ABSTRACT
Patients with drug-resistant tuberculosis (DR-TB) have received community-based care in Eswatini since 2009. Trained and compensated community treatment supporters (CTSs) provide directly observed therapy (DOT), injectables and psychological support. We examined the acceptability of this model of care among DR-TB patients, including the perspective of family members of DR-TB patients and their CTSs in relation to the patient’s experience of care and quality of life. This qualitative research was conducted in rural Eswatini in February 2018. DR-TB patients, CTSs and family members participated in in-depth interviews, paired interviews, focus group discussions and PhotoVoice. Data were thematically analysed and coded, and themes were extracted. Methodological triangulation enhanced the interpretation. All patients and CTSs and most family members considered community-based DR-TB care to be supportive. Positive aspects were emotional support, trust and dedicated individual care, including enabling practical, financial and social factors. Concerns were related to social and economic problems within the family and fears about infection risks for the family and the CTSs. Community-based DR-TB care was acceptable to patients, family members and CTSs. To reduce family members’ fears of TB infection, information and sensitisation within the family and constant follow-up appear crucial.
Introduction
Drug-resistant tuberculosis (DR-TB) is a serious public health threat in resource-limited settings (RLS) where access to care, diagnosis, and treatment initiation and continuation remain challenging (WHO, Citation2018). In 2017 only an estimated 30% of all DR-TB cases in Africa were laboratory diagnosed and treatment outcomes remained suboptimal (WHO, Citation2018). Failure to improve DR-TB care in RLS reduces the chances of ending TB epidemic by 2030 (WHO, Citation2017).
The World Health Organization (WHO) recommends ambulatory DR-TB care comprising clinic-based and community-based service delivery (WHO, Citation2014). In clinic-based care, patients travel daily to facilities for directly observed therapy (DOT) and injectables during the intensive phase for approximately eight months. In community-based care, daily treatment delivery occurs in the community, provided by either nurses or trained lay cadres (Seung et al., Citation2009).
Community-based DR-TB care with involvement of trained lay people has the potential to overcome barriers to access and to facilitate uninterrupted treatment for rural populations and patients with socio-economic constraints (USAID, Citation2017; WHO, Citation2008). Few studies have looked at the quality of care of DR-TB services from the patients’ perspective, and those that have shown poor experiences for affected patients (Daftary et al., Citation2014; Guo et al., Citation2009; Isaakidis et al., Citation2013; Laxmeshwar et al., Citation2019; Shringarpure et al., Citation2016; Singla et al., Citation2009; Udwadia & Furin, Citation2019). Community-based DR-TB care may have the potential to provide patient-centred social and emotional support (USAID, Citation2017). This model of care has been shown to be feasible in rural Eswatini and in a similar setting in Lesotho, achieving favourable treatment outcomes at acceptable costs (Kerschberger et al., Citation2019; Satti et al., Citation2012; Seung et al., Citation2009). However, experiences and perceptions of DR-TB patients regarding community-based DR-TB care remain unstudied.
This paper presents the experiences and perceptions of patients receiving community-based DR-TB care in rural Eswatini, as well as the experiences and perceptions of CTSs and family members of patients. The results are part of a larger study conducted for Médecins Sans Frontières (MSF) Switzerland to document the acceptability of the implemented community-based DR-TB care model to patients, CTSs, and family and community members. We aim to inform health policy and to contribute to the discussion on expansion and implementation of quality DR-TB care in RLS.
Methods
Study design
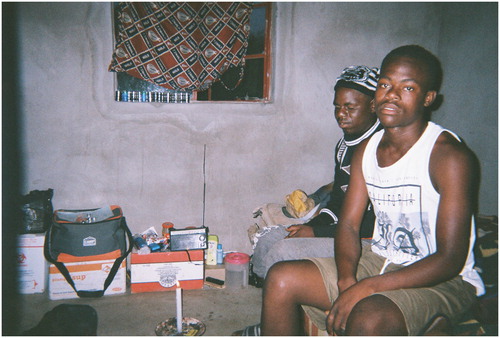
This study applied an exploratory qualitative research design (Skovdal & Flora, Citation2015) and used 26 in-depth individual interviews (IDIs), three paired interviews, two focus group discussions (FDGs) and PhotoVoice in the Shiselweni region (Eswatini) in February 2018.
PhotoVoice was used as a culturally sensitive participatory approach to involve mostly HIV co-infected DR-TB patients actively in the research. This visual representation technique combined with interactive discussions gave economically and socially disadvantaged DR-TB patients a voice to tell their stories, revealing their everyday realities with DR-TB treatment. Visual participatory methods play an important role in qualitative research as they provide contextual information (Blackman & Fairey, Citation2007; Daniel & Logie, Citation2016; Mitchell et al., Citation2005; Mohammed et al., Citation2013; O’Donovan et al., Citation2020; Teti et al., Citation2015; Wang & Burris, Citation1997). IDIs and paired interviews were conducted while patients and CTSs took photos to gain in-depth understanding of patients’ CTSs’ and family members’ perception of and experience with community-based DR-TB treatment. FGDs gave insight into communities’ views on this model of care.
The primary analysis focused on the acceptance of community-based care by patients enrolled into this model of care, including their CTSs and family members.
Setting
The Shiselweni region (population 204,000 (Central Statistical Office of Eswatini. The 2017 Population and Housing Census Preliminary Results, Citation2017)) has an HIV prevalence of 32% among adults aged 18–47 years (Bicego et al., Citation2013) and an estimated TB incidence of 308 cases per 100,000 population (WHO, Citation2018). Among TB cases, 8% of new and 34% of re-treatment cases were infected with multidrug-resistant TB (Sanchez-Padilla et al., Citation2012), of which 79% had HIV co-infection (Kerschberger et al., Citation2019).
The National TB Control Programme (NTCP) and MSF have provided ambulatory DR-TB care since 2008 (Kerschberger et al., Citation2019). A two-week hospitalisation was encouraged at treatment initiation and HIV co-infected patients were initiated on antiretroviral therapy. Thereafter, clinic-based care was offered to patients without access constraints to health facilities where they received daily DOT and injectables for DR-TB treatment. According to standard operating procedures, patients were eligible for community-based care if they had difficulties in daily access to health facilities for whatsoever reason, including living in remote locations, having socio-economic constraints and being stigmatised or immobile (e.g. age, disability). Volunteer lay people living near patients’ homes were identified by the TB nurse and the patients to become CTSs. The CTSs received a theoretical and practical training over two weeks and monetary compensation for providing DR-TB care support, including daily DOT and intramuscular injections at the patient’s home during the intensive phase. The community TB nurse visited the homestead at least twice a month for supportive visits and could be contacted by phone by the patient and CTS in case of any medical needs. The patient and CTS attended secondary facilities once a month for clinical and laboratory follow-up, support groups and drug refills. Patients received a travel allowance and food package to support treatment adherence. All care provided was free.
Study population and sampling
Purposive sampling was applied to include patients facing constraints in access to treatment; the sample size was based on the notion of saturation (O'Reilly & Parker, Citation2012). Firstly, criterion sampling was used for patients of both sexes and different ages based on the criteria of receiving community-based DR-TB care during the intensive phase in remote locations. Secondly, patient’s CTS and one family member were interviewed. This approach enabled triangulation of the results from each participant group, comparing how they concurred and diverged in terms of findings. Lastly, interviews with health workers involved in the delivery of community-based care were conducted. The characteristics of study participants are presented in .
Table 1. Characteristics of main participants.
Data collection
provides an overview of data collection methods used. Firstly, an introductory session to PhotoVoice was run at the MSF office in the Shiselweni region as a culturally sensitive participatory method (Cannuscio et al., Citation2009; Wang & Burris, Citation1997). Patients and their CTSs attended a half-day workshop where PhotoVoice was explained to them, and they received disposable cameras for one week including guiding questions to take pictures of issues related to the DR-TB treatment experience. Secondly, patients, CTSs, family members and one TB counsellor were individually interviewed at the home of the patient or the CTS or at the facility, while patients and CTSs took photographs. Nearly all individual interviews were conducted before the PhotoVoice release workshop; three IDIs with patients and four IDIs with CTSs were done after this. Thirdly, patients and CTS attended a one-day photo-release workshop to select and present three photographs to the group. The photos provided the participant’s interpretation and meaning regarding community-based DR-TB care. Fourthly, paired interviews were conducted with family members at the patient’s home and with a TB nurse and TB counsellor at the facility. Different topic guides were used for the interviews and FDGs, with a photo reflection sheet for the photo-release workshops.
Table 2. Overview of data collection methods and number of interviews conducted.
Analysis
All interviews were conducted by the principal investigator (DB), either in English or in Siswati with the help of a female or male translator, audio-recorded and transcribed verbatim directly from Siswati into English. Recorded discussions and notes of the presentations from the photo-release workshops, each photograph and its accompanying description, whether written or spoken, transcriptions of IDIs and FGDs, and notes taken during or after any encounters formed the basis for the analysis. An iterative and inductive approach was applied (Green & Thorogood, Citation2018), reviewing notes and interview transcripts as they were transcribed in the field to draw preliminary observations related to the research questions. An initial set of conceptual codes was identified by the principal investigator and the two research assistants in collaboration. The principal investigator analysed and coded the notes and interview transcripts manually and the research assistants coded in NVivo 11, systematically applying codes to blocks of text (usually of three to five sentences in length). Data validation was ensured through a methodological triangulation by combining in-depth individual interviews with group discussions, PhotoVoice and document reviews (Green & Thorogood, Citation2018; Patton, Citation2002), and emergent themes were tested by examining exceptions and counter examples.
Ethics
The study protocol was approved by the MSF Ethics Review Board and the National Health Research Review Board of Eswatini. All participants provided written informed consent before study enrolment.
Results
Patients, CTSs and most family members considered community-based DR-TB care to be a supportive and appropriate care model and in most instances preferred this model to the facility-based care model. From the analysis, three overall themes emerged in relation to life quality and quality of DR-TB treatment and care: ‘Everyday life continuity’, ‘supportive and professional care’, and ‘infection risk and care responsibility’.
Everyday life continuity
For DR-TB patients, being able to continue everyday life to some degree, being with family and keeping social networks intact while on treatment were of great importance and an essential aspect of what they most appreciated about the community-based care. In that sense, patients were able to keep their social roles of being a head of family, a father, a spouse or a friend and were not only seen as a patient.
Patients valued being at home to keep their social relations with other family members, being in direct contact with them, something that could be difficult if hospitalised:
Being treated at home, it’s a good thing because, at home they are able to visit, to greet you, even if they don’t have money. Even that alone can make you feel better, feel at home. In my home the economy is not good, so going to the hospital takes time to give you those fruits or something small [meaning money]. Male patient, 32 years
There would be an emotional challenge, if it would be there [hospital], because when I’m treated there then it means I wouldn’t be able to see my children and really it would affect me. Female patient, 32 years
I’ve seen that at first he [patient] had fear, that now that I have DR-TB, it may mean that I’ll die, as you [MSF] visited him, I’ve seen that he is getting relaxed emotionally, and he is gaining weight and hasn’t changed. I can see that all this is due to that he accepted his condition and that you [MSF] are with [treat] him. Female and male family member, 35 and 34 years
At the same time, some patients evoked the risk of being emotionally stressed and disturbed in the facility because of other sick patients admitted there, and additional distress was caused by unfriendly and harsh medical staff who do not know the patient well while having many other patients to care for. Patients did not feel ‘free’ and could not go out to meet friends and relatives or buy basic things like soap or fruits. Patients also mentioned limited opportunities in relation to sleeping and food, as in the facility they would not be able to decide when to sleep or when and what to eat because they have fixed eating times; occasionally patients feel dizzy and unwell after the injections and even do not want to eat at all.
It’s like you are in jail, arrested. I can say that it’s like you are arrested you see. Because you are not able to go to the shops to buy … you need to ask those relatives to carry for you. If you don’t have relatives, then nothing! Male patient, 45 years
When he is treated in the hospital, he feels like, he is just in jail, he is unable, he is not free, he can’t even see his relatives, he just can’t do what he wants to do, you see, just like at home! CTS, 40 years
The way you eat at the hospital, when they say ‘here is food’ you are indeed supposed to eat that, you don’t have a choice. Male patient, 25 years
With this picture I want to show that my livestock are under my supervision now since I am [treated] at home. After taking medication, I am able to check on my animals and feed them. Male patient, 41 years
Financial support to the patient (travel allowance and food) also helped families by reducing the family’s direct expenses for food.
The patients are too far from the facilities; when we visited them they are saying, having the MSF staff coming to the community is like having money in your bank account. Female counsellor, 37 years
Supportive and professional care
Patients, family members and CTSs highlighted positive aspects of facility-based DR-TB care and community-based DR-TB care depending on the situation. For patients, the support they received from their treatment supporter was linked to adherence to treatment and retention on treatment, and they mentioned how ‘encouraging words’ and ‘positive stories’ of other DR-TB patients helped them to continue treatment:
I am helped most by my treatment supporter. She has words of encouraging me, even if I feel that my strength is going down, it’s my treatment supporter who has the big support that I have the energy to continue to take my treatment. Male patient, 33 years
What she [CTS] supports me with is that she encourages me that I will be well, taking the pills properly. She [CTS] uses others as examples, those who survived, that ‘there is that one, they survived too.’ Even with food, she says that I should try to eat well and I should drink the pills after having eaten. Male patient, 31 years
In the hospital, you get disturbed, there is someone dying nearby you, yet when you are here [at home] you become stress-free you see. Male patient, 32 years
She [CTS] has greatly supported me … even emotionally, because all homes can never be the same that everything is always perfect, so I am able to confide everything [family problems] to her and then she is able to help me. Male patient, 45 years
I chose this picture to show gratitude to my CTS for agreeing to help me because the care I get from her is better than hospital care. Male patient, 31 years
I took the picture of them [patient and his brother] to show that X [patient] is open with me. We sometimes sit down and talk about life and what stresses him. He treats me like his mother. CTS, 49 years
This work, it’s a difficult job which needs a calm heart or love. Have love for it because you have to think for the patient that, it may happen that after finishing to get an injection they feel like their bones, the body is feeling sleepy. CTS, 54 years
Infection risk and care responsibility
While DR-TB community care was positively valued by patients, family members and CTSs, especially in relation to adherence to treatment and retention on treatment, DR-TB care within health facilities was appreciated for the routine monitoring of the condition and gave a sense of security in cases where the condition of the patient was more serious:
What is better in the hospital, I can say that every Monday morning the doctor comes and asks you, checks you if you have any problem. Also that BP [blood pressure] and temperature is checked always, every day. Male patient, 25 years
The good thing about being treated in the hospital is that if there is any change occurring in your condition, you usually get quickly help because they [health professionals] have sufficient knowledge and sufficient education. They know if a person is doing, what they are supposed to do in helping him. They are able to see the mysteries of a condition, and are able to know when they should refer that patient to someone else. At the hospital they are special trained. Male patient, 32 years
It [facility-based treatment] is good in a case or event when he [the patient] is very sick, it’s okay that he gets treated in the hospital because we may not have the knowledge of what to do since he is very sick, I wouldn’t know how I can help him. Female family member, 59 years
One thing that I feel is wrong, you see, my mother [patient] and there’s that child [mother’s grandchild], once she gets the injection, she gets drowsy and she’s lying down. I’m the one who is going to cook for her and taking the plate from her room. I am not comfortable entering her room; not because I discriminate her but I am still young and look for job opportunities; so when I enter her room and then find out that I’m now having this disease it will not go down well with me because you aren’t going to work if they know you have TB. Male family member, 27 years
It is very true when it is found that one is having TB legwamile [DR-TB], there is fear, and then the fear decreases after we have been told at the hospital that ‘you don’t have it’ after being tested and then also we get told on how to live at home. In real sense, there is the fear. Female and male family member, 35 and 34 years
I try and encourage her and say my child in the way you’re going you’ll survive this but you just have to be patient, when you follow what the doctors are saying you’ll live longer, but then she wouldn’t understand you because drinking and smoking is nice yet she knows that the treatment is affected by such, like when going to the bar she’ll take the treatment with. CTS, 78 years
The husband [of the patient] would go and drink alcohol saying he’s drowning his sorrows and his stress and when he comes back, he gets into his room and sleeps. … that is what sparked the fights. CTS, 49 years
Yes it’s a good thing that I see and that they [MSF] do follow ups on the patients and visit; you would see by the car coming such that if there is a problem, maybe you are not well maybe you are lying down because of the pills, if you call MSF for help, they can always come at any time. Male family member, 34 years
It’s good to me, I see it good because I get to see and monitor his condition and if there is something I see that is not okay, I was able to call the nurses who will promptly come and assist and try to assess the situation. Female family member, 59 years
Maybe [I] am not protected 100% but I usually tell myself that there are verses I usually read. In the holy book there is where it says God protects us even in diseases that are contagious. I then sacrificed myself wholly that aaay let me help him because even to me one day, either my relative or my child will be like this and a person will be needed to look after them. CTS, 49 years
It is not dangerous, and I don’t see any risks because I sleep alone in my room like they told me, my children are sleeping with their grandmother and my husband sleeps in his own [room]. Female patient, 32 years
I want to say that, they [facility] have their own place where they [DR-TB patients] stay, so you or someone else who is okay, who doesn’t have the TB, maybe the chances of getting the TB are low. Female family member, 33 years
Another good thing about being treated at the hospital is that you’re going to sleep on a clean bed and maybe at home there wouldn’t be anyone to make sure the bedding is clean and that might lead to other infections. Male family member, 27 years
Discussion
Community-based DR-TB care has been used in different resource-poor contexts where it has been shown to be feasible and has achieved favourable treatment outcomes for patients (Arshad et al., Citation2014; Brust et al., Citation2012; Colvin et al., Citation2014; Demissie et al., Citation2003; Duwell et al., Citation2013; Escott & Walley, Citation2005; Farmer & Kim, Citation1998; Hadley & Maher, Citation2000; Heller et al., Citation2010; Hendrix-Jenkins, Citation2008; Horter et al., Citation2014; Shin et al., Citation2004; WHO, Citation2008). This study, explored patients’, family members’ and CTSs’ perceptions and experiences of this model of care with regards to involvement of trained lay people by using different qualitative approaches including the visual PhotoVoice method. Overall, the study found that community-based care was an encouraging experience for patients and families and was the favoured model of care over facility-based DR-TB treatment, which should be envisaged only for the very sick patients.
Findings in context
Study findings suggest that community-based care with involvement of CTSs for treatment and patient support was preferred by all patients who were involved in the programme, their treatment supporters and their family members. Other studies that examined community-based models of DR-TB care complement these findings, showing that this model of care is feasible and acceptable (Arshad et al., Citation2014; Colvin et al., Citation2014; Demissie et al., Citation2003; Heller et al., Citation2010; Horter et al., Citation2014). It was seen as a supportive and professional model of care that was conducive to patients’ emotional and mental condition and physical well-being to continue everyday life. It allowed patients to feel ‘free’ and be with their families in their own homes and, most importantly, it gave patients a sense of self-esteem and respect of being recognised as an individual and not just a patient. For family members witnessing and patients themselves observing their recovery was a positive experience that influenced DR-TB perception in general and reduced fears of the disease.
Community-based DR-TB was characterised not only by a close and trustful relationship between the patient and the CTS but also by dedicated individual quality care for the patient (Escott & Walley, Citation2005; Horter et al., Citation2014). CTSs’ empathy to care for patients and the time and devotion they addressed to them was highly valued by patients, as nicely addressed in a similar study (Snyman et al., Citation2018). CTSs on the other hand went through a process of empowerment by acquiring a role of responsibility, learning new skills, and gaining a feeling of self-worth and a sense of professionalism, which stands in strong contrast to findings from another study on community health workers’ experiences (O’Donovan et al., Citation2020). While some health care providers still had doubts about trained CTSs giving injections, they also recognised the benefit in terms of workload reduction (WHO, Citation2008). Notably, these concerns should be eliminated with the expansion of fully oral DR-TB treatment regimens, thus possibly facilitating the use of CTSs. WHO allows for community-based treatment by trained lay people but acknowledges that operationalisation might be challenging due to legal requirements and social traditions (WHO, Citation2014). However, study results show that patients and family members follow the rules and respect the conditions put on them in relation to community-based treatment. The authors believe that both the local context and the patient’s needs should be considered for the delivery of community-based care in an acceptable way.
Community-based care is a favourable model of care for stable patients, particularly in terms of adherence to and retention on treatment, with the CTSs closely supported by the DR-TB nurses of the programme. Study findings clearly suggest that facility-based care is valued for patients who have serious health conditions and need close monitoring by DR-TB professionals. Challenges with community-based DR-TB care were mainly related to worries about infection risks in the homes and social and economic problems within the families (Escott & Walley, Citation2005). In a similar study, patients who were treated at home did not see higher risks of infection but expressed concerns about nosocomial infections (Horter et al., Citation2014). Knowledge of such concerns before the implementation of this model of care enabled anxieties to be mitigated through information and sensitisation within the family and constant follow-up of patients and families (e.g. through TB screening). However, CTSs are exposed to infection risks and at times experience feelings of insecurity while doing their job, but qualified training complemented by support from health professionals helped them to overcome these fears. However, the major characteristic that helped them in their role was their self-sacrificing attitude in fulfilling their activities. In addition, community-based care requires sufficient organisation and planning in order not to result in frustration of CTSs. For instance, the low level of stipend demotivated treatment supporters in another setting where they also felt the emotional strain of caring for sick people (Escott & Walley, Citation2005). In our setting, CTSs were compensated for their work (Kerschberger et al., Citation2019) and no complaints were reported. However, it was beyond the scope of this study to assess their satisfaction with the level of compensation.
Lastly, it is supposed that community-based DR-TB treatment possibly also increases awareness and knowledge about DR-TB within the communities. This model of care simultaneously suggests a reduction in stigma because not only were patients cured but community members witnessed it.
Future perspectives
As TB infections and most of the treatment occur at the community level, the mobilisation of community assets in RLS is likely key to ending the TB epidemic by 2030. Underfunded TB programmes struggle to deliver injectable-based DR-TB treatment regimens in RLS lacking qualified human resources for health. Although this study did not investigate the role of CTSs in the delivery of the newly recommended fully oral DR-TB regimen, the authors believe that community support will continue to play an important role in the expansion of culturally acceptable and affordable quality DR-TB care.
Limitations
The main limitation was that the selected sample of patients included in the study might not be representative of all DR-TB patients from this and other settings. In addition, DR-TB care provided by MSF or other non-governmental organisations may not be fully generalisable to settings with care predominantly provided through government structures.
Conclusion
Community-based DR-TB care appeared to be an appropriate care model and supportive for patients, CTSs and most family members. This study showed that it is fostering DR-TB patients’ quality of life in receiving professional, dedicated and individual care from their CTSs. On the other side, CTSs experienced empowerment and self-esteem and fulfilled their care responsibility with empathy. It is essential not to overlook concerns related to social and economic problems within the families and to seriously take into consideration family members’ fears and worries about potential infection risks. To mitigate these anxieties, information and sensitisation within the family and constant follow-up of patients are crucial. Further research is needed to understand the perception of participants in the use of CTS for expansion of fully oral DR-TB treatment regimens.
Acknowledgements
We would like to thank all the research participants in Eswatini who participated in this research, trusted us, and shared with us their personal experiences with community-based DR-TB care, which led to the arguments made in this paper. Thanks also go to the National Tuberculosis Control Program, as well as the anonymous reviewers at Global Public Health for their helpful feedback and critiques on earlier drafts of this article. We finally thank all MSF teams at field and headquarters level, for their valuable support of this research.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Arshad, A., Salam, R. A., Lassi, Z. S., Das, J. K., Naqvi, I., & Bhutta, Z. A. (2014). Community based interventions for the prevention and control of tuberculosis. Infectious Diseases of Poverty, 3(1), 27–27. https://doi.org/10.1186/2049-9957-3-27
- Bicego, G. T., Nkambule, R., Peterson, I., Reed, J., Donnell, D., Ginindza, H., Duong, Y. T., Patel, H., Bock, N., Philip, N., Mao, C., Justman, J., & Schildgen, O. (2013). Recent patterns in population-based HIV prevalence in Swaziland. PLoS One, 8(10), Article e77101. https://doi.org/10.1371/journal.pone.0077101
- Blackman, A., & Fairey, T. (2007). The PhotoVoice manual - A guide to designing and running participatory photography projects.
- Brust, J. C. M., Shah, N. S., Scott, M., Chaiyachati, K., Lygizos, M., van der Merwe, T. L., Bamber, S., Radebe, Z., Loveday, M., Moll, A. P., Margot, B., Lalloo, U. G., Friedland, G. H., & Gandhi, N. R. (2012). Integrated, home-based treatment for MDR-TB and HIV in rural South Africa: An alternate model of care. The International Journal of Tuberculosis and Lung Disease, 16(8), 998–1004. https://doi.org/10.5588/ijtld.11.0713
- Cannuscio, C., Weiss, E., Fruchtman, H., Schroeder, J., Weiner, J., & Asch, D. (2009). Visual epidemiology: Photographs as tools for probing street-level etiologies. Social Science & Medicine, 69(4), 553–564. https://doi.org/10.1016/j.socscimed.2009.06.013
- Central Statistical Office of Eswatini. (2017). The 2017 population and housing census preliminary results. Mbabane, Eswatini: Central Statistical Office of Eswatini.
- Colvin, C., Mugyabuso, J., Munuo, G., Lyimo, J., Oren, E., Mkomwa, Z., Makame, M., Mwangomale, A., Mahamba, V., Mueller, L., & Richardson, D. (2014). Evaluation of community-based interventions to improve TB case detection in a rural district of Tanzania. Global Health: Science and Practice, 2(2), 219–225. https://doi.org/10.9745/ghsp-d-14-00026
- Daftary, A., Padayatchi, N., & O’Donnell, M. (2014). Preferential adherence to antiretroviral therapy over tuberculosis treatment: A qualitative study of drug-resistant TB/HIV co-infected patients in South Africa. Global Public Health, 9(9), 1107–1116. https://doi.org/10.1080/17441692.2014.934266
- Daniel, C., & Logie, C. (2016). Contexts of risk: A photo-voice study of Haitian youth perceptions of their HIV risk. Global Social Welfare, 3(4), 255–267. https://doi.org/10.1007/s40609-016-0065-1
- Demissie, M., Getahun, H., & Lindtjorn, B. (2003). Community tuberculosis care through “TB clubs” in rural North Ethiopia. Social Science & Medicine, 56(10), 2009–2018. https://doi.org/10.1016/s0277-9536(02)00182-x
- Duwell, M. M., Knowlton, A. R., Nachega, J. B., Efron, A., Goliath, R., Morroni, C., Maartens, G., & Chaisson, R. E. (2013). Patient-nominated, community-based HIV treatment supporters: Patient perspectives, feasibility, challenges, and factors for success in HIV-infected South African adults. AIDS Patient Care and STDs, 27(2), 96–102. https://doi.org/10.1089/apc.2012.0348
- Escott, S., & Walley, J. (2005). Listening to those on the frontline: Lessons for community-based tuberculosis programmes from a qualitative study in Swaziland. Social Science & Medicine, 61(8), 1701–1710. https://doi.org/10.1016/j.socscimed.2005.03.040
- Farmer, P., & Kim, J. Y. (1998). Community based approaches to the control of multidrug resistant tuberculosis: Introducing “DOTS-plus”. BMJ, 317(7159), 671–674. https://doi.org/10.1136/bmj.317.7159.671
- Green, J., & Thorogood, N. (2018). Qualitative methods for health research. Sage.
- Guo, N., Marra, F., & Marra, C. A. (2009). Measuring health-related quality of life in tuberculosis: A systematic review. Health and Quality of Life Outcomes, 7(1), 14. https://doi.org/10.1186/1477-7525-7-14
- Hadley, M., & Maher, D. (2000). Community involvement in tuberculosis control: Lessons from other health care programmes. The international Journal of Tuberculosis and Lung Disease, 4(5), 401–408.
- Heller, T., Lessells, R. J., Wallrauch, C. G., Bärnighausen, T., Cooke, G. S., Mhlongo, L., Master, I., & Newell, M. L. (2010). Community-based treatment for multidrug-resistant tuberculosis in rural KwaZulu-Natal, South Africa. The international Journal of Tuberculosis and Lung Disease, 14(4), 420–426.
- Hendrix-Jenkins, A. (2008). The expansion of community-based tuberculosis programming: Critical program design issues for new partners.
- Horter, S., Stringer, B., Reynolds, L., Shoaib, M., Kasozi, S., Casas, E. C., Verputten, M., & du Cros, P. (2014). “Home is where the patient is”: A qualitative analysis of a patient-centred model of care for multi-drug resistant tuberculosis. BMC Health Services Research, 14(1), 81. https://doi.org/10.1186/1472-6963-14-81
- Isaakidis, P., Rangan, S., Pradhan, A., Ladomirska, J., Reid, T., & Kielmann, K. (2013). ‘I cry every day’: Experiences of patients co-infected with HIV and multidrug-resistant tuberculosis. Tropical Medicine & International Health, 18(9), 1128–1133. https://doi.org/10.1111/tmi.12146
- Kerschberger, B., Telnov, A., Yano, N., Cox, H., Zabsonre, I., Kabore, S. M., Vambe, D., Ngwenya, S., Rusch, B., Tombo, M. L., & Ciglenecki, I. (2019). Successful expansion of community-based drug-resistant TB care in rural Eswatini - a retrospective cohort study. Tropical Medicine & International Health, 24(10), 1243–1258. https://doi.org/10.1111/tmi.13299
- Laxmeshwar, C., Stewart, A. G., Dalal, A., Kumar, A. M. V., Kalaiselvi, S., Das, M., Gawde, N., Thi, S. S., & Isaakidis, P. (2019). Beyond ‘cure’ and ‘treatment success': Quality of life of patients with multidrug-resistant tuberculosis. The International Journal of Tuberculosis and Lung Disease, 23(1), 73–81. https://doi.org/10.5588/ijtld.18.0149
- Mitchell, C., De Lange, N., Moletsane, R., Stuart, J., & Buthelezi, T. (2005). Giving a face to HIV and AIDS: On the uses of photo-voice by teachers and community health care workers working with youth in rural South Africa. Qualitative Research in Psychology, 2(3), 257–270. https://doi.org/10.1191/1478088705qp042oa
- Mohammed, S., Sajun, S. Z., & Khan, F. S. (2013). Harnessing photovoice for tuberculosis advocacy in Karachi, Pakistan. Health Promotion International, 30(2), 262–269. https://doi.org/10.1093/heapro/dat036
- O’Donovan, J., Hamala, R., Namanda, A. S., Musoke, D., Ssemugabo, C., & Winters, N. (2020). ‘We are the people whose opinions don’t matter’. A photovoice study exploring challenges faced by community health workers in Uganda. Global Public Health, 15(3), 384–401. https://doi.org/10.1080/17441692.2019.1663233
- O'Reilly, M., & Parker, N. (2012). . ‘Unsatisfactory saturation’: A critical exploration of the notion of saturated sample sizes in qualitative research. Qalitative Research, 1–8. https://doi.org/10.1177/1468794112446106
- Patton, Q. M. (2002). Qualitative research & evaluation methods (3rd ed.). Sage Publications Thousand Oaks.
- Sanchez-Padilla, E., Dlamini, T., Ascorra, A., Rüsch-Gerdes, S., Tefera, Z. D., Calain, P., de la Tour, R., Jochims, F., Richter, E., & Bonnet, M. (2012). High prevalence of multidrug-resistant tuberculosis, Swaziland, 2009-2010. Emerging Infectious Diseases, 18(1), 29–37. https://doi.org/10.3201/eid1801.110850
- Satti, H., McLaughlin, M. M., Hedt-Gauthier, B., Atwood, S. S., Omotayo, D. B., Ntlamelle, L., & Seung, K. J. (2012). Outcomes of multidrug-resistant tuberculosis treatment with early initiation of antiretroviral therapy for HIV Co-infected patients in Lesotho. PLoS One, 7(10), Article e46943. https://doi.org/10.1371/journal.pone.0046943
- Seung, K. J., Omatayo, D. B., Keshavjee, S., Furin, J. J., Farmer, P. E., Satti, H., & Pai, M. (2009). Early outcomes of MDR-TB treatment in a High HIV-prevalence setting in Southern Africa. PLoS One, 4(9), Article e7186. https://doi.org/10.1371/journal.pone.0007186
- Shin, S., Furin, J., Bayona, J., Mate, K., Kim, J. Y., & Farmer, P. (2004). Community-based treatment of multidrug-resistant tuberculosis in Lima, Peru: 7 years of experience. Social Science & Medicine, 59(7), 1529–1539. https://doi.org/10.1016/j.socscimed.2004.01.027
- Shringarpure, K. S., Isaakidis, P., Sagili, K. D., Baxi, R. K., Das, M., Daftary, A., & Escobar-Gutiérrez, A. (2016). “When treatment is more challenging than the disease”: A qualitative study of MDR-TB patient retention. PLoS One, 11(3), Article e0150849. https://doi.org/10.1371/journal.pone.0150849
- Singla, N., Singla, R., Fernandes, S., & Behera, D. (2009). Post treatment sequelae of multi-drug resistant tuberculosis patients. The Indian Journal of Tuberculosis, 56(4), 206–212.
- Skovdal, M. A., & Flora, C. (2015). Qualitative research for development: A guide for practitioners. Practical Action Publishing Ltd.
- Snyman, L., Venables, E., Trivino Duran, L., Mohr, E., Azevedo, V. D., Harmans, X., & Isaakidis, P. (2018). ‘I didn’t know so many people cared about me’: Support for patients who interrupt drug-resistant TB treatment. The International Journal of Tuberculosis and Lung Disease, 22(9), 1023–1030. https://doi.org/10.5588/ijtld.17.0826
- Teti, M., French, B., Bonney, L., & Lightfoot, M. (2015). “I created something new with something that had died”: photo-Narratives of positive transformation among women with HIV. AIDS and Behavior, 19(7), 1275–1287. https://doi.org/10.1007/s10461-015-1000-7
- Udwadia, Z., & Furin, J. (2019). Quality of drug-resistant tuberculosis care: Gaps and solutions. Journal of Clinical Tuberculosis and Other Mycobacterial Diseases, 16, Article 100101. https://doi.org/10.1016/j.jctube.2019.100101
- USAID. (2017). TB CARE II community-based care for drug-resistant tuberculosis: a guide for implementers.
- Wang, C., & Burris, M. A. (1997). Photovoice: Concept, methodology, and use for participatory needs assessment. Health Education & Behavior, 24(3), 369–387. https://doi.org/10.1177/109019819702400309
- WHO. (2008). Community involvement in tuberculosis care and prevention: Towards partnerships for health: Guiding principles and recommendations based on a WHO review. World Health Organization.
- WHO. (2014). Companion handbook to the WHO guidelines for the programmatic management of drug-resistant tuberculosis.
- WHO. (2017). End TB by 2030. Framework for implementing the “End TB Strategy” in the African region 216–2020. Geneva, Switzerland: World Health Organization.
- WHO. (2018). World Health Organization. Global tuberculosis report 2018.