ABSTRACT
Effective implementation of policies for expanding antiretroviral therapy (ART) requires a well-trained and adequately staffed workforce. Changes in national HIV workforce policies, health facility practices, and provider experiences were examined in rural Malawi and Tanzania between 2013 and 2017.
In both countries, task-shifting and task-sharing policies were explicit by 2013. In facilities, the cadre mix of providers varied by site and changed over time, with a higher and growing proportion of lower cadre staff in the Malawi site. In Malawi, the introduction of lay counsellors was perceived to have eased the workload of other providers, but lay counsellors reported inadequate support. Both countries had guidance on the minimum numbers of personnel required to deliver HIV services. However, patient loads per provider increased in both settings for HIV tests and visits by ART patients and were not met with corresponding increases in provider capacity in either setting. Providers reported this as a challenge.
Although increasing patient numbers bodes well for achieving universal antiretroviral therapy coverage, the quality of care may be undermined by increased workloads and insufficient provider training. Task-shifting strategies may help address workload concerns, but require careful monitoring, supervision and mentoring to ensure effective implementation.
Background
Global efforts to end the AIDS epidemic by 2030 have focused on achieving universal access to antiretroviral therapy (ART) (Joint United Nations Programme on HIV/AIDS, Citation2014). In line with this goal, HIV care and treatment policies have rapidly evolved in recent years to expand eligibility for ART. In 2013, the World Health Organization (WHO) recommended that all pregnant and breastfeeding women with HIV should initiate lifelong ART regardless of immunological stage (Option B+) (World Health Organization, Citation2016), following successful implementation in Malawi from 2011(Ministry of Health Malawi, Citation2011). The recommendation was expanded in 2015 to include all people living with HIV, termed Universal Test and Treat (UTT)(World Health Organization, Citation2016). UTT was rapidly adopted as national policy in many sub-Saharan countries including Tanzania and Malawi in 2016 (Ministry of Health and Social Welfare National AIDS Control Programme (NACP), Citation2015; Ministry of Health Malawi, Citation2016).
A key challenge to expanding ART coverage relates to having an adequate health workforce to deliver HIV services(Kalua et al., Citation2017). Even prior to Option B+ implementation, only 32% of government health facilities in Malawi met the staffing norms of two nurse-midwives and one medical assistant or clinical officer, described in the Essential Health Package (Bemelmans et al., Citation2010; Ministry of Health, Citation2017). By 2017, estimates showed that there was a 33% gap between the number of providers required to deliver health services and the number of providers available (Ministry of Health Malawi, Citation2015). Similar challenges have been documented in Tanzania, where estimates from 2012 suggest a 67% gap in district hospitals and a 59% gap in health centres between the number of providers needed to meet essential health care needs, including HIV treatment, compared to the number available in the health facilities (Nationa Aids Control Programme, Citation2008).
Efforts to address the health workforce shortages for HIV in resource-limited settings have focused on task-sharing and task-shifting, including expanded or new roles for lay or community health workers (Callaghan et al., Citation2010; Woldie et al., Citation2018; World Health Organization, Citation2008, Citation2010). These approaches have led to shorter waiting times in clinics and reduced workloads among health workers in some settings, resulting in greater availability and uptake of HIV services including HIV testing (Flick et al., Citation2019). However, whilst these strategies have increased the number of providers available to deliver HIV services, various challenges have been documented including inadequate regulation, monitoring, training and supervision, lack of clarity over roles and responsibilities, and insufficient funding which may undermine service quality if not addressed (Munga et al., Citation2012; Vojnov et al., Citation2019).
These challenges may be further exacerbated when the implementation of new HIV treatment guidelines leads to a rapid increase in patient numbers, without ensuring that necessary workforce arrangements are in place. For example, the introduction of Option B+ increased the number of ART patients in many settings, but also led to health workers reporting longer working hours, raising concerns that service quality may have been affected (Nkhata et al., Citation2016). A recent study in 89 health facilities in eight districts in Malawi reported that over half of the 520 HIV health workers reported emotional exhaustion, depersonalisation, and a sense of low personal accomplishment (Kim et al., Citation2018). In the same study, the majority of health workers reported engaging in poor patient care, including making mistakes with treatment, shouting at patients, and sometimes not performing all necessary diagnostic tests due to a desire to finish quickly (Kim et al., Citation2018). In a qualitative study to determine determinants of HIV guidelines implementation in the Tanzania setting, providers reported that HIV testing, comprehensive counselling and completion of registers were not always done when patient loads got high(Mwangome et al., Citation2017).
The ability of health systems in different settings to effectively deliver UTT in a sustainable way and to meet global treatment targets will partly depend on having an adequately prepared health workforce. However, to date, there has been little research on how national policies which determine the roles and conditions of health workers in African countries have evolved in the context of changing ART treatment guidelines, and how they are implemented at the health facility level. In this paper, we examine and compare the implications of evolving HIV treatment policies on the health workforce drawing on data from policy reviews, facility surveys and in-depth interviews in rural Malawian and Tanzanian settings between 2013 and 2017.
Methods
Study settings
The study was undertaken in two health and demographic surveillance sites (HDSS) in Karonga, Malawi and Ifakara, Tanzania. The two HDSS are part of the Network for Analyzing Longitudinal Population-based HIV/AIDS data on Africa (ALPHA) (Reniers et al., Citation2016) and are two of the three that were included in the larger project known as SHAPE UTT (Strengthening Health systems for the Application of Policy to Enable Universal Test and Treat). In this study three of the HDSS sites within ALPHA were selected to represent early (Malawi), mid (Tanzania) and late (South Africa) adoption of Option B+ (2011, 2013, 2015, respectively). In this sub-study, data from two of the countries were included, based on the timing of their survey data collection.
Study population
The adult HIV prevalence in the Karonga HDSS was estimated at 7% among men and 9% among women in 2012 among a total population of 37,500 adults (Dasgupta et al., Citation2016). In Ifakara, HIV prevalence was estimated at 4.8% among men and 7.4% among women in a population of 8,403 residents of 15 years and older who accepted HIV testing (Mtenga et al., Citation2015). Both HDSS has been conducting regular demographic surveillance through household surveys for over ten years(Crampin et al., Citation2012; Geubbels et al., Citation2015; National Statistical Office (NSO), Citation2017).
Data sources
Policy reviews
We reviewed national HIV policies published between 2003 and 2018 in each country to document changes over time in WHO guidance and national policies relating to the delivery of HIV care and treatment services (Church et al., Citation2015). The review was conducted by retrieving documents identified through online searches of WHO and relevant departments, programs or units within the Ministry of Health in each country and/or retrieved in person from official offices. Inclusion criteria for the national documents were: (i) nationally relevant (not clinic- or district specific); (ii) containing programmatic or clinical guidance on one of the three key adult HIV services: HIV testing and counselling (HTC), prevention of mother-to-child transmission (PMTCT) or HIV care and treatment.
Data from 35 policy documents meeting these criteria were extracted and summarised using Excel tables that captured the date of policy adoption, key content and the reference (). Policy indicators were defined following a review of the literature and through a consultative process with HIV and health systems researchers during a workshop, and then aligned to the WHO building blocks (Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies 2010). For the purposes of this analysis, we selected all five indicators relating to the health workforce covering cadre and roles of health workers, training, staffing requirements and maximum staff workloads for facilities offering HIV care services.
Health facility surveys
This analysis utilised data collected through three health facility surveys undertaken between 2013 and 2017 in each country (Church et al., Citation2017). The surveys were conducted in all 17 health facilities providing HIV care services to the populations of the HDSS in Karonga (n=5) and in Ifakara (n=12) (). The survey questionnaire was developed by reviewing existing HIV health facility surveys, including the WHO Service Availability and Readiness Assessment surveys (World Health Organization, Citation2015b), and was administered in English by trained research staff to the facility manager or head of the relevant service units. The questionnaire covered health facility characteristics and staffing, service delivery and service usage across HTC, PMTCT and HIV care and treatment services. For this analysis, the workforce data were extracted from the full facility survey database covering the same domains as those included in the policy review (roles and cadre of health workers, training, staffing requirements and workload). Service usage data were collected for the three months preceding the date of the survey and the figures were divided by three to estimate the number of monthly HIV tests and monthly clinic visits for PMTCT. The number of ART patient visits was estimated using total number of patients on treatment at the facility and assuming that all patients on ART visit the facility for ART refills once every three months while newly initiated patients visit the facility once every month. Provider workloads were calculated by dividing the number of monthly visits by the number of medical staff (defined as doctors, clinical officers, nurses, trained counsellors) available in the facility that provide PMTCT/HTC/ART services (as reported in the facility survey).
Table 1. Characteristics of facilities and in-depth interview participants.
In-depth interviews with service providers
In each of the HDSS sites, three health facilities were stratified by type (hospital versus smaller facility) and location (district centre verses remote); in each HDSS a hospital was selected and then one remote and one facility near the district centre was randomly selected. In-depth interviews were conducted in 2018 with 7 purposively selected healthcare workers per setting involved in provision of HTC, PMTCT and HIV care and treatment services ensuring a range of cadres and roles. (). The initial plan was to conduct five interviews per site, however data collection continued for an extra two participants per site to ensure that a varied range of cadre and roles were included. Saturation was reached on the challenges faced by the health workforce in delivery HIV care and treatment services.
Interviews were conducted by the lead researcher in each setting in the local language, and audio-recorded for subsequent transcription and translation into English. The topic guides explored the health workers’ experiences of service delivery amid evolving policies, their views on policies guiding HIV service delivery and their perceptions of how policy changes had affected their ability to do their job, including challenges that they faced, and availability of support and training.
Data analysis
Data collected from through the facility surveys were entered centrally into an SQL database, and transferred to STATA13 (Stata Corp, Texas, USA) for cleaning and analysis.
In-depth interview transcripts and detailed field notes were written and together with the translations were inductively coded and analyzed thematically in each site, aided by Nvivo (QSR International Pty Ltd. Version 11, 2015). Regular discussions were held between the lead researchers to draw out similarities and differences in emerging themes across settings.
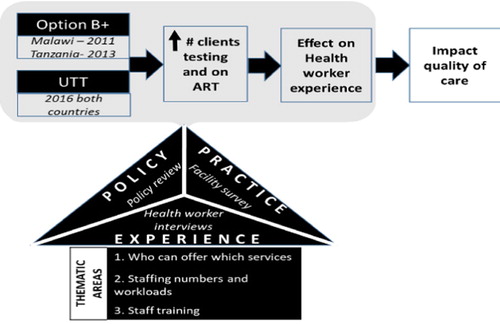
To understand how HIV policies which aimed to increase client testing and treatment numbers were implemented in facilities and experienced by providers, we triangulated data from the policy reviews, facility surveys and health worker interviews across three thematic areas shown in .
Ethics
Ethical approval was obtained from the Internal Review Boards of the Ifakara Health Institute and National Institute for Medical Research for Tanzania (#2579), National Health Science Research Committee for Malawi (#1861) and from the London School of Hygiene and Tropical Medicine (#13536-1).
Written informed consent from participants was obtained prior to undertaking the facility surveys and in-depth interviews (or through a witnessed thumbprint if the respondent was illiterate). Unique identifiers were used for identification purposes for all participants. All documents were maintained by the local study coordinator on a password-protected computer.
Results
We present the findings for each of the three thematic areas, drawing on the data from the policy review, followed by the facility survey data and in-depth interviews.
Workforce composition for delivering HTC, ART and PMTCT services
At the time of Option B+ adoption in each country, WHO guidance recommended task-shifting to allow HTC to be provided by lay workers(World Health Organization, Citation2008) (). National policies adopted in 2009 in Malawi and 2013 in Tanzania allowed HIV rapid tests and counselling to be conducted by trained and certified medical or lay workers who have at least Ordinary (O) level education and undergo a basic three week training to become certified HTC providers (Bemelmans et al., Citation2010; Ministry of Health and Social Welfare National AIDS Control Programme (NACP), Citation2012; Ministry of Health Malawi, Citation2009; World Health Organization, Citation2008). In both countries, ART prescription and dispensing was authorised for trained and certified ART or PMTCT providers including medical doctors, clinical officers, medical assistants, registered nurses, and nurse/midwife technicians by 2013 (Ministry of Health and Social Welfare National AIDS Control Programme (NACP), Citation2012; Ministry of Health Malawi, Citation2011; World Health Organization, Citation2013) ().
Table 2. Health workforce Summary.
Table 3. List of documents reviewed in policy review.
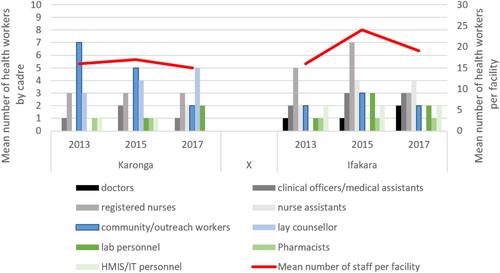
Our findings from the facility survey showed that the distribution of cadres of providers varied by site and changed over time, with a higher and growing proportion of lower cadre facility-based staff in Karonga compared to Ifakara. In Karonga, the mean number of lay counsellors per facility increased from 3 to 5 between 2013 and 2017, and the mean number of nursing assistants per facility increased from 0 to 2 over the same period (), corresponding with the period of UTT implementation. However, there was a decrease in number of community and outreach workers from an average of 7 to 2 per facility between 2013 and 2017. A similar trend was seen in Ifakara where the mean number of nurse assistants per facility increased from 2 to 4 between 2013 and 2017 and the number of registered nurses peaked at 7 in 2015 before dropping to 3 in 2017. The mean number of lay counsellors remained less than 1 per facility over the three rounds.
Through the in-depth interviews, most providers in both sites reported having more than one role in the facility, and having to make time for each, which sometimes resulted in conflicting schedules and needs. In Karonga, lay counsellors reported that they were in most cases also working as family planning counsellors and community health surveillance assistants (HSAs) and had to juggle these time-competing roles. In both sites, nurses reported having to balance time between ANC service provision (e.g. pregnancy examinations and delivery), and at the same time provide PMTCT services such ART initiation and ART refills for pregnant women. These providers felt that sometimes this contributed to long waiting times for ART refills. In more than one instance, nurses reported having to stop providing ART refills in order to assist in a delivery. The resultant delays for ART refills led to patient dissatisfaction with services.
Sometimes when we are busy supplying drugs to clients, we hear that a patient has come and needs our immediate attention, which means we have to leave whatever we have been doing to go and attend to this patient. And most of the time, this annoys our clients.(Nurse & Midwife)
You know our clients complain too much, she may complain to the extent that we may lose her … she may see that she has spent too much time (Nurse Attendant)
There are three of us. I am the only one who is a government employee my other colleagues are community based counsellors. These two colleagues of mine sometimes they don’t come, but I am always here because I am a government employee” (Lay provider)
Staffing requirements and provider workloads
In 2009, Malawi HTC guidelines stated that each HTC counsellor should only see between 8 and 15 clients per day, depending on whether individual pre-test counselling or group pre-test information sessions were conducted(Ministry of Health Malawi, Citation2009) (.). This was later updated in the 2016 guidelines to state that the number of clients seen by each counsellor per day must be ‘within the range of what is practically possible when all standard HTC protocols are followed’ and should depend on whether individual pre-test counseling or group pretest education sessions are conducted (The Ministry of Health Malawi, Citation2016). No guidance was found regarding the number of clients per provider per day in Tanzanian policy documents or WHO recommendations.
By 2013, policy in Malawi stated that health facilities should be able to determine the number and type of staff needed to run ART clinics, but with a minimum of one clinician, one nurse and one ward clerk(Ministry of Health Malawi, Citation2008). By 2013, policy in Tanzania stated that a facility should have a dedicated team of at least three health workers comprising one clinician, one adherence counsellor and one other health worker(Ministry of Health and Social Welfare National AIDS Control Programme (NACP), Citation2012). The 2015 WHO HTC guidelines recommended the use of standardised tools such as the ‘Workload Indicator of Staffing Needs’ to determine the number of health workers and lay providers needed to provide adequate services(World Health Organization, Citation2015a). By 2017, policy in both countries explicitly stated that each HTC site should have a minimum of two HTC trained, certified, and practicing staff, and that facilities should start implementing new treatment guidelines (including UTT) when at least two health workers had received training on the new guidelines (Tanzania Ministry of Health, Citation2017); Ministry of Health Malawi, Citation2016; The Ministry of Health Malawi, Citation2016).
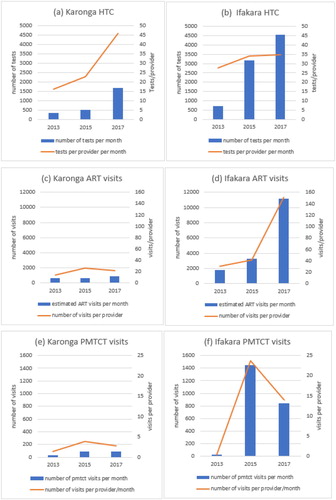
The facility survey data showed that there was a steady increase in the number of patient visits to the clinics over the three rounds of the survey in both sites (). The total number of HIV tests conducted per month in the five facilities in Karonga more than tripled from 358 in 2013–1692 in 2017 ((a)). There was a similar pattern in Ifakara where the number of tests across all facilities rose from 717 per month in 2013–4561 per month by 2017 ((b)). There was also an increase in the total number of providers across the services over the three rounds in both sites. The number of providers in HTC rose from 22 to 37 in Karonga and from 26 to 131 in Ifakara from 2013 to 2017 ((a,b)). However, the increase in providers was relatively lower than the increase in HIV tests, resulting in a rise in the number of HIV tests per provider per month from 16 to 45 from 2013 to 2017 in Karonga and from 28 to 35 in Ifakara over the same period ((a,b)).
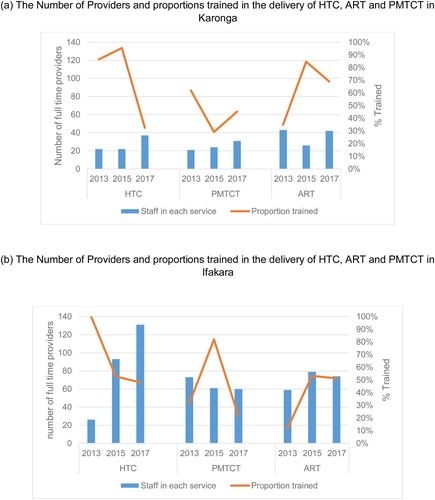
Figure 4. (a): The Number of Providers and proportions trained in the delivery of HTC, ART and PMTCT in Karonga. (b): The Number of Providers and proportions trained in the delivery of HTC, ART and PMTCT in Ifakara.
The number of clinic visits for patients who were on ART or in pre-ART care also increased from 628 to 929 per month in Karonga between 2013 and 2017 and from 1767 to 11177 per month over the same period in Ifakara ((c,d)). In both Karonga and Ifakara, the number of providers providing ART care remained roughly constant over the three rounds ((a,b)). The number of monthly patient visits per provider for ART and pre-ART care rose from 15 to 22 in Karonga and from 30 to 151 in Ifakara between 2013 and 2017 ((c,d)).
There was also an increase in the number of monthly visits for PMTCT services for HIV positive women from 30 to over 85 per month in Karonga and from 33 to over 800 visits per month in Ifakara between 2013 and 2017 ((e,f)). The number of providers in PMTCT across the facilities rose from 21 to 31 in Karonga, but decreased slightly from 73 to 60 in Ifakara ((a,b)). The number of monthly PMTCT visits per provider rose from 1 to 3 in Karonga between 2013 and 2017 and from 0 to 14 in Ifakara and in the same period ((e,f)).
In both sites, providers reported that increasing patient numbers had increased their workloads and led to long waiting times for patients seeking HTC and HIV care and treatment services. In Karonga, some providers reported abrupt increases in the number of patients seeking HIV care following policy changes, limiting their ability to find solutions to manage the higher demand without additional personnel:
Universal test and treat affected us in a number of ways because the change was abrupt not gradual, so the number of people wanting to be tested shot up tremendously but the number of staff was the same and that was increasing our workload (Nurse/ Midwife)
Personally I think there isn’t much difference because at first we used to send people home and ask them to come back later this was like doing the same work twice in terms of registration and other logistics.(Nurse/ Midwife)
We are able to deal with this large number of people because of personal commitment especially on the part of the volunteers who work with us (Lay provider)
We were trained four of us … as you know with the President’s concern [over the occurrence of] incorrect certificates, some of our colleagues also faced that problem [of having incorrect certificates] but [what is] important is despite the staff shortage, we have to divide ourselves to ensure patients get the needed services (Nurse)
We divided service provision in days due to shortage of staff. There are some activities that cannot be done by anyone except me, for example enrolment or drugs dispensing which need to be done with a person with my level. (Nurse)
Training of health workers to provide HTC, ART and PMTCT services
The 2008 Malawi guidelines on use of ART stated that health workers working at new ART sites should be trained and receive annual refresher trainings (Ministry of Health Malawi, Citation2008) (.). Similarly, the 2012 National Guidelines for the Management of HIV and AIDS in Tanzania stipulated annual refresher trainings for all health workers providing HTC services (Ministry of Health and Social Welfare National AIDS Control Programme (NACP), Citation2012). Between 2013 and 2017, Malawi policy stipulated that training on ART care and PMTCT was required as scale-up continued or guidelines were changed, which translated to around every two years (Ministry of Health Malawi, Citation2014; The Ministry of Health Malawi, Citation2016). The 2015 National Guidelines for the Management of HIV and AIDs in Tanzania stated that ART care and adherence training was to ‘be offered and updated periodically for all health care team members’, but without specifying the frequency (Ministry of Health and Social Welfare National AIDS Control Programme (NACP), Citation2015, 2017).
The facility survey data showed that the proportion of all providers in each facility who received HTC training in the past two years dropped between 2013 and 2017 from 86% to 32% in Karonga and from 100% to 48% in Ifakara ((a,b)), suggesting non-alignment to policy. The proportion of all providers who received training in HIV care and treatment in the past two years fluctuated from 35% in 2013–85% in 2015–69% in 2017 in Karonga ((a)). A similar overall increase was also noted in Ifakara where the proportion of providers trained in HIV care and treatment in the past 2 years increased from 12% in 2013–53% in 2015, remaining stable at 51% in 2017 ((b)). In both sites, the proportion of trained providers is lower than that suggested by national policy. In Karonga, the proportion of providers who received PMTCT training in the past two years was highest in 2013 at 62%, before dropping to 29% in 2015 and rising to 45% in 2017 ((a)). The corresponding figure in Ifakara was highest in 2015 (89%), before dropping to 22% by 2017 ((b)). The proportion trained at the different time points corresponds to changes in policy guidance (namely the uptake of Option B+ in 2011 in Malawi and 2013 in Tanzania).
Most providers who were interviewed who initiated ART and administered ART refills reported undergoing training following the introduction of new guidelines on UTT and Option B+, with mentorship also being adopted to address training needs in some facilities. However, lay workers, mostly reported having to rely on on-the-job training from their senior peers as training opportunities were limited to higher cadre staff, which could lead to some resentment.
When he/she (new health workers) come here for the first time, we just do mentorship while waiting for formal training. If it happens there is training she/he will go. But sometimes trainings come with criteria, such as trainings for a certain cadre to attend. So those who are not in that cadre might miss … and this happens usually to medical attendants who are the ones mostly working in this department.” (Nurse)
Discussion
This study used data from three sources to compare how evolving HIV treatment policies affected the health workforce in rural Malawian and Tanzanian settings between 2013 and 2017. We found that despite similar policies in both settings, there were differences in facility-level implementation that had consequences for providers’ experiences.
The mix of cadre among the providers varied by site, with a more medical and specialised workforce delivering HIV services in Ifakara, compared to Karonga, where policies on task-shifting had been more actively pursued. Documented benefits of task-shifting for health systems include greater cost efficiencies in service delivery and reduced queues in health services (Callaghan et al., Citation2010). Furthermore, several studies have demonstrated comparable ART patient outcomes when treatment services are delivered by nurses instead of clinicians(Iwu & Holzemer, Citation2014), and evidence from systematic reviews suggests that the use of lay healthcare providers is effective in increasing HIV service uptake, including those for PMTCT and increasing retention of HIV-positive mothers and their infants in PMTCT programmes (Vrazo et al., Citation2018). In Karonga, lay counsellors were perceived to have eased the workload of providers, but reported challenges included lack of adequate support within clinics and absenteeism, which has also been noted in other African settings such as South Africa, Zambia, Rwanda, Uganda, Kenya (Callaghan et al., Citation2010). Greater emphasis needs to be placed on supporting lay cadres and ensuring the quality of care by providing ongoing mentoring and appropriate training opportunities, which have been reported to have been effective in improving lay provider performance and retention in Malawi, Tanzania and other sub-Saharan Africa settings(Decroo et al., Citation2013; Feldacker et al., Citation2017). Further research is needed to identify a suitable model to sustainably integrate these workers into the government structures.
Task-sharing, whereby one cadre performs many roles, was common in both study settings, and may increase the efficiency of HIV service delivery. However, in Karonga, providers noted that being pulled away from serving HIV patients by competing responsibilities from other services (notably deliveries), may lead to longer waiting times for HIV patients. Whilst there is a growing literature supporting task-sharing of HIV care including the initiation of ART by non-clinical personnel (Kredo et al., Citation2014; McNairy et al., Citation2017) to support the level of scale-up of access to ART required to meet the 90-90-90 targets. Attention still needs to be paid to ensure that task-sharing efforts do not undermine other services (Walsh et al., Citation2010) including the progress made in terms of reducing waiting times for patients in these settings.
In both settings, we observed substantial increases in HIV service use following expanded ART eligibility criteria, which bodes well for achieving the 90-90-90 targets. However, we also observed that increases in the numbers of visits from patients seeking HIV services in both settings did not systematically correspond with an increase in provider capacity to deliver these services. While the change in the number of providers noted could be a result of changes in their classification and roles within the clinics, especially between community health workers and lay counsellors, there was a general decline in the mean number of providers per facility between round 2 and round 3. This is of concern since health provider workload is associated with quality of care. A recent study in Kenya, Ivory Coast and Mozambique found that for each additional first antenatal care visit per nurse per month, the odds that an HIV-positive pregnant woman would receive both HIV testing and antiretroviral medications declined by 4% (95% confidence interval (CI): 1%-6%)(Rustagi et al., Citation2017). In other studies, ART clients have perceived a better sense of care and reported better well-being in health facilities where providers were deemed to be more ‘available’ and ‘accessible’ (Ondenge et al., Citation2017). Retention in care and favourable health outcomes for ART patients have been closely linked to provider and patient interactions(Ondenge et al., Citation2017). While a formal assessment of the impact of health workforce challenges on patient outcomes including retention in care goes beyond the scope of this analysis, our findings suggested that the lengthy waiting times that resulted from the sudden increases in provider workloads could serve to undermine the quality of care and contribute to disengagement from care. Whilst the WHO provides a workload indicator for staffing needs, the most recent policy guidelines in both countries only specify the actual number of providers required but not in the context of the ratio to service users. Our study supports the application of a workload indicator, specifically in the context of quality of care, to enable a more nuanced understanding of factors that may be influencing retention and adherence.
The providers in our study settings reported challenges arising from increased workloads as HIV eligibility criteria expanded, but they also reported implementing ad hoc solutions that went beyond the specifics of national policies, including the provision of some services on specific days and impromptu task-shifting which allowed the health workers to prioritise HIV care service users on specific days and reduce patient waiting times. While less explicit policies may encourage facility-level solutions to be sought, the impact of decisions to restrict service availability on HIV service access and uptake is unclear. As other studies in Tanzania have suggested, spontaneous task-shifting to cope with high workloads may undermine the quality of care and should be carefully monitored (Munga et al., Citation2012).
The need for additional resources for training and supervisory tasks were also considered important factors in ensuring task-shifting does not compromise the quality of care(Munga et al., Citation2012). In both sites, training frequency was inadequate. Providers in both sites reported that insufficient, or ‘on the job’ training hampered the quality of patient care, although efforts were being made in some facilities to provide mentoring to new staff and lower cadre staff. Our findings suggest that further investments are needed to ensure formalised mentoring strategies are widely adopted within clinics.
There are various strengths and limitations that need to be considered when interpreting our data. Firstly, the survey responses which were derived from health facility managers may be subject to reporting biases and could lead to skewed estimates of the services and staff available. Staffing numbers were reported by the facility managers and may not have taken into account part time workers. Furthermore, the facilities that were surveyed were selected as they served health and demographic surveillance system site populations, and were not nationally representative. Although this limits the generalisability of our findings, the facilities can be considered typical of those found in rural areas in each country. However, it should be noted that their small number meant that it was not appropriate to assess for statistical significance in changes over time. With regards to the qualitative data, social desirability bias may underlie some of the providers’ responses, leading them to highlight positive or negative experiences, if they felt that they may be at risk of being sanctioned, or they thought that the research results may lead to improvements in their working conditions. However, fieldworkers explained the study and developed rapport with the interviewees to minimise this effect. The main strength of this analysis is that it offers a detailed case-study of facility-level impacts and provider experiences of evolving HIV policies on the HIV workforce using data from three sources at three time points.
In conclusion, whilst universal ART policies have resulted in intended increases in the number of people living with HIV who are diagnosed and receiving treatment, health workforce policies need to evolve at a similar pace to ensure that the health systems and workforce are better equipped to implement these policies without risking reduced quality of care and poorer health outcomes for patients.
Author contribution statement
The study was conceived by JS, AW and JR. AW, JT, AC, EG and JT designed the protocol and study tools; which were adapted and implemented by JS, AD, LL and FH. Initial analyses were conducted by JS, EM, SV, LL, TK, DK, ES, EG, and JR. Final analyses were conducted by JS, AW, and JR. The manuscript was drafted by JS, with input from all authors. All authors read and approved the final manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Bemelmans, M., Van Den Akker, T., Ford, N., Philips, M., Zachariah, R., Harries, A., Schouten, E., Hermann, K., Mwagomba, B., & Massaquoi, M. (2010). Providing universal access to antiretroviral therapy in Thyolo, Malawi through task shifting and decentralization of HIV/AIDS care. Tropical Medicine & International Health, 15(12), 1413–1420. https://doi.org/10.1111/j.1365-3156.2010.02649.x
- Callaghan, M., Ford, N., & Schneider, H. (2010). A systematic review of task- shifting for HIV treatment and care in Africa. Human Resources for Health, 8(1), 8–8. https://doi.org/10.1186/1478-4491-8-8.
- Church, K., Kiweewa, F., Dasgupta, A., Mwangome, M., Mpandaguta, E., Gómez-Olivé, F. X., Oti, S., Todd, J., Wringe, A., Geubbels, E., Crampin, A., Nakiyingi-Miiro, J., Hayashi, C., Njage, M., Wagner, R. G., Ario, A. R., Makombe, S. D., Mugurungi, O., & Zaba, B. (2015). A comparative analysis of national HIV policies in six African countries with generalized epidemics. Bulletin of the World Health Organization, 93(April), 457–467. https://doi.org/10.2471/BLT.14.147215
- Church, K., Machiyama, K., Todd, J., Njamwea, B., Mwangome, M., Hosegood, V., Michel, J., Oti, S., Nyamukapa, C., Crampin, A., Amek, N., Nakigozi, G., Michael, D., Gómez-Olivé, F. X., Nakiyingi-Miiro, J., Zaba, B., & Wringe, A. (2017). Identifying gaps in HIV service delivery across the diagnosis-to-treatment cascade: Findings from health facility surveys in six sub-Saharan countries. Journal of the International AIDS Society, 20(1), 21188–21188. https://doi.org/10.7448/IAS.20.1.21188.
- Crampin, A. C., Dube, A., Mboma, S., Price, A., Chihana, M., Jahn, A., Baschieri, A., Molesworth, A., Mwaiyeghele, E., Branson, K., Floyd, S., McGrath, N., Fine, P. E. M., French, N., Glynn, J. R., & Zaba, B. (2012). Profile: The Karonga health and demographic surveillance system. International Journal of Epidemiology, 41(3), 676–685. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3396313/. https://doi.org/10.1093/ije/dys088
- Dasgupta, A. N. Z., Wringe, A., Crampin, A. C., Chisambo, C., Koole, O., Makombe, S., Sungani, C., Todd, J., & Church, K. (2016). HIV policy and implementation: A national policy review and an implementation case study of a rural Area of Northern Malawi †. AIDS Care, 28(9), 1097–1109. https://doi.org/10.1080/09540121.2016.1168913
- Decroo, T., Decroo, T., Rasschaert, F., Telfer, B., Remartinez, D., Laga, M., & Ford, N. (2013). Community-based antiretroviral therapy programs can overcome barriers to retention of patients and decongest health services in sub-Saharan Africa: A systematic review. International Health, 5(3), 169–179. https://doi.org/10.1093/inthealth/iht016
- Feldacker, C., Pintye, J., Jacob, S., Chung, M. H., Middleton, L., Iliffe, J., Kim, H. N., & Leroyer, C. (2017). Continuing professional development for medical, nursing, and midwifery cadres in Malawi, Tanzania and South Africa: A qualitative evaluation. PloS one, 12(10), 1932–6203. https://doi.org/10.1371/journal.pone.0186074
- Flick, R. J., Flick, R. J., Simon, K. R., Nyirenda, R., Namachapa, K., Hosseinipour, M. C., Schooley, A., Kavuta, E., Theu, J., Kazembe, P. N., Ahmed, S., & Kim, M. H. (2019). The HIV diagnostic assistant. AIDS, 33(7), 1215–1224. https://doi.org/10.1097/QAD.0000000000002159
- Geubbels, E., Amri, S., Levira, F., Schellenberg, J., Masanja, H., & Nathan, R. (2015). Health & demographic surveillance system profile: The Ifakara rural and urban health and demographic surveillance system (Ifakara HDSS). International Journal of Epidemiology, 44(3), 848–861. https://doi.org/10.1093/ije/dyv068
- Iwu, E. N., & Holzemer, W. L. (2014). Task shifting of HIV management from doctors to nurses in Africa: Clinical outcomes and evidence on nurse self-efficacy and job satisfaction. AIDS Care, 26(1), 42–52. https://doi.org/10.1080/09540121.2013.793278
- Joint United Nations Programme on HIV/AIDS. (2014). “90-90-90; An ambitious treatment target to help end the AIDS epidemic.” United Nations.
- Kalua, T., Tippett Barr, B. A., van Oosterhout, J. J., Mbori-Ngacha, D., Schouten, E. J., Gupta, S., Sande, A., Zomba, G., Tweya, H., Lungu, E., Kajoka, D., Tih, P., & Jahn, A. (2017). Lessons learned from Option B+ in the evolution toward test and start from Malawi, Cameroon, and the United Republic of Tanzania. JAIDS Journal of Acquired Immune Deficiency Syndromes, 75, S43–S50. https://doi.org/10.1097/QAI.0000000000001326
- Kim, Maria, Mazenga, Alick, Simon, Katie, Yu, Xiaoying, & Ahmed, Saeed. (2018). Burnout and self-reported suboptimal patient care amongst health care workers providing HIV care in Malawi. PloS one, 13(2), e0192983–e0192983. https://doi.org/10.1371/journal.pone.0192983
- Kredo, T., Adeniyi, F. B., Bateganya, M., & Pienaar, E. D. (2014). Task shifting from doctors to non-doctors for initiation and maintenance of antiretroviral therapy - The Cochrane library - Kredo - Wiley online Library. Cochrane Database of Systematic Reviews, 7, 1465–1858. doi:10.1002/14651858.CD007331.pub3.
- McNairy, M. L., Bashi, J. B., Chung, H., Wemin, L., Lorng, M.-N. A., Brou, H., Nioble, C., Lokossue, A., Abo, K., Achi, D., Ouattara, K., Sess, D., Sanogo, P. A., Ekra, A., Ettiegne-Traore, V., Diabate, C. J., Abrams, E. J., & El-Sadr, W. M. (2017). Task-sharing with nurses to enhance access to HIV treatment in côte d’Ivoire. Tropical Medicine and International Health, 22(4), 431–441. https://doi.org/10.1111/tmi.12839
- Ministry of Health and Social Welfare. (2013). National comprehensive guidelines for HIV testing and counselling. Tanzania.
- Ministry of Health and Social Welfare, National AIDS control programme. (2015). National guidelines for the management of HIV and AIDs (5th ed.). Ministry of Health and Social Welfare.
- Ministry of Health and Social Welfare National AIDS Control Programme (NACP). (2012). National guidelines for the management of HIV and AIDS.
- Ministry of Health, Community Development, Gender and Elderly. (2017). “National guidelines for the management of HIV and AIDS.” 6(October): (6th ed.). Tanzania.
- Ministry of Health Malawi. (2008). “Guidelines for the use of antiretroviral therapy in Malawi.” Ministry of Health, Lilongwe, Malawi 3(April).
- Ministry of Health Malawi. (2009). “Government of Malawi guideline for HIV testing and counsellling (HTC).” Ministry of Health, Lilongwe, Malawi: 3rd edition.
- Ministry of Health Malawi. (2011). “Clinical management of HIV in children and adults.” Ministry of Health, Lilongwe, Malawi (1st Edition).
- Ministry of Health Malawi. (2014). “Clinical management of HIV In children and adults.” Ministry of Health, Lilongwe, Malawi (2nd Edition).
- Ministry of Health Malawi. (2015). “Health sector strategic plan II 2017–2022.” Ministry of Health, Lilongwe, Malawi 2(2).
- Ministry of Health Malawi. (2016). “Clinical management of HIV in children and adults.” Ministry of Health, Lilongwe, Malawi (3rd Edition).
- The Ministry of Health Malawi. (2016). HIV testing services guidelines.
- Ministry of Health, Malawi. (2017). “Health sector strategic plan II 2017-2022.” II. Monitoring the building blocks of health systems: A handbook of indicators and their measurement strategies. 2010.
- Mtenga, S. M., Pfeiffer, C., Merten, S., Mamdani, M., Exavery, A., Haafkens, J., Tanner, M., & Geubbels, E. (2015). Prevalence and social drivers of HIV among married and cohabitating heterosexual adults in South-Eastern Tanzania: Analysis of adult health community Cohort data. Global Health Action, 8(1), 28941–28941. https://doi.org/10.3402/gha.v8.28941
- Munga, M. A., Kilima, S. P., Mutalemwa, P. P., Kisoka, W. J., & Malecela, M. N. (2012). Experiences, opportunities and challenges of implementing task shifting in underserved remote settings: The case of Kongwa district, Central Tanzania. BMC International Health and Human Rights, 12(1), 27–27. https://doi.org/10.1186/1472-698X-12-27
- Mwangome, M. N., Geubbels, E., Wringe, A., Todd, J., Klatser, P., & Dieleman, M. (2017). A qualitative study of the determinants of HIV guidelines implementation in two south-eastern districts of Tanzania. Health Policy and Planning, 32(6), 825–834. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC5448494/. https://doi.org/10.1093/heapol/czx023
- National Aids Control Programme. (2008). Human resources for health strategic plan 2008-2013.
- National Statistical Office (NSO). (2017). “Malawi demographic and health survey.” National Statistics Office The DHS Program.
- Nkhata, M. J., Muzambi, M., Ford, D., Chan, A. K., Abongomera, G., Namata, H., Mambule, I., South, A., Revill, P., Grundy, C., Mabugu, T., Chiwaula, L., Hakim, J., Kityo, C., Reid, A., Katabira, E., Sodhi, S., Gilks, C. F., Gibb, D. M., … Cataldo, F. (2016). Shifting human resources for health in the context of ART provision: Qualitative and quantitative findings from the Lablite Baseline study. BMC Health Services Research, 16(1), 1472–6963. https://doi.org/10.1186/s12913-016-1891-7.
- Ondenge, K., Renju, J., Bonnington, O., Moshabela, M., Wamoyi, J., Nyamukapa, C., Seeley, J., Wringe, A., & Skovdal, M. (2017). ‘I am treated well if I adhere to my HIV medication’: Putting patient-provider interactions in context through insights from qualitative research in five sub-Saharan African countries. Sexually Transmitted Infections, 93(Suppl 3), e052973–e052973. https://doi.org/10.1136/sextrans-2016-052973.
- Reniers, G., Wamukoya, M., Urassa, M., Nyaguara, A., Nakiyingi-Miiro, J., Lutalo, T., Hosegood, V., Gregson, S., Gómez-Olivé, X., Geubbels, E., Crampin, A. C., Wringe, A., Waswa, L., Tollman, S., Todd, J., Slaymaker, E., Serwadda, D., Price, A., Oti, S., … Zaba, B. (2016). Data resource profile: Network for analysing longitudinal population-based HIV/AIDS data on Africa (ALPHA Network). International Journal of Epidemiology, 45(1), 83–93. https://doi.org/10.1093/ije/dyv343
- Rustagi, A. S., Gimbel, S., Nduati, R., Cuembelo, M. d. F., Wasserheit, J. N., Farquhar, C., Gloyd, S., & Sherr, K. (2017). Health facility factors and quality of services to prevent mother-to-child HIV transmission in côte d’Ivoire, Kenya, and Mozambique. International Journal of STD & AIDS, 28(8), 788–799. https://doi.org/10.1177/0956462416668766
- Vojnov, L., Taegtmeyer, M., Boeke, C., Markby, J., Harris, L., Doherty, M., Peter, T., Ford, N., & Kufa, T. (2019). “Performance of non-laboratory staff for diagnostic testing and specimen collection in HIV programs: A systematic review and meta-analysis. PLOS ONE, 14(5), e0216277–e0216277. ed. Tendesayi Kufa. https://doi.org/10.1371/journal.pone.0216277.
- Vrazo, A. C., Firth, J., Amzel, A., Sedillo, R., Ryan, J., & Phelps, B. R. (2018). Interventions to significantly improve service uptake and retention of HIV-positive pregnant women and HIV-exposed infants along the prevention of mother-to-child transmission continuum of care: Systematic review. Tropical Medicine & International Health, 23(2), 136–148. https://doi.org/10.1111/tmi.13014
- Walsh, A., Ndubani, P., Simbaya, J., Dicker, P., & Brugha, R. (2010). Task sharing in Zambia: HIV service scale-up compounds the human resource crisis. BMC Health Services Research, 10(1), 272–272. https://doi.org/10.1186/1472-6963-10-272.
- Woldie, M., Feyissa, G. T., Admasu, B., Hassen, K., Mitchell, K., Mayhew, S., McKee, M., & Balabanova, D. (2018). Community health volunteers could help improve access to and use of essential health services by communities in LMICs: An umbrella review. Health Policy and Planning, 33(10), 0268–1080. https://doi.org/10.1093/heapol/czy094.
- World Health Organization. (2008). “Operations manual for delivery of HIV prevention, care and treatment at primary health centres in high-prevalence, resource-constrained settings.” WHO publications. Retrieved March 19, 2019, from https://www.who.int/hiv/pub/imai/operations_manual/en/.
- World Health Organization. (2010). “Taking stock: Task shifting to tackle health worker shortages.” WHO publications: 1–12. Retrieved March 10, 2019, from https://www.who.int/healthsystems/task_shifting_booklet.pdf.
- World Health Organization. (2013). “Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: Recommendations for a public health approach.” WHO publications. Retrieved March 30, 2019 from https://www.who.int/hiv/pub/arv/arv-2016/en/.
- World Health Organization. (2015a). “Consolidated guidelines on HIV testing services.” WHO publications (July). Retrieved March 29, 2019, from https://www.who.int/hiv/pub/guidelines/hiv-testing-services/en/.
- World Health Organization. (2015b). Service Availability and Readiness Assessment (SARA). Retrieved March 21, 2019, from https://www.who.int/healthinfo/systems/sara_reference_manual/en/on.
- World Health Organization. (2016). Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection - Recommendations for a public health approach - Second Edition. Retrieved March 12, 2019, from https://www.who.int/hiv/pub/arv/arv-2016/en/.