ABSTRACT
Effective tuberculosis (TB) treatment has existed for more than 50 years, but TB remains a leading cause of death worldwide and in the Philippines, in part because symptomatic individuals delay or avoid seeking care. Through qualitative interviews in Pampanga, Philippines, we investigated barriers to care-seeking using a behavioural science lens. We found barriers to TB care-seeking to be shaped by: (1) ambiguous symptoms; (2) association of TB risk with lifestyle and habits; (3) expectations of stigma, discrimination, and isolation; (4) short-term costs and long-term financial burden of TB; and (5) visibility of care in public sector facilities. Findings suggest that these barriers are deeply intertwined and that, typically, it is a combination of barriers that holds back a particular symptomatic individual from seeking care, as the barriers influence implicit trade-offs related to health, social, and financial consequences of having TB or another serious illness and of seeking care or not seeking care. The findings suggest avenues for more effectively reaching those with symptoms and their family members to encourage care-seeking by elevating the perceived benefits and putting perceived costs in proper perspective.
Introduction
Effective tuberculosis (TB) treatment has existed for more than 50 years, but TB remains a leading cause of death worldwide (World Health Organization, Citation2018b). With an estimated incidence of 581,000 cases in 2017, the Philippines was ranked among the 30 highest TB burden countries, which together account for 87% of the world’s TB cases (World Health Organization, Citation2018a). The Philippines also had the fourth largest gap between reported cases and best estimates of TB incidence, or ‘missing’ TB cases (World Health Organization, Citation2018a). Missing TB cases occur when individuals are undiagnosed, either because they do not access health care or because they are not properly diagnosed when they do seek care. Moreover, not all of those diagnosed with TB begin treatment, and not all of those who begin treatment complete it. These undiagnosed and untreated cases accelerate the transmission of TB and lead to preventable death and morbidity.
In the Philippines, a large number of missing TB cases occur because symptomatic individuals do not seek professional medical care. According to the 2016 National Tuberculosis Prevalence Survey (NTPS), only 19% of Filipinos with symptoms suggestive of TB – a cough with duration of two or more weeks and/or hemoptysis (coughing up blood) – sought professional care. The remaining 81% either self-medicated or did nothing at all (Philippines Department of Health et al., Citation2018b).
The NTPS provides some insight into what holds back symptomatic Filipinos from seeking professional care. Among those with TB who experienced symptoms, the most common reason given for not seeking care was the impression that symptoms were too trivial (41%), followed by cost, including travel to the healthcare facility or days of work lost (35%); other reasons included time constraints (10%), distance (5%), and fear or embarrassment (3%) (Philippines Department of Health et al., Citation2018b). Other research in the Philippines revealed similar barriers, such as coughs being dismissed as ‘normal’ and work-related costs and hassles (Auer et al., Citation2000; Reyes & Amores, Citation2014). While these reported reasons for failing to seek care might suggest that stigma and discrimination are not an important barrier, recent qualitative research in the Philippines suggests otherwise, identifying stigma and discrimination as a reason that patients fail to seek timely care or complete all necessary steps along the care-seeking pathway (Philippines Department of Health et al., Citation2018a). Research from other settings has also suggested a range of barriers to care-seeking that include stigma as well as failure to recognise symptoms, low awareness of TB, and cost (Storla et al., Citation2008).
The differences between the barriers described by quantitative and qualitative research on care-seeking in the Philippines suggest that the reasons symptomatic people fail to seek care are not fully understood. Moreover, qualitative studies on barriers to TB care-seeking do not typically describe the causes of, relative importance of, and connections between different barriers. The more nuanced understanding of behavioural barriers afforded by such descriptions could inform more targeted policies and programmes to encourage care-seeking.
Behavioural science research from other contexts suggests that insight into the psychological dimensions of care-seeking may help to explain nuances of the choices and actions of symptomatic individuals. For example, it is well documented that individuals tend to avoid confronting unpleasant or frightening information, including health information, even when that information is costless to acquire and would be useful to inform their choices (Ganguly & Tasoff, Citation2016; Golman et al., Citation2017). If a similar tendency is observed in those experiencing symptoms suggestive of TB, it may help to explain the failure to recognise symptoms and provide clues as to how to more effectively encourage care-seeking by addressing the reasons it is intimidating, unpleasant, or frightening. Research has also found that health-related stigmas arise from a range of causes and lead to delay and avoidance of care for various reasons, including fear of mistreatment by providers, desire to hide the stigmatised condition from others, and self-blame (Stangl et al., Citation2019). Research that unpacks the drivers of TB stigma and their connections to care-seeking could inform more targeted interventions to encourage care-seeking through stigma reduction.
Through the lens of behavioural science, this study addresses the gaps in understanding of care-seeking, investigating the problem of delay and avoidance of care by symptomatic individuals. It helps to explain how the observed experiences of people affected by TB (PATB), expectations regarding the consequences of a TB diagnosis, attributes of the disease itself, and other features of the context experienced by symptomatic individuals combine to shape care-seeking decisions and actions. By identifying the contextual cues and psychological biases that contribute to delays in care-seeking, it suggests opportunities for innovative programme design to improve care-seeking behaviours and health outcomes for PATB.
Methods
Study context
Data was collected in the province of Pampanga of the Philippines in February 2019. Pampanga was selected for fieldwork based on its high TB prevalence (Philippines Department of Health et al., Citation2019), the relative dearth of TB research in the region to date, and guidance from representatives from the Philippines Department of Health and USAID-supported TB programmes in the Philippines that it would generate insights of relevance to other metropolitan areas in the Philippines.
Data collection
We conducted 116 in-depth qualitative interviews with segments of participants that were expected to have different perspectives on TB, stigma, and care-seeking. These interviews investigated hypothesised barriers to care-seeking that authors generated through a review of literature on care-seeking for TB, the relation of stigma and discrimination to healthcare behaviours, and other behavioural science principles of relevance to care-seeking. Sample sizes for each segment were based on the number of hypothesised behavioural barriers relevant to their experiences and perspectives and the likely diversity of experience within the segment (both highest among PATB and community members), as well as expectations of saturation. In-depth individual interviews were employed due to the sensitive nature of the topics explored, in particular those relating to individual medical history and stigma. summarises the number of interviews conducted with each segment of participants, as well as the sampling method used for each segment.
Table 1. Interview participants.
summarises the sites visited. PATB and health provider participants were recruited through health facilities selected by the Regional Health Office, with the aim of representing a range of facility levels and geographies. Doctors and nurses who administer TB testing and dispense treatment were invited to participate in interviews at facilities where they worked at times when they were not otherwise occupied with professional obligations. PATB currently undergoing treatment were identified and invited by health providers to participate in interviews in the health facility or in their homes. Most PATB participants chose to participate in the interview at the health facility, before or after receiving treatment.
Table 2. Sites visited for data collection in Pampanga.
Family members (spouses and adult children) who accompanied PATB for treatment were identified through referrals from PATB participants. Community members, managers and employers who employ at-risk populations, and community leaders were invited to participate in interviews in community areas, places of employment, and local government buildings (Barangay Halls).
Interviews followed semi-structured interview guides and were conducted by three of the authors. All interviews were recorded with the exception of two in which participants did not give consent to record. Participants were invited to have the interview conducted in the language they felt most comfortable with (English, Filipino, or Kapampangan); most interviews were conducted with simultaneous English-Filipino or English-Kapampangan translation. The English portions of the audio recordings were transcribed by Filipino transcribers, who listened to the Filipino and Kapampangan portions to check for inaccuracies in the translation.
Interviews with health providers covered background, professional responsibilities, the testing and treatment process, and perceptions of TB and PATB. Interviews with PATB and family members covered participant background, symptoms, testing and treatment experiences, and feelings about the diagnosis and the treatment process. Interviews with PATB also investigated whether and why the participant delayed care-seeking after experiencing a cough of 2 or more weeks or any cough with blood – the symptoms for which professional medical care is recommended by the Philippines Department of Health. Interviews with community members covered participant background, health care-seeking patterns, symptom recognition, perceptions of TB risk, and perceptions of PATB. Because community members residing in a high-prevalence area were also at risk of contracting TB, their perceptions and reactions to the symptoms of TB provide insight into how a symptomatic but undiagnosed person might approach the care-seeking decision. Moreover, because the symptoms for which care-seeking is recommended are common, community members could frequently reflect on past personal experiences with those symptoms even if they had never been diagnosed with TB. Interviews with managers and employers covered these themes as well as ones related to experiencing symptoms at work, TB testing policies, and the response to a TB diagnosis.
Analysis
We employed thematic analysis using a combination of inductive and deductive analytical techniques, drawing from the approach outlined by Braun and Clarke (Citation2006). The research team generated an initial codebook of 15 topical codes from the behavioural barriers that were hypothesised prior to data collection. Extracts of text were copied into a Microsoft Excel spreadsheet and tagged with one or more topical codes. Throughout the coding process, the codes were adjusted – some were merged and others added. Early in the coding process, 12 transcripts from a range of respondent segments (approximately 10% of all transcripts) were coded by two different coders to assess and improve inter-coder reliability, following the process outlined by Campbell et al. (Citation2013). Only minor variations in coding were detected, and the codes were compared and discussed until consensus was reached to ensure consistency throughout the remainder of the process.
To evaluate the evidence relevant to the hypothesised behavioural barriers, two of the authors began by matching each hypothesis to between one and three relevant codes. Discrepancies were discussed among the team until consensus was reached. Three authors then assessed the strength of the evidence supporting or refuting each hypothesis against the amassed coded data relevant to the hypothesis. Each reviewer identified a subset of barriers that were most strongly supported by the evidence. The authors then discussed, refined, and consolidated these barriers.
Ethics
Ethical approval was obtained from the Institutional Review Board of the Population Council in the United States (protocol 881) and St. Cabrini Medical Center – Asian Eye Institute in the Philippines (protocol 2018-033). Permission to conduct the research was also obtained from the Regional Health Office, barangay (local government) administrators, and health facility supervisors. A written informed consent process was completed with each participant before beginning the interview.
Results
Five behavioural barriers to care-seeking emerged from the analysis. Each of these barriers is grounded in a feature of the context that surrounds those experiencing symptoms – past experiences, interactions with others, and attributes of the symptoms of TB – and shapes their behavioural responses. Barriers to TB care-seeking were found to be shaped by: (1) ambiguous symptoms; (2) association of TB risk with lifestyle and habits; (3) expectations of stigma, discrimination, and isolation; (4) short-term costs and long-term financial burden of TB; and (5) visibility of care in public sector facilities.
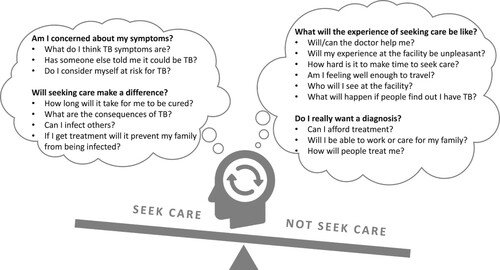
The reflections of PATB also suggest that these barriers are deeply intertwined and that it is typically a combination of barriers that holds back a particular symptomatic individual from seeking care. Symptomatic individuals face a series of implicit trade-offs related to health, social, and financial consequences of having TB or another serious illness and of seeking care or not seeking care ().
While our research does not suggest that these trade-offs are explicitly or systematically weighed, it does suggest that certain aspects of the choice loom particularly large at different moments, that the barriers described below are deeply interconnected, and that the balance of the anticipated consequences of care-seeking is perceived differently over time. When the potential for a negative experience of care or negative financial or social consequences of care-seeking is particularly salient, symptomatic individuals may avoid even considering the possibility that they might have TB. Conversely, when a symptomatic person perceives clear and salient benefits to seeking care, the barriers influence their behaviour less strongly.
Barrier 1: Ambiguous symptoms
People experiencing TB symptoms frequently do not recognise their symptoms as suggestive of TB because they hold a mental model that TB symptoms are always distinct and severe and find it reassuring to attribute milder symptoms to a less frightening explanation.
Mental model that TB symptoms must be distinct and severe
Our research revealed that people who have not yet been diagnosed with TB perceive that symptoms must be distinct and particularly severe to suggest TB or another serious illness. This perception was reflected in the initial reaction to symptoms prior to diagnosis described by PATB; it was also reflected in community members’ description of their understanding of and response to TB symptoms. Coughs are considered common and can be attributed to a range of other, non-critical conditions. For example, one community member recounted how her son was ‘coughing and coughing’ and she thought it was asthma, but eventually took him to a doctor where he tested positive for TB. Given how common coughs are, typically only very painful coughs, coughs with blood, or coughs accompanied by extreme weight loss are associated with TB. PATB and community members reflected that even chronic coughs are considered normal, and PATB commonly described thinking that their early symptoms did not seem severe enough to indicate a serious illness.
[I had the cough for] more than three months or four months … At first it's normal, and it becomes severe. (PATB)
I have a non-stop cough … I have a heavy chest and back pain. But there's no blood in my cough. I just have a normal cough. (PATB who had a painful cough but did not suspect TB)
Medicines to treat coughs are widely available in pharmacies and marketed through mass media channels, which reinforces the perception that most coughs are not serious and can be healed without professional care.
At first it was just an ordinary cough and I'm also taking medicines, the ordinary medicines that we can buy. And after that, [as] days passed by my cough [became] harder. A little bit harder until it reached two months that when I coughed, I spit out blood. (PATB)
Cases of severe symptoms come most readily to mind
Severe TB symptoms are more observable than mild or early symptoms, and people who are publicly known to have TB are more likely to display severe symptoms than others who are not known to have the disease. Anticipated stigma (described in barrier 3 below) leads some PATB to hide their illness from community members for as long as they can, but the disease becomes known to others when symptoms become so severe that they can no longer be hidden. These factors contribute to the belief among people who have not yet been diagnosed with TB that the symptoms are always severe. When asked how they know if someone has TB, community members named severe symptoms that generally do not present until the disease has advanced.
People who live there who have TB, they are vomiting with blood. (Community member)
If the person is thin or seems to be unhealthy, I would advise him or her to ask for the consultation with doctor. (Community member, who reflected that she knows who has TB based the person’s figure)
People tend to confuse the ease with which an instance is recalled (such as observing someone with very severe TB symptoms) with its representativeness (the likelihood that other PATB will have similarly severe symptoms) – a phenomenon known as availability bias (Gabrielcik & Fazio, Citation1984). Availability bias may contribute to the perception that TB is unlikely unless severe symptoms are present.
Barrier 2: Association of TB risk with lifestyle and habits
People who have not yet been diagnosed with TB describe a mental model of who is at risk of contracting TB that excludes themselves. Those who experience symptoms are motivated to avoid acknowledging those symptoms or to find an alternative explanation.
Mental model of risk focuses on others
The community members interviewed all resided in areas with high TB prevalence and as a result were at risk of contracting the disease. However, those who had not been diagnosed with TB expressed a perception of who is at risk for TB that excluded themselves: people of lower socioeconomic status than themselves, people who displayed vices that they did not have, or people who displayed vices they did have, but practiced with lesser intensity.
Most of those who are infected by TB are the ones who are poor and less fortunate. Because they’re the ones who mostly do those things like smoking, staying up late and lacking sleep. (Community member)
Here? None [of the people in this community get TB]. It’s the less fortunate ones. (Community member)
Community members also described other unhealthy behaviours or conditions related to socioeconomic status, such as poor nutrition, as a reason for elevated TB risk.
[The people most at risk for TB] have low income, those people who have so many children, they will just drink coffee and a piece of bread. (Community member)
I think I have a low chance of getting TB. … Of course I avoid those … like cigarettes, and drinking. Me myself, I don’t drink. (Community member)
[People most at risk are] poor, lack of food, vices … lack of sleep because of drinking, because of gambling. (Community member)
These strong associations of TB with self-control-related vices, poverty, and dirtiness were commonly reported alongside social judgment, stigma, and blame.
[TB risk is highest among] people who are not that well-off in terms of finance and who live in places where it’s dirty, you know? It’s not suitable for them. (Pharmacist)
[TB risk was highest] in the squatter’s area because all the sickness and diseases are there. … Children in the depressed areas are not taken care of by their parents. (Community member)
It's really up to them. And I believe it’s their fault because instead of buying food, they instead buy alcoholic beverages. That’s what they prioritize, that’s how, that’s why they ended like that. (Community member)
Experiencing symptoms challenges one’s conception of risk and self
If a person constructs a mental model of what (other) type of person is at risk for TB but later experiences TB symptoms, that person is faced with new evidence that conflicts with existing beliefs about their own risk of contracting the disease. This invokes cognitive dissonance, the mental discomfort experienced when a person holds contradictory beliefs (Festinger, Citation1962). People are strongly motivated by cognitive dissonance to resolve contradictions, and a person experiencing TB symptoms can do this in one of three ways.
First, the symptomatic person might reassess their personal TB risk and admit to engaging in risky behaviours or holding other undesired attributes. However, few participants (PATB reflecting on their own TB diagnosis or community members reflecting on their past experience with TB symptoms) showed willingness to do this. Such an admission would be psychologically painful, requiring them to admit something at odds with the positive image they hold of themselves.
A second possible response to resolve the cognitive dissonance is for the person experiencing symptoms to update their mental model of risk factors in a way that preserves a positive self-image. PATB and their families did this in some cases after receiving a diagnosis by attributing their own TB to hard work. Hard work is viewed in the local context as honourable or at least neutral, which allows PATB to escape blame and judgment from both themselves and others for acquiring the disease.
When I’m driving the tricycle it’s dusty, so, so hot. … It will rain, I’m getting cold, I get wet, even my feet. That’s the reason, I think. … But in the other case of those people, yes, they are drinking, they are smoking. But in my case, you know what, I think I got this sick not because of the smoking, but I got this when I’m driving the tricycle. (PATB)
I keep asking myself where did I get this TB. … They told me that it is – we can get it by smoking. But for me, it’s not just about smoking because maybe for hard work. Because I … carry half-sacks of camote. (PATB)
The third and most common resolution of the cognitive dissonance is for a person experiencing symptoms to attribute the symptoms to some cause other than TB, and avoid recognising that they may be at risk of contracting TB. This response was commonly reported by PATB to be their initial reaction to the symptoms, as discussed above (barrier 1). Because it does not require individuals experiencing symptoms to challenge an existing belief about themselves or their risk of contracting TB, it is likely to be the least cognitively taxing response.
Barrier 3: Expectations of stigma, discrimination, and isolation
Reactions of disgust to TB are common, leading communities and sometimes families to isolate and judge PATB. Anticipated stigma elevates the social cost of a diagnosis and deters care-seeking among people experiencing symptoms.
Fear of infection and disgust drive stigma
Consistent with prior research on stigma (Courtwright & Turner, Citation2010; Stangl et al., Citation2019) we found that the drivers of stigma include fear of infection, which leads to avoidance and isolation.
Several participants noted that extreme isolation of PATB was not common anymore since people now understand that TB is curable. However, many also remembered that it was not always curable or knew of people who had died of the disease, and our interviews revealed that isolating practices and experiences continue. We found that modes of infection are misunderstood and sometimes exaggerated, specifically transmission through sharing utensils and being in close proximity to PATB.
If you go to their house, you will eat with them, their breath, you can smell, or … you might have TB. (Community member)
PATB also described isolating in ways that health workers had explained to them were unnecessary. For example, one PATB shared that he had been told at the health centre that separating utensils was not necessary, but that some TB patients and his mother believed that he needed to separate utensils. Insistence on isolation to eliminate all risk of transmission to loved ones, even when it implies emotional pain for the PATB, may be explained in part by the certainty effect. The certainty effect describes people’s tendency to overweight the benefit of moving from an extremely low risk to zero risk (Tversky & Kahneman, Citation1981).
In addition to intentional risk avoidance in reaction to fear of infection, our research highlighted a connection between contagiousness and automatic feelings of disgust.
They felt like I’m so disgusting … because some people know that if you have TB, it’s so infectious. (PATB)
Anticipated stigma elevates the social cost of a diagnosis
Anticipated stigma and isolation represent immediate social costs for PATB, which can deter care-seeking. By contrast, people with TB symptoms who had some assurance from family members of not being stigmatised or isolated as a result of a TB diagnosis reported seeking care more promptly.
Even the people beside me then they went away when they found out that I have TB. My daughter got mad; ‘They don’t want to be beside you? I will sit beside you.’ (Recovered PATB)
[The one who brought up care-seeking was] us, his children and his in laws as well as his wife. … We said that we will have it checked, then you just have to take your medication continuously and seriously and eat the nutritious food. We did everything we can, all the effort we exerted to support him. (PATB’s daughter-in-law)
Barrier 4: Anticipation of large and uncertain financial burden
The unpredictable direct and indirect costs of TB loom large. Fear of not being able to continue working within or outside the household threatens identities as caregivers and breadwinners, providing further incentives to avoid confronting the prospect of a TB diagnosis.
An expectation of large and uncertain costs make the prospect of TB frightening
TB testing and treatment are free in public sector facilities in the Philippines, and most community members interviewed were aware of that fact. Participants generally expressed an understanding that those who needed treatment would be able to access it. Nonetheless, community members described significant and unpredictable indirect expenses related to TB treatment, which contribute to the perception that having TB is expensive.
Tuberculosis [is expensive]. Those people that have tuberculosis mostly go to the health centre to get medicine. But sometimes if there’s no available medicine they go to the hospital office for additional medicine or other medicines they can recommend. If the centre ran out of medicine they will have to go to the city health office so that’s where they get their medicine. (Community member, reflecting on which illnesses cause people to spend a lot of money)
The thing is, even if you will take medicine, if you don’t have food to eat, it’s useless. … If you have TB or you are taking meds, you must have good food, delicious foods for you to contradict the taste of those medicines. (PATB)
The prospect of not being able to continue working because of weakness or pain due to the illness or medication or because of required leave due to infectiousness weighs particularly heavily on people’s minds. Losing a job implies significant expense, and this possibility may lead an individual to defer care-seeking until the symptoms become so severe they are not able to work normally.
[People delay seeking care because of] finances, lack of finances, or sometimes they will just think of their family instead of themselves … for the cost of medications, their travel cost, or they might lose their job because of it, because of the effect of the medications. (Public health provider)
Inability to work threatens identity
In addition to the anticipated financial consequences, PATB reflected on the emotional hardship caused by not being able to continue their daily work in or outside the household. For men, this hardship was primarily felt in not being able to financially support their families, while for women it was more commonly related to the inability to play the role of caretaker within the household.
[Before seeking care I worried] if I get sick, how about my family … how would they live if I'm not there? (Female PATB)
[TB was] a big problem. I pawned some of our things. For more than 6 months [I was unable to work]. (Male PATB)
Before [going to the doctor] I was really sad. I was thinking a lot. Of course I’m worried about my family, that they might not able to eat. (Male PATB)
Interview responses suggest that not being able to work or contribute may threaten core elements of social identity and self worth, as people fear losing their role as caretaker or breadwinner, or being a burden on their families.
The hardest thing on my part is that I cannot help my family because I need a rest. It’s a big problem for me. I think I’m worthless. (Male PATB)
Barrier 5: Visibility of care in the public sector
The visibility of TB testing and treatment services leads people to expect that seeking care at a local public facility would reveal their TB status to others. The separation of TB services from other services at health facilities may prime people to anticipate similar isolation in their communities.
Care-seeking for TB is expected to expose TB status
PATB believe that seeking care at a public health facility leads to others finding out that they have TB, while anticipated stigma means that most would prefer to keep their diagnosis private. Public providers recounted stories of people who did not want to seek care at their local facility for this reason.
We have a patient, he’s from another barangay but … he doesn’t want to get meds from that barangay. So we think that he’s ashamed that his co-barangays might know that he has that kind of disease. So he is getting his meds from us, but not from his barangay. (Public health provider)
Because there are a lot of people going to the health centre, and most of the time I know all the community members here, so one of them is there. That’s the time I worry that [someone] may know that what my illness is. (PATB)
Symptomatic individuals may overestimate the visibility of care-seeking behaviour
Respondents commonly mentioned that community members can see who is at the facility for TB treatment.
Because they see this patient go in there every day, taking the medication, so they – even if the nurses or the health staff will not tell you that this is TB – they will know. Yeah, because they’re the only ones there. I mean, going there every day to take medications. ‘Ooh, it’s probably TB.’ (Public health provider)
Because you can see. Because sometimes he will remove his t-shirt and you can see in his figure and his back pain. … [The] sounds that he is making every morning that he wakes up, he is spitting phlegm, we can hear him. (Community member, reflecting on how he knows that a neighbour has TB)
Discussion
Our study builds on existing work related to delays in care-seeking for TB and the experience of TB stigma. Existing research has suggested reasons why those with symptoms may delay care-seeking. This study builds on that research by bringing a behavioural science perspective to identify psychological bases for barriers to care-seeking and ways in which barriers are interconnected. This additional lens deepens our understanding of the emotional and psychological experience of TB testing and treatment and resultant stigmatisation and isolation and helps to explain the differences in the relative importance of different barriers found in previous studies. It also helps identify more targeted opportunities for intervention to encourage care-seeking.
Several of our findings support and add to prior work. For instance, other researchers have noted that symptomatic individuals may fail to recognise symptoms (Storla et al., Citation2008). They have not consistently attributed these gaps to intentional avoidance of a feared diagnosis or a drive to preserve one’s positive self-conception by downplaying TB risk. Similarly, while others have noted that cost may be a barrier to care-seeking for some individuals (Reyes & Amores, Citation2014), prior studies have not described the psychological pain associated with a threat to one’s identity as a breadwinner or caregiver. Literature on TB has proposed that the physical aspects of testing and treatment facilities affect patients’ experience of treatment (Storla et al., Citation2008), and our work builds on this finding by proposing how these physical features may prime those with symptoms for an uncomfortable experience even before they pursue testing, hampering an initial care-seeking step.
An additional contribution of this study is its analysis of the series of trade-offs symptomatic individuals make as they experience, assess, and respond to their symptoms and make choices to seek care or avoid or delay care-seeking. The patient journey with regard to TB has been previously mapped; this study describes in detail how symptomatic individuals may assess costs and benefits they perceive to be associated with seeking care, and how these assessments may change over time. This description of barriers encountered along the patient journey elucidates how, given the strong incentives symptomatic individuals face to avoid confronting the prospect of a TB diagnosis, other obstacles and hassles to care-seeking exert an outsized effect. It also underscores the strong positive effect on care-seeking that can stem from efforts to reduce the perceived costs and to highlight the benefits of care-seeking, such as encouragement and reassurance from a loved one.
Several limitations may apply to this work. Our findings may be subject to bias due to the way questions were asked during interviews, though our systematic process for generating a large number of hypothesised barriers and for formulating interview guides to address each of these hypotheses sought to minimise bias in the data collection process. We also reviewed and revised interview guides to avoid biased or leading questions. An additional limitation is that findings may not be generalisable to other contexts, though delayed care-seeking may result for similar reasons in contexts with similar perceptions of TB and of associated stigma as well as obstacles to testing and treatment. We are unable to definitively assert psychological mechanisms believed to be at play, but where evidence indicates these concepts apply, solutions predicated on them are likely to be valid. Finally, our research is limited by the fact that it was not feasible to recruit a sample of research participants who were currently experiencing symptoms suggestive of TB and also avoiding care. Instead, we relied on the reflections of PATB who eventually sought care (many of whom had delayed care-seeking when they experienced the symptoms for it is recommended) and community members (many of whom had at some time experienced or observed those symptoms).
Conclusion
Through in-depth qualitative research in Pampanga, Philippines, we applied a behavioural science lens to identify cues in individuals’ contexts that prompt them to seek care for TB symptoms, or conversely to avoid or delay care-seeking. These contextual cues include the symptoms a person is experiencing, observed characteristics and experiences of PATB, what is said by others in the community about TB and PATB, and their own past experiences with care-seeking for other needs. This research elaborates on previous findings by documenting anticipated and experienced isolation and ostracisation associated with a TB diagnosis. It also builds on these findings by proposing the psychological mechanisms that may underlie these associations, including avoidance of symptoms, mental models of who is likely to contract TB, ambiguity around cost of testing and treatment, threats to symptomatic individuals’ identities, and cues that prime a symptomatic person to anticipate a negative testing and treatment experience. We add to the literature by describing how these dynamics interact with one another and how people experiencing symptoms may respond differently at different times. These findings provide insight into the care-seeking journey of symptomatic individuals. They also suggest avenues for more effectively reaching those with symptoms and their family members to encourage care-seeking, elevating the perceived benefits and putting perceived costs in proper perspective.
Acknowledgements
This work was made possible by the generous support of the American people through the United States Agency for International Development (USAID) under Breakthrough RESEARCH (cooperative agreement no. AID-OAA-A-17-00018). The contents of this manuscript are the sole responsibility of the authors and do not necessarily reflect the views of USAID or the United States Government.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Auer, C., Sarol, J., Tanner, M., & Weiss, M. (2000). Health seeking and perceived causes of tuberculosis among patients in Manila, Philippines. Tropical Medicine & International Health, 5(9), 648–656. https://doi.org/https://doi.org/10.1046/j.1365-3156.2000.00615.x
- Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. https://doi.org/https://doi.org/10.1191/1478088706qp063oa
- Campbell, J. L., Quincy, C., Osserman, J., & Pedersen, O. K. (2013). Coding in-depth semistructured interviews: Problems of unitization and intercoder reliability and agreement. Sociological Methods & Research, 43(3), 294–320. https://doi.org/https://doi.org/10.1177/0049124113500475
- Courtwright, A., & Turner, A. N. (2010). Tuberculosis and stigmatization: Pathways and interventions. Public Health Reports, 125(Suppl 4), 34–42. https://doi.org/https://doi.org/10.1177/00333549101250S407
- Curtis, V., de Barra, M., & Aunger, R. (2011). Disgust as an adaptive system for disease avoidance behaviour. Philosophical Transactions of the Royal Society B: Biological Sciences, 366(1563), 389–401. https://doi.org/https://doi.org/10.1098/rstb.2010.0117
- Festinger, L. (1962). A theory of cognitive dissonance (Vol. 2). Stanford University Press. http://www.sup.org/books/title/?id=3850.
- Philippines Department of Health, USAID, & FHI 360. (2019). KNOW TB newsletter. https://www.fhi360.org/sites/default/files/media/documents/png-know-tb-newsletter-april-2019.pdf
- Gabrielcik, A., & Fazio, R. H. (1984). Priming and frequency estimation: A strict test of the availability heuristic. Personality and Social Psychology Bulletin, 10(1), 85–89. https://doi.org/https://doi.org/10.1177/0146167284101009
- Ganguly, A. R., & Tasoff, J. (2016). Fantasy and dread: The demand for information and the consumption utility of the future. Management Science, 63(12), 4037–4060. https://doi.org/https://doi.org/10.1287/mnsc.2016.2550
- Gilovich, T., Medvec, V. H., & Savitsky, K. (2000). The spotlight effect in social judgment: An egocentric bias in estimates of the salience of one’s own actions and appearance. Journal of Personality and Social Psychology, 78(2), 211–222. https://doi.org/https://doi.org/10.1037//0022-3514.78.2.211
- Golman, R., Hagmann, D., & Loewenstein, G. (2017). Information avoidance. Journal of Economic Literature, 55(1), 96–135. https://doi.org/https://doi.org/10.1257/jel.20151245
- Philippines Department of Health, Foundation for the Advancement of Clinical Epidemiology, Inc., & Philippine Council for Health Research and Development. (2018a). Annex H: Missing TB cases seen in the Philippines national tuberculosis prevalence survey 2016.
- Philippines Department of Health, Foundation for the Advancement of Clinical Epidemiology, Inc., & Philippine Council for Health Research and Development. (2018b). Philippines national tuberculosis prevalence survey 2016. http://www.ntp.doh.gov.ph/downloads/publications/Philippines_2016%20National%20TB%20Prevalence%20Survey_March2018.pdf
- Reyes, K., & Amores, J. C. (2014). Barriers of early TB diagnosis among the poor in highly urbanized areas in the Philippines (Discussion Paper Series No. 2014-18). Philippine Institute for Development Studies.
- Stangl, A. L., Earnshaw, V. A., Logie, C. H., van Brakel, W. C., Simbayi, L., Barré, I., & Dovidio, J. F. (2019). The health stigma and discrimination framework: A global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Medicine, 17(1), 31. https://doi.org/https://doi.org/10.1186/s12916-019-1271-3
- Storla, D. G., Yimer, S., & Bjune, G. A. (2008). A systematic review of delay in the diagnosis and treatment of tuberculosis. BMC Public Health, 8, 15. https://doi.org/https://doi.org/10.1186/1471-2458-8-15
- Tversky, A., & Kahneman, D. (1981). The framing of decisions and the psychology of choice. Science, 211(4481), 453–458.
- World Health Organization. (2018a). Global tuberculosis report (Licence: CC BY-NC-SA 3.0 IGO).
- World Health Organization. (2018b). The top 10 causes of death. http://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death.