ABSTRACT
National HIV testing policies aim to increase the proportion of people living with HIV who know their status. National HIV testing policies were reviewed for each country from 2013 to 2018, and compared with WHO guidance. Three rounds of health facility surveys were conducted to assess facility level policy implementation in Karonga (Malawi), uMkhanyakude (South Africa), and Ifakara (Tanzania). A policy ‘implementation’ score was developed and applied to each facility by site for each round. Most HIV testing policies were explicit and aligned with WHO recommendations. Policies about service coverage, access, and quality of care were implemented in >80% of facilities per site and per round. However, linkage to care and the provision of outreach HIV testing for key populations were poorly implemented. The proportion of facilities reporting HIV test kit stock-outs in the past year reduced over the study period in all sites, but still occurred in ≥17% of facilities per site by 2017. The implementation score improved over time in Karonga and Ifakara and declined slightly in uMkhanyakude. Efforts are needed to address HIV test kit stock-outs and to improve linkage to care among people testing positive in order to reach the 90-90-90 targets.
Introduction
Over the past two decades national governments in sub-Saharan Africa (SSA) have rapidly scaled up of HIV testing and treatment services in a bid to reduce HIV-related mortality and bring the epidemic under control (Murray et al., Citation2014; Reiniers et al., Citation2017; Slaymaker et al., Citation2014; UNAIDS, Citation2017a). Efforts have accelerated since 2016, partly driven by the 2015 UNAIDS ‘90-90-90’ targets, where the first ‘90’ aim for 90% of people living with HIV (PLHIV) knowing their status by 2020 (UNAIDS, Citation2014). By 2017, estimates showed that more than two-thirds of the 36.9 million PLHIV in the region were aware of their HIV status (UNAIDS, Citation2018), although recent surveys suggest that there is substantial variation across countries (Ministry of Health of Lesotho, Citation2017; Ministry of Health of Malawi, Citation2017; Ministry of Health of Swaziland, Citation2017; Ministry of Health of Zambia, Citation2016; MoHCC, Citation2016; MoHCGEC, Citation2017b). In South Africa, where 21% of adults (aged 15–49 years) are HIV-positive, the first 90 target had almost been reached by 2017 (UNAIDS, Citation2018). However, in other countries, including Tanzania and Malawi, where 4.5% and 9.6% of the adult population are HIV-positive, progress has lagged further behind with 61% and 73% of adult PLHIV knowing their HIV status respectively by 2017 (Ministry of Health of Malawi, Citation2017; MoHCGEC, Citation2017b).
HIV testing approaches have evolved over the past 15 years, initially with a view to scaling up access to HIV services for the general population, and more recently with the aim of diagnosing PLHIV who are not aware of their HIV status (WHO, Citation2007, Citation2017b). During the early response to the HIV epidemic, stand-alone Voluntary Counselling and Testing (VCT) clinics were established in many settings. This was followed by the roll-out of Provider-Initiated Testing and Counselling (PITC) in many settings, following recommendations by the World Health Organisation (WHO) in 2007, in a bid to increase HIV diagnosis rates among pregnant women and those with signs and symptoms of HIV (WHO, Citation2007). By 2004, WHO endorsed non-laboratory rapid HIV tests and algorithms (WHO, Citation2004). The introduction of rapid tests enabled different HIV testing approaches to be introduced outside of health facilities, including through mobile clinics and home-based testing (Belza et al., Citation2015; Iwuji et al., Citation2016). More recently, HIV self-testing policies have been adopted in many settings with a view to increase diagnosis rates among populations who are less likely to present at health facilities (UNITAID, Citation2018; WHO, Citation2017a). Nevertheless, despite an increasing number of HIV testing modalities, the majority of HIV tests are conducted within health facilities, with PITC still representing the most common testing approach in most countries (Balogun & Owoaje, Citation2016; Mwenge et al., Citation2017).
As the number of people testing for HIV has increased (Kharsany et al., Citation2015; UNAIDS, Citation2016, Citation2017b), several health systems challenges have been observed including insufficient human resources, problems with consistent supply chain management and a lack of quality assurance mechanisms (IMF, Citation2004; Roura et al., Citation2013). Implementation challenges such as staff shortage, high workloads and lack of supplies, in the context of changing guidelines from WHO, may hamper the quality of HIV testing services and the accuracy of the test results (Bott et al., Citation2015). Poorly implemented HIV testing services can impact on patients’ experiences and have knock on effects for retention among those who are diagnosed with HIV (Wringe, Moshabela, et al., Citation2017). Despite these concerns, there have been few studies that have investigated the extent to which health facilities in rural African settings have been able to keep pace with changing HIV testing policies. This study addresses this gap by assessing the implementation of HIV testing and counselling policies in rural health facilities in Malawi, South Africa and Tanzania over the period 2013–2018.
Materials and methods
The data for this study are drawn from the study for ‘Strengthening Health systems for the Application of Policy to Enable Universal Test and Treat’ (SHAPE-UTT), which aimed to assess the policy implementation and health systems impacts of Universal test and treat (UTT). The study included policy reviews and surveys that were undertaken in health facilities serving the populations of rural Health and Demographic Surveillance System (HDSS) sites in Malawi (Karonga), South Africa (uMkhanyakude) and Tanzania (Ifakara) ().
Table 1. HDSS study sites characteristics and timing of the facility survey.
Conceptual framework
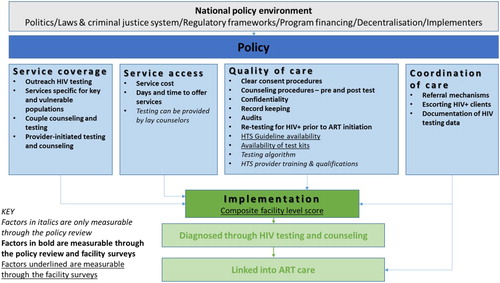
This analysis draws on a conceptual framework initially developed by Church et al. (Citation2017) that identified HIV policy and health service factors across five domains which influence mortality among PLHIV in sub-Saharan settings. The development of the framework has been described in detail elsewhere (Church et al., Citation2017), however in brief it involved a comprehensive review of published literature and policy documents, and consultation with 28 HIV researchers and practitioners. Our modified framework () focuses on the policy and health service factors relating to HIV testing which expand upon the three of the original domains as described by Church et al. (Citation2017) to now include (1) service coverage (2) access, (3) quality of care, and (4) linkage to care among those who test positive. Our refinement of the original domains; namely by separating service coverage from access allows us to better present the implementation of policies related to these related yet distinct concepts.
Policy review
A review of WHO guidance and national HIV policies on HIV testing was conducted in 2013 (Church et al., Citation2017), and updated for the period 2013–2017. Documents containing information on HIV testing were retrieved online or in person, and included HIV testing and counselling guidelines, policy documents, HIV clinical management guidelines, national strategic plans, training manuals and national guidelines for home-based care. A total of 46 policy documents published between 2004 and 2017 were reviewed.
An Excel-based extraction tool was used to summarise the data from the policy review, including the title of the policy document, year of policy adoption, content of the policy, and additional information regarding whether the policy content related to the selected indicators was explicit (stated clearly and in detail, providing details of how implementation should take place), not explicit (there is some mention but no prescriptive detail to guide implementation is provided) or not mentioned (not stated at all in the policy documents).
Facility survey
In each country, three survey rounds were conducted in all of the health facilities serving the populations of the three HDSS sites (): round one (R1) in 2013–2015, round two (R2) in 2015–2016, and round three (R3) in 2017–2018. Throughout the paper we use the HDSS name to describe the data collected at the facility level.
The facility survey questionnaire included modules on the delivery of HIV testing and counselling services, antenatal care (ANC) services, and antiretroviral therapy (ART) services, as described elsewhere (Church et al., Citation2017). The questionnaires were administered in English to the person in charge at the health facility. In addition, registers, log books, pharmacy records and quarterly reports were reviewed to document HIV testing episodes and HIV test kit stock-outs. The availability of guidelines was verified by the interviewer. Data were entered into MS SQL Server (Microsoft Corp, Redmond, U.S.A.), and subsequently cleaned and exported for analysis using STATA 13 (Stata Corp). Descriptive statistics were used to show the proportion of facilities implementing each policy, by survey round and site. HIV test kit stock-outs were recorded for the previous year.
Facility level Implementation analysis
In order to assess the extent to which national HIV policies were implemented in each HDSS site in the countries, we compared the proportion of health facilities within each site implementing each policy. Implementation was classified as good if >70% of facilities implemented the policy; moderate if between 30% and 70% of the facilities implemented the policy, and poor if <30% of facilities implemented the policy.
Facility-level HIV testing policy implementation score
An implementation score was calculated for each facility across the four HIV testing services (HTS) domains (coverage; access; quality; and linkage to care) using the 20 indicators listed in . Each indicator was scored 0 if the policy was not implemented in the facility, and 1 if it was reported as being implemented. Scores within each domain were then summed and divided by the total number of indicators within that domain so that the maximum score within a domain that the facility could attain was 1. An overall facility HTS score was then calculated by summing the four domain level scores in each facility. The maximum score a facility could attain was 4, with scores closest to 4 indicating closest alignment to national HTS guidelines.
Table 2. Indicators and coding structure used to construct the composite implementation score.
Ethical approval
Ethical approval was obtained from the Internal Review Boards of the Ifakara Health Institute and National Institute for Medical Research for Tanzania (#2579), National Health Science Research Committee for Malawi (#1861), the Biomedical Research Ethics Committee for South Africa (BREC REF: BE400/14) and from the London School of Hygiene and Tropical Medicine (#13536-1).
Results
Changes in numbers of HIV testing episodes
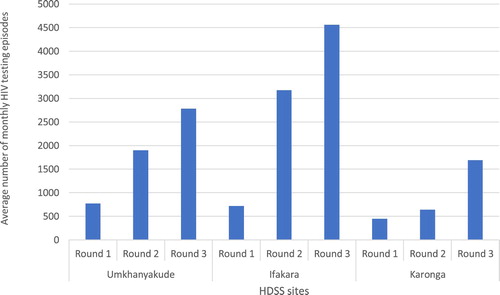
In R1, the average number of tests per site conducted per month was similar across the sites, ranging from 445 in Karonga to 772 in uMkhanyakude. The average number of HIV tests conducted per site increased over the three rounds, by a factor of 6, 3.8 and 3.6 in Ifakara, Karonga, and uMkhanyakude respectively ().
Assessment of the service coverage, access, quality and linkage into care
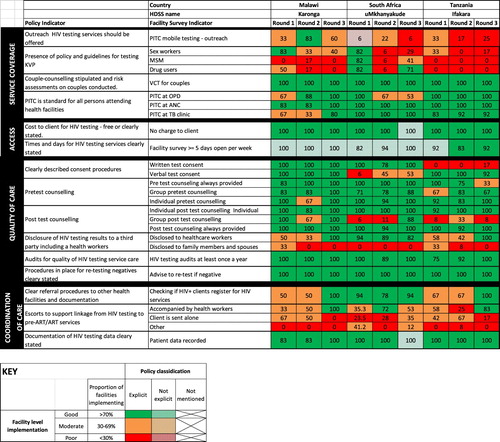
Across all four HIV testing components, policies relating to the associated indicators were generally explicitly stated (). However, while the proportion of facilities implementing policies relating to access and quality of care indicators was high, implementation of policies that influence HIV testing coverage and linkage to care indicators was more varied.
Service coverage
In all three countries, policies relating to the provision of outreach services (with the exception of South Africa in R1); testing services targeted to key and vulnerable populations (KVP); VCT for couples; and PITC were explicit. In uMkhanyakude (South Africa) and Ifakara (Tanzania) implementation of outreach services was poor across all three survey rounds, whereas in Karonga (Malawi) implementation of outreach was moderate in R1 and R3, and good in R2. In uMkhanyakude, there was good implementation of testing services for KVPs in R1, poor in R2 and varied depending on the KVP in R3, with good implementation of testing for drug users, moderate for MSM and poor for sex workers. In Karonga and Ifakara, implementation of testing for KVPs was moderate or poor throughout with the exception of testing for Sex workers in Karonga in R1. A high proportion of facilities implemented VCT for couples and PITC services at outpatient department (OPD), ANC and TB clinics, with the exception of OPD in uMkhanyakude which was moderately implemented in R1 and R2.
Access
Explicit policies on the provision of free HIV tests existed in all three countries, and it was well implemented in each HDSS site and across all survey rounds. There was no explicit policy on the number of days per week that health facilities offered HIV tests in Malawi and South Africa. However, in Tanzania, policy stated that facilities should provide HTS at least five days a week by 2015. In practice, almost all health facilities in all three sites offered HTS at least five days a week. Trained lay counsellors were allowed to perform HTS in South Africa and Malawi over the study period, whereas this policy was introduced in Tanzania in 2013 ().
Table 3. Changes in the personnel who are able to conduct HIV tests by country and round.
Quality of care
Quality of care relates to pre-testing, testing as well as post-test referral. Policies on consent procedures, pre- and post-test counselling, and frequency of facility audits were explicit in each country over all three rounds. A high proportion of facilities reported obtaining patient consent over all three rounds. Overall pre-and post-test counselling was implemented in the majority of facilities, however the modality of implementation varied. With some exceptions pre-test counselling was provided both at the individual and group level, for post-test counselling most facilities offered individual counselling only. The exceptions included moderate implementation of pre-test counselling in R3 and group pre-test counselling in R2 in Ifakara, moderate implementation of individual pre-test counselling in Karonga in R2. In each country, policy stated that counselling could be conducted individually or in groups. At the facility level in each country and in each round, individual level counselling (especially post-test) was more commonly offered. Policy guidance on the registration and referral of patients who test positive and documenting patient information were explicitly stated in all countries and across all survey rounds (with the exception of documenting patient information in South Africa in R3). The proportion of facilities undertaking annual audits ranged from 75% in R1 in uMkhanyakude (South Africa) to 100% in all sites, aligning with each country’s policy. Policies on repeat testing for those who were HIV negative, depending on their risk assessment and for pregnant women in third trimester, were explicit and well implemented in all facilities and across all survey rounds.
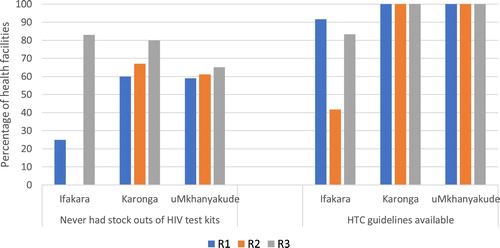
More than 50% of the health facilities in Karonga (Malawi) and uMkhanyakude (South Africa) experienced no stock outs of HIV test kits in the 12 months prior to interview in all rounds (). However, all health facilities in Ifakara (Tanzania) experienced at least one stock out episode in R2. HIV testing guidelines were available in all facilities in Karonga and uMkhanyakude in all rounds (). In Ifakara, only 42% of facilities had the latest guidelines available in R2.
WHO guidance on HIV testing had recommended a serial HIV testing algorithm in high prevalence settings (WHO, Citation2012). National policy in Tanzania and South Africa adopted a serial testing approach (Ministry of Health and Social Welfare of Tanzania, Citation2013; MoHCGEC, Citation2017a; NACP, Citation2015; National Department of Health of South Africa, Citation2009, Citation2015b, Citation2016; South African National AIDS council, Citation2010) whereby clients undergo a second test if the first one is HIV-positive. In the event of discordant results, the test is repeated, preferably by a different HTC provider. If still discordant, the client is advised to return after 2–4 weeks to re-test. In Malawi, a parallel testing approach was adopted when a serial approach gave discordant results () (Government of Malawi, Citation2013; Ministry of Health of Malawi, Citation2016a). In Malawi and South Africa, during the study period, a person with discordant HIV test results could undergo four HIV tests before HIV status confirmation. More than 75% of facilities in all rounds and sites reported to have conducted quality of care audits at least once a year.
Table 4. Changes in HIV testing algorithms.
In 2015, WHO (WHO, Citation2015) recommended retesting all individuals diagnosed with HIV to verify their HIV status prior to initiating ART. This policy was adopted for pregnant women in South Africa in 2015 (National Department of Health of South Africa, Citation2015a) and everyone who was diagnosed HIV positive in Malawi since 2016 (Ministry of Health of Malawi, Citation2016b) but had not been adopted in Tanzania for any HIV diagnosed persons by the end of the study period.
In 2015, WHO first released guidance on the kind of providers required for different HIV testing services (WHO, Citation2015). For facility-based services, WHO recommended trained healthcare workers and trained lay providers to perform HIV testing. In the context of the three countries involved in this study, minimum qualifications of HTS providers differed to a small degree (). For Tanzania and Malawi, no change was observed over the three rounds. For South Africa, the minimum qualifications were not clear in R1 but became clear in R2 with no change in R3. In Malawi in R1 there was no guidance for HTS refresher trainings, in R2 and R3 policy clearly stated it should be conducted every two years. In South Africa, guidance on refresher training was not stated in R1 but was clear in other rounds, every 3 years in R2 and every 2 years in R3. For Tanzania, guidance stated training should be conducted at least once a year over all the rounds.
Table 5. Policy changes in the qualification and training for HIV testing and counselling personnel by country and round.
Linkage to care
In uMkhanyakude, the policy of checking that HIV positive patients register for care and treatment services was well implemented across all three survey rounds, whereas in Karonga and Ifakara implementation improved over time. Policies stating that health workers should escort those who test HIV positive to required services was explicit in all countries, yet was moderately practiced in R1 and R2 in Karonga, R1 and R3 in uMkhanyakude and R1 in Ifakara. However, implementation was high by R3 in Karonga and Ifakara, and in R2 in uMkhanyakude.
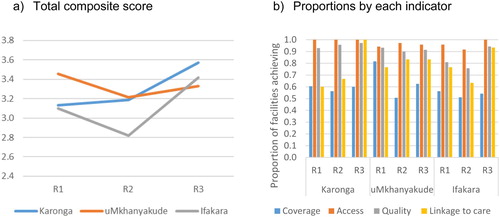
Facility level HIV testing policy implementation score
Overall the HIV testing policy implementation score improved over each successive time frame in Karonga ((a)). In uMkhanyakude the score improved between R2 and R3, but both scores were still lower than the R1 score. In Ifakara the score decreased in R2 then increased to its highest level in R3 ((a)). Notable improvements were made in linkage to care in Karonga, and in quality and linkage to care in Ifakara. In uMkhanyakude the lower implementation score in R2 and R3 were mostly likely caused by declines in coverage ((b)) (which was also the most poorly implemented indicator), notably outreach and targeted service provision to KVP.
Discussion
Our study has illustrated that in the context of increasing testing numbers in all countries, facilities within three HDSS in Tanzania, Malawi and South Africa are responding well in terms of implementing changing HIV testing policies. The proportion of facilities reporting stock outs of HIV test kits reduced over the rounds in each site, but still occurred in round 3.
Across all three countries, the majority of national HIV testing policies were explicit throughout the study period, and aligned with WHO guidance. Policies pertaining to service access and quality of care were well implemented at the facility level in all three sites, although gaps were observed in relation to implementing mobile testing, testing services for key and vulnerable populations, and linkage to care and treatment for people diagnosed with HIV. These implementation gaps reduced over time in facilities in Karonga and Ifakara, but increased in facilities of uMkhanyakude, the reason for the decrease was due to the poorer implementation of the coverage indicators over time. Overall however, the implementation of HIV testing policies remained high and improved over the rounds, as demonstrated by the facility level HIV testing implementation score which improved over the rounds with a slight decline in uMkhanyakude. Additional facility level research is needed to explore the reasons for the decline in coverage for KVP testing in uMkhanyakude.
The UNAIDS 90-90-90 targets are central to current efforts to eliminate AIDS (UNAIDS, Citation2017a). Whilst the first 90 aims for 90% of infected individuals to know their status, each individual may undergo multiple tests at each testing time point. Furthermore, we know that many patients undergo repeat HIV tests – even after receiving an HIV positive diagnosis – as a process to trust the results and reach an acceptance of their status (Horter et al., Citation2017; Wringe, Renju, et al., Citation2017). From a health systems perspective, specifically in terms of the supply of test kits and provider time, the actual number of tests conducted rather than the number of individuals testing dictates part of the burden on the service (Baryamutuma et al., Citation2017; Chan et al., Citation2014; Church et al., Citation2017; Nyogea et al., Citation2015). Our study therefore focused on testing episodes, rather than the number of individuals who undergo testing.
We found that not less than 15% of all facilities in all settings and across all rounds continued to experience stock outs of HIV test kits, in line with findings from other countries in the region (Baryamutuma et al., Citation2017; Chan et al., Citation2014; Church et al., Citation2017). Whilst fewer stock outs are being reported over time in our three sites, these supply chain issues still represent a challenge that could lead to missed opportunities for diagnosing people living with HIV. Whilst earlier we discussed how some people re-test as part of their process to accept their status, in other situation re-testing is taking place due to a lack of continuity of care from testing through to treatment initiation. Efforts are needed to not only ensure a more consistent supply of test kits at all facilities but also to focus on reducing any unnecessary re-testing caused by inadequate linkage to care.
The second of the UNAIDS 90’s refers to linkage to care and starting ART. Multiple studies have shown significant challenges in reaching this target (Asiimwe et al., Citation2017; Church et al., Citation2017; d’Elbée et al., Citation2018; Iwuji et al., Citation2016; Phillips et al., Citation2018; Reddy et al., Citation2016; Sanga et al., Citation2017). Findings from recent large scale community randomised trials for UTT (including PopART and TasP), continue to emphasise the importance of linkage to care in efforts to reduce onward HIV infection and AIDS mortality (Farouki et al., Citation2016; Iwuji et al., Citation2018). The additional efforts in the PopART trial, to accompany newly diagnosed HIV patients to ART clinics likely led to their achievement of the second 90 (National Institutes of Health, Citation2019). In this study, we found that implementation of linkage to care policies improved over time in facilities in Karonga and Ifakara (reaching 100% facilities in Karonga and 83% of facilities in Ifakara by round 3) but remained weakly implemented in facilities in uMkhanyakude. Only half of the facilities in uMkhanyakude reported accompanying the newly diagnosed clients to ART services by round 3. Efforts to ensure that diagnosed patients are linked to care are vital in order to reach the second 90 target.
In this study, we found that explicit policies to reach KVP with HIV testing services had been adopted in the three study countries, but implementation of these policies was poor, particularly in Ifakara in all three rounds. All three HDSS are situated in rural settings and possibly do not serve large numbers of KVPs in their catchment areas compared to urban areas. However further analysis of this effect was not possible given our small and non-random sample of facilities. It is also possible that outreach programmes and community-based approaches existed to provide HTS for KVPs, with the data not recorded by the health facilities (Ndori-Mharadze, Citation2017; Ubuguyu et al., Citation2016). It is also likely that policies for the provision of services for KVPs were weakly implemented in these rural settings because this population were not considered to be sufficiently concentrated in these settings, or were not aligned with some increasingly prohibitive standpoints pertaining to homosexuality (REUTERS, Citation2017).
Strengths and limitations
Our study is strengthened by its unique longitudinal perspective coupled with the detailed case study design in a sample of facilities which provided an opportunity to capture the continuum from policy to practice over the period from 2013 to 2017; a period marked by several changes in testing and treatment guidance from WHO. However, our study has various limitations that should be considered when interpreting the findings. Firstly, the study only focuses on facility-based HIV testing, while there is an increasingly strong focus being placed on comprehensive community-based models (Iwuji et al., Citation2018). Secondly the facilities in this study are few and are all situated within rural populations with HDSS which prohibited any statistical analysis of trends over time and assumptions that the results are nationally representative. Whilst the health seeking behaviour of residents of the HDSS may be different to those in the general population (Slaymaker et al., Citation2014), the services offered within these government-run facilities are typical of those offered across the country. Thirdly, the study is subject to potential reporting bias through the completion of the survey by facility managers; meaning the results may illustrate what they think should be done rather than what they are routinely doing for every client. Furthermore, although the same questionnaire was used across the rounds, different personnel administered and completed the survey, potentially further compounding reporting biases. However, our application of a composite measure of multiple indicators aimed to provide a more holistic measure of policy implementation and could minimise the effect of reporting biases in individual indicators. Fourthly, this study established if a policy was implemented, but not to what extent. For instance, PITC for ANC attendants was implemented, but we did not look into the coverage among pregnant women. To reach the 90-90-90 goals the policies need not only to be implemented, but reach the majority of patients seen in health facilities. Finally, in this study we chose to stratify implementation as good, moderate or poor, to aid the description of the results and illustrate the various nuances of facility level implementation and to account for some of the aforementioned study limitations (e.g. small sample size, social-desirability bias, respondent characteristics and changes over time). However one could also say that anything below 100% implementation is sub-optimal. Despite these limitations, this study provides a detailed picture of the implementation of HIV testing policies at a time of rapid HIV policy evolution, in three countries with generalised HIV epidemics.
Conclusion
Country policies have evolved to get more people to test for HIV, and health facilities are coping well with implementation and generally adhere to guidelines promoting good quality services. However, to reach the first 90 and consequently the second and third 90, continued efforts are needed to ensure KVPs and others who do not know their status have access to HIV testing services. Increasing the demand and uptake of facility based testing will reach those who attend facilities, however increased out of facility testing options, e.g. mobile testing, work/public testing sites, self-testing options continue to be important to increase testing coverage. Finally strong systems are needed to ensure those who test positive are effectively linked to care and adequately supported to initiate treatment so as to achieve the 2nd and 3rd ‘90’ and reduce ongoing transmission.
Acknowledgements
This work was supported by the Medical Research Council, through a Health Systems Research Initiative grant [grant number MR/ P014313/1]. JR receives funding support from DELTA/THRIVE under DEL15-011/07742/Z/15/Z.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Asiimwe, S., Ross, J. M., Arinaitwe, A., Tumusiime, O., Turyamureeba, B., Roberts, D. A., O’Malley, G., & Barnabas, R. V. (2017). Expanding HIV testing and linkage to care in southwestern Uganda with community health extension workers. Journal of the International AIDS Society, 20. https://doi.org/10.7448/IAS.20.5.21633
- Balogun, F. M., & Owoaje, E. T. (2016). Perception about the “opt out strategy” for HIV testing and counselling among pregnant women attending antenatal clinic in Ibadan, Nigeria. Journal of Community Medicine and Primary Health Care, 28(1), 45–51.
- Baryamutuma, R., Kansiime, E., Nuwagaba, C. K., Nabitaka, L., Muhumuza, S., Akello, E., Musinguzi, J., Bazeyo, W., Celentano, J., & Lindan, C. (2017). An early assessment of Uganda’s roll-out of option B+: Service capacity and infant outcomes. East African Journal of Applied Health Monitoring and Evaluation, 1, 16–21.
- Belza, M. J., Hoyos, J., Balbuena, S. F., Diaz, A., Bravo, M. J., la de Fuente, L., Oliva, J., Ruiz, M., Rosales-Statkus, M. E., Gutiérrez, J., Sánchez, R., & Álvarez, J. (2015). Assessment of an outreach street-based HIV rapid testing programme as a stradegy to promote early diagnosis: A comparison with two surveillance systems in Spain, 2008–2011. Eurosurveillance, 20(14), 1–11. https://doi.org/10.2807/1560-7917.es2015.20.14.21089.
- Bott, S., Neuman, M., Helleringer, S., Desclaux, A., Asmar, K. E., & Obermeyer, C. M. (2015). Rewards and challenges of providing HIV testing and counselling services: Health worker perspectives from Burkina Faso, Kenya and Uganda. Health Policy and Planning, 30(8), 964–975. https://doi.org/10.1093/heapol/czu100
- Chan, A. K., Ford, D., Namata, H., Muzambi, M., Nkhata, M. J., Abongomera, G., Mambule, I., South, A., Revill, P., Grundy, C., Mabugu, T., Chiwaula, L., Cataldo, F., Hakim, J., Seeley, J., Kityo, C., Reid, A., Katabira, E., Sodhi, S., … The Lablite Team (2014). The Lablite project: A cross-sectional mapping survey of decentralized HIV service provision in Malawi, Uganda and Zimbabwe. BMC Health Services Research, 14(1), 352. https://doi.org/10.1186/1472-6963-14-352
- Church, K., Machiyama, K., Todd, J., Njamwea, B., Mwangome, M., Hosegood, V., Michel, J., Oti, S., Nyamukapa, C., Crampin, A., Amek, N., Nakigozi, G., Michael, D., Gómez-Olivé, F. X., Nakiyingi-Miiro, J., Zaba, B., & Wringe, A. (2017). Identifying gaps in HIV service delivery across the diagnosis-to-treatment cascade: Findings from health facility surveys in six sub-Saharan countries. Journal of the International AIDS Society, 20(1). https://doi.org/10.7448/IAS.20.1.21188
- d’Elbée, M., Indravudh, P. P., Mwenge, L., Kumwenda, M. M., Simwinga, M., Choko, A. T., Hensen, B., Neuman, M., Ong, J. J., Sibanda, E. L., Johnson, C. C., Hatzold, K., Cowan, F. M., Ayles, H., Corbett, E. L., & Terris-Prestholt, F. (2018). Preferences for linkage to HIV care services following a reactive self-test: Discrete choice experiments in Malawi and Zambia. AIDS, 32(14), 2043–2049. https://doi.org/10.1097/QAD.0000000000001918
- Department of Health of South Africa. (2010). National HIV counselling and tetsting policy guideline.
- Farouki, K. E., Iwuji, C., Okesola, N., & Orne-gliemann, J. (2016). Access to HIV care in the context of universal test and treat: Challenges within the ANRS 12249 TasP cluster-randomized trial in rural South Africa. Journal of the International AIDS Society, 1–12. https://doi.org/10.7448/IAS.19.1.20913
- Government of Malawi. (2013). Malawi comprehensive HIV testing and counselling training: Participant handbook.
- Horter, S., Thabede, Z., Dlamini, V., Bernays, S., Stringer, B., Mazibuko, S., Dube, L., Rusch, B., & Jobanputra, K. (2017). “Life is so easy on ART, once you accept it”: Acceptance, denial and linkage to HIV care in Shiselweni, Swaziland. Social Science and Medicine, 176, 52–59. https://doi.org/10.1016/j.socscimed.2017.01.006
- IMF. (2004). The macroeconomics of HIV/AIDS. https://www.imf.org/external/pubs/ft/AIDS/eng/
- Iwuji, C. C., Orne-Gliemann, J., Larmarange, J., Balestre, E., Thiebaut, R., Tanser, F., Okesola, N., Makowa, T., Dreyer, J., Herbst, K., McGrath, N., Bärnighausen, T., Boyer, S., De Oliveira, T., Rekacewicz, C., Bazin, B., Newell, M. L., Pillay, D., Dabis, F., … Hontelez, J. (2018). Universal test and treat and the HIV epidemic in rural South Africa: A phase 4, open-label, community cluster randomised trial. The Lancet HIV, 5(3), e116–e125. https://doi.org/10.1016/S2352-3018(17)30205-9
- Iwuji, C. C., Orne-Gliemann, J., Larmarange, J., Okesola, N., Tanser, F., Thiebaut, R., Rekacewicz, C., Newell, M.-L., Dabis, F., & ANRS 12249 TasP trial group (2016). Uptake of home-based HIV testing, linkage to care, and community attitudes about ART in rural KwaZulu-Natal, South Africa: Descriptive results from the first phase of the ANRS 12249 TasP cluster-randomised trial. PLOS Medicine, 13(8). https://doi.org/10.1371/journal.pmed.1002107
- Kharsany, A., Frohlich, J., Yende-Zuma, N., Mahlase, G., Samsunder, N., Dellar, R., Zuma-Mkhonza, M., Karim, S., & Karim, Q. (2015). Trends in HIV prevalence in pregnant women in rural South Africa. Journal of Acquired Immune Deficiency Syndromes, 70(3), 289–295. https://doi.org/10.1097/QAI.0000000000000761.Trends doi: 10.1097/QAI.0000000000000761
- Ministry of Health and Social Welfare of Tanzania. (2013). National comprehensive guidelines for HIV testing and counselling.
- Ministry of Health Malawi. (2009). Guideline for HIV testing and counsellling.
- Ministry of Health of Lesotho. (2017). Lesotho population-based HIV impact assessment (issue November 2017).
- Ministry of Health of Malawi. (2016a). Malawi guidelines for clinical management of HIV in children and adults.
- Ministry of Health of Malawi. (2016b). Malawi HIV testing services guidelines.
- Ministry of Health of Malawi. (2017). Malawi population-based HIV impact assessment 2015–2016.
- Ministry of Health of Swaziland. (2017). Swaziland HIV incidence measurement survey 2: A population-based HIV impact assessment. http://phia.icap.columbia.edu/wp-content/uploads/2017/11/Swaziland_new.v8.pdf
- Ministry of Health of Zambia. (2016). Zambia population-based HIV impact assessment.
- MoHCC. (2016). Zimbabwe population-based HIV impact assessment. https://doi.org/10.2166/wrd.2014.061
- MoHCGEC. (2017a). National guidelines for the management of HIV and AIDS (6th ed.).
- MoHCGEC. (2017b). Tanzania HIV impact survey 2016–2017.
- Murray, C., Ortblad, K., Guinovart, C., Lim, S., & Al, E. (2014). Global, regional, and national incidence and mortality for HIV, tuberculosis, and malaria during 1990–2013: A systematic analysis for the global burden of disease study 2013. Lancet. https://doi.org/10.1016/S0140-6736(14)60844-8
- Mwenge, L., Sande, L., Mangenah, C., Ahmed, N., Kanema, S., D’Elbée, M., Sibanda, E., Kalua, T., Ncube, G., Johnson, C. C., Hatzold, K., Cowan, F. M., Corbett, E. L., Ayles, H., Maheswaran, H., & Terris-Prestholt, F. (2017). Costs of facility-based HIV testing in Malawi, Zambia and Zimbabwe. PLoS ONE, 12(10), 1–16. https://doi.org/10.1371/journal.pone.0185740
- NACP. (2015). National guidelines for the management of HIV and AIDS (5th ed.).
- National AIDS Control Programme. (2010). National guidelines for home based care services.
- National Department of Health of South Africa. (2009). Policy guideline for HIV counselling and testing.
- National Department of Health of South Africa. (2015a). National consolidated guidelines for the prevention of mother-to-child transmission of HIV (PMTCT) and the management of HIV in children, adolescents and adults. www.doh.gov.za.
- National Department of Health of South Africa. (2015b). National HIV counselling and testing policy guidelines.
- National Department of Health of South Africa. (2016). National HIV testing services: Policy.
- National Institutes of Health. (2019). HIV prevention study finds universal “test and treat” approach can reduce new infections. https://www.nih.gov/news-events/news-releases/hiv-prevention-study-finds-universal-test-treat-approach-can-reduce-new-infections
- Ndori-Mharadze, T. (2017). Differentiated prevention and HIV testing for female sex workers, Zimbabwe. www.ceshhar.co.zw.
- Nyogea, D. S., Said, H., Mwaigomole, G., Stoeckle, M., Felger, I., Hatz, C., Henning, L., Franzeck, F., Letang, E., Geubbels, E., & Tanner, M. (2015). An assessment of the supply chain management for HIV/AIDS care and treatment in Kilombero and Ulanga districts in southern Tanzania. Tanzania Journal of Health Research, 17(2), 1–9. https://doi.org/10.4314/thrb.v17i2.2
- Phillips, T. K., Clouse, K., Zerbe, A., Orrell, C., Abrams, E. J., & Myer, L. (2018). Linkage to care, mobility and retention of HIV-positive postpartum women in antiretroviral therapy services in South Africa. Journal of the International AIDS Society, 21, e25114. https://doi.org/10.1002/jia2.25114
- Reddy, E. A., Agala, C. B., Maro, V. P., Ostermann, J., Pence, B. W., Itemba, D. K., Safley, D., Yao, J., Thielman, N. M., & Whetten, K. (2016). Test site predicts HIV care linkage and antiretroviral therapy initiation: A prospective 3.5 year cohort study of HIV-positive testers in northern Tanzania. BMC Infectious Diseases, 16(1). https://doi.org/10.1186/s12879-016-1804-8
- Reiniers, G., Blom, S., Calvert, C., Martin-Onraet, A., Herbst, A., Eaton, J., Bor, J., Slaymaker, E., Li, Z., Clark, S., Bärnighausen, T., Zaba, B., & Hosegood, V. (2017). The burden of HIV mortality following the rollout of antiretroviral therapy: Evidence from an observational community cohort study in KwaZulu-Natal, South Africa. The Lancet HIV. https://doi.org/10.1016/S2352-3018(16)30225-9
- REUTERS. (2017). Tanzania threatens crackdown on LGBT advocates – Reuters. https://uk.reuters.com/article/uk-tanzania-lgbt-idUKKBN19H1OD?il=0
- Roura, M., Watson-Jones, D., Kahawita, T. M., Ferguson, L., & Ross, D. A. (2013). Provider-initiated testing and counselling programmes in sub-Saharan Africa: A systematic review of their operational implementation. AIDS, 27(4), 617–626. https://doi.org/10.1097/QAD.0b013e32835b7048
- Sanga, E. S., Lerebo, W., Mushi, A. K., Clowes, P., Olomi, W., Maboko, L., & Zarowsky, C. (2017). Linkage into care among newly diagnosed HIV-positive individuals tested through outreach and facility-based HIV testing models in Mbeya, Tanzania: A prospective mixed-method cohort study. BMJ Open, 7(4). https://doi.org/10.1136/bmjopen-2016-013733
- Slaymaker, E., Todd, J., Marston, M., Calvert, C., Michael, D., Nakiyingi-Miiro, J., Crampin, A., Lutalo, T., Herbst, K., & Zaba, B. (2014). How have ART treatment programmes changed the patterns of excess mortality in people living with HIV? Estimates from four countries in East and Southern Africa. Global Health Action, 7. https://doi.org/10.3402/gha.v7.22789
- South African National AIDS Council. (2010). The national HIV counselling and testing campaign strategy.
- Ubuguyu, O., Tran, C. O., Bruce, D., Masao, F., Nyandindi, C., Sabuni, N., McCurdy, S., Mbwambo, J., & Lambdin, H. B. (2016). Improvements in Health-related quality of life among methadone maintenance clients in Dar es Salaam, Tanzania. International Journal of Drug Policy, 5(6), 1–8. https://doi.org/10.4172/2157-7633.1000305
- UNAIDS. (2014). 90-90-90: An ambitious treatment target to help end the AIDS epidemic.
- UNAIDS. (2016). 90-90-90: On the right track towards the global target. https://doi.org/10.4102/phcfm.v7i1.883
- UNAIDS. (2017a). 90-90-90 – an ambitious treatment target to help end the AIDS epidemic. http://www.unaids.org/en/resources/documents/2017/90-90-90
- UNAIDS. (2017b). Ending AIDS: Progress towards the 90-90-90 targets. https://www.unaids.org/en/resources/documents/2017/20170720_Global_AIDS_update_2017
- UNAIDS. (2018). UNAIDS data 2018. https://www.unaids.org/en/resources/documents/2018/unaids-data-2018
- UNITAID. (2018). HIV rapid diagnostic tests for self-testing.
- WHO. (2004). Rapid HIV tests: Guidelines for use in HIV testing and counselling services in resource-constrained settings.
- WHO. (2007). Guidance on provider-initiated HIV testing and counselling in health facilities.
- WHO. (2012). Service delivery approaches to HIV testing and counselling (HTC): A strategic HTC programme framework. http://apps.who.int/iris/bitstream/10665/75206/1/9789241593877_eng.pdf
- WHO. (2015). Consolidated guidelines on HIV testing services.
- WHO. (2017a). Number of countries adopting HIV self-testing policies rises sharply. https://www.who.int/hiv/mediacentre/news/hiv-self-testing-increases/en/
- WHO. (2017b). Policy brief HIV prevention, diagnosis, treatment and care for key populations.
- Wringe, A., Moshabela, M., Nyamukapa, C., Bukenya, D., Ondenge, K., Ddaaki, W., Wamoyi, J., Seeley, J., Church, K., Zaba, B., Hosegood, V., Bonnington, O., Skovdal, M., & Renju, J. (2017). HIV testing experiences and their implications for patient engagement with HIV care and treatment on the Eve of “test and treat”: Findings from a multicountry qualitative study. Sexually Transmitted Infections, 93, 1–5. https://doi.org/10.1136/sextrans-2016-052969 doi: 10.1136/sextrans-2016-053045
- Wringe, A., Renju, J., Seeley, J., Moshabela, M., & Skovdal, M. (2017). Bottlenecks to HIV care and treatment in sub-Saharan Africa: A multi-country qualitative study. Sexually Transmitted Infections, 93(Suppl 3), e053172. https://doi.org/10.1136/sextrans-2017-053172