located far away from their communities. Having to miss work resulted in reduced availability of resources among already poor families. Chronic conditions affected both individuals’ and caregivers’ capacity to work, either in income-generating activities for those living in peri-urban areas in Mozambique and Nepal or activities necessary for the family’s subsistence in rural communities.
Expenses, time and family dynamics
Chronic conditions also had financial implications as a result of out-of-pocket expenditures on medications for managing their condition. Despite the fact that the three countries have policies in place to provide free medications for diabetes and hypertension, the participants’ account show that these benefits do not reach rural areas, or do not reach them in a reliable way.
In some cases, the financial burden of the disease was directly related with the challenge of allocating money for pills that are expensive and that are not provided for free at local health facilities: ‘The price of pills is very high and this makes it difficult because it is not easy to have money to buy pills every month’ (Female-diabetes-Mozambique. Age 52). In other cases the financial impact of having to buy pills often appeared as an additional burden due to the many other ‘competing’ expenses: ‘I am having so many problems. I am the single earning member in my family, my children are studying, and there are also more expenses to purchase medicine’ (Male-Caregiver-diabetes-Nepal. Age 45)
Expenses associated with regular costs for medications, in the context of these low-income families appear as an additional stress over the fact of having a chronic condition. In those settings where non-Western medical services are available and widely used, expenses include using therapies provided by traditional healers:
Because of this disease, I have already tried many traditional treatments that have made me spend a lot of money and (buy) many things. People come and say that they can heal you, but in the end nothing happens. (Female-hypertension-Mozambique, Age 56)
In both Nepal and Peru, no mention was made regarding traditional treatments for diabetes and hypertension although they were mentioned for other conditions.
The need to cover the different expenses activated social support networks. In Peru, caretakers explained that they had to make arrangements among family members, particularly their adult children and their siblings living in the city, to ensure the costs of medications were covered. These financial arrangements did not appear so clearly in the testimonies of people in Nepal and Mozambique, but families played an important role in other caretaking duties. Families had to accommodate the needs of the person affected by a chronic condition such as accompanying the relative to the health facility: ‘I have to make time to go to the Doctor with her’ (Male-Caregiver-diabetes-Nepal. Age 45); ‘It is my children who accompany me to the hospital’ (Female-hypertension-Mozambique. Age 54).
Besides the regular visits to overcrowded health facilities and overseeing the daily intake of medications, family members’ social activities were disrupted. In Nepal, caregivers mentioned they had reduced their social lives to ensure the patient is not alone at home: ‘I cannot leave him and go just because he is ill. I need to take care of him as I am the guardian. I feel sad about it’ (Female-Caregiver-diabetes-Nepal. Age 80) or ‘I cannot leave him alone for long time, can’t go to my mother’s place’ (Female-Caregiver-hypertension-Nepal. Age 45). In Peru, the concerns of caregivers did not highlight reduced social activities but, an effort to avoid upsetting the individual as this might increase their blood pressure.
Other individuals shared the impact of the chronic condition in their relationship with their partners. The husband of a woman with hypertension in Peru said he missed working together with his wife in the fields and one female patient from Mozambique connected her marital problems with her chronic condition:
I had a husband who lived with me. He left home to live with another woman, so I wonder what is it with this disease that made him leave home, because I don’t know where he went to after living together for so many years. (Female-diabetes-Mozambique. Age 45)
The key element present in all the testimonies is that in one way or another, suffering from a chronic condition is not only a health issue, but a social one that disrupts family lives and social relations.
Emotional distress among family members
Throughout the interviews it became apparent that beyond concern for their own distress, individuals worried about their families:
… nowadays my family is worried every moment, if it is a hot day I get a call from all my children asking: ‘Papa, how are you today? How’s the temperature, are you okay?’ Everyone, including my wife, is calling: ‘How about this temperature? Are you in your office? Is the air conditioner on?’ You see … because people are worried about my health, I realize I’ve become like a baby. (Male-hypertension-Mozambique. Age 48)
[They ask me] ‘Mom, are you having high blood pressure now? You can no longer be as you were before: working or taking care of this or that’. (Female-hypertension-Peru. Age 51)
Perceptions of the stress felt by their relatives match what the relatives themselves said. They reported feeling constantly concerned about the individual’s wellbeing, either because he/she might die, because they are weak and more vulnerable, or their condition might get worse as a result of not following doctor’s prescriptions:
… you no longer live at peace because you are constantly thinking ‘she will die.’ And the truth is that high blood pressure is very dangerous; the brain can burst … (Female-Caregiver-hypertension-Peru. Age 48)
I sometimes feel bad due to his illness. I feel tense when he goes to PHC alone. I have a bad feeling that he might fall down on the way. (Male-Head of household-hypertension-Nepal. Age 33)
I am very tense because of his illness; he is ill but he doesn’t avoid foods. Fear and worry about him has increased. (Female-Caregiver-hypertension-Nepal. Age 45)
It is relevant to note that hypertension appears to cause more worries than diabetes because family members are aware that a stroke is a possible outcome. Worries about relatives with diabetes are related to ensuring the individual have and take their pills on time.
The distress among patients had to do with more personal issues such as the changes with their physical appearance or their capacity to perform sexually. Two women in Peru shared that they did not feel attractive anymore because of the significant weight loss due to poorly managed diabetes; and two men with diabetes in Mozambique mentioned the impact of their condition on their sex lives or relationship with their partners:
What complicates (your life) much more is diabetes, because sometimes it weakens the man, even more when he is going to have sex. (Male-diabetes- Mozambique. Age 50)
I said: ‘Look, I can’t have sex, I’m weak … that is because of this disease … it neutralizes the whole system of being a man’, I always talk to my wife but she says that I am having an affair and that is why I’m tired when I go to her. (Male-diabetes-Mozambique. Age 61)
These issues brought up mostly by individuals with diabetes show that chronic conditions also impact feelings of self-worth associated with being attractive for the opposite sex, their sexual performance and their couple relationships. In Nepal, participants did not bring up these matters when discussing the impact of having a chronic condition probably because people do not openly talk about these issues.
Changing the diet and cooking separate meals
The most dominant theme to emerge in the interviews was how diabetes and hypertension demanded a change in diets. Interviewees complained about having to avoid eating things they enjoy while incorporating ingredients or food preparations that they did not like so much:
I used to use more salt in my food, now it has decreased. I used to like oily food a lot, now I don’t eat such food. They say that sugar should also be avoided … (Male-hypertension- Nepal. Age 66)
(I have to eat) less salt, less spices (…) more fruits, more vegetables, all that (…) and well, I really dońt like vegetables that much (laughter). But well, (…) you end up getting used to not eating all those things ever. It is for our own good (…) Now, I have to drink only water (instead of juice) and I dońt like water that much … (Male-hypertension-Peru. Age 71)
… the most difficult thing for people is to get used to eating food without many things (…) When I cook cabbage, I cannot add peanuts, I have to live on salads or things like that. I cannot eat fried fish, we have to grill it, (we also cannot eat) meat, we don’t have anything left. (Female-diabetes- Mozambique. Age 60)
The implications of dietary changes in the food taste are the ones patients appear to resent the most. Having to reduce salt, sugar, and oil that are core components of the local diet are changes that are hard to incorporate. In Nepal, oily and spicy food are missed; in Peru, patients longed for desserts that are part of the local food culture and in Mozambique patients mentioned the reduction of fried food as a problem. The husband of a Mozambican patient considered diabetes worse than AIDS because of the dietary restrictions.
Change in diet affected the whole family since they had to adjust to the dietary modifications needed for managing hypertension or diabetes. Interviewees explained they reduced the frequency of fried meals, sugar, and salt, and everybody had to adjust to the new taste. In some cases, individuals had to prepare meals separately which represents an additional burden for female members of the family:
During preparation of food, I have to cook parboiled rice for myself, for others common rice. Regarding the vegetables, for myself I have to cook vegetables without potato. (Female-diabetes-Nepal. Age 45)
They have to prepare separate meals for me, avoiding spices in my food and also cooking vegetables without potato for me. For dinner they prefer rice but for me they cook roti (local bread). (Male-diabetes-Nepal. Age 45)
In addition to the time investment of cooking separate meals, there are financial implications that cannot be overlooked when thinking about chronic disease management in contexts of poverty: ‘Now we have to cook two meals, one for me and one for the other members of the family. But this is not always possible because of lack of money’ (Male-diabetes-Mozambique. Age 72).
Sometimes the cost of certain ingredients meant that people could not follow the diets recommended by the health workers, with potential negative consequences to their health and additional stress:
It is going to be two months or three months that I have not been able to buy vegetables [due economic constraints]. I am afraid that my blood pressure will go up, they say you can die because of high blood pressure. (Female-hypertension-Peru. Age 64)
Finally, the social role of sharing food is also affected when food preparation needs to be altered to accommodate the needs of people with diabetes or hypertension. As one woman from Mozambique explained:
I used to cook two pots (one with salt and one without salt) but now cooking two pots is difficult. When I cook rice I do not put salt, but it is difficult for the people at home to eat what they do not like, it does not make me feel good. (Female-diabetes- Mozambique. Age 52)
This quote highlights that cooking is not only about providing food for other family members but to ensure it is something others enjoy.
Dietary changes have an important meaning across all the interviewees. It meant extra work that usually fell on women, resulted in additional food expenditure and adjusting to different food tastes as that were less, salty, sweet or oily. Respondents expressed feeling responsible for other family members missing out on tastier foods, but also stress at the potential consequences of failing not to follow the dietary changes advised by health workers.
Discussion
Despite the differences among the countries, people’s daily lives, interpersonal relationships and family dynamics were similarly disrupted by chronic conditions. Having a chronic condition translated into a reduced capacity to fully participate in work and household activities that in turn impacted their families. Given that most of our participants lived in rural settings where productive activities are physically demanding and crucial for survival, disruption meant affecting their family’s wellbeing. Hondras et al.’s (Citation2016) finding on the implications of musculoskeletal disorders in rural Botswana also suggest that the meaning and consequences of physical ailments are exacerbated when lives are labour-intensive.
The economic implications of chronic condition management constituted stressful experiences for our participants as limited disposable income and financial means are not available to purchase different types of food or paying for necessary medications. Furthermore, adaptive strategies were also limited because in these countries there are no public-sponsored support schemes for unemployment or disability. Ill-health in these settings results in the disruption of the lives of other family members who need to step in to sustain the household.
To face the impacts produced by the chronic condition, individuals and their family members needed to change and reconfigure social roles and responsibilities. The inability to fulfil specific gender roles was particularly disruptive and translated into frustration, which has been documented by other studies (Allotey, Gyapong, & UNICEF/UNDP/World Bank/WHO Special Programme for Research and Training in Tropical Diseases, Citation2005; Charmaz, Citation1983; Weaver, Worthman, DeCaro, & Madhu, Citation2015). Charmaz (Citation1983) identified the lack of capacity to perform household chores as an additional source of distress for women with chronic conditions because the unattended chores translated into ‘tremendous amounts of self-blame and guilt’. In our study, female participants’ accounts mentioned the distress of failing their ‘duties’ as mothers and wives.
Our findings add to the literature on the disruptive effects of having a chronic condition (Becker, Citation1994; Bury, Citation1982; Mattingly & Garro, Citation2000) and the literature that highlights economic costs, changes in time allocation, emotional adjustments by those who live with a person affected by a chronic condition (Basra & Finlay, Citation2007; Bell, Tyrrell, & Phoenix, Citation2016; Lawrence, Citation2012; Mayberry, Harper, & Osborn, Citation2016). The experiences shared by informants coincide with what has been conceptualised as ‘disruption’, yet they also highlight the relevance of taking into consideration specific contextual issues such as the available resources to face the condition, including understanding their interaction with the health system (Unwin, Epping Jordan, & Bonita, Citation2004). The testimonies point to the additional economic stress caused by chronic conditions among low-income individuals in countries where public services do not provide an adequate social and health ‘safety net’.
Our research was not guided by the disruption framework, but rather this became our analytical reference. Unlike other qualitative studies on disruption and chronic conditions which used lengthy narratives or reiterative in-depth interviews in a longitudinal research project, the results we present are part of a broader study aimed at understanding the challenges of chronically ill patients in accessing timely and reliable care at the PHC. The testimonies collected did not render enough information about the impact on the sense of self, but more about the disruption at the family level under conditions of limited economic resources.
Although we had a gender balance in the informants, we did not explore the impact of chronicity with a gender lens. Another study would certainly need to incorporate these issues purposefully from the outset. We recognise that a deeper understanding of the meanings associated with being healthy or unhealthy in the selected communities as well as the explanatory models for chronic conditions would have enabled a more thorough comparison of our data. It was challenging to do a comparative study as data were collected in at least six different languages (Portuguese, Xangane, Nepali, Maithili, Hindi and Spanish), then translated into the main national language of the country, and then into English for comparison. We are certain some nuanced details of the data have been lost in this process of translation and cross translation and precluded a detailed discussion on the implications of chronic diseases in each setting. To address these challenges research teams were in regular contact to clarify any doubts and confirm the interpretation of the data.
Our study adds to the growing literature on disruption in LMIC. Using a comparative approach to analyse data across three very different countries, on three different continents, speaking at least six different languages is innovative, despite its challenges and limitations. The study shows that suffering from a chronic condition is more than a health issue, but also a social and economic one affecting individuals and their families in various ways; requiring health systems to respond to chronic care needs more widely and effectively.
Acknowledgements
We would like to thank all the people from the communities for sharing their time and their stories. We would also like to thank Dr Khatia Munguambe for her support during the design of the methodology and the data collection process in Mozambique. We also want to acknowledge the support from Jaime Miranda, Albertino Damasceno and Nilambar Jha for their advice at different stages of the research process.
Disclosure statement
No potential conflict of interest was reported by the authors.
ORCID
Maria Amalia Pesantes http://orcid.org/0000-0002-0649-3649
Claire Somerville http://orcid.org/0000-0002-2335-160X
Suman Bahadur Singh http://orcid.org/0000-0002-5375-1110
Silvana Perez-Leon http://orcid.org/0000-0003-4860-587X
Tavares Madede http://orcid.org/0000-0001-8194-8597
Suzanne Suggs http://orcid.org/0000-0001-6084-5468
David Beran http://orcid.org/0000-0001-7229-3920
Additional information
Funding
References
- Allotey, P., Gyapong, M., & UNICEF/UNDP/World Bank/WHO Special Programme for Research and Training in Tropical Diseases. (2005). The gender agenda in the control of tropical diseases: A review of current evidence. Retrieved from http://www.who.int/iris/handle/10665/69067
- Azungah, T. (2018). Qualitative research: Deductive and inductive approaches to data analysis. Qualitative Research Journal. doi: 10.1108/QRJ-D-18-00035
- Barros, M. E., Cesar, C. L. G., Carandina, L., & Torre, G. C. (2006). Social inequalities in the prevalence of chronic diseases in Brazil. Saúde Coletiva, 11(4), 911–926. doi: 10.1590/S1413-81232006000400014
- Basra, M. K. A., & Finlay, A. Y. (2007). The family impact of skin diseases: The greater patient concept. The British Journal of Dermatology, 156(5), 929–937. doi: 10.1111/j.1365-2133.2007.07794.x
- Becker, G. (1994). Metaphors in disrupted lives: Infertility and cultural constructions of continuity. Medical Anthropology Quarterly, 8(2), 383–410. doi: 10.1525/maq.1994.8.4.02a00040
- Bell, S. L., Tyrrell, J., & Phoenix, C. (2016). Ménière’s disease and biographical disruption: Where family transitions collide. Social Science & Medicine, 166, 177–185. doi: 10.1016/j.socscimed.2016.08.025
- Bentzen. (2003). WONCA dictionary of general/family practice. Copenhagen.
- Burridge, L., Foster, M., Donald, M., Zhang, J., Russel, A. W., & Jackson, C. (2016). Making sense of change: Patients’ views of diabetes and GP-led integrated diabetes care. Health Expectations, 19, 74–86. doi: 10.1111/hex.12331
- Bury, M. (1982). Chronic illness as biographical disruption. Sociology of Health and Illness, 4(2), 167–182. doi: 10.1111/1467-9566.ep11339939
- Bury, M. (1991). The sociology of chronic illness: A review of research and prospects. Sociology of Health and Illness, 13(4), 451–468. doi: 10.1111/j.1467-9566.1991.tb00522.x
- Büssing, A., Ostermann, T., Neugebauer, E. A., & Heusser, P. (2010). Adaptive coping strategies in patients with chronic pain conditions and their interpretation of disease. BMC Public Health, 10, 507. doi: 10.1186/1471-2458-10-507
- Campbell, R., Pound, P., Pope, C., Britten, N., Pill, R., Morgan, M., & Donovan, J. (2003). Evaluating meta-ethnography: A synthesis of qualitative research on lay experiences of diabetes and diabetes care. Social Science & Medicine, 56, 671–684. doi:10.3310/hta15430 doi: 10.1016/S0277-9536(02)00064-3
- Charmaz, K. (1983). Loss of self: A fundamental form of suffering in the chronically ill. Sociology of Health & Illness, 5(2), 168–195. doi: 10.1111/1467-9566.ep10491512
- Charmaz, K. (1994). Identity dilemmas of chronically ill men. The Sociological Quarterly, 35(2), 269–288. doi: 10.1111/j.1533-8525.1994.tb00410.x
- Eshun-Wilson, I., Rohwer, A., Hendricks, L., Oliver, S., & Garner, P. (2019). Being HIV positive and staying on antiretroviral therapy in Africa: A qualitative systematic review and theoretical model. PLOS ONE, 14(1), e0210408. doi: 10.1371/journal.pone.0210408
- health.data.org. (2016). Financing Global Health Database. Retrieved from Financing Global Health Database.
- Hondras, M., Hartvigsen, J., Myburgh, C., & Johannessen, H. (2016). Everyday burden of musculoskeletal conditions among villagers in rural Botswana: A focused ethnography. Journal of Rehabilitation Medicine, 48(5), 449–455. doi: 10.2340/16501977-2083
- Hsieh, H.-F., & Shannon, S. E. (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277–1288. doi: 10.1177/1049732305276687
- INEI. (2017). CENSO NACIONAL. XII de Poblacion, VII de Vivienda y II de Comunidades Indigenas.
- Instituto Nacional de Estatística. (2015). Relatório final do inquérito ao orçamento familiar – iof-2014/15. Maputo, Moçambique.
- Lawrence, E. (2012). The Impact of Chronic Illness on the Family. IG Living, June–July.
- Mairami, F. F., Warren, N., Allotey, P. A., Mak, J. S., & Reidpath, D. D. (2018). Documenting the impact of stroke in a middle-income country: A Malaysian case study. Disability and Rehabilitation, 1–12. doi: 10.1080/09638288.2018.1493544
- Mattingly, C., & Garro, L. C. (2000). Narrative and the cultural construction of illness and healing. London: University of California Press.
- Mayberry, L., Harper, K., & Osborn, C. Y. (2016). Family behaviors and type 2 diabetes: What to target and how to address in interventions for adults with low socioeconomic status. Chronic Illness, 12(3), 199–215. doi: 10.1177/1742395316644303
- Nolte, E., & McKee, M. (2008). Caring for people with chronic conditions: An introduction. In European observatory on health systems and policies series. Caring for people with chronic conditions. A health system perspective (pp. 1–14). Berkshire: Open University Press.
- Pound, P., Gompertz, P., & Ebrahim, S. (1998). Illness in the context of older age: The case of stroke. Sociology of Health & Illness, 20(4), 489–506. doi: 10.1111/1467-9566.00112
- Rimal, B. (2013). Population growth and land use dynamics in Eastern part of Jhapa district, Nepal. GISNepal, XII, 12–17.
- Robinson, C. A. (1993). Managing life with a chronic condition: The story of normalization. Qualitative Health Research, 3(1), 6–29. doi: 10.1177/104973239300300102
- Unwin, N., Epping Jordan, J., & Bonita, R. (2004). Rethinking the terms non-communicable disease and chronic disease. Journal of Epideliology Community Health, 2004(58), 801–803.
- Weaver, L. J., Worthman, C. M., DeCaro, J. A., & Madhu, S. V. (2015). The signs of stress: Embodiments of biosocial stress among type 2 diabetic women in New Delhi, India. Social Science & Medicine, 131, 122–130. doi: 10.1016/j.socscimed.2015.03.002
- WHO. (2002). Innovative care for chronic conditions: Building blocks for action: Global report. Geneva: World Health Organization.
- WHO. (2015). Country health profiles. Retrieved from http://www.who.int/countries/
- Williams. (2000). Chronic illness as biographical disruption or biographical disruption as chronic illness? Reflections on a core concept. Sociology of Health & Illness, 22(1), 40–67. doi: 10.1111/1467-9566.00191
- The World Bank Group. (2018). World development indicators.
- Wouters, E., & Wet, K. D. (2016). Women’s experience of HIV as a chronic illness in South Africa: Hard-earned lives, biographical disruption and moral career. Sociology of Health & Illness, 38(4), 521–542. doi: 10.1111/1467-9566.12377