ABSTRACT
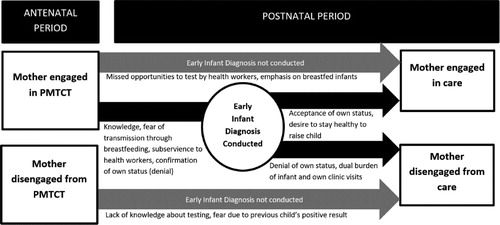
Few studies have explored the relationship between early infant diagnosis (EID) of HIV and mothers’ engagement in care under Option B+. We conducted in-depth interviews with 20 women who initiated antiretroviral therapy (ART) under Option B+ in rural South Africa to explore the interactions between EID and maternal care engagement. Drawing on practice theory, we identified themes relating to Option B+ care engagement and EID. Women’s practice of engagement with HIV care shaped their decision-making around EID. Mothers who disengaged from care during pregnancy were less inclined to utilise EID as they lacked information about its availability and benefits. For some mothers, tensions between wanting to breastfeed and perceptions that it could facilitate transmission led to repeated utilisation of EID as reassurance that the child remained negative. Some mothers used their child’s negative result as a proxy for their status, subsequently disengaging from care. For some participants, an HIV diagnosis of their infant and the subsequent double burden of treatment visits for themselves and their infant, contributed to their disengagement. Women’s care-seeking practices for themselves and their infants work in a symbiotic ecosystem and should be viewed interdependently to tailor interventions to improve EID uptake and Option B+ care engagement.
KEYWORDS:
Introduction
By 2015, Option B+, which involves initiating all HIV positive pregnant women on antiretroviral therapy (ART) regardless of immunological stage (WHO, Citation2015) and testing all exposed infants (UNAIDS, Citation2011) had been adopted as national policy for prevention of mother-to-child transmission of HIV (PMTCT) programmes in the majority of sub-Saharan African countries, including South Africa (South Africa: National Department of Health, Citation2015). Option B+ has dramatically increased the number of pregnant women initiating ART, however retention has been challenging, particularly in the postnatal period and after breastfeeding cessation (Dzangare et al., Citation2016; Erlwanger et al., Citation2017; Knettel et al., Citation2017; Tenthani et al., Citation2014). Attrition from Option B+ programmes contributes to morbidity and mortality linked to ART cessation (Ananworanich et al., Citation2006; Kranzer & Ford, Citation2011; Strategies for Management of Antiretroviral Therapy (SMART) Study Group et al., Citation2006). Furthermore, if the women are not virally suppressed it increases their potential onward transmission both horizontally and vertically (in their current or subsequent pregnancies) (Donnell et al., Citation2010; Eyawo et al., Citation2010; Hoffman et al., Citation2010). In addition, for PMTCT programmes to be effective, mothers need to attend services to receive prophylaxis for new-borns, test their infants (early infant diagnosis (EID)) and for those who test positive, initiate them onto lifelong ART.
Serological assays used for adult testing are not reliable for infants given that maternal HIV antibodies can persist in infants up to 18 months. EID seeks to establish the presence of HIV infection in children less than 18 months old through DNA polymerase chain reaction (PCR) testing. EID allows for HIV-infected infants to be linked to care and treatment early, which reduces infant morbidity and mortality (Collins et al., Citation2014; Violari et al., Citation2008; Wamalwa et al., Citation2012). Ninety percent of HIV exposed infants (HEI) should be tested by eight weeks according to the World Health Organisation global targets, but EID uptake in many sub-Saharan African countries is suboptimal (Kalk et al., Citation2018; Ministry of Health, Government of Malawi, Citation2012; SAPMTCTE study group, Citation2012), with only half of HEI in 21 priority countries reported to have been tested in 2015 (UNAIDS, Citation2015).
A growing body of qualitative research has explored underlying reasons for poor retention across the Option B+ cascade (Atanga et al., Citation2017; Clouse et al., Citation2014; Knettel et al., Citation2017; McLean et al., Citation2017). Many of these reasons mirror those identified among the general population on ART, including stigma, grappling with the lifelong commitment of daily treatment-taking (Chadambuka et al., Citation2017; Katirayi, Chouraya, et al., Citation2016), denial of HIV status (Clouse et al., Citation2014; Flax et al., Citation2017; Kim et al., Citation2016; Napúa et al., Citation2016), and treatment side effects (Buregyeya et al., Citation2017; Gill et al., Citation2017; Ngarina et al., Citation2014; Stinson & Myer, Citation2012). Other reasons that are specific to Option B+ included still feeling healthy, and lack of readiness to start ART when still coming to terms with a recent positive diagnosis (Cataldo et al., Citation2017; McLean et al., Citation2017), especially in settings where same-day ART initiation is offered and expected (Katirayi, Namadingo, et al., Citation2016). Disengagement from care following transfer from PMTCT programmes to routine care can occur if women have to attend different HIV clinics for themselves and their child (van Lettow et al., Citation2014), or if they have not yet disclosed to anyone, and post pregnancy they no longer have an easy explanation to attend HIV clinics or take daily medication (Clouse et al., Citation2014), or they do not have anyone they can leave the baby with (Ngarina et al., Citation2014). Some post-partum women feel their babies are no longer at risk of HIV transmission and no longer feel the need to take medication (Ngarina et al., Citation2014), while others who experience post-partum depression may also struggle to remain engaged in care (Dow et al., Citation2014).
An infant’s engagement in care is inextricably linked to that of the mother, however EID rates are lower than maternal care engagement (Etoori et al., Citation2018; Sibanda et al., Citation2013), suggesting additional factors drive this poor uptake. Poor quality counselling, fear of stigma, fear of disclosure, costs of multiple clinic visits, and a lack of service integration have been highlighted as barriers to achieving optimal EID coverage (Braitstein et al., Citation2011; Braun et al., Citation2011; Ciampa et al., Citation2011; Cook et al., Citation2011; Cromwell et al., Citation2015; Nuwagaba-Biribonwoha et al., Citation2014). The stressfulness of EID for the mother, lack of knowledge regarding EID and infant ART, the perception of health care workers as authority figures, fear of disclosure of own and/or child's HIV status, lack of psychosocial support, and intent to shorten the life of the child have also been shown to be significant barriers and facilitators of EID (Donahue et al., Citation2012; Lazarus et al., Citation2009). However, few studies have investigated how experiences with EID may influence a mother’s engagement and retention in care. Given that one key motivation for mothers to start ART is to prevent transmission to their baby (McLean et al., Citation2017), a positive EID result for example could be a direct cause of disengagement.
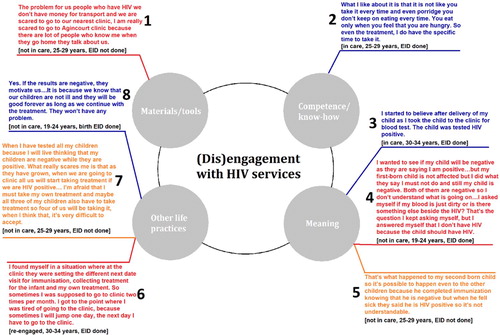
Practice theory is increasingly being used to understand HIV engagement in sub-Saharan African settings (Kippax et al., Citation2013; Skovdal, Citation2019; Skovdal et al., Citation2018). Practice theorists treat practices – the elements that shape our perceptions, interpretations and actions – as their primary units of enquiry and contend that people’s practices can be explained by generic ‘elements’ which include materials or tools required to enact a practice, symbolic meanings associated with a practice, and competence and know-how to enact a practice. Each individual has a constellation of practices that they engage in, with some of these practices interacting either harmoniously or in conflict. Consequently, the enactment of one practice is likely to affect other practices (Blue et al., Citation2016; Schatzki, Citation2002; Shove et al., Citation2012; Skovdal et al., Citation2017). Shove et al. (Citation2012) and Schatzki (Citation2002) speak of ‘bundles of practices’ to describe such a grouping of inter-reliant practices and encourage the understanding of how these bundles evolve, share and compete for resources through their connections.
We draw on theories of practice in our analysis to explore how the practices of engaging in HIV care and utilising EID are socially situated, being shaped by the materials, competences and meanings in the lives of women offered Option B+ in a rural South African setting.
Methods
Study design and setting
Data for this analysis are part of a larger mixed methods study which aimed to ascertain patients’ treatment outcomes after they become lost to follow-up and to explore experiences of HIV services, disengagement and re-engagement in care from the perspective of people living with HIV living in Agincourt in rural South Africa. The larger parent study (not included in these analyses) involved a comprehensive record review of clinic records of patients meeting the LTFU criteria, as well as supplementary tracing by community healthcare workers (HCWs) (Etoori et al., Citation2020). As part of this larger parent study, we conducted thirty-two in-depth interviews (IDIs) between January and February 2018 (20 Option B+ women, 7 non-Option B+ women, and 5 men).
The qualitative sub-study presented here includes the IDIs conducted with Option B+ women living with HIV (n = 20, 7 not engaged in care) who had given birth since 2015 and who resided in the area covered by the Agincourt health and demographic surveillance system (AHDSS) in rural Bushbuckridge, Mpumalanga province, north-eastern South Africa in 2017 (Kahn et al., Citation2012).
The AHDSS has been tracking demographic and health events in Tsonga or Shangaan people since 1992. The populace of approximately 115,000 people spread over 30 villages is served by eight government health facilities: five clinics and three community health centres. PMTCT services have been offered in all facilities since 2004, with Option B+ starting in 2015. Participants in the AHDSS who attend health facilities in the study area give consent to have their clinic records linked to their demographic surveillance data.
Sampling and recruitment
We drew up a sampling frame using the linked AHDSS and clinic database of all patients who initiated ART during pregnancy since 2015. We then recruited participants purposively to ensure diversity in terms of age, parity, clinic attended, and current treatment status. We utilised home Global Positioning System (GPS) coordinates collected routinely by the AHDSS to locate potential participants including those currently disengaged from care, many of whom have been lost to the health system and as a result are under-represented in research (Wringe, Renju, et al., Citation2017). Avoiding recruitment through health services was also to help limit bias that may arise from refusals that might result from participants’ perceptions that recruitment was an attempt to re-engage them in care.
Participants were approached and invited by a fieldworker who explained the study. This population is routinely studied through demographic surveillance and participants give permission to be contacted at home for further research, so contact with fieldworkers is not unusual and would not inadvertently breach their privacy. Participants received an information sheet with study details and contact information and were asked to give written informed consent prior to the interview.
The first author, a male PhD student, trained and supervised five female fieldworkers who conducted the interviews, four of whom had previous experience with conducting IDIs. The research team emphasised their role as researchers to participants to minimise the power dynamics that may be associated with patient provider interactions.
Trained fieldworkers that were previously unknown to the participants conducted IDIs in Shangaan language based on a topic guide. Interviews were conducted in a private location of the patient’s choice. Interviews lasted approximately 60–90 min, and participants were encouraged to speak candidly as their accounts would only be reported anonymously. The topic guide covered experiences using HIV care and treatment services, including EID services, and episodes of engagement and dis-engagement from care. Field notes were taken and all IDIs were audio-recorded and transcribed directly into English. Transcripts were anonymised, password-protected and stored on a non-networked password-protected hard-drive.
Data analysis
We analysed the data generated thematically drawing on the principles of inductive coding to construct themes. Three initial interviews were transcribed and manually open coded by the lead author to identify emerging themes, refine the topic guide and develop the coding framework. We held debriefing sessions with fieldworkers to provide an opportunity to reflect on the interviews, refine the topic guides and provide guidance on interviewing techniques. All the transcripts were then coded with the aid of Nvivo11. The coding framework was continually refined as more transcripts were analysed to capture new codes as they emerged. Codes were then grouped and conceptualised to identify themes and considered in relation to the main social practices of interest. Interpretations were built by exploring relationships between the social practices mentioned by the participants and considering the meanings they gave to these practices and the competences they described in relation to enacting them. We drew quotations from individuals that exemplify the findings to highlight certain thematic areas and to allow greater depth of exploration (participant quotations are presented in and and numbered for easy reference, for example (, 1) refers to quote 1 in ).
Figure 1. Schematic illustration with quotations to show how practice theory can be applied to explore the utilisation of early infant diagnosis. *Blue quotes represent positive aspects of the elements of the practice which might facilitate its enactment while red quotes represent negative aspects which might impede its enactment.
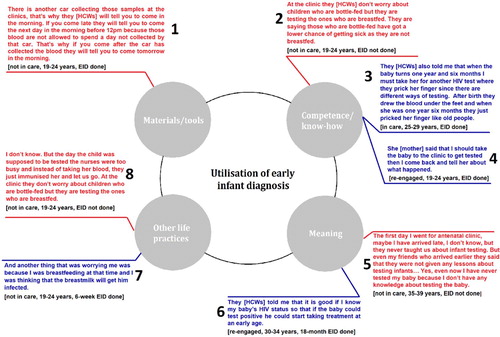
Figure 2. Schematic illustration with quotations to show how practice theory can be applied to explore (dis)engagement with HIV services. *Orange quotes represent what could be interpreted as either positive or negative aspects of an element of a practice which might facilitate or impede its enactment.
Ethics
This study received ethics clearance from the London School of Hygiene and Tropical Medicine, the University of Witwatersrand and the Mpumalanga department of health. All participants provided their written informed consent for the study in addition to the consent they had already provided as participants of the AHDSS. They were informed that their participation was voluntary and that their refusal would not affect the services they received through the healthcare system or result in any loss of benefits pertaining to medical treatment.
Results
Overall, 32 Option B+ women were sampled to participate and 20 were interviewed (three were not at home, five had migrated temporarily or permanently, one could not be found, and three refused to participate). Participants’ ages ranged from 19 to 37 years. Most participants were in informal relationships (12) and had some secondary school education (15) (). Participants came from 11 villages.
Table 1. Demographic and treatment characteristics of the participants and non-participants.
The focus of this analysis is the interrelatedness of the practices of undertaking EID and maternal engagement with HIV services. The different elements of practice theory were seen to underly the enactment or impediment of both EID and engagement in HIV care throughout participants’ narratives and accounts.
Theories of practice and early infant diagnosis of HIV
Materials and tools were necessary for EID often reflecting the level of HIV care infrastructure. For example, one participant mentioned that EID samples were collected at a specific time each day and if mothers brought their infants to test after this time, they would be asked to come back the next day (, 1) which could have major implications for whether EID was performed. One advantage of dried blood spots is their stability at room temperature and might indicate a lack of understanding from the clinic staff which speaks to competence and know-how constellation of practice theory. Competence is further elucidated with some participants mentioning the HCWs’ prioritisation of breastfed infants over those that were bottle-fed (, 2). Competence could be gained through interactions with HCWs (, 3) or from other family members (, 4). Furthermore, if mothers placed some meaning on EID, usually manifested as the need to diagnose their infants expeditiously, they appeared to be more likely to utilise EID (, 6). Finally, maternal engagement in care and breastfeeding emerged as other practices that might help or hinder the utilisation of EID (, 7 & 8).
Theories of practice and engagement in HIV care
Materials and tools were equally important for engagement in HIV care. Lack of funds required for the logistics of remaining engaged in care for example to cover transports costs to the clinic were mentioned by some participants (, 1). Competence was acquired through HCWs and expert clients who helped with counselling patients and equipping them with the tools needed to navigate a life of daily treatment taking, regular clinic visits and stigma management. Where participants accepted this new normal, they were more likely to remain engaged in care (, 2). The meaning participants placed on remaining engaged in care could also help or hinder their continued engagement in care and this meaning could be derived from other practices that were enacted (, 5). Early infant diagnosis emerged as another practice that could affect engagement in care (, 8).
We found that mothers’ continued engagement in care could be undermined by EID especially in instances where the EID experience fostered denial or complicated clinic visits (usually due to scheduling conflicts regarding their infant and their own clinic visits). It could also foster engagement in care by facilitating the acceptance process. Continued engagement in care was of paramount significance in the utilisation of EID ().
Maternal engagement in HIV care and its influence on EID uptake
Engagement with HIV services encouraged uptake of EID by giving it meaning and improving women’s competence and know-how regarding EID. The need for EID was not common knowledge to all the participants at their first antenatal care (ANC) visit, particularly those who were newly diagnosed, younger, or primigravida. However, information and counselling sessions throughout the ANC period ensured that most participants were aware of infant testing by the time of delivery. Consequently, women who disengaged from care early on in their pregnancy missed opportunities to learn about the procedures and benefits of EID (, 5).
Interactions with HCWs (an element associated with engagement in care) provided opportunities to learn about EID and HCWs influenced mothers’ decision to test their infants with some mothers expressing subservience or suggesting they did not have a choice in the matter. In other cases, HCWs were, according to patients, too busy and mothers missed opportunities to undergo EID (, 8). Some mothers felt that priority for EID was given to mothers who breastfed their babies reinforcing their perception that this mode of feeding was riskier than bottle-feeding (, 7), subsequently driving EID uptake.
Infant testing and its influence on maternal engagement in care
The practice of undergoing EID for their babies, and mothers’ responses to the results of the tests, had consequences for their own engagement with HIV care. In most cases, mothers expressed an initial fear of testing their infant, which they had overcome through the desire to know their infant’s HIV status so that they could decide the next appropriate steps to sustain their child’s health. However, a positive infant HIV test result was often met with fear, with little knowledge about the next steps and fear that the child would die if they did not receive proper treatment. Conversely, many women reported that a negative result for their child encouraged them to adhere to their own ART, because they wanted to live long lives to see their children grow up (, 8).
For some mothers who had not fully accepted their own HIV status, the infant test could be seen as proxy for their own HIV status (, 3). However, discordant results for the mother and child often caused confusion and could hinder the acceptance process, or even reinforce denial (, 4). In this example in the participant’s confusion was exacerbated by the fact that the negative HIV status of her child did not correspond with her expectations of it being positive because she had not adhered to HCWs’ advice about taking ART. The use of the child’s status as evidence for the necessity of ART was also seen among some other mothers, for whom the negative HIV status of their child was proof of their own regular treatment-taking. One participant who suggested that she had problems with proving to HCWs that she was taking treatment as prescribed mentioned that the negative result for her infant proved once and for all that she was taking treatment properly.
For some mothers, a confluence of issues relating to EID and the subsequent practice of linking their child to care worked together to undermine their own engagement in care. One participant described how her second born fell ill, was hospitalised, and tested positive while she was in Gauteng province. She moved back to Agincourt and twice attempted to initiate her child on treatment but was unsuccessful because she did not have the child’s paperwork. She also anticipated stigma and maltreatment by the clinic staff at her nearest clinic, but she did not have the finances to travel to a further clinic (, 1). She only wanted to start treatment after she had ‘sorted’ herself out but suggested that she felt far from achieving this. The confusing and difficult time she had with initiating her second born child on ART undermined her trust in the HCWs and undergoing EID this time around (, 5). This late seroconversion undermined her own engagement in care and was reinforced by her fear that her other children might also have HIV and the double burden this would entail (, 7).
Subsequent uptake of infant treatment, for those who tested positive, could interfere with engagement in care for some mothers, especially if they were expected to visit the clinic on separate occasions for their own treatment and that of their infant. Some mothers expressed fatigue at this dual burden of appointments for themselves and their child, which resulted in them prioritising their infant’s treatment over their own, and in some of these cases, the mother stopped going to the clinic all together (, 6).
Discussion
In this study with mothers living with HIV in north-eastern South Africa, we explored the interplay between mothers’ engagement in HIV care and EID, highlighting its complexity and bi-directional nature ().
Our findings build on those from previous studies which have shown that mothers who remained engaged in HIV care were more likely to access EID (Cook et al., Citation2011; Cromwell et al., Citation2015), by describing the aetiology of this relationship. Mothers’ practice of continued engagement in care facilitated EID uptake through improved knowledge about the availability of EID and risk factors for transmission like breastfeeding, and also increased the influence of HCWs over mothers regarding their decision to undergo EID. However, a lack of understanding of vertical transmission for some mothers could also reflect a failing of the HCWs who might either not understand it themselves or might not have taken the appropriate time to communicate effectively with the mothers for a myriad reasons and could reflect an over-burdened system. This highlights the need to consider more innovative solutions to deliver the multiple facets of care like ongoing counselling using lay HCWs (Jennings et al., Citation2011).
Other studies suggest that HCWs are often perceived as authority figures by mothers, leading to mothers’ subservience towards them in the clinic setting (Donahue et al., Citation2012). Whilst mothers who were engaged in care benefited from multiple interactions with HCWs, which often included encouragement to undergo EID, others may have felt pressured to test their infants. Other researchers have noted that the hierarchies of power that are implicitly present in patient-provider relationships can enable potentially coercive practices to increase HIV testing rates among pregnant women (An et al., Citation2015; Angotti et al., Citation2011; Hardon et al., Citation2012; Lyatuu et al., Citation2008), with unintended consequences for women’s disengagement from care in the longer term (Wringe, Moshabela, et al., Citation2017), and similar risks of disengagement should be considered for mothers who feel pressured to test their infants before they feel ready to receive the results. Health workers’ apparent prioritisation of EID for breastfed babies shows that this practice was not solely dependent on the competence of mothers but also that of HCWs. The consequences of this may include missed opportunities for infant testing, as well as driving concern among breastfeeding mothers about HIV transmission risks.
Blue et al. (Citation2016) suggest that the requisite elements necessary for a practice to be enacted are not evenly distributed within society. This coupled with how these practices are reproduced, synchronised and coordinated in daily life and become more deeply embedded than others, helps to explain why some women utilised EID while others did not. Our findings suggest that the practice of EID is linked to other practices such as breastfeeding and immunisation. Conversely, engagement in care is linked to EID and other practices such as maternal testing, with counselling playing a role in how the two practices interact by providing meaning and supporting competencies among women who are enrolled in Option B+. We found that for some mothers who had not accepted their HIV status, the practice of EID could prove detrimental to continued engagement in care especially in the case of a discordant result with the infant. This suggests the need for a better understanding of the ecosystem of practices in which EID and engagement in care are enacted, and how they interact, in order to effectively intervene to improve both the utilisation of EID and engagement with HIV services.
Women responded to EID results in different ways. The process of acceptance of an HIV status is influenced by various events and experiences that are unique to each individual (Horter et al., Citation2017). Our findings suggest that receiving EID results can feed into this process by either helping to confirm or challenge mothers’ beliefs about their own HIV status. Similarly, other studies have also shown how denial of HIV status can manifest itself in repeat testing (Wringe, Moshabela, et al., Citation2017) or use of a partner’s results as a confirmatory test (Wamoyi et al., Citation2017), highlighting the fluid and protracted nature of the acceptance process for some persons living with HIV and the need for ongoing counselling to help some mothers to accept their own status, particularly if it differs from that of their child.
EID facilitated mothers’ engagement in care in many ways. Mothers desired to stay healthy and raise their children, expressing an innate maternal desire to protect their children and mirroring findings around women’s motivation to initiate ART in PMTCT programmes (Clouse et al., Citation2014; McLean et al., Citation2017). When an infant’s HIV results were concordant with their own, EID could also act as an important aid in the mothers’ acceptance process of her own HIV status.
Conversely, for other mothers, a negative result for her infant was seen as proof of their own adherence to treatment, recalling Vale’s notion of the blood ‘panopticon’ whereby blood test results can be a powerful disciplining tool to ensure patients’ continued compliance to health provider rules and expectations, but may also serve to reinforce the patient’s version of their adherence history (Vale et al., Citation2017).
Our findings also highlight the importance of testing mothers throughout the MTCT risk period including breastfeeding, given the additional challenges that mothers may face in accepting their own and their child’s seroconversion after earlier HIV negative results. Country policies regarding postnatal testing for negative mothers vary (Ministry of Health, The United Republic of Tanzania, Citation2017; South Africa: National Department of Health, Citation2016) and are linked to the infant immunisation schedule, although challenges with implementation include other caregivers bringing the infant for immunisation. Nevertheless, given the significant HIV incidence in the postnatal period and the high vertical transmission risk linked to this (Drake et al., Citation2014), more emphasis should be placed on testing during the breastfeeding period.
Conflicting scheduling of clinic visits for mothers and HIV-infected babies led to disengagement from care with mothers prioritising their infant’s visits over their own, in line with results from studies in Malawi and Mozambique (Braun et al., Citation2011; Ciampa et al., Citation2011), highlighting an urgent need for longer-term integrated and coordinated maternal and infant HIV services beyond 6–10 weeks postpartum as one strategy to keep more HIV-infected mothers engaged in care.
Our findings highlighted some important areas for further research. As HIV programmes expand, and more pregnant women living with HIV have initiated ART prior to pregnancy or during past pregnancies, it will be important to explore how experiences and responses to EID utilisation vary between newly diagnosed and experienced ART patients with a view to optimising the timing and frequency of EID counselling for different patients. Future research should also consider adolescent mothers, who often have poorer engagement in HIV care, as their experiences may differ from those of women represented here.
A strength of this study was our ability to include women that were not currently in care, a group that has been underrepresented in previous studies. Nevertheless, their response rate was lower, and it is plausible that some of the women who chose not to be interviewed could have had deferring views from the included participants. Other limitations include the fact that we interviewed participants once, making it difficult to get a sense of the fluidity of their views regarding EID or their engagement in care over time. One-time interviews also meant less time to develop rapport with these women which may have resulted in them speaking less candidly about their experiences in relation to EID and care engagement.
Furthermore, although they did not emerge as findings in our study, other factors have been shown to affect women’s engagement in care which might also influence EID utilisation in other settings, including clinic factors such as stock-outs and disclosure status (Black et al., Citation2014; Iroezi et al., Citation2013). This is perhaps because these were not important issues in this setting or because we did not probe about them. Finally, while the women interviewed for this research share similarities with other sub-Saharan settings, they represent a specific population and findings and conclusions drawn from this research should be interpreted with this in mind.
Conclusions
We found that practice of engagement with HIV care under Option B+ shaped their decision-making around EID. Engagement in care, EID and other practices that patients enact need to be viewed and researched as an interdependent system. A failure to recognise this interconnectedness may lead to outcomes that are counter to expectations. Furthermore, since one size does not fit all with regards to HIV care and treatment, a more practice-centred, differentiated care approach might enable HIV programmes to better serve women living with HIV and their children in the future.
Acknowledgements
The authors would like to thank all the participants in the study. The authors would also like to thank Ella Sihlangu for her contributions to the study. JR is partially supported through DELTA/THRIVE-2 under DEL15-011/07742/Z/15/Z. The study was conceived by DE, GR and AW. DE, AW, JR, GR and FXGO designed the protocol and study tools. Data collection and transcription was performed by VN, SN, PM, MM and DE. Initial coding was conducted by DE, JR, AW, VN, SN, PM and MM. Analyses and interpretation of the findings were conducted by DE, AW and JR. The manuscript was drafted by DE, with input from all authors. All authors read and approved the final manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability
Data will be available for the next five years upon request to the study PI: [email protected]
Additional information
Funding
References
- An, S. J., George, A. S., LeFevre, A., Mpembeni, R., Mosha, I., Mohan, D., Yang, A., Chebet, J., Lipingu, C., Killewo, J., Winch, P., Baqui, A. H., & Kilewo, C. (2015). Program synergies and social relations: Implications of integrating HIV testing and counselling into maternal health care on care seeking. BMC Public Health, 15(1), 24. https://doi.org/10.1186/s12889-014-1336-3
- Ananworanich, J., Gayet-Ageron, A., Le Braz, M., Prasithsirikul, W., Chetchotisakd, P., Kiertiburanakul, S., Munsakul, W., Raksakulkarn, P., Tansuphasawasdikul, S., Sirivichayakul, S., Cavassini, M., Karrer, U., Genné, D., Nüesch, R., Vernazza, P., Bernasconi, E., Leduc, D., Satchell, C., Yerly, S., … Hirschel, B. (2006). CD4-guided scheduled treatment interruptions compared with continuous therapy for patients infected with HIV-1: Results of the Staccato randomised trial. Lancet (London, England), 368(9534), 459–465. https://doi.org/10.1016/S0140-6736(06)69153-8
- Angotti, N., Dionne, K. Y., & Gaydosh, L. (2011). An offer you can’t refuse? Provider-initiated HIV testing in antenatal clinics in rural Malawi. Health Policy and Planning, 26(4), 307–315. https://doi.org/10.1093/heapol/czq066
- Atanga, P. N., Ndetan, H. T., Achidi, E. A., Meriki, H. D., Hoelscher, M., & Kroidl, A. (2017). Retention in care and reasons for discontinuation of lifelong antiretroviral therapy in a cohort of Cameroonian pregnant and breastfeeding HIV-positive women initiating ‘Option B+’ in the South West Region. Tropical Medicine & International Health: TM & IH, 22(2), 161–170. https://doi.org/10.1111/tmi.12816
- Black, S., Zulliger, R., Marcus, R., Mark, D., Myer, L., & Bekker, L.-G. (2014). Acceptability and challenges of rapid ART initiation among pregnant women in a pilot programme, Cape Town, South Africa. AIDS Care, 26(6), 736–741. https://doi.org/10.1080/09540121.2013.855300
- Blue, S., Shove, E., Carmona, C., & Kelly, M. P. (2016). Theories of practice and public health: Understanding (un)healthy practices. Critical Public Health, 26(1), 36–50. https://doi.org/10.1080/09581596.2014.980396
- Braitstein, P., Songok, J., Vreeman, R., Wools-Kaloustian, K., Koskei, P., Walusuna, L., Ayaya, S., Nyandiko, W., & Yiannoutsos, C. (2011). ‘Wamepotea’ (They have become lost): Outcomes of HIV-positive and HIV-exposed children lost to follow-up from a large HIV treatment program in western Kenya. Journal of Acquired Immune Deficiency Syndromes (1999), 57(3), e40–e46. https://doi.org/10.1097/QAI.0b013e3182167f0d
- Braun, M., Kabue, M. M., McCollum, E. D., Ahmed, S., Kim, M., Aertker, L., Chirwa, M., Eliya, M., Mofolo, I., Hoffman, I., Kazembe, P. N., van der Horst, C., Kline, M. W., & Hosseinipour, M. C. (2011). Inadequate coordination of maternal and infant HIV services detrimentally affects early infant diagnosis outcomes in Lilongwe, Malawi. Journal of Acquired Immune Deficiency Syndromes (1999), 56(5), e122–e128. https://doi.org/10.1097/QAI.0b013e31820a7f2f
- Buregyeya, E., Naigino, R., Mukose, A., Makumbi, F., Esiru, G., Arinaitwe, J., Musinguzi, J., & Wanyenze, R. K. (2017). Facilitators and barriers to uptake and adherence to lifelong antiretroviral therapy among HIV infected pregnant women in Uganda: A qualitative study. BMC Pregnancy and Childbirth, 17(1), 94. https://doi.org/10.1186/s12884-017-1276-x
- Cataldo, F., Chiwaula, L., Nkhata, M., van Lettow, M., Kasende, F., Rosenberg, N. E., Tweya, H., Sampathkumar, V., Hosseinipour, M., Schouten, E., Kapito-Tembo, A., Eliya, M., Chimbwandira, F., & Phiri, S. (2017). Exploring the experiences of women and health care workers in the context of PMTCT Option B plus in Malawi. JAIDS Journal of Acquired Immune Deficiency Syndromes, 74(5), 517–522. https://doi.org/10.1097/QAI.0000000000001273
- Chadambuka, A., Katirayi, L., Muchedzi, A., Tumbare, E., Musarandega, R., Mahomva, A. I., & Woelk, G. (2017). Acceptability of lifelong treatment among HIV-positive pregnant and breastfeeding women (Option B+) in selected health facilities in Zimbabwe: A qualitative study. BMC Public Health, 18(1), 57. https://doi.org/10.1186/s12889-017-4611-2
- Ciampa, P. J., Burlison, J. R., Blevins, M., Sidat, M., Moon, T. D., Rothman, R. L., & Vermund, S. H. (2011). Improving retention in the early infant diagnosis of HIV program in rural Mozambique by better service integration. Journal of Acquired Immune Deficiency Syndromes (1999), 58(1), 115–119. https://doi.org/10.1097/QAI.0b013e31822149bf
- Clouse, K., Schwartz, S., Van Rie, A., Bassett, J., Yende, N., & Pettifor, A. (2014). ‘What they wanted was to give birth; nothing else’: Barriers to retention in option B+ HIV care among postpartum women in South Africa. Journal of Acquired Immune Deficiency Syndromes (1999), 67(1), e12–e18. https://doi.org/10.1097/QAI.0000000000000263
- Collins, I. J., Judd, A., & Gibb, D. M. (2014). Immediate antiretroviral therapy in young HIV-infected children: Benefits and risks. Current Opinion in HIV and AIDS, 9(1), 87–94. https://doi.org/10.1097/COH.0000000000000027
- Cook, R. E., Ciampa, P. J., Sidat, M., Blevins, M., Burlison, J., Davidson, M. A., Arroz, J. A., Vergara, A. E., Vermund, S. H., & Moon, T. D. (2011). Predictors of successful early infant diagnosis of HIV in a rural district hospital in Zambézia, Mozambique. Journal of Acquired Immune Deficiency Syndromes (1999), 56(4), e104–e109. https://doi.org/10.1097/QAI.0b013e318207a535
- Cromwell, E. A., Dow, A. E., Low, D., Chirambo, C., Heyderman, R. S., Dube, Q., & Rie, A. V. (2015). Barriers to successful early infant diagnosis of HIV infection at primary care level in Malawi. The Pediatric Infectious Disease Journal, 34(3), 273–275. https://doi.org/10.1097/INF.0000000000000625
- Donahue, M. C., Dube, Q., Dow, A., Umar, E., & Van Rie, A. (2012). ‘They have already thrown away their chicken’: Barriers affecting participation by HIV-infected women in care and treatment programs for their infants in Blantyre, Malawi. AIDS Care, 24(10), 1233–1239. https://doi.org/10.1080/09540121.2012.656570
- Donnell, D., Baeten, J. M., Kiarie, J., Thomas, K. K., Stevens, W., Cohen, C. R., McIntyre, J., Lingappa, J. R., & Celum, C. (2010). Heterosexual HIV-1 transmission after initiation of antiretroviral therapy: A prospective cohort analysis. Lancet (London, England), 375(9731), 2092–2098. https://doi.org/10.1016/S0140-6736(10)60705-2
- Dow, A., Dube, Q., Pence, B. W., & Van Rie, A. (2014). Postpartum depression and HIV infection among women in Malawi. Journal of Acquired Immune Deficiency Syndromes (1999), 65(3), 359–365. https://doi.org/10.1097/QAI.0000000000000050
- Drake, A. L., Wagner, A., Richardson, B., John-Stewart, G., & Mofenson, L. M. (2014). Incident HIV during pregnancy and postpartum and risk of mother-to-child HIV transmission: A systematic review and meta-analysis. PLoS Medicine, 11(2), e1001608. https://doi.org/10.1371/journal.pmed.1001608 Retrieved January 16, 2019 , from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3934828/
- Dzangare, J., Takarinda, K. C., Harries, A. D., Tayler-Smith, K., Mhangara, M., Apollo, T. M., Mushavi, A., Chimwaza, A., Sithole, N., Magure, T., Mpofu, A., Dube, F., & Mugurungi, O. (2016). HIV testing uptake and retention in care of HIV-infected pregnant and breastfeeding women initiated on ‘Option B+’ in rural Zimbabwe. Tropical Medicine & International Health: TM & IH, 21(2), 202–209. https://doi.org/10.1111/tmi.12637
- Strategies for Management of Antiretroviral Therapy (SMART) Study Group, El-Sadr, W. M., Lundgren, J. D., Neaton, J. D., Gordin, F., Abrams, D., Arduino, R. C., Babiker, A., Burman, W., Clumeck, N., Cohen, C. J., Cohn, D., Cooper, D., Darbyshire, J., Emery, S., Fätkenheuer, G., Gazzard, B., Grund, B., Hoy, J., Klingman, K., … Rappoport, C. (2006). CD4+ count-guided interruption of antiretroviral treatment. The New England Journal of Medicine, 355(22), 2283–2296. https://doi.org/10.1056/NEJMoa062360
- Erlwanger, A. S., Joseph, J., Gotora, T., Muzunze, B., Orne-Gliemann, J., Mukungunugwa, S., Farley, T., & Mangwiro, A.-Z. (2017). Patterns of HIV care clinic attendance and adherence to antiretroviral therapy among pregnant and breastfeeding women living with HIV in the context of Option B+ in Zimbabwe. Journal of Acquired Immune Deficiency Syndromes (1999), 75(Suppl 2), S198–S206. https://doi.org/10.1097/QAI.0000000000001347
- Etoori, D., Kerschberger, B., Staderini, N., Ndlangamandla, M., Nhlabatsi, B., Jobanputra, K., Mthethwa-Hleza, S., Parker, L. A., Sibanda, S., Mabhena, E., Pasipamire, M., Kabore, S. M., Rusch, B., Jamet, C., Ciglenecki, I., & Teck, R. (2018). Challenges and successes in the implementation of Option B+ to prevent mother-to-child transmission of HIV in southern Swaziland. BMC Public Health, 18(1), 374. https://doi.org/10.1186/s12889-018-5258-3
- Etoori, D., Wringe, A., Kabudula, C. W., Renju, J., Rice, B., Gomez-Olive, F. X., & Reniers, G. (2020). Misreporting of patient outcomes in the South African national HIV treatment database: Consequences for programme planning, monitoring, and evaluation. Frontiers in Public Health, 8, Frontiers. https://doi.org/10.3389/fpubh.2020.00100 Retrieved March 24, 2020 , from https://www.frontiersin.org/articles/10.3389/fpubh.2020.00100/full#supplementary-material
- Eyawo, O., de Walque, D., Ford, N., Gakii, G., Lester, R. T., & Mills, E. J. (2010). HIV status in discordant couples in sub-Saharan Africa: A systematic review and meta-analysis. The Lancet Infectious Diseases, 10(11), 770–777. https://doi.org/10.1016/S1473-3099(10)70189-4
- Flax, V. L., Hamela, G., Mofolo, I., Hosseinipour, M. C., Hoffman, I. F., & Maman, S. (2017). Factors influencing postnatal Option B+ participation and breastfeeding duration among HIV-positive women in Lilongwe District, Malawi: A qualitative study. PloS One, 12(4), e0175590. https://doi.org/10.1371/journal.pone.0175590
- Gill, M. M., Umutoni, A., Hoffman, H. J., Ndatimana, D., Ndayisaba, G. F., Kibitenga, S., Mugwaneza, P., Asiimwe, A., & Bobrow, E. A. (2017). Understanding antiretroviral treatment adherence among HIV-positive women at four postpartum time Intervals: Qualitative results from the Kabeho study in Rwanda. AIDS Patient Care and STDs, 31(4), 153–166. https://doi.org/10.1089/apc.2016.0234
- Hardon, A., Vernooij, E., Bongololo-Mbera, G., Cherutich, P., Desclaux, A., Kyaddondo, D., Ky-Zerbo, O., Neuman, M., Wanyenze, R., & Obermeyer, C. (2012). Women’s views on consent, counseling and confidentiality in PMTCT: A mixed-methods study in four African countries. BMC Public Health, 12(1), 26. https://doi.org/10.1186/1471-2458-12-26
- Hoffman, R. M., Black, V., Technau, K., van der Merwe, K. J., Currier, J., Coovadia, A., & Chersich, M. (2010). Effects of highly active antiretroviral therapy duration and regimen on risk for mother-to-child transmission of HIV in Johannesburg, South Africa. Journal of Acquired Immune Deficiency Syndromes (1999), 54(1), 35–41. https://doi.org/10.1097/QAI.0b013e3181cf9979
- Horter, S., Thabede, Z., Dlamini, V., Bernays, S., Stringer, B., Mazibuko, S., Dube, L., Rusch, B., & Jobanputra, K. (2017). ‘Life is so easy on ART, once you accept it’: Acceptance, denial and linkage to HIV care in Shiselweni, Swaziland. Social Science & Medicine (1982), 176, 52–59. https://doi.org/10.1016/j.socscimed.2017.01.006
- Iroezi, N. D., Mindry, D., Kawale, P., Chikowi, G., Jansen, P. A., & Hoffman, R. M. (2013). A qualitative analysis of the barriers and facilitators to receiving care in a prevention of mother-to-child program in Nkhoma, Malawi. African Journal of Reproductive Health, 17(4 Spec No), 118–129.
- Jennings, L., Yebadokpo, A. S., Affo, J., Agbogbe, M., & Tankoano, A. (2011). Task shifting in maternal and newborn care: A non-inferiority study examining delegation of antenatal counseling to lay nurse aides supported by job aids in Benin. Implementation Science: IS, 6(1), 2. https://doi.org/10.1186/1748-5908-6-2
- Kahn, K., Collinson, M. A., Gómez-Olivé, F. X., Mokoena, O., Twine, R., Mee, P., Afolabi, S. A., Clark, B. D., Kabudula, C. W., Khosa, A., Khoza, S., Shabangu, M. G., Silaule, B., Tibane, J. B., Wagner, R. G., Garenne, M. L., Clark, S. J., & Tollman, S. M. (2012). Profile: Agincourt health and socio-demographic surveillance system. International Journal of Epidemiology, 41(4), 988–1001. https://doi.org/10.1093/ije/dys115
- Kalk, E., Kroon, M., Boulle, A., Osler, M., Euvrard, J., Stinson, K., Timmerman, V., & Davies, M.-A. (2018). Neonatal and infant diagnostic HIV-PCR uptake and associations during three sequential policy periods in Cape Town, South Africa: A longitudinal analysis. Journal of the International AIDS Society, 21(11), e25212. https://doi.org/10.1002/jia2.25212
- Katirayi, L., Chouraya, C., Kudiabor, K., Mahdi, M. A., Kieffer, M. P., Moland, K. M., & Tylleskar, T. (2016). Lessons learned from the PMTCT program in Swaziland: Challenges with accepting lifelong ART for pregnant and lactating women – a qualitative study. BMC Public Health, 16(1), 1119. https://doi.org/10.1186/s12889-016-3767-5
- Katirayi, L., Namadingo, H., Phiri, M., Bobrow, E. A., Ahimbisibwe, A., Berhan, A. Y., Buono, N., Moland, K. M., & Tylleskär, T. (2016). HIV-positive pregnant and postpartum women’s perspectives about Option B+ in Malawi: A qualitative study. Journal of the International AIDS Society, 19(1), 20919. Retrieved September 16, 2017 , from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4911420/ https://doi.org/10.7448/IAS.19.1.20919
- Kim, M. H., Zhou, A., Mazenga, A., Ahmed, S., Markham, C., Zomba, G., Simon, K., Kazembe, P. N., & Abrams, E. J. (2016). Why did I stop? Barriers and facilitators to uptake and adherence to ART in Option B+ HIV care in Lilongwe, Malawi. PloS One, 11(2), e0149527. https://doi.org/10.1371/journal.pone.0149527
- Kippax, S., Stephenson, N., Parker, R. G., & Aggleton, P. (2013). Between individual agency and structure in HIV prevention: Understanding the middle ground of social practice. American Journal of Public Health, 103(8), 1367–1375. https://doi.org/10.2105/AJPH.2013.301301
- Knettel, B. A., Cichowitz, C., Ngocho, J. S., Knippler, E. T., Chumba, L. N., Mmbaga, B. T., & Watt, M. H. (2017). Retention in HIV care during pregnancy and the postpartum period in the Option B+ era: A systematic review and meta-analysis of studies in Africa. JAIDS Journal of Acquired Immune Deficiency Syndromes, Publish Ahead of Print. Retrieved January 7, 2018 , from http://journals.lww.com/jaids/Abstract/publishahead/Retention_in_HIV_Care_During_Pregnancy_and_the.96776.aspx
- Kranzer, K., & Ford, N. (2011). Unstructured treatment interruption of antiretroviral therapy in clinical practice: A systematic review. Tropical Medicine & International Health: TM & IH, 16(10), 1297–1313. https://doi.org/10.1111/j.1365-3156.2011.02828.x
- Lazarus, R., Struthers, H., & Violari, A. (2009). Hopes, fears, knowledge and misunderstandings: Responses of HIV-positive mothers to early knowledge of the status of their baby. AIDS Care, 21(3), 329–334. https://doi.org/10.1080/09540120802183503
- Lyatuu, M. B., Msamanga, G. I., & Kalinga, A. K. (2008). Clients’ satisfaction with services for prevention of mother-to-child transmission of HIV in Dodoma rural district. East African Journal of Public Health, 5(3), 174–179. https://doi.org/10.4314/eajph.v5i3.38999
- McLean, E., Renju, J., Wamoyi, J., Bukenya, D., Ddaaki, W., Church, K., Zaba, B., & Wringe, A. (2017). ‘I wanted to safeguard the baby’: A qualitative study to understand the experiences of Option B+ for pregnant women and the potential implications for ‘test-and-treat’ in four sub-Saharan African settings. Sexually Transmitted Infections, 93(Suppl 3), e052972. https://doi.org/10.1136/sextrans-2016-052972
- Ministry of Health, Government of Malawi. (2012). Integrated HIV Program Report July—September 2012.
- Ministry of Health, The United Republic of Tanzania. (2017). National guidelines for the management of HIV and AIDS. www.nacp.go.tz/site/download/NATIONAL_DECEMBER_2017.pdf
- Napúa, M., Pfeiffer, J. T., Chale, F., Hoek, R., Manuel, J., Michel, C., Cowan, J. G., Cowan, J. F., Gimbel, S., Sherr, K., Gloyd, S., & Chapman, R. R. (2016). Option B+ in Mozambique: Formative research findings for the design of a facility-level clustered randomized controlled trial to improve ART retention in antenatal care. Journal of Acquired Immune Deficiency Syndromes (1999), 72(Suppl 2), S181–S188. https://doi.org/10.1097/QAI.0000000000001061
- Ngarina, M., Tarimo, E. A. M., Naburi, H., Kilewo, C., Mwanyika-Sando, M., Chalamilla, G., Biberfeld, G., Ekstrom, A. M., & Thorne, C. (2014). Women’s preferences regarding infant or maternal antiretroviral prophylaxis for prevention of mother-to-child transmission of HIV during breastfeeding and their views on Option B+ in Dar es Salaam, Tanzania. PloS One, 9(1), e85310. https://doi.org/10.1371/journal.pone.0085310
- Nuwagaba-Biribonwoha, H., Jakubowski, A., Mugisha, V., Basinga, P., Asiimwe, A., Nash, D., & Elul, B. (2014). Low risk of attrition among adults on antiretroviral therapy in the Rwandan national program: A retrospective cohort analysis of 6, 12, and 18 month outcomes. BMC Public Health, 14(1), 889. https://doi.org/10.1186/1471-2458-14-889
- SAPMTCTE study group. (2012). Evaluation of the Effectiveness of the National Prevention of Mother-to-Child Transmission (PMTCT) Programme Measured at Six Weeks Postpartum in South Africa, 2010. Retrieved September 19, 2017 , from http://www.mrc.ac.za/healthsystems/SAPMTCTE2010.pdf
- Schatzki, T. R. (2002). The site of the social: A philosophical account of the constitution of social life and change. Penn State Press.
- Shove, E., Pantzar, M., & Watson, M. (2012). The dynamics of social practice: Everyday life and how it changes. SAGE.
- Sibanda, E. L., Weller, I. V. D., Hakim, J. G., & Cowan, F. M. (2013). The magnitude of loss to follow-up of HIV-exposed infants along the prevention of mother-to-child HIV transmission continuum of care: A systematic review and meta-analysis. AIDS (London, England), 27(17), 2787–2797. https://doi.org/10.1097/QAD.0000000000000027
- Skovdal, M. (2019). Facilitating engagement with PrEP and other HIV prevention technologies through practice-based combination prevention. Journal of the International AIDS Society, 22(Suppl 4), e25294. https://doi.org/10.1002/jia2.25294
- Skovdal, M., Maswera, R., Kadzura, N., Nyamukapa, C., Rhead, R., Wringe, A., & Gregson, S. (2018). Parental obligations, care and HIV treatment: How care for others motivates self-care in Zimbabwe. Journal of Health Psychology, 1359105318788692. Advance online publication. https://doi.org/10.1177/1359105318788692
- Skovdal, M., Wringe, A., Seeley, J., Renju, J., Paparini, S., Wamoyi, J., Moshabela, M., Ddaaki, W., Nyamukapa, C., Ondenge, K., Bernays, S., & Bonnington, O. (2017). Using theories of practice to understand HIV-positive persons varied engagement with HIV services: A qualitative study in six Sub-Saharan African countries. Sexually Transmitted Infections, 93(Suppl 3), e052977. https://doi.org/10.1136/sextrans-2016-052977
- South Africa: National Department of Health. (2015). National Consolidated Guidelines for PMTCT and the Management of HIV in Children, Adolescents and Adults. Retrieved March 30, 2017 , from https://www.health-e.org.za/2015/07/02/guidelines-national-consolidated-guidelines-for-pmtct-and-the-management-of-hiv-in-children-adolescents-and-adults/
- South Africa: National Department of Health. (2016). National HIV testing services: Policy. https://sahivsoc.org/Files/HTS%20Policy%2028%20July%20final%20copy.pdf
- Stinson, K., & Myer, L. (2012). Barriers to initiating antiretroviral therapy during pregnancy: A qualitative study of women attending services in Cape Town, South Africa. African Journal of AIDS Research: AJAR, 11(1), 65–73. https://doi.org/10.2989/16085906.2012.671263
- Tenthani, L., Haas, A. D., Tweya, H., Jahn, A., van Oosterhout, J. J., Chimbwandira, F., Chirwa, Z., Ng’ambi, W., Bakali, A., Phiri, S., Myer, L., Valeri, F., Zwahlen, M., Wandeler, G., & Keiser, O. (2014). Retention in care under universal antiretroviral therapy for HIV-infected pregnant and breastfeeding women (‘Option B+’) in Malawi. AIDS (London, England), 28(4), 589–598. https://doi.org/10.1097/QAD.0000000000000143
- UNAIDS. (2011). Countdown to zero: Global plan towards the elimination of new HIV infections among children by 2015 and keeping their mothers alive. Retrieved September 3, 2017 , from http://www.unaids.org/sites/default/files/media_asset/20110609_JC2137_Global-Plan-Elimination-HIV-Children_en_1.pdf
- UNAIDS. (2015). 2015 Progress report on the global plan towards the elimination of new HIV infections among children and keeping their mothers alive. Retrieved September 3, 2017 , from http://www.unaids.org/sites/default/files/media_asset/JC2774_2015ProgressReport_GlobalPlan_en.pdf
- Vale, B., Hodes, R., Cluver, L., & Thabeng, M. (2017). Bureaucracies of blood and belonging: Documents, HIV-positive youth and the State in South Africa. Development and Change, 48(6), 1287–1309. https://doi.org/10.1111/dech.12341
- van Lettow, M., Bedell, R., Mayuni, I., Mateyu, G., Landes, M., Chan, A. K., van Schoor, V., Beyene, T., Harries, A. D., Chu, S., Mganga, A., & van Oosterhout, J. J. (2014). Towards elimination of mother-to-child transmission of HIV: Performance of different models of care for initiating lifelong antiretroviral therapy for pregnant women in Malawi (Option B+). Journal of the International AIDS Society, 17(1), 18994. https://doi.org/10.7448/IAS.17.1.18994
- Violari, A., Cotton, M. F., Gibb, D. M., Babiker, A. G., Steyn, J., Madhi, S. A., Jean-Philippe, P., & McIntyre, J. A. (2008). Early antiretroviral therapy and mortality among HIV-infected infants. The New England Journal of Medicine, 359(21), 2233–2244. https://doi.org/10.1056/NEJMoa0800971
- Wamalwa, D., Benki-Nugent, S., Langat, A., Tapia, K., Ngugi, E., Slyker, J. A., Richardson, B. A., & John-Stewart, G. C. (2012). Survival benefit of early infant antiretroviral therapy is compromised when diagnosis is delayed. The Pediatric Infectious Disease Journal, 31(7), 729–731. https://doi.org/10.1097/INF.0b013e3182587796
- Wamoyi, J., Renju, J., Moshabela, M., McLean, E., Nyato, D., Mbata, D., Bonnington, O., Seeley, J., Church, K., Zaba, B., & Wringe, A. (2017). Understanding the relationship between couple dynamics and engagement with HIV care services: Insights from a qualitative study in Eastern and Southern Africa. Sexually Transmitted Infections, 93(Suppl 3), e052976. https://doi.org/10.1136/sextrans-2016-052976
- WHO. (2015). Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV. WHO guidelines approved by the guidelines review committee. World Health Organization. Retrieved March 28, 2017 , from http://www.ncbi.nlm.nih.gov/books/NBK327115/
- Wringe, A., Moshabela, M., Nyamukapa, C., Bukenya, D., Ondenge, K., Ddaaki, W., Wamoyi, J., Seeley, J., Church, K., Zaba, B., Hosegood, V., Bonnington1, O., Skovdal, M., & Renju, J. (2017). HIV testing experiences and their implications for patient engagement with HIV care and treatment on the eve of ‘test and treat’: Findings from a multicountry qualitative study. Sexually Transmitted Infections, 93(Suppl 3), e052969. https://doi.org/10.1136/sextrans-2016-052969
- Wringe, A., Renju, J., Seeley, J., Moshabela, M., & Skovdal, M. (2017). Bottlenecks to HIV care and treatment in sub-Saharan Africa: A multi-country qualitative study. Sexually Transmitted Infections, 93(Suppl 3), e053172. https://doi.org/10.1136/sextrans-2017-053172