ABSTRACT
Universal antiretroviral therapy (ART) strategies have dramatically changed HIV programming across sub-Saharan Africa. We explored factors that influenced the development, adoption and implementation of universal ART policies in Tanzania, South Africa and Malawi. We conducted 26 key informant interviews and applied Kingdon’s ‘streams’ model to explore how problems, policies and politics converged to provide a window of opportunity for universal ART roll-out. Weak health systems and sub-optimal care retention were raised as problems during Option B+ implementation, which preceded universal ART , and persisted after its implementation. The adoption and implementation of Option B+ policy facilitated the uptake of universal ART. Politics played out through pressures from different stakeholders to accelerate or slow down implementation, from governments, civil society groups, researchers and donors. Policy processes leading to universal ART were open to pressures and influence. The extraordinary financial support which enabled the widespread and rapid implementation of universal ART skewed the power balance and sometimes left little space for locally-derived solutions to respond to specific health system abilities and epidemiological contexts. Donors may be more effective if they ensure a greater focus on strengthening the whole health system as well as accounting for local contextual factors and recent policy development histories when funding policy implementation.
Introduction
Despite two decades of global and national initiatives and efforts to bring the HIV epidemic under control, there were still 37.9 million people living with HIV by the end of 2018, with 54% of those living in Eastern and Southern Africa (UNAIDS, Citation2019). The drive to end AIDS by 2030 through targets to reach 95% of people living with HIV (PLHIV) knowing their status, 95% of diagnosed PLHIV accessing treatment and 95% of PLHIV on treatment being virally suppressed has led to dramatic changes in HIV programming across sub-Saharan Africa. Universal antiretroviral therapy (ART), or providing ART to all persons diagnosed with HIV, regardless of their CD4 count, was first recommended by the World Health Organization (WHO) in 2015, following evidence from epidemiological and modelling studies that showed that high levels of HIV testing followed by rapid initiation of antiretroviral therapy (ART) for all PLHIV brought individual health benefits and reduced HIV transmission risks (World Health Organization, Citation2016). Unprecedented global efforts have meant that despite the growing budgets needed to scale-up antiretroviral therapy, and concerns that donor fatigue may lead to lower international contributions (Grépin, Citation2012), some funders are providing record contributions to national HIV programmes (The Global Fund, Citation2020). Governments in some countries, including South Africa, are spending a growing proportion of their Gross Domestic Product on health, including the response to HIV (Dieleman et al., Citation2018; National Treasury, Citation2020; Remme et al., Citation2016).
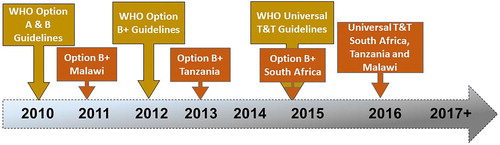
In 2011, Malawi modified the prevention of mother-to-child transmission (PMTCT) recommendation from the WHO by implementing a national strategy that aligned with the constraints of its health system (Kalua et al., Citation2017). The implementation of this programme in Malawi, which was named Option B+, stimulated a global debate about the public health benefits of lifelong ART among all pregnant and lactating women and culminated in the WHO pragmatic update recommending Option B or B+ in 2012 (see ) (World Health Organisation [WHO], Citation2012) . Shortly after this, WHO formalised the Option B+ recommendation in its 2013 consolidated ARV guidelines (World Health Organisation [WHO], Citation2013) ()..
Table 1. ARV treatment guidelines for prevention of mother-to-child transmission of HIV, Cited from Gourlay A et al. (Gourlay et al., Citation2013).
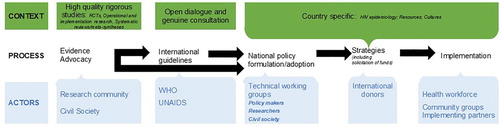
The development of national health policies and implementation strategies is a process that involves multiple actors to identify needs and resources, and to define operational plans. Ideally, policies are aligned with international guidance which is based on the available evidence, and evolves from local understandings of which strategies are best suited for the particular epidemiological context, as well as taking into account the availability of resources and the political economy (see ). Several theorists have proposed models to explore the policy adoption and implementation process (Howlett, Citation2018; Howlett et al., Citation2014), including Kingdon, who identified three ‘streams’ (‘problems’, ‘policies’ and ‘politics’) that converge to provide a ‘window of opportunity’ for a policy change (Brodkin & Kingdon, Citation1985; Howlett et al., Citation2014). This approach allows dynamic and non-linear processes to be unpacked, explaining uptake and implementation of policy in specific settings.
Figure 2. Schematic illustration of the policy process accounting for the context, the process and the actors.
This analysis draws on data collected by the ‘SHAPE UTT’ (Strengthening Health systems for the Application of Policy to Enable Universal Test and Treat) study, which aimed to assess the policy implementation and health systems impacts of universal ART in Malawi, the United Republic of Tanzania (hereafter referred to as Tanzania) and South Africa (Renju et al., Citation2020). Drawing on Kingdon’s theory, we explore how the different ‘streams’ converged to influence the evolution of universal ART treatment policies in these three countries, contributing to differences in scale-up approaches and ART coverage.
Methods
Study design and setting
This was a cross-sectional study using key informant (KI) interviews to capture policy formulation, adaptation and implementation of HIV policies since 2011, specifically Option B+ and universal ART. The study took place between 3rd April and 7th July 2019 in the three study countries. The three countries represent early (Malawi), mid-term (Tanzania) and late (South Africa) adopters of Option B+ policies (in 2011, 2013 and 2015 respectively), thereby enabling comparisons of the policy implementation processes and subsequent impacts on each health system. Each of these countries adopted and rolled out universal ART as national policy from 2016, although through different policy pathways. Each country had different HIV demographics in 2015, just prior to the implementation of universal ART (in 2015) and different ART policy and implementation milestones ().
Table 2. HIV demographics and ART policy and implementation milestones by country.
By the end of 2019, the three countries had achieved varying degrees of ART coverage. In Tanzania, 78% of PLHIV knew their status, of those who knew their status, 92% were on ART, and of those on ART, 87% were virally suppressed (Avert, Citation2018c). In Malawi, the corresponding figures were 90%, 87% and 89% (Avert, Citation2018a), while in South Africa, it was 90%, 68% and 78% (Avert, Citation2018b).
Study participants
KI interviews were conducted to explore the decision-making contexts including the financial and governance factors that underlay the development, adoption and implementation of HIV policies such as Option B+ and universal treatment. Respondents included policymakers, programmers, technical advisors and academics. In Tanzania and Malawi, participants were sampled at the national level, while in South Africa, where decision-making happens at a provincial level, we only sampled from the province of KwaZulu-Natal (the province in which the SHAPE study took place). In total, 25 key informant interviews were conducted as disaggregated in .
Table 3. Characteristics of the study participants.
Data collection and management
A sampling frame of potential KIs was prepared by the study coordinators in each country using networks maintained by the co-investigators and additional snowball sampling techniques. Potential KIs were initially contacted by phone, by email or during in-person meetings to describe the aims and methods of the study and invite them to participate. Up to four attempts were made to contact each potential participant. After this point the participant was not contacted again. For those that agreed, a time and private location of the participant’s choice were agreed. Identified KIs were also able to refuse to participate at any point during the recruitment and interview process.
The interviews were semi-structured and drew on topic guides. The KI interviews explored reasons for Option B+ and universal treatment policy implementation gaps in each setting and aimed to understand the participant’s views on how different actors, the policy content, context and processes influenced the implementation of these policies in each setting. This included the participant’s views on the influence of political will underlying the timing of HIV treatment policy adoption and delivery, as well as the role of scientific evidence, the historical context, funding sources and financing mechanisms in influencing HIV policy decisions in each country.
All interviews were audio-recorded and conducted in English or a mix of English and Swahili (in Tanzania). Translations into English were conducted where necessary, and all interviews were then transcribed verbatim. Interview transcripts were made available to study participants when requested. Interviews were conducted by experienced, senior researchers from the three countries (MK in Malawi, HS in Tanzania and RC and MM in South Africa) who were familiar with the HIV policy landscape in their respective countries.
Debriefings between the members of the research team took place regularly to share experiences across sites, ensure broad consistency in terms of the topic areas covered, identify and discuss emerging themes and relationships between them, discuss amendments to the topic guides as new areas of interest emerged, and compare findings across countries.
Data analysis
After the initial review of each field summary and transcripts, data were iteratively imported into NVIVO11 for coding by the lead author (MK). A broad coding framework was developed guided by the topics covered in the interview guide with transcripts coded to the different stages of policy adoption, adaption and implementation. We combined this deductive coding with an inductive approach taken to develop more refined sub-codes driven by the content of the data. We then drew on Kingdon’s ‘Streams’ Model as an analytical framework to interpret the patterns within the coded data in relation to our research question. Data were initially analysed by country, with cross-country comparisons of key areas of interest, and the main themes that arose within the ‘streams’.
Ethical statement
Ethical approval for the data collection was obtained from the University of KwaZulu-Natal Biomedical Research Committee in South Africa (BE400/14), from the National Institute of Medical Research in Tanzania (NIMR/HQ/R.8a/Vol. IX /2579) and from the National Health Sciences Research Committee in Malawi (17/07/1861). The study was also approved by the ethics committee at the London School of Hygiene and Tropical Medicine (13536).
Results
The application of the Kingdon’s streams identified various ‘problems’, ‘policies’ and ‘politics’ that arose from the discussions with the key informants (see ).
Problems
KIs described challenges in the health systems and sub-optimal care retention as problems that had arisen during the implementation of Option B+ and were still persistent in the build up to universal ART. Specifically, they mentioned how the health systems had limited laboratory capacity for CD4 testing (in Malawi) and viral load testing in all three countries. The implementation of universal ART negated the need for CD4 testing to determine ART eligibility and therefore was seen as a solution to this problem by many of the participants.
However, for viral load testing, the limited availability of testing machines or their malfunctioning led to long turnaround times. These long turnaround times limited the timely guidance for clinical care and prevented the accurate monitoring of treatment failure and drug resistance.
It [viral load monitoring] is not happening most of the time … you don’t get the results back when you need them, you are told that the machine is not working well. Sometimes the machine is working but the skills are not there, we have qualified staff but we do not have the skills for using these machines, so that’s the challenge. (Female, Policy maker, Tanzania, Participant 05)
Health systems also struggled with having inadequate infrastructure, in terms of space, to accommodate large client numbers. KIs felt that such challenges compromised the privacy afforded to clients and had subsequent implications on the health workers’ ability to provide quality care.
… infrastructure was also a challenge, because I think initially most of the facilities were built before the HIV era which led to the implementation of many interventions. A lot of these programs required space and this was also one of the challenges. (Female, Government implementing partner, Malawi, Participant 09)
You have done your ordering … so when changes come, you know you cannot say: ‘okay stop using these and send them back to where they came from!’ Some will be pushed to the facility just to make sure that they get to people and get used … That has been one of the common challenges. And you know now we are moving to another regimen, to DTG, starting this month. The question of expiry is there on the table … . (Male, Policy maker, Tanzania, Participant 10)
The information system is the only way you can track a client. If I want to have the entire care history of this client, I must be able to have a system that I can access. If I can just put in a client’s ID number … then all the information just pops up there in front of me. So, if we do not have that, it’s going to be very difficult for us to manage the movement of clients and to be able to really say we have clients defaulting treatment or not. (Female, Government official implementer, South Africa, Participant 01)
… if you have universal ART coverage, transmission has to go down, but this is not reflected in our estimates. It is more to do with a data quality but I don’t think we have got to the bottom of it. … we have not invested enough at the grass root where data is collected. Mistake are made by those who record the data which cannot be reworked by people who sit at the Ministry level or at the program level. They have a lot of books to fill in and now they also need time to enter the data into the computer programs … a lot can go wrong … we spend a lot of time training our health care workers to deliver services but we don’t make similar investments in recording and reporting, if we do not do this we will keep seeing this problem. (Male, Development partner, Tanzania, Participant 10)
Policies
The prior adoption and implementation of Option B+ was unanimously recognised by all KIs as having facilitated the roll-out of Universal treatment. KIs felt that some of the processes that preceded the uptake of Option B+ facilitated the progression to universal treatment for the general population in various different ways. The implementation of Option B+ prompted all of the study countries to broaden stakeholder representation in their technical working groups (TWGs) and consultations, including government bureaucrats, civil society representatives, donors, academics and researchers. Representation from different groups within the TWGs created an atmosphere of openness and frank dialogue where participants could express opinions.
It [Option B + ] got academic institutions involved like university institutions … in order to even start drafting a policy, to say this is what we are going to implement … (Female, Government official implementer, South Africa, Participant 01)
So it is a lot of consultation … members of TWG the academia, the civil society, the actual practitioners, the service providers … once the policy has been developed, it also has to be approved by senior management of Ministry health … to scrutinize the policy and see its applicability. (Female, Government official policy maker, Malawi, Participant 09)
The previous delays … have kind of been removed because you don’t have to wait for a week for a sample to come back before you make a decision and all that and it has made it a bit easier (Female, Government official implementer, Tanzania, Participant 03)
And for me, it really re-emphasised the need for a simplified protocol, even if it means cutting of few corners clinically. Certainly it will have a much bigger public health impact than a sophisticated policy that looks good on paper, but cannot really be implemented within our setting. … our clinics are run by the auxiliary staff and so designing a policy that presumes that there is a professional medical person implementing [would be a challenge] for the majority of our sites. (Male, Technical Advisor, Malawi, Participant 01)
… the natural progression was already there and it just need a little bit of a push to go to test and treat … so it [universal treatment] is simpler, it’s much simpler because everybody is eligible. It is easy to implement. People were already expecting it, it was just a matter of getting the money and getting ready for the idea (Male, Academic, Malawi, Participant 10)
Politics
Politics played a critical role in either promoting or inhibiting action during the formulation of Option B+ and universal ART policies in Malawi, Tanzania and KwaZulu-Natal, South Africa. In each of these three settings, various hurdles needed to be overcome in order to both adopt and then implement Option B+ and universal ART. The KIs highlighted that the three countries followed somewhat different pathways to culminate in the adoption of Option B+, which affected the timing of adoption and the pathway to universal ART adoption.
In Malawi, the HIV unit within the Ministry of Health faced initial resistance to Option B+ formulation and implementation. Many KIs highlighted the challenges of convincing national policy makers and politicians, international donors and community members why they believed that it was important to start implementing Option B+.
… [it was] quite difficult because it was against WHO guidelines and then you have to defend it … he [head of HIV unit at the time] must have used all of his convincing powers in the ministry. (Male, Academic, Malawi, Participant 10)
There was also quite a lot of pushback from various people in the media, amongst academic and activists, there were quite a lot of people who said this is not good for women and ethically it's not right. People felt it would lead to coercion and there were quite a lot of counterarguments so initially it was a little bit tricky (Male, Academic, Malawi, Participant 10)
It was ethical question about ..men [and their rights to] immediate [access to] ARVs. Why healthy women [receive] ARV but men are not … . (Male, Development partner, Malawi, Participant 02)
… by the time we had finished launching the elimination of mother to child transmission (eMTCT) strategic plan, we received the WHO recommendation regarding the use of ART for PMTCT and also for mother’s health. (Government official implementer, Tanzania, Participant 11)
… That time we had the issue that they could see that if we are going to put too many people on treatment, we have to treat them for the rest of their life. So the costs of the programs would increase, and they were speaking about mortgage, so like similar if you take out mortgage you have to pay for the next 30 years to pay for the mortgage and they saw this is a mortgage. (Male, Technical advisor, Malawi, Participant 03)
… we are exerting pressure, as donors we are pressurizing, as development partners were pressuring yes … Listen sometimes when you are pressurized to do a good thing, you are not supposed to complain, if the intervention is good and it works and it will help the mother and the kids. (Male, Development partner, Tanzania, Participant 04)
Typically, when our partners, external donors and funders come they are shown … places which have dedicated ART clinics with dedicated staff that do nothing but ART services. But the reality for most of our clients is different, because they are seen by health workers who rotate out of ART clinics, and a lot of the time there isn’t even a trained nurse (Male, Technical Advisor, Malawi, Participant 01)
We actually had more pushback from the Global Fund [for universal treatment as opposed to Option B + ]; when we were in the process of submitting a new funding application, our portfolio manager was very strongly opposed to the idea [of universal treatment based] primarily on sustainability grounds. So they essentially said that your funding envelope doesn’t stretch far enough for us to do that. … It was much tougher at that point to push the Global Fund to accept our funding application for universal treatment because they had the impression that we were overreaching our resources. … I remember we had some negotiations after the technical review panel had essentially initially rejected it on the same basis, [especially given that there was] no WHO policy, and no money to do this [stating that] we couldn’t sustain [the programme] and that Malawi shouldn’t be doing it. (Male, Technical Advisor, Malawi, Participant 01)
… you know universal treatment was a mandate. Universal treatment was announced on World AIDS day [2016]. [We were then told] that we were going this way. There was pressure that it must be implemented and there was a hype with universal treatment for many reasons. (Female, Policy maker, South Africa, Participant 02)
… Tanzania depends on donor funding … PEPFAR has its own … areas. So this in a way will affect others or other areas where actually PEPFAR cannot give resources to continue with other regions. (Male, Development partner, Tanzania, Participant 07)
… they [PEPFAR] did an analysis in Washington, they looked at every health facility especially those high volume sites. [They looked at] on average how many HIV positive clients do they have? How many are new? How many are on treatment? They see the number is still low, while we know who there are and who are still in need of the service, [following this] … we were told to go and see why those numbers are not improving. So that’s a lot of pressure. (Male, Development partner, Tanzania, Participant 04)
Now we often see that for examples donors becoming normative … [and] … not following the normal policy procedures. This wasn’t always the case, this is something happening now (Male, Technical advisor, Malawi, Participant 03)
I think in the current environment this [country-led development of Option B + ] would have been much more difficult … there is no space to shape any kind of national policy anymore because it almost entirely dictated from outside. (Male, Technical advisor, Malawi, Participant 01)
And now you are told that you are positive. Then you start treatment, yet you still haven’t processed everything. Yet it did not mean that the exact day. You could still be initiated during that week, but you need time to come to terms and understand what is this, if we push aggressively you will stop taking and become lost to follow up. (Female, Policy maker, South Africa, Participant 02)
… when we say ‘test and treat’, there are some health care workers that interpret it like you are positive today you start your treatment today. We have seen that by doing that, there is huge loss to follow up … . So now it was revised that we can allow the individual to start within two weeks and still for us it’s test and treat. So, that communication from our understanding at national level we have the same understanding at lower level. But also I think PEPFAR are complicating it; their indicators report that X number started on the same day. They are talking about the same day initiative. (Female, Development partner, Tanzania, Participant 02)
… our national policy said that the clients should be given up to two weeks to decide when they’re ready to start ART … but the implementing partners were told by PEPFAR that they have to implement same-day initiation and so their numbers had to be reported in that way and so they were pushing everybody to essentially start the same day. You know that the consequences are obvious in our data: in many of those districts there is a clear surge in dropouts. (Male, Technical advisor, Malawi, Participant 01)
Discussion
We interviewed a range of key informants about the evolution of universal ART policies and implementation in Malawi, Tanzania and South Africa. By comparing and contrasting their experiences with the implementation of universal ART we have unravelled how ongoing problems, past policy experiences, and donor relations converge to determine how universal ART, as a global health policy, dynamically evolves in different settings, in complex, messy and highly politicised ways.
The KIs in this study constituted health systems and retention in care as particular kinds of ‘problems’ in relation to universal ART. Whilst some problems persisted, such as sub-optimal quality of care, lack of essential services such as viral load testing, and problems with supply chain systems, others surfaced along the trajectory of universal ART implementation. Whilst KIs saw universal ART as a natural and timely progression from Option B+, these ongoing problems ignited important questions and concerns about how existing health system ‘problems’ would affect or undermine its cale-up Although the 2015 WHO recommendation for universal treatment resulted in adaptation of existing Option B+ policies in multiple countries, it was also clear from our findings that past experiences of Option B+ resulted in different universal ART adaptation journeys. Malawi, for instance, who paved the way for universal ART by pioneering Option B+, had been ready to implement universal treatment since 2014, but was held back because of opposition from funding institutions or due to their decision-making procedures which required alignment to WHO recommendations. Stakeholders in Tanzania and South Africa, on the other hand, spoke about how some donors, or international implementing partners pushed the ‘how’, ‘where’ and ‘when’ to adopt universal ART with little consideration of local constraints. For example, in Tanzania, we heard of the challenges faced by the rapid change in PMTCT guidelines, with Option B+ coming to the forefront just after the Tanzanian government had completed the roll-out of their new eMTCT strategy (Ministry of Health and Social Welfare National AIDS Control Programme (NACP), Citation2012). Nonetheless, it was evident from our findings that past experiences of Option B+ and the recommendation from the WHO for universal ART, allowed all three countries to more easily transition towards large-scale implementation of universal treatment. These scenarios highlight how one policy (Option B+) came to have a ripple-effect paving the way for universal ART for the general population. Similar observations have been made in Zimbabwe, where past experiences of adapting and implementing Option B+ policy recommendations was noted to provide policymakers with the know-how and operational tools to adopt and implement universal treatment more smoothly and in a timely fashion (Moran et al., Citation2020). Our study supports the argument made by Moran et al. (Citation2020) that policy adoption and implementation ought to be considered in temporal contexts, with universal ART being both timely, a development from past policies, and affected by the readiness of health systems. However, adding to this work, our multi-country study has also shown how universal treatment policy adoption and implementation is intrinsically linked to the influence of the WHO guidance, the international donor agencies, as well as other actors including CSOs.
Our findings also highlight how some donors, specifically those who provide substantial budgetary support for specific health programmes, risked interfering with the autonomy of the countries to develop or interpret their own universal treatment policies in the context of their own health systems. Because the countries had different donors and donor relations, the pressures differed and policies were interpreted differently, as exemplified by diverging definitions of ‘same-day initiation’. Our analysis demonstrated that a greater degree of local autonomy in the development of policies responding to context specific health systems challenges was an important ingredient that drove creativity and innovation in Malawi leading to the development of Option B+ policy, which later became universal treatment. However, the pressure that these three African countries have been receiving from donors after the introduction of Option B+ policy exemplifies how a globalisation and standardisation of HIV responses can disempower national policymaking structures to craft policies that respond to the local situation (Campbell et al., Citation2012; Moshabela et al., Citation2020). We extend calls made by Aveling (Aveling, Citation2010) and Skovdal et al (Skovdal et al., Citation2017), based on research in Cambodia and Zimbabwe respectively, for greater attention to how power asymmetries, conditioned by the aid architecture, undermine equitable partnerships in the HIV response.
Our findings are constrained by some methodological limitations which deserve mentioning. First, the study relies primarily on self-reported data collected at one time point. Future research in this area of study may consider adopting a more in-depth and longitudinal ethnographic approach. Second, and relatedly, our participants could have wanted to protect their own, or their organisation’s reputation, meaning the study was susceptible to social desirability bias, with participants representing themselves in particularly positive way. In line with this, our third limitation relates to the selection of our study participants. Our snowballing sampling strategy led to the inclusion of a mix of professionals all with different mandates, which differed in each country, potentially leading to a selection bias. In our study we found that the ‘technical advisors’ were the most outspoken, perhaps related to their positionality between the country and its policy adoption and implementation processes and our research team (Merriam et al., Citation2001). In this study, we only had two technical advisors both emanating from one country. It is therefore possible that the opinions of these KIs are over-represented due to their relative ease with which they were able to navigate these discussions. Fourthly, and again relatedly, the generalizability of our findings is limited by the small number of key informants, specifically in South Africa, where only five participants were recruited all of whom spoke of their experiences and attitudes towards HIV policies development and implementation in one Province (KwaZulu Natal). Future research could usefully broaden its scope and include the perspectives and experiences of other actors, with specific inclusion of other non-government players, which would involve both donors, technical partners such as WHO, and more implementing partners.
Nonetheless, by drawing on Kingdon’s framework (Brodkin & Kingdon, Citation1985), we have painted a complex picture of the factors shaping the evolution of universal treatment policy adoption and implementation. We showed that international global health policies are not merely discreet products that are delivered in one direction, from one location (e.g. WHO in Geneva) to another (e.g. health systems in sub-Saharan Africa) (Jenkins, Citation2007), but are contextually bound by ongoing problems, past policy experiences and donor relations. Our study challenges the ‘policy transfer’ logic and smooth policy spaces (Dolowitz & Marsh, Citation2000) that characterises much global health policy analysis, and highlight the need for further multi-country studies to unravel the place-specific problems, past experiences and donor-relations that affect the adoption of global health policies.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data will be available for the next five years upon request to the study PI: [email protected].
Additional information
Funding
References
- Aveling, E. L. (2010). The impact of aid chains: Relations of dependence or supportive partnerships for community-led responses to HIV/AIDS?. AIDS Care, 22(sup2), 1588–1597. https://doi.org/10.1080/09540121.2010.507954
- Avert. (2018a). HIV and AIDS in Malawi. Retrieved August 3, 2020, from https://www.avert.org/professionals/hiv-around-world/sub-saharan-africa/malawi
- Avert. (2018b). HIV and AIDS in South Africa. Retrieved August 3, 2020, from https://www.avert.org/professionals/hiv-around-world/sub-saharan-africa/south-africa
- Avert. (2018c). HIV and AIDS in Tanzania. Retrieved August 3, 2020, from https://www.avert.org/professionals/hiv-around-world/sub-saharan-africa/tanzania
- Brodkin, E., & Kingdon, J. (1985). Agendas, alternatives, and public policy. Political Science Quarterly, 100(1), 165. https://doi.org/10.2307/2150882
- Campbell, C., Cornish, F., & Skovdal, M. (2012). Local pain, global prescriptions? Using scale to analyse the globalisation of the HIV/AIDS response. Health & Place, 18, https://doi.org/10.1016/j.healthplace.2011.10.006
- Dieleman, J. L., Haakenstad, A., Micah, A., Moses, M., Abbafati, C., Acharya, P., Adhikari, T. B., Adou, A. K., Ahmad Kiadaliri, A., Alam, K., Alizadeh-Navaei, R., Alkerwi, A., Ammar, W., Antonio, C. A. T., Aremu, O., Asgedom, S. W., Atey, T. M., Avila-Burgos, L., Awasthi, A., … Murray, C. J. L. (2018). Spending on health and HIV/AIDS: Domestic health spending and development assistance in 188 countries. The Lancet, 391(10132), 1799–1829. https://doi.org/10.1016/S0140-6736(18)30698-6
- Dolowitz, D., & Marsh, D. (2000). Learning from abroad: The role of policy transfer in contemporary policy-making. Governance, 13(1), 5–23. https://doi.org/10.1111/0952-1895.00121
- The Global Fund. (2020). The Global Fund. Retrieved August 5, 2020, from https://www.theglobalfund.org/en/government/.
- Gourlay, A., Birdthistle, I., Mburu, G., Iorpenda, K., & Wringe, A. (2013). Barriers and facilitating factors to the uptake of antiretroviral drugs for prevention of mother-to-child transmission of HIV in sub-Saharan Africa: A systematic review. Journal of the International AIDS Society, https://doi.org/10.7448/IAS.16.1.18588
- Grépin, K. A. (2012). Efficiency considerations of donor fatigue, universal access to ARTs and health systems. Sexually Transmitted Infections, https://doi.org/10.1136/sextrans-2011-050148
- Howlett, M. (2018). Moving policy implementation theory forward: A multiple streams/critical juncture approach. Public Policy and Administration, 34(4), 405–430. https://doi.org/10.1177/0952076718775791
- Howlett, M., Mcconnell, A., & Perl, A. (2014). Streams and stages: Reconciling kingdon and policy process theory. European Journal of Political Research, 54, https://doi.org/10.1111/1475-6765.12064
- Jenkins, R. (2007). The meaning of policy/policy as meaning. In S. Hodgson & Z. Irving (Eds.), Policy reconsidered: Meanings, politics and practices (pp. 21–36). Policy Press Scholarship Online.
- Kalua, T., Tippett Barr, B. A., van Oosterhout, J. J., Mbori-Ngacha, D., Schouten, E. J., Gupta, S., Sande, A., Zomba, G., Tweya, H., Lungu, E., Kajoka, D., Tih, P., & Jahn, A. (2017). Lessons learned from option B+ in the evolution towards test and start; from Malawi, Cameroon, and the United Republic of Tanzania. Journal of Acquired Immune Deficiency Syndromes (1999), 75(Suppl 1), S43–S50. https://doi.org/10.1097/QAI.0000000000001326
- Merriam, S. B., Johnson-Bailey, J., Lee, M.-Y., Kee, Y., Ntseane, G., & Muhamad, M. (2001). Power and positionality: Negotiating insider/outsider status within and across cultures. International Journal of Lifelong Education, 20(5), 405–416. https://doi.org/10.1080/02601370120490
- Ministry of Health and Social Welfare National AIDS Control Programme (NACP). (2012). Tanzania elimination of mother to child transmission of HIV Plan, 2012–2015. The Government of the United Republic of Tanzania.
- Moran, M., Skovdal, M., Mpandaguta, E., Maswera, R., Kadzura, N., Dzamatira, F., … Tlhajoane, M. (2020). The temporalities of policymaking: The case of HIV test-and-treat policy adoption in Zimbabwe. Health and Place, https://doi.org/10.1016/j.healthplace.2019.102246
- Moshabela, M., Renju, J., Thokozani, K., Schouten, E., Njau, P., Rwebemberas, A., … Wringe, A. (2020). ‘Blueprints, blinkers, and blind spots’: The unintended consequences and ripple effects of HIV policy formulation and implementation in sub-Saharan Africa. Global Public Health, In Press.
- National Treasury. (2020). Budget review.
- Remme, M., Siapka, M., Sterck, O., Ncube, M., Watts, C., & Vassall, A. (2016). Financing the HIV response in sub-Saharan Africa from domestic sources: Moving beyond a normative approach. Social Science & Medicine, 169, 66–76. https://doi.org/10.1016/j.socscimed.2016.09.027
- Renju, J. R., Moshabela, M., Seeley, J., & Wringe, A. (2020). “Strengthening Health systems for the Application of policy to Enable (SHAPE) Test and Treat study.” Global Public Health, Editorial In Press.
- Skovdal, M., Magutshwa-Zitha, S., Campbell, C., Nyamukapa, C., & Gregson, S. (2017). Getting off on the wrong foot. How community groups in Zimbabwe position themselves for partnerships with external agencies in the HIV response. Globalization and Health, 13(1), 29. https://doi.org/10.1186/s12992-017-0253-5
- UNAIDS. (2019). UNAIDS data 2019. Geneva, Switzerland. https://www.unaids.org/sites/default/files/media_asset/2019-UNAIDS-data_en.pdf.
- World Health Organisation (WHO). (2012). Programmatic update use of antiretroviral drugs for treating pregnant women and preventing HIV infection in infants executive summary (Vol. 45). https://doi.org/10.1162/LEON_r_00464
- World Health Organisation (WHO). (2013). Consolidated guidelines on the use of antiretroviral drugs for treatmenting and preventing HIV infection: Recommendations for a public health approach. WHO.
- World Health Organization. (2016). Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection – Recommendations for a public health approach –- Second edition. https://www.who.int/hiv/pub/arv/arv-2016/en/.