 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
This article examines the adaptation and biomedical transition of people living with HIV (PLHIV) to antiretroviral treatment (ART) in Burkina Faso. The study employs a representative sample of 3625 randomly selected patients. Subjective and objective measures of health and their predictors are compared for short-term (≤24 months) versus longer-term ART adherents (>24 months) in a cohort study. Subjective health is measured as Likert scale self-rating and objective health as CD4 count. The results show that subjective and objective health capture different aspects of adaptation to ART: 90% of the short-term and 94% of the longer-term patients give a subjective health rating of at least good, while the objective measure of good health is higher among longer-term (42%) compared to short-term patients (27%). For subjective health, short-lived pleasures are predictors among short-term adherents while economic characteristics are determinants among longer-term patients. Meanwhile, objective health is associated with factors that determine ART adherence (i.e. participating in self-help groups). To achieve a wholistic resilience management that caters to the needs of PLHIV, we need to acknowledge adaptation to the disease and to ART and design health programs, in particular in developing countries, away from one-size-fits-all solutions to stage-of-disease specific support.
Introduction
People living with HIV (PLHIV) can now adapt to the disease and enjoy a long and healthy life by adhering to antiretroviral treatment (ART). Recent studies show that patients transit from an early period of disruptive psychological and physical trauma to a stable long-term state of good health (Baranov, Bennett, & Kohler, Citation2015; Thornton, Citation2012). This process involves changes in priorities, values and objectives in life between the early phase of uncertainty and fear about survival, and the mature phase after securing survival and reincorporating into society (Russell & Seeley, Citation2010; Russell et al., Citation2007). While confronting a life-threatening disease is unsettling and transformative, the literature on adaptation explains that people first react strongly to negative health shocks but revise to conventional levels of wellbeing over time (Albrecht & Devlieger, Citation1999). To date, there is scarce evidence on how subjective and objective measures of health are shaped throughout the course of the transition phase, and there is even less evidence about the role of socio-economic correlates in the adaptation process.
This paper investigates how patients cope and adapt to the life-threating diagnosis of HIV in a resource-poor setting. We assess whether there are shifts in subjective and objective measures of health and their associated socio-economic determinants. Changes in both health measures are contrasted since the adjustment processes are likely to be different as the indicators capture different aspects of wellbeing.
Three general reasons guide the research on subjective and objective measures of health. First, both measures have become an important goal of public policies and a non-negligible criterion for resource allocation in health care (Dolan & Kahneman, Citation2008). Second, existing evidence has demonstrated that measures of health and wellbeing are credible predictors of economic activity and biological outcomes. Indicators of subjective health and wellbeing have enhanced our understanding of unemployment, inflation, gross domestic product, social capital, migration, social relationships, and related areas (Di Tella, MacCulloch, & Oswald, Citation2001; Dolan & Kahneman, Citation2008). Similar studies have found a strong association between subjective and objective measures with health conditions such as mortality, severity of mental disorders, disability, intensity and prevalence of chronic diseases, medical expenses and utilization, stress, and physical functioning (Benjamins, Hummer, Eberstein, & Nam, Citation2004; Doiron, Fiebig, Johar, & Suziedelyte, Citation2015; Jylhä, Citation2009; Wu et al., Citation2013). Yet, the findings have to be interpreted knowing that the ratings of subjective health may vary across patients’ understanding, believes and sociocultural context even within one country. Third, the success in predicting health outcomes has encouraged research on the underlying determinants that predict subjective health (Addai & Adjei, Citation2014; Koelmeyer, English, Smith, & Grierson, Citation2014).
The leading theories on hedonic adaptation and response shift provide a rationale why PLHIV may adapt to the disease over time. First, hedonic adaptation involves the reaction and judgment of individuals to negative or positive stimuli according to their own histories that act as reference points of comparison (Frederick & Loewenstein, Citation1999). The phenomenon conceptualizes that a person who undergoes a negative (health) shock could adapt to the situation so that the new poorer state does not translate into lower subjective health in the long-term (Dolan & Kahneman, Citation2008). A host of research confirms the presence of hedonic adaptation in diverse areas of wellbeing demonstrating that life shocks can have small impacts on happiness (Oswald & Powdthavee, Citation2008). There is also evidence of hedonic adaptation in many areas of health such as disability, chronic illnesses, and long-term treatments. In a longitudinal study, patients with prior heart histories were less likely to report worse subjective health when they experienced a new heart problem compared to first-time patients (Wu, Citation2001). In a similar vein, a study on patients of haemodialysis shows that they are happier than the predictions of healthy individuals (Riis et al., Citation2005). Moreover, people with a new sudden physical disability initially report aversion to work, but over time, they return to their initial level of wellbeing at a rate of about 30–50% (Schwartz, Andresen, Nosek, & Krahn, Citation2007). And more recently, it has been shown that women adapt to breast cancer in terms of health-quality (Tessier, Blanchin, & Sébille, Citation2017).
Second, response shift is a phenomenon closely related to hedonic adaptation (Schwartz & Sprangers, Citation2000). Response shift conceptualizes that life priorities and expectations are updated and recalibrated after new life circumstances (Postulart & Adang, Citation2000; Schwartz & Sprangers, Citation1999; Sharpe & Curran, Citation2006). Three factors may trigger this redefinition: (i) recalibration, (ii) reprioritization, and (iii) reconceptualization. Recalibration involves the alteration in an individual’s internal standards after a new life-changing situation. Reprioritization refers to changes in personal priorities and values such as valuing health more than income after the announcement of a deadly disease. Reconceptualization comprises the redefinition of an individual’s standard of health over their life (Pierret, Citation2007). Thus, response shift implies a change in the reference point of what good health means when confronted with an unfortunate diagnosis. Previous research has documented response shift in patients of asthma, diabetes, epilepsy, hemophilia, breast cancer, and kidney disease (Sharpe, Butow, Smith, McConnell, & Clarke, Citation2005; Tessier et al., Citation2017).
The present study contributes to the literature in four ways presenting an important feature compared to past research. First, we compare short-term versus longer-term adherents to ART to assess whether patients of HIV reach a steady level of subjective health in the course of treatment adherence. We also approximate the response shift phenomenon by investigating whether subjective health is higher among PLHIV compared to the healthy population. Second, we contrast subjective and objective measures of health since they evaluate different aspects of wellbeing and their adjustment processes are likely to differ. Third, our analysis strengthens the existing literature by using a nationally representative sample of 3625 PLHIV in a resource-poor setting, namely Burkina Faso. Fourth and most importantly, although there is ample research about hedonic adaptation and response shift for a range of medical conditions, there is scant evidence about patients of HIV under ART, especially in resource-poor contexts where income constraints and perceived social stigma may be more intense. The study that is closest to ours analyses 1700 Australian PLHIV showing that income, employment, presence of social support, self-reports about recent sexual activity and participation in support groups are strong predictors of subjective health (Koelmeyer et al., Citation2014).
To test the adaptation and biomedical transition in health we investigate subjective and objective measures of health analyzing a database with 3625 observations in a cohort study design. The subjective health measure that we employ uses a five-point Likert scale to provide a qualitative self-report about patients’ perception of their health status. Rankings range from (1) very bad to (5) very good health. The objective measure is a physical biomarker and consists of patients’ CD4 counts, which is the measure of disease progression that is most readily available in the Burkinabe health system. According to WHO (Citation2013), the CD4 count provides an impartial indication about the state of the immune system of PLHIV. In the empirical analysis of adaptation and biomedical transition in health measures we employ two steps: First, we assess changes in subjective health and its socio-economic determinants. Second, we compare the findings for subjective health with the predictors of the objective indicator of health.
Adaptation and biomedical transition in PLHIV: From short-term to long-term adherents
PLHIV experience a severe and intense process of adjustment between the early phase of shock after discovering the disease, and the mature phase of management and acceptance (Kralik, Koch, Price, & Howard, Citation2004). The early experience of starting ART is disruptive for a person’s life (Russell & Seeley, Citation2010). Treatment initiators struggle to maintain control and a positive outlook on life since they experience stigma, fear, isolation, distress, and uncertainty about survival (Rhodes, Bernays, & Terzić, Citation2009). Incorporating ART in daily routines requires major non-linear adjustments in activities and living standards that involve many challenges along the way (Sharpe & Curran, Citation2006). Accommodating the treatment scheme and the new health condition require drastic adjustments in activities, relationships, parenting, employment and consumption patterns, leisure, and many other areas of life (Kralik et al., Citation2004; Pierret, Citation2007; Rhodes et al., Citation2009; Russell & Seeley, Citation2010; Russell et al., Citation2007).
Instead, research demonstrates that patients can return to an improved and healthy status when adhering to ART in the long-term. Several studies describe how PLHIV experience transformative and empowering effects after maturing in the management and acceptance of the treatment (Neuman, Obermeyer, & MATCH Study Group, Citation2013; WHO, Citation2013). By securing survival and recovering physical strength, long-term adherents take agency and reactivate their life as independent workers and achievers (Russell & Seeley, Citation2010). Long-term adherents can even attain the leading status of experts in their communities becoming valuable resources for new patients and the broader community (Pierret, Citation2007; Russell & Seeley, Citation2010).
Conceptual framework: Predictions about adaptation and biomedical transition
Assuming the presence of response shift we expect that as PLHIV integrate antiretroviral treatment into their daily routines they demonstrate higher ratings of subjective health compared to the general population (). PLHIV revalue their state of health since loss aversion changes their perception of good health. This effect increases their perception of subjective good health. We do not anticipate hedonic adaptation as patients experience permanent costs and side effects of the disease. Thus, response shift will not revert or disappear so that subjective health will stay high and stable over time (or as long as patients adhere to ART). We hypothesize that the subjective report could increase among long-term adherents as they continuously feel physically better. Comparatively, with regard to objective health, we expect that short-term adherents show lower health than the general population since they have only recently initiated ART as a response to a deterioration of their health. In contrast, those patients that remain under ART will improve their objective health status in the long-term. Long-term adherence to ART can suppress HIV leading to (a close to) normal life.
Figure 1: Theoretical predictions.
sNotes: The vertical axis displays the level of health and the horizontal axis the duration under ART. SH abbreviates subjective health. The hypothesis HSH,i is formulated for short-term adherents with respect to subjective health; the hypothesis HSH,l is formulated for long-term adherents with respect to subjective health; hypothesis H is for all PLHIV and refers to both subjective and objective health.
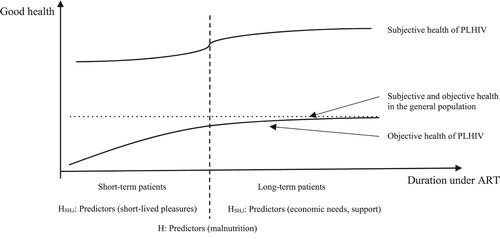
Furthermore, we also expect adaptation in the determinants of health. Since the early process of adaptation shifts patients’ priorities, we expect that short-lived pleasures that are sources of immediate happiness will be positively correlated with the subjective health measure (Pierret, Citation2007; Russell & Seeley, Citation2010). The focus on short-lived pleasures is plausible since patients are aware that ART does not necessarily work for everybody (Russell & Seeley, Citation2010; Russell et al., Citation2007; WHO, Citation2013). This is what we refer to as hypothesis HSH,i in . In contrast, long-term adherents can return to ‘normality’ once they have adapted to the disease and have managed to integrate ART in their lives (Pierret, Citation2007; Russell et al., Citation2007). In terms of the determinants of subjective health we anticipate that short-lived pleasures lose their importance in the long-term by shifting personal values towards economic needs and social success. This is denoted as hypothesis HSH,l in . Thus, we expect the reversal to pre-disease levels in the determinants.
Independent of phase of adherence, we expect that patients of HIV with better nutrition also report better subjective health (see hypothesis H in ) (Masa, Chowa, & Nyirenda, Citation2018).
For the measure of objective health, we expect a sharp and strong biomedical transition from a very low level in early adherents to a higher level in long-term patients. The existing literature provides little guidance on determinants of health biomarkers among PLHIV. Nutrition is the only exception that has systematically shown to support the development of resilience against HIV (Anema, Vogenthaler, Frongillo, Kadiyala, & Weiser, Citation2009; Houtzager, Citation2009; Koethe et al., Citation2010). The literature has identified three pathways: (i) there is an overlap between HIV prevalence and malnutrition (Anema et al., Citation2009), (ii) PLHIV are more vulnerable to malnutrition than the general population (Houtzager, Citation2009), and (iii) malnutrition is a predictor of mortality among PLHIV (Koethe et al., Citation2010). Thus, we consider malnutrition as the link between subjective and objective health, and we expect malnutrition to be negatively associated with both indicators.
Materials and methods
Study setting
Burkina Faso is a land-locked West-African country. According to the Human Development Index in 2018 the country scores (very) low in human development by ranking 183 out of 189 nations. The country is ethnically diverse and multilingual where the ‘Mossi’ ethnicity constitutes 50% of the population.
In 2016, the adult (15–49 years) HIV prevalence rate was 0.8% (UNAIDS-a, Citation2016). Since 2005, the prevalence rate has been stable, and by 2010 new HIV infections had decreased by 45% (UNAIDS, Citation2012). Nevertheless, there are considerable disparities in prevalence rates by place of residence and region: Prevalence is lower in rural (0.6%) compared to urban areas (2.3%) (UNAIDS, Citation2012). The feminization of HIV is also a phenomenon observed in Burkina Faso with two-thirds of the registered HIV cases being women (UNAIDS-b, Citation2016).
Burkina Faso provides medical HIV support in 100 public, private and community health centers located in 13 regions of the country (UNAIDS-a, Citation2016). Since 2010 antiretroviral medication is free, and in 2015, Burkina Faso achieved the continuous provision of ART to all patients under treatment. There are an estimated 95,000 PLHIV in the country, of whom between 46,000 and 70,300 are on ART (UNAIDS, Citation2012). By 2016, the coverage rate of ART was 70% (UNAIDS-a, Citation2016). However, the challenges of transportation, stigma and time frequently prevent PLHIV to adhere to ART. In practice, some centers also require patients to pay for specialized medical tests such as the CD4 count. For that reason, not all PLHIV have up-to-date test results in the study.
Another important feature of the Burkinabe context is the presence of HIV/AIDS self-help groups/associations. These voluntary associations serve as support groups offering regular meetings, counselling, and occasional financial funds for nutrition and medical tests. The main objective of the self-help groups is to prevent PLHIV from social isolation, leading them to a functional life as individuals, family members and members of their communities.
Study design
We analyze a nationally representative sample of patients of HIV who undergo ART in Burkina Faso in 2015. The total dataset comprises 3625 patients randomly selected from 80 health centers across the 13 health regions of the country. The patients were interviewed between February and May 2015. Eligibility consisted in being older than 15 years and providing written informed consent. Moreover, trained enumerators privately administered the survey to ensure confidentiality (Wagner, Ouedraogo, Artavia-Mora, Bedi, & Thiombiano, Citation2016). The survey contains information on patients’ subjective health, CD4 counts, as well as demographic and socio-economic characteristics.
Data analysis
Outcome indicators
The outcome indicator for subjective health is based on responses to the survey question ‘How do you rate your health?’. Responses are given on a five-point Likert scale ranging from (1) very bad, (2) bad, (3) fair, (4) good, to (5) very good. We employ the responses in two ways. First, we directly assess the given health ratings. Second, we build a dichotomous variable combining response categories (4) and (5) as being in good health, denoted by one and zero otherwise. We analyze both subjective health variables to assess the sensitivity of our findings to the definition of subjective health.
The measure of objective health is the CD4 count as it provides an indication of the health of the immune system and no other biomarker is regularly assessed by the Burkinabe health system. The CD4 count of a healthy person ranges between 500 and 1500 CD4 cells per cubic millimeter of blood. PLHIV who have a CD4 count over 500 are in good health whereas those below 200 are at a high risk of death (WHO, Citation2013). Similar to subjective health, we analyze the CD4 count directly and by building a dichotomous variable with patients with CD4 counts above 500 (in good health), coded as one, and zero, otherwise.
Control variables
As determinants of good health we consider an individual’s nutritional status, demographic, educational and economic characteristics, and two related variables: (i) whether the individual participates in an HIV/AIDS self-help group, and (ii) whether the individual had sexual intercourse in the week prior to the survey. We capture nutritional status employing weight. Ideally, we would have used BMI to proxy nutrition but we do not have height measurements for the majority of the sampled individuals. The individual-level demographics are gender, age, marital status, religion and ethnicity.
Additionally, we control for household demographics. The household demographics capture household size using: (i) whether the individual has children, and (ii) the share of male and female individuals above 15 years. The latter two variables show whether the household has female adults and capture the possibility of labor sharing. We also use four educational categories and a binary variable for fluency in French. We compare patients with primary, basic secondary and higher education to no formal education (excluded category).
Three variables reflect the economic situation of the patient: (i) an indicator evaluates active work; (ii) there is information on individual income; and (iii) we include whether the individual comes from an agricultural household. Moreover, we use a binary variable to indicate whether the patient participates in an HIV/AIDS self-help group. Finally, we control for sexual intercourse in the last seven days. Because sexual transmission is one of the major transmission channels of HIV, there have been considerable sensitization efforts around HIV and sex (Kalichman, Carey, & Johnson, Citation1996). Therefore, we consider information about sexual activity a potential determinant of the wellbeing of PLHIV.
Empirical specification
We employ descriptive and multivariate analyses to examine our predictions. First, we carry out an independent sample t-test for a comparison of means of the outcome variables. Second, we implement a linear regression model for the multivariate analysis. As a robustness check we make use of an ordered probit model for the subjective health ratings. We specify the following model for patient i who has attended health center c to assess the determinants of health across the transition path:(1)
(1) where Yic represents either subjective or objective health. We control for malnutrition using weight (Malnutric) and the demographic variables are denoted by Demoic. To adjust for non-linearities we include weight and its squared term.Footnote1 In a second step we add the educational and economic controls represented by Edu_Ecoic and, in a third step we add two related variables: Groupic capturing the membership in an HIV/AIDS self-help group, and Sexic comprising active sexual intercourse in the last seven days. In all specifications we include health center-specific effects (λc) to capture differences in infrastructure, local traditions, local policies, and geography. The fixed effects also address concerns about context-specific perceptions of the subjective health rations. The standard errors are clustered at the health centre level to account for correlations in the unobservable characteristics (εic).
We split our sample into two groups to allow for a comparison of cohorts within our sample: short-term and long-term adherents. We divide the sample at 24 months of adhering to ART. Three criteria guide this choice. First, the recent medical literature on HIV demonstrates that PLHIV experience the strongest psychological and biological changes during the first two years on ART (Russell et al., Citation2007). Second, current qualitative evidence explains how the early challenges that PLHIV face in quality of life and objectives become more mature and complete after two years (Kralik et al., Citation2004; Rhodes et al., Citation2009; Russell et al., Citation2007; WHO, Citation2013). And third, drop-out rates are higher during the initial two years of adherence to ART (Fox & Rosen, Citation2010; Rosen, Fox, & Gill, Citation2007). But there is limited evidence on the psychological and physical evolution of PLHIV after two years of adherence to ART. By splitting the sample at 24 months we capture the most prominent differences between shorter and longer-term ART adherents. Hence, we estimate Equation (1) separately for the two cohorts of HIV patients in our database to compare short-term (≤24 months) versus long-term adherents (>24 months).
Results
This section contains four parts. First, we introduce the characteristics of our sample. Second, we provide descriptive statistics for the health outcomes. The third part outlines adaptation in the predictors of subjective health and the fourth part shows the results for the transition in the determinants of the objective health indicator.
Descriptive statistics
Descriptive statistics: Determinants
Descriptive statistics are presented in . The average age of a patient in our sample is 41.3 years and the majority are female (69%). The high rate of female PLHIV is not unusual and is commonly referred to as the feminization of HIV (Quinn & Overbaugh, Citation2005). But the large share of women may simply reflect a higher detection rate as in Burkina Faso HIV testing is part of antenatal care. Likewise, sex differences in health-seeking behaviors between Burkinabe women and men may also explain the lower level of ART enrolment by men (Auld et al., Citation2015).
Table 1. Descriptive statistics.
The average household size is 7 which is similar to the average household size of 7.4 reported in the 2014 Burkina Faso Continuous Multisector Survey (Enquête Multisectorielle continue) (World Bank, Citation2017). The majority of respondents have children (89%) and are married or live in cohabitation (57%). Among short-term adherents the share of married individuals is larger, namely 59.6% versus 55.8% among long-term adherents (p-value = 0.066). A considerable share of the sample loses their partner in the course of the disease. We observe nearly 23.7% of widows/widowers among long-term adherents versus 18.1% among short-term patients (p-value = 0.000). We also report the share of working age (fe)males in the households of the respondents to capture intra-household demographics. The average household has a share of 26.4% (35.9%) (wo)men. Muslims account for roughly half the sample (50.7%), Christians for 44.9%. Mossi represent the main ethnicity with 52.6% of respondents, which is similar to official country statistics.
More than half the sample has no formal education with no differences between short-term and long-term patients. Concerning economic characteristics, we observe that long-term adherents are qualitatively speaking 3.3 percentage points more likely to report that they are actively working. This is reasonable as survival encourages patients to continue their life and work.
Almost 40% of the patients are members of an HIV/AIDS self-help group. This figure highlights that Burkina Faso is a country with very active associations. However, participation in these groups is not very prominent among short-term adherents (24.9%). It increases among long-term adherents to almost 50% (p-value = 0.000). The literature confirms this finding as social isolation and stigma are an initial reaction in the process of adjustment to the disease (Russell & Seeley, Citation2010; Russell et al., Citation2007). Lastly, about 37% of individuals had sexual intercourse in the week prior to the survey.
Descriptive statistics: Outcome indicators
The self-assessed health rating is very high with an average of 4.36 out of 5 and 92% (n = 3625) of patients report that they are in good or very good health. This is a substantially higher figure compared to the general population. According to the latest World Values Survey for Burkina Faso in 2007, the general population reports an average rating of 2.96 out of 4 (after transforming the scale for comparison), and only 72% (n = 1519) report good subjective health. This finding is consistent with previous evidence on the response shift. Amongst short-term patients we observe an average health rating of 4.3, whereas longer-term adherents have an average of 4.4. This difference is small albeit statistically significant (p-value = 0.000) showing that while response shift continuous after 24 months, the main force driving the shift occurs in the initial 24-months.
The response shift phenomenon is further highlighted when considering the share of individuals who report being in (very) good health. Among the short-term patients this share amounts to 89.6% (n = 1408) while among the long-term adherents the share is 93.7% (n = 2217). The difference of 4.1 percentage points corresponds to a small positive and statistically significant difference between the two cohorts (p-value = 0.003). Thus, we document a response shift in subjective health which occurs quickly and does not change greatly over time.
Furthermore, we find strong patterns of biomedical transition between short-term and long-term adherents.Footnote2 Short-term patients have an average CD4 count of 388 while for long-term adherents it is 490 (p-value = 0.000). Similarly, the share of short-term patients in good health is 26.6% whereas it is 42.3% among long-term adherents. The increase in the CD4 count is consistent with medical and economic research demonstrating the efficacy and usefulness of ART to boost CD4 counts in PLHIV (WHO, Citation2013). Notably, the contrasting evolution between the sharp change in CD4 counts and the slow change in the subjective health measure suggests that while both indicators are useful and informative, they measure different dimensions of wellbeing. A pairwise correlation between subjective health and the CD4 count yields a small (4%) albeit statistically significant (p-value = 0.059) correlation.
In sum, subjective health is an omnibus measure, contrarily to the CD4 count, and includes both physical and psychological aspects. The rapid adjustment in subjective health may occur as reaction to obtaining ART and the sense of relief that comes with acquiring a new lease of life. Instead, psychological factors influence less the objective measure, which is mainly driven by the use of antiretroviral medication. Therefore, both health measures should not be used as substitutes in this context.
Adaptation in subjective health
In we present the determinants of subjective health for short-term versus long-term patients. The outcome variable is a five-point Likert scale rating of subjective health. Three results stand out that are similar across cohorts: First, individuals with better nutritional status also report higher subjective health. The coefficient is small albeit statistically significant. A one standard deviation increase in weight (10.65) increases subjective health by 0.23 to 0.28. This increase is small given that the average subjective health rating is 4.4. Although small, the effect of one sample standard deviation increase in weight (10.65) amounts to 35% of the sample standard deviation of subjective health (0.65).Footnote3
Table 2. Determinants of subjective wellbeing for ART short-term versus long-term patients (Outcome variable: Likert scale rating of subjective wellbeing).
Second, being economically active is a positive determinant of subjective health for short-term and long-term adherents. We observed in the field and in the literature that for the former, having a paid task gives them purpose and meaning in a period where they are experiencing emotional distress. Suspending work promotes feelings of solitude, low self-esteem and poor outlook (Neuman, Obermeyer, & MATCH Study Group, Citation2013; Rhodes et al., Citation2009; Russell & Seeley, Citation2010; Russell et al., Citation2007). For long-term adherents, having economic activity and income secures household wellbeing. This implies that general economic wellbeing regains importance in long-term patients once they have secured their survival (Kralik et al., Citation2004; Russell & Seeley, Citation2010; Russell et al., Citation2007; WHO, Citation2013).
Third, adherents from households with a larger share of women above 15 years report higher subjective health. In the field, we found that women are more likely to be supportive in work share arrangements. Since two-thirds of our sample consists of women, this finding is not particularly surprising but only highlights the collectivist culture of Burkina Faso. Note that the relationship becomes more pronounced for long-term ART patients showing that help from family members might be considered more important in the long-run.
Next, we identify two main determinants of subjective health among short-term patients. First, we observe that individuals who have children report higher subjective health. The effect is 16% to 18% of a standard deviation in subjective health. Second, enjoying the short-lived pleasure of sexual intercourse is positively associated with subjective health among short-term patients. The estimate of 0.12 explains as much as 18% of the standard deviation in subjective health. This finding shows that individuals who are in the early phase of disruption and adjustment place a relatively larger importance for living now and enjoying the current happiness of life.
In contrast, for long-term adherents the (short-term) effects of having children and sexual intercourse fully vanish. We find a shift in determinants away from short-lived and subjective sources of joy towards purely economic and practical considerations. Income is positively and statistically significantly associated with the subjective health of long-term patients.Footnote4 While the economic effect is small –a one standard deviation increase in income (59.78) increases subjective health by 0.02– it indicates that economic concerns gain importance in the long-run. A second finding shows that members of agricultural households report lower subjective health in the long-term. This is not surprising since the agricultural households in the sample are poor and engage in labor-intensive activities. Thus, this result supports the notion that economic concerns regain importance among long-term adherents. In addition to economic factors, we find that married individuals report higher subjective health. Being married increases subjective health by 17% of a standard deviation and supports the idea of a positive effect of stable family arrangements for long-term antiretroviral patients. Finally, we find a small negative effect stemming from age.
To assess the robustness of our findings we employ two additional models. First, we estimate a model employing a dichotomous subjective health variable coding (very) good health as one and zero otherwise. The results confirm the patterns discussed above suggesting that the findings are not sensitive to the scaling or the definition of the outcome variable. Second, we employ an ordered probit model for the subjective health ratings and the findings are again similar to those discussed above (results not shown).Footnote5
Biomedical transition in objective health
presents the results associated with the determinants of objective health.Footnote6 Three patterns persist throughout the adaptation process. First and similar to subjective health, weight is positively associated with the objective health measure. The effect is larger for short-term patients but persists for long-term patients. An increase in weight of one standard deviation (10.65) increases the CD4 count of short-term patients by about 90. This finding suggests that weight is the link function between the two health measures.
Table 3. Determinants of CD4 counts for ART short-term versus long-term patients.
Second, while there is no gender difference in subjective health, we find strong gender differences in the objective indicator of health. Across treatment stages, women have a CD4 count that is at least 50 counts higher on average. This is consistent with the pattern found in the data that women have spent a longer duration on ART as compared to men. Third, individuals who are members of self-help groups have substantially higher CD4 counts.
Moreover, we also identify treatment stage-specific determinants. We find an interesting sign reversal with respect to being married. Short-term adherents who are married report a CD4 count that is roughly 25 counts lower but statistically insignificant. Since early PLHIV experience feelings of stigma, fear, and isolation, it might be that the closeness of living as a married couple makes it harder for short-term patients to (secretly) take their medication (Pierret, Citation2007; Rosen et al., Citation2007; Russell & Seeley, Citation2010). However, for long-run adherents, marriage increases CD4 counts and the coefficient is precisely identified. The effect is similar to an increase of at least 60 counts. A similar sign reversal is present in patients with secondary or higher education. Initially, patients that are more educated have lower CD4 counts compared to non-educated individuals but the effect reverts for long-term patients. While we do not find any direct income or economic effects, we observe that long-term adherents who live in large households are worse off. Reducing household size by one sample standard deviation (5.19) increases their CD4 count by roughly 10 counts.
To assess the robustness of our results we also employ an indicator variable of objective health. Individuals are coded as healthy who have a CD4 count of 500 or above. We identify the same determinants and dynamics as for the model with the counts.Footnote7
Overall, the biomedical transition is more pronounced than changes in subjective health. Moreover, the changes occur at different speeds indicating that subjective and objective health measures capture different aspects of patient wellbeing.
Discussion
We contribute to the literature on response shift by examining temporal changes in subjective and objective health amongst PLHIV. We also examine the socio-economic determinants of these health outcomes between a cohort of short-term (24 months or less) and long-term patients (more than 24 months). To examine the adaptation process we employ a nationally representative sample of PLHIV undergoing ART in Burkina Faso. The subjective health measure employs a qualitative 5-point Likert scale from very poor (1) to very good (5) health, while the objective measure uses the CD4 count.
We find a small and statistically significant increase in self-reported good health from short-term to longer-term patients (90% to 94%, p-value = 0.000). We also find that there is response shift in subjective health resulting in a higher proportion of patients rating their health as good (92%) as compared to the general population (72%). A comparison of determinants of subjective health between short-term and longer-term patients shows that patients have different priorities, objectives and values between the two ART phases. In the cohort of short-term patients we find that the presence of children and recent sexual intercourse increases their subjective health. In longer-term chronic patients we find that economic and practical considerations determine their subjective health. Thus, we observe a considerable shift in the predictors of subjective health over time.
We contrast changes in subjective health with the biomedical transition using a measure of objective health. Contrary to subjective health we find a gradual process of adjustment in the CD4 count. The CD4 count of short-term antiretroviral patients is about 100 counts lower compared to long-term adherents. The transitional dynamics in the determinants of the objective measure show that in the short-term more educated individuals have lower CD4 counts. However, in the long-term, highly educated individuals have better biomarkers. Another interesting finding is that while across disease stages men and women do not differ in subjective health, females have considerably higher health biomarkers. This raises the need for gender-specific responses to HIV/AIDS.
Overall, the findings indicate that subjective and objective measures of health capture different aspects of wellbeing. The subjective health measure provides an overly optimistic indication while the objective measure underestimates the actual beneficial effects of ART (in particular at ART initiation). Nutrition is the only parameter that consistently predicts higher levels of subjective and objective health across disease stages. Thus, our research provides further evidence for integrating food support and nutritional training within the existing system of HIV care. This fact is particularly important in the current situation of funding uncertainties and competing budget priorities (Dolan & Kahneman, Citation2008; Loewenstein & Ubel, Citation2008).
The study is not free from limitations: First, the research suffers from drawbacks that are inherent to the analysis of self-reported data. The results may comprise reporting errors and biases if the participants have systematically misinterpreted scales and/or questions. To the extent possible we aimed at limiting this source of bias by carefully training our enumerators. In addition, the response ratings may vary across patients’ understandings, believes and sociocultural contexts. Since all patients are from Burkina Faso we consider the results valid for the country but it needs to be empirically verified whether our results are generalizable to other African countries. Second, patients might report good health in response to survey questions as signaling mechanism of good adherence. However, this hypothesis has shown no real effects in other chronic diseases (Parkinson) (Dolan & Kahneman, Citation2008; Skogar et al., Citation2012). Moreover, even if there is over-reporting about the quality of health, our findings would hold although the underlying mechanisms would change. Response shift would not be due to a change in the internal reference point but vis-à-vis the outside world. Third, the differences in sample sizes across short-term versus longer-term patients is likely to affect precision and comparability of our estimates. Note that the overall sample of 3625 observations is a nationally representative, random sample of PLHIV in Burkina Faso. The sample split was introduced with respect to the duration under ART and the resulting imbalance in the sample size between short-term and longer-term patients is merely a representation of the study context, i.e. patients can prolong their life substantially by adhering to ART. Importantly, both sub-samples include more than 1400 patients and are similar in the number of observations to other international surveys that are often used for micro and macro cross-country comparisons such as the Worlds Values Survey (n = 1500) and Afro-Barometer Survey (n = 1200). Therefore, we expect the estimates to be precise and the comparison to be credible.
In sum, this research highlights the variations in patients’ health outcomes and predictors across the different stages of the disease. Treating all individuals under ART in the same way, independently of how long they have been taking medication, is likely to miss out the variability in living situations and constraints of short-term versus long-term patients. Thus, the study advances our understanding of adaptation processes of PLHIV. We need to acknowledge adaptation to the disease and design health programs away from one-size-fits-all solutions to stage of disease-specific support and counseling. Incorporating adaptation processes in the design of health programs allows us to develop better tailored and ultimately more cost-efficient support strategies (Loewenstein & Ubel, Citation2008; WHO, Citation2013). In conceptualizing policies, we should focus on ameliorating treatment and resilience management by accounting for situational and context-specific factors and the possibility that these are likely to change in the course of the disease. A recent systematic review about mobile phone interventions (SMS/IVR/calls) to support PLHIV on ART in low and middle-income countries suggests that effective tools still need to be found to accompany PLHIV in the long-run (Demena, Artavia-Mora, Ouedraogo, Thiombiano, & Wagner, Citationforthcoming). The research at hand suggests that it is particularly important to diminish obstacles to ART continuation and to recognize the needs of PLHIV depending on their specific demographic, economic, social and physical characteristics, especially given that HIV is nowadays a life-long chronic condition that societies must bear. Related, additional research should examine the generalizability of the presented results for other African countries and for other life-threating diseases (i.e. Tuberculosis).
Disclosure statement
No potential conflict of interest was reported by the authors.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
Notes
1 According to WHO only 5.2% of the total Burkinabe population is obese (WHO, Citation2016). As comparison, in the United States adult obesity rates exceed 35% in five states, the lowest rate is 22.3% (SOB, Citation2017).
2 The average CD4 count is 454.3. The share of individuals with objective good health is 36.8% (CD4 count of 500 or above).
3 Note that for the sample at hand, the negative impact of the squared weight term is negligible since it is almost zero. It only affects individuals with a weight above 170 kilograms. None of the respondents weighs that much.
4 For short-term patients, income is negatively and insignificantly associated with subjective health.
5 Detailed results are omitted for the sake of brevity but available from the authors upon request.
6 Information on CD4 counts was collected directly from health facility records and is not based on patients’ self-reported recollections. Trained hospital staff provided the information. For confidentiality reasons we did not have access to the health facility records. The CD4 count is available for 66% of the patients (2,394 of 3,625) and as discussed earlier, on average, it increased from 388 among short-term patients to 490 among long-term adherents.
7 Detailed results are omitted for the sake of brevity but available from the authors upon request.
References
- Addai, I., & Adjei, J. (2014). Predictors of self-appraised health status in sub-Saharan Africa: The case of Ghana. Applied Research in Quality of Life, 9(2), 233–253. doi: 10.1007/s11482-013-9220-3
- Albrecht, G. L., & Devlieger, P. J. (1999). The disability paradox: High quality of life against all odds. Social Science & Medicine, 48(8), 977–988. doi: 10.1016/S0277-9536(98)00411-0
- Anema, A., Vogenthaler, N., Frongillo, E. A., Kadiyala, S., & Weiser, S. D. (2009). Food insecurity and HIV/AIDS: Current knowledge, gaps, and research priorities. Current HIV/AIDS Reports, 6(4), 224–231. doi: 10.1007/s11904-009-0030-z
- Auld, A. F., Shiraishi, R. W., Mbofana, F., Couto, A., Fetogang, E. B., El-Halabi, S., … Mutasa-Apollo, T. (2015). Lower levels of antiretroviral therapy enrollment among men with HIV compared with women—12 countries, 2002–2013. Morbidity and Mortality Weekly Report, 64(46), 1281–1286. doi: 10.15585/mmwr.mm6446a2
- Baranov, V., Bennett, D., & Kohler, H. P. (2015). The indirect impact of antiretroviral therapy: Mortality risk, mental health, and HIV-negative labor supply. Journal of Health Economics, 44, 195–211. doi: 10.1016/j.jhealeco.2015.07.008
- Benjamins, M. R., Hummer, R. A., Eberstein, I. W., & Nam, C. B. (2004). Self-reported health and adult mortality risk: An analysis of cause-specific mortality. Social Science & Medicine, 59(6), 1297–1306. doi: 10.1016/j.socscimed.2003.01.001
- Demena, B. A., Artavia-Mora, L., Ouedraogo, D., Thiombiano, B. A., & Wagner, N. (forthcoming). A systematic review of mobile phone interventions (SMS/IVR/calls) to improve adherence and retention to antiretroviral treatment in low and middle-income countries. AIDS Patient Care and STDs.
- Di Tella, R., MacCulloch, R. J., & Oswald, A. J. (2001). Preferences over inflation and unemployment: Evidence from surveys of happiness. American Economic Review, 91(1), 335–341. doi: 10.1257/aer.91.1.335
- Doiron, D., Fiebig, D. G., Johar, M., & Suziedelyte, A. (2015). Does self-assessed health measure health? Applied Economics, 47(2), 180–194. doi: 10.1080/00036846.2014.967382
- Dolan, P., & Kahneman, D. (2008). Interpretations of utility and their implications for the valuation of health. The Economic Journal, 118(525), 215–234. doi: 10.1111/j.1468-0297.2007.02110.x
- Fox, M. P., & Rosen, S. (2010). Patient retention in antiretroviral therapy programs up to three years on treatment in sub-Saharan Africa, 2007–2009: Systematic review. Tropical Medicine & International Health, 15, 1–15. doi: 10.1111/j.1365-3156.2010.02508.x
- Frederick, S., & Loewenstein, G. (1999). Hedonic adaptation. In D. Kahneman, E. Diener & N. Schwarz (Eds.), Well-being: The foundations of hedonic psychology (pp. 302–329). Russell Sage Foundation.
- Houtzager, L. M. (2009). Nutrition in HIV: A review. Benin Journal of Postgraduate Medicine, 11(1), doi: 10.4314/bjpm.v11i1.48829
- Jylhä, M. (2009). What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Social Science & Medicine, 69(3), 307–316. doi: 10.1016/j.socscimed.2009.05.013
- Kalichman, S. C., Carey, M. P., & Johnson, B. T. (1996). Prevention of sexually transmitted HIV infection: A meta-analytic review of the behavioral outcome literature. Annals of Behavioral Medicine, 18(1), 6–15. doi: 10.1007/BF02903934
- Koelmeyer, R., English, D. R., Smith, A., & Grierson, J. (2014). Association of social determinants of health with self-rated health among Australian gay and bisexual men living with HIV. AIDS Care, 26(1), 65–74. doi: 10.1080/09540121.2013.793273
- Koethe, J. R., Lukusa, A., Giganti, M. J., Chi, B. H., Nyirenda, C. K., Limbada, M. I., … Stringer, J. S. (2010). Association between weight gain and clinical outcomes among malnourished adults initiating antiretroviral therapy in Lusaka, Zambia. Journal of Acquired Immune Deficiency Syndromes (1999), 53(4), 507. doi: 10.1097/QAI.0b013e3181b32baf
- Kralik, D., Koch, T., Price, K., & Howard, N. (2004). Chronic illness self-management: Taking action to create order. Journal of Clinical Nursing, 13(2), 259–267. doi: 10.1046/j.1365-2702.2003.00826.x
- Loewenstein, G., & Ubel, P. A. (2008). Hedonic adaptation and the role of decision and experience utility in public policy. Journal of Public Economics, 92(8–9), 1795–1810. doi: 10.1016/j.jpubeco.2007.12.011
- Masa, R., Chowa, G., & Nyirenda, V. (2018). Socioeconomic correlates of dietary diversity and its association with adherence and psychosocial functioning of people living with HIV in rural Zambia. Nutrition and Health, 24(2), 93–102. doi: 10.1177/0260106018761282
- Neuman, M., Obermeyer, C. M., & MATCH Study Group. (2013). Experiences of stigma, discrimination, care and support among people living with HIV: A four country study. AIDS and Behavior, 17(5), 1796–1808. doi: 10.1007/s10461-013-0432-1
- Oswald, A. J., & Powdthavee, N. (2008). Does happiness adapt? A longitudinal study of disability with implications for economists and judges. Journal of Public Economics, 92(5–6), 1061–1077. doi: 10.1016/j.jpubeco.2008.01.002
- Pierret, J. (2007). An analysis over time (1990–2000) of the experiences of living with HIV. Social Science & Medicine, 65(8), 1595–1605. doi: 10.1016/j.socscimed.2007.06.017
- Postulart, D., & Adang, E. M. (2000). Response shift and adaptation in chronically III patients. Medical Decision Making, 20(2), 186–193. doi: 10.1177/0272989X0002000204
- Quinn, T. C., & Overbaugh, J. (2005). HIV/AIDS in women: An expanding epidemic. Science, 308(5728), 1582–1583. doi: 10.1126/science.1112489
- Rhodes, T., Bernays, S., & Terzić, K. J. (2009). Medical promise and the recalibration of expectation: Hope and HIV treatment engagement in a transitional setting. Social Science & Medicine, 68(6), 1050–1059. doi: 10.1016/j.socscimed.2008.12.017
- Riis, J., Loewenstein, G., Baron, J., Jepson, C., Fagerlin, A., & Ubel, P. A. (2005). Ignorance of hedonic adaptation to hemodialysis: A study using ecological momentary assessment. Journal of Experimental Psychology: General, 134(1), 3. doi: 10.1037/0096-3445.134.1.3
- Rosen, S., Fox, M. P., & Gill, C. J. (2007). Patient retention in antiretroviral therapy programs in sub-Saharan Africa: A systematic review. PLoS Medicine, 4(10), e298. doi: 10.1371/journal.pmed.0040298
- Russell, S., & Seeley, J. (2010). The transition to living with HIV as a chronic condition in rural Uganda: Working to create order and control when on antiretroviral therapy. Social Science & Medicine, 70(3), 375–382. doi: 10.1016/j.socscimed.2009.10.039
- Russell, S., Seeley, J., Ezati, E., Wamai, N., Were, W., & Bunnell, R. (2007). Coming back from the dead: Living with HIV as a chronic condition in rural Africa. Health Policy and Planning, 22(5), 344–347. doi: 10.1093/heapol/czm023
- Schwartz, C. E., Andresen, E. M., Nosek, M. A., Krahn, G. L., & RRTC Expert Panel on Health Status Measurement. (2007). Response shift theory: Important implications for measuring quality of life in people with disability. Archives of Physical Medicine and Rehabilitation, 88(4), 529–536. doi: 10.1016/j.apmr.2006.12.032
- Schwartz, C. E., & Sprangers, M. A. (1999). Methodological approaches for assessing response shift in longitudinal health-related quality-of-life research. Social Science & Medicine, 48(11), 1531–1548. doi: 10.1016/S0277-9536(99)00047-7
- Schwartz, C. E., & Sprangers, M. A. (2000). Adaptation to changing health: Response shift in quality-of-life research. American Psychological Association, doi: 10.1037/10382-000
- Sharpe, L., Butow, P., Smith, C., McConnell, D., & Clarke, S. (2005). Changes in quality of life in patients with advanced cancer: Evidence of response shift and response restriction. Journal of Psychosomatic Research, 58(6), 497–504. doi: 10.1016/j.jpsychores.2005.02.017
- Sharpe, L., & Curran, L. (2006). Understanding the process of adjustment to illness. Social Science & Medicine, 62(5), 1153–1166. doi: 10.1016/j.socscimed.2005.07.010
- Skogar, Ö, Fall, P. A., Hallgren, G., Bringer, B., Carlsson, M., Lennartsson, U., … Lökk, J. (2012). Parkinson’s disease patients’ subjective descriptions of characteristics of chronic pain, sleeping patterns and health-related quality of life. Neuropsychiatric Disease and Treatment, 8, 435. doi: 10.2147/NDT.S34882
- SOB. (2017). Adult Obesity in the United States [Internet]. The Trust for America’s Health and the Robert Wood Johnson Foundation. The State of Obesity; 2004–2018.
- Tessier, P., Blanchin, M., & Sébille, V. (2017). Does the relationship between health-related quality of life and subjective well-being change over time? An exploratory study among breast cancer patients. Social Science & Medicine, 174, 96–103. doi: 10.1016/j.socscimed.2016.12.021
- Thornton, R. L. (2012). HIV testing, subjective beliefs and economic behavior. Journal of Development Economics, 99(2), 300–313. doi: 10.1016/j.jdeveco.2012.03.001
- UNAIDS. (2012). Rapport d’activités sur la riposte au sida du Burkina Faso 2012. The Joint United Nations Programme on HIV/AIDS.
- UNAIDS-a. (2016). Rapport d’activités sur la riposte au sida du Burkina Faso 2016. The Joint United Nations Programme on HIV/AIDS.
- UNAIDS-b. (2016). Country fact sheets. The Joint United Nations Programme on HIV/AIDS.
- Wagner, N., Ouedraogo, D., Artavia-Mora, L., Bedi, A., & Thiombiano, B. A. (2016). Protocol for a randomized controlled trial evaluating mobile text messaging to promote retention and adherence to antiretroviral therapy for people living with HIV in Burkina Faso. JMIR Research Protocols, 5(3), e170. doi: 10.2196/resprot.5823
- World Bank. (2017). Burkina Faso Poverty, Vulnerability, and Income Source. Report No. 115122.
- World Health Organization. (2013). Consolidated guidelines on general HIV care and the use of antiretroviral drugs for treating and preventing HIV infection: Recommendations for a public health approach (p. 269). Geneva: World Health Organization. ISBN9789241505727
- World Health Organization. (2016). Diabetes country profiles – Burkina Faso. World Health Organization http://www.who.int/diabetes/country-profiles/bfa_en.pdf
- Wu, S. (2001). Adapting to heart conditions: A test of the hedonic treadmill. Journal of Health Economics, 20(4), 495–507. doi: 10.1016/S0167-6296(01)00084-4
- Wu, S., Wang, R., Zhao, Y., Ma, X., Wu, M., Yan, X., & He, J. (2013). The relationship between self-rated health and objective health status: A population-based study. BMC Public Health, 13(1), 320. doi: 10.1186/1471-2458-13-320
