ABSTRACT
District health managers (DHMs) lead and manage Ministry of Health programmes and system performance. We report on the acceptability and feasibility of inter-related activities to increase the agency of DHMs in Kenya, Nigeria, South Africa and Uganda using a cross-sectional rapid appraisal with 372 DHMs employing structured questionnaires. We found differences and similarities between the countries, in particular, who becomes a DHM. The opportunity to provide leadership and effect change and being part of a team were reported as rewarding aspects of DHMs’ work. Demotivating factors included limited resources, bureaucracy, staff shortages, lack of support from leadership and inadequate delegation of authority. District managers ranked the acceptability of the inter-related activities similarly despite differences between contexts. Activities highly ranked by DHMs were to employ someone to support primary care staff to compile and analyse district-level data; to undertake study tours to well-functioning districts; and joining an African Regional DHM Association. DHMs rated these activities as feasible to implement. This study confirms that DHMs are in support of a process to promote bottom-up, data-driven, context-specific actions that can promote self-actualisation, recognises the roles DHMs play, provides opportunities for peer learning and can potentially improve quality of care.
Introduction
Transforming health service delivery is critical to achieving improved health outcomes for twenty-first century Africa. While progress has been made in the last 10 years through the adoption and resourcing of activities aimed to achieve the Millennium Development Goals, a recent Lancet Commission described the slow pace of achieving improved quality of health care in Africa as ‘a recipe for failure’ (Agyepong et al., Citation2017). African governments have committed themselves to Universal Health Coverage (UHC) in order to improve health outcomes, but UHC is dependent on modernised health systems that support primary health care (PHC) as the cornerstone of UHC (Binagwaho & Ghebreyesus, Citation2019). Essential to achieving change are: African-elaborated approaches that focus on people-centred health systems, PHC and public health (including prevention), which include a skilled workforce and improved research capacity that incorporates local generation and use of innovations (Agyepong et al., Citation2017). While the importance of leadership and management at all levels of health systems has been reaffirmed repeatedly (Bonenberger et al., Citation2015; Bradley et al., Citation2015; WHO, Citation2007), it is district health management teams (DHMTs) who are responsible for the implementation, administration and oversight of PHC programmes such as vaccination and antenatal services, treatment of HIV, TB and more recently NCDs. District health managers (DHMs) are expected to lead and manage staff and engage with external partners to achieve results under complex conditions (Daire & Gilson, Citation2014; Kawonga et al., Citation2016; Ndavi et al., Citation2009). The district level is where implementation occurs and where multiple PHC programmes intersect with health workers, health infrastructure, management style and the population served.
Importantly DHMs need the authority to be able to lead and to test innovations in service delivery in a context-sensitive manner. Decentralisation, which in theory included devolution of authority, was meant to achieve this and has been adopted in many African countries over the last 20 years. The motivation for decentralisation was that context-specific decision-making would improve allocative efficiency in service delivery and allow greater accountability and responsiveness to the local population. The evidence of the impact of decentralisation on health outcomes is inconclusive, however, due to variability of accountability structures, the complexity of relationships and contexts and poor data quality for comparative analyses (Dwicaksono & Fox, Citation2018). Inadequate resources, lack of management training, poor team-work and absence of job descriptions are some of the barriers described which impede improved health outcomes (Egger & Ollier, Citation2006; Filerman, Citation2003; Muchekeza et al., Citation2012; Ndavi et al., Citation2009). Rigid hierarchical structures which prevent local health systems (districts) from acting on their insights have also been described (Tetui et al., Citation2018). These are areas for more enquiry and research.
DHMs, often a doctor, senior nurse or an administrator, usually head a DHMT (Egger & Ollier, Citation2006; Kawonga et al., Citation2016; Ndavi et al., Citation2009; Nzinga et al., Citation2013). The skills needed to do so are not articulated and the management training required is not standard across low- and middle-income countries (LMICs). Filerman (Citation2003) distinguishes between public health competencies necessary for programme planning and evaluation, and managerial competencies related to control of and accountability for resources, effective management of personnel and assuring results. Both are essential and complementary, but ‘public health competence without a firm foundation of management skills does not produce successful results’ (Filerman, Citation2003, p. 2). This coincides with what others have argued: that management skills such as strategic problem-solving, human resource management, financial management and operations management are fundamental to health system strengthening (Fetene et al., Citation2019). Moreover, improved management arises through a complex interplay of factors at different levels, as complex adaptive systems, rather than from building individual skills and technical capacity alone (Heerdegen et al., Citation2020; Kwamie et al., Citation2014). Yet many health professionals take on management positions without any prior management training and may get further training after appointment to improve their credibility (Loh, Citation2015). Doctors are often appointed to district leadership positions after only one year of work experience while nurses may have more experience when they become leaders but rarely go through specialised training (Nzinga et al., Citation2013).
Further frustrating DHMs’ efficacy is a tendency for nationally determined programmes, often inserted as vertical interventions, to dominate. These vertical programmes often by-pass district leadership, are centrally planned and narrowly targeted, encouraged by donors, funded and managed separately from routine health services. Vertical programme managers are frequently accountable directly to national programme directors or international donors, rather than to DHMs and DHMTs. They often receive targeted investments (e.g. additional training and resources like transport) in preference to and bypassing DHMs (Henriksson et al., Citation2017; Kawonga et al., Citation2013; Kawonga et al., Citation2016).
While district health information systems generate large amounts of data that could be used for local decision-making, priority-setting, resource allocation and the planning and evaluation of district services to make them more responsive to local population health needs, they are not used in that manner (Nzinga et al., Citation2013; Wickremasinghe et al., Citation2016). Health data are often collected and collated at the district level, taking up a significant proportion of the working time of DHMs (Bonenberger et al., Citation2015), but are often not used locally by DHMs for decision-making (Kawonga et al., Citation2012; Wickremasinghe et al., Citation2016). In Uganda, district-specific evidence enabled DHMTs to draw up work plans related to articulated priorities, but they lacked autonomy and had limited decision and fiscal space to implement their ideas. Heavy dependence on funding from donor agencies with their own priorities, undermined the DHMTs’ ability to respond to their own perceived district health needs and plans (Henriksson et al., Citation2019).
Writing from a US perspective, Birken et al. (Citation2012) suggest that the role of middle managers has been neglected in the growing literature on healthcare innovation implementation, yet they play a crucial role in synthesising and diffusing information, mediating between strategy and day-to-day activities, and promoting innovative implementation (Birken et al., Citation2012). We argue that the same applies in Africa and that agency – the ability and willingness to act on issues they feel are important – among DHMs is an important ingredient in managers’ ability to effect change, implement innovations and improve quality. Along with other authors, we also stress that contextual factors, political, social and economic, in addition to individual managers’ knowledge and skills, are important in understanding the limitations that DHMs experience in LMICs (Heerdegen et al., Citation2020). Research has shown that decentralisation fails unless DHMs are given the power they need to deal with their challenges (Aberese-Ako et al., Citation2018). Central to enhancing the impact that DHMs could have is to provide them with an enabling environment in which they are acknowledged for the skills and experience they have (WHO, Citation2007).
A multi-country research collaboration seeking to develop methods to improve the efficacy of human resources for health involving senior researchers from Kenya, Nigeria, South Africa and Uganda was initiated. The research was developed in phases. The research consortium organised and met at several workshops. At the first workshop, the research consortium identified common human resource problems; at the second workshop data from document reviews, key informant interviews and group discussions with care providers and managers in each country was reviewed. We used these data and information from the scientific literature in this field to diagnose part of the problem. Our collective experiences of working in public health institutions in these and other countries (for some of us this included working in the past as DHMs) contributed significantly to our understanding of the context. We noted that DHMs operated in an environment that did not enable them to generate and implement locally developed innovations. We posited a compendium of possible activities that could increase knowledge-sharing, analytical capability, confidence and willingness of DHMs to exercise their agency. We hypothesised that these activities in combination could be useful in promoting bottom-up, data-driven, context-specific actions that promote self-actualisation, recognise the roles that DHMs play, provide an opportunity for peer learning and can potentially improve quality of care and health outcomes in the long term. To ensure we were not imposing ideas from the outside we wanted to test our ideas first. To do this, we developed data collections tools to test our hypothesis and then later met to refine our data entry and to write up our results.
The logic of the compendium of activities we developed and how they may promote agency in DHMs has been published elsewhere (Fonn et al., Citation2011) but is described briefly here. We noted that DHMs as a category were not recognised, though they had particular experiences and problems, and had implemented solutions in some instances that, if they had a forum, could be shared for horizontal cross-learning. The activities we proposed would fill a need that has more recently also been identified by others: a need for on-going reflective iterative, complex and dynamic capacity-building (Kwamie et al., Citation2014; Tetui et al., Citation2016).
The compendium of activities included providing some form of recognition for DHMs such as an autonomous recognised professional association. Importantly, the association should include a forum where local research undertaken by DHMs can be presented. We envisaged that DHMs would use the district health information they already collect to review their own services, implement changes as required and monitor the impact of such changes. This would provide opportunities for peer learning and encourage local research to produce bottom-up data on which to plan or assess local initiatives. We noted that technical support at the district level to analyse local data may be required so we included this support in the compendium of activities. We postulated that DHMs study tours to well-functioning districts would provide for peer learning and would validate the work undertaken by DHMs. Our research, presented in this paper, tested the acceptability and feasibility of these activities.
The purpose of this paper is to document the opinions of DHMs in four countries in Africa regarding the acceptability and feasibility of a set of inter-related activities that could enable them to develop greater agency and innovation in their work to improve the quality of healthcare. We also collected data on DHMs’ perceptions of their work environment in order to describe the various contexts in which they work and the relevance of such interventions in each context. The study presented here was conducted in Kenya, Nigeria, South Africa and Uganda. These countries were chosen based on an existing collaboration amongst researchers from these countries, and because they represent Western, Eastern and Southern Africa where there has been a range of experiences in district health services.
The analyses presented here are of data collected in 2010, which is a limitation of this study. However, the activities we tested in this study aim to address problems that resonate with current discussions and give attention to gaps that are reported to persist in health systems in Sub-Saharan Africa now. It is still reported that DHMs need the space to be more innovative, engaged and motivated to improve the quality of care for their populations, and for them to be recognised for the important role they play (Aberese-Ako et al., Citation2018; Tetui et al., Citation2018). There are two reasons why the findings presented here are still relevant. Firstly interventions similar to the inter-related activities tested in this study have, subsequent to our study, shown some success at national levels such as through health leadership and management courses and mentorship (Edwards et al., Citation2015; Mutale et al., Citation2017). There are also examples where the strong leadership capacity of mid-level managers led to innovations and flexibility in ensuring essential services continued (Mccollum et al., Citation2018). These findings show that opportunities where DHMs can learn from each other are relevant and could be scaled up for greater impact, as we propose. Secondly, while the context in each country has changed since our data were collected; similar limits to DHMs’ decision-making space exist even now, for example, in Uganda, as described earlier (Henriksson et al., Citation2019). Kenya changed from a mainly centralised health service to a devolved one in 2013, with expectations of greater efficiency, equity and expansion of UHC and improved service delivery. Despite these changes, considerable variations have been found in priority-setting in health planning and budgeting by key decision-makers at the county (district) level. In South Africa, the White Paper on the new National Health Insurance Scheme, the vehicle chosen by the government for achieving UHC, was only published in 2017 (South African National Department of Health, Citation2017). However, it has been noted that disparities between districts, including differences in a district management capacity, may frustrate implementation (Fusheini & Eyles, Citation2016). More recently, it has been reported that the quality of primary care provided across districts is very variable (Muthathi & Rispel, Citation2020) and that considerable attention is needed to establish decentralised structures such as districts (Blecher et al., Citation2019).
Materials and methods
This exploratory cross-sectional rapid appraisal was carried out simultaneously in Kenya, Nigeria, South Africa and Uganda by the locally based research groups who were members of our research consortium. DHMs from urban and rural government district health facilities were interviewed in these four countries using structured questionnaires which were either self- or interviewer-administered. Where self-administered the researchers were present to answer questions either in person or by telephone. The questionnaire included open-ended and closed questions on demographic characteristics, job satisfaction, what they liked and disliked about being a DHM, what prevented the provision of quality of care in their districts, and factors that impeded them from doing their work well. Some questions required DHMs to choose between a set of options and rank which most affected them. DHMs were asked to rank the top five factors affecting their performance at work; they were also asked to choose and rank interventions they thought were most desirable to increase their effectiveness as managers. The individual rankings were aggregated using two different methods. First, we analysed the proportion of DHMs selecting each factor as the most important factor. Second, the full rankings were analysed using a form of the Borda count method (Black, Citation1976) where first choices score 5, second choices score 4, etc., and the sum of these scores for each factor is then used to rank them. The acceptability and feasibility of particular activities to improve district management were tested by asking DHMs to rank the desirability of the compendium of activities and indicate if they thought them feasible.
Data from the questionnaires were entered in Epi-Info and analysed using Stata v14. Country data were collated and a single combined data set was created. Open-ended questions were coded using the entire data set to get uniformity across all sites.
Study sample
Kenya comprises eight provinces. Nairobi was excluded as this large urban area is not run on a district model. For the remaining 7 provinces, 92 DHMs were conveniently selected from across 46 districts based on where district managers were available because district meetings or training sessions were taking place, making interviewing logistically possible.
In Nigeria, the equivalent of a DHM is the PHC coordinator in the Local Government Area (LGA), who is usually a Community Health Officer (CHO). The CHOs are usually nurses or midwives who have undergone an additional 2-year training programme which includes some management skills. LGAs in each state were listed and every third LGA was selected giving 240 LGAs. The response rate was 92% with 222 PHC coordinators participating.
South Africa has 52 designated districts. All DHMs were invited to participate. Repeated calls to each DHM were made to arrange face-to-face interviews in the first instance. If unsuccessful, telephone interviews were conducted with the DHMs who received the interview schedules in advance of the phone call. After many attempts, 31 DHMs (60% response rate) were successfully interviewed.
In Uganda, 27 districts were randomly selected from a total of 77 after stratifying by region (south-west, western, northwest, northern, eastern, central and Kampala), urban and rural and better and worse functioning districts based on available health indicators and outcomes. All district managers from the selected districts were interviewed.
Ethical approval was obtained in each country by the lead institution in that country as follows: in Kenya from the Institutional Research and Ethics Committee of Moi University and Moi Teaching and Referral Hospital, Eldoret (FAN:IREC 000423), and district health management at all involved facilities; in Nigeria from the Research and Ethics Committee of the Oyo State Ministry of Health, Ibadan and Ethics Review Committee of Zamfara State, Gusau; in South Africa from the University of the Witwatersrand Human Research Ethics Committee (Medical) (M090674), from relevant ethical review bodies of each province, and from the National Department of Health; in Uganda from the Makerere University Faculty of Medicine Research Ethics Committee (REF_2009_134) and the Uganda National Council of Science and Technology.
Results
The characteristics of the 372 DHMs interviewed are shown in . The managers were mostly men, except for South Africa where just over half the managers were women. They were younger in Nigeria and Kenya than in Uganda and South Africa. In Uganda and Nigeria DHMs were in their positions longer than in Kenya and SA. In Uganda, South Africa and Kenya the majority of DHMs reported having a higher qualification (post-school certificate, diploma or degree) compared to only 10% in Nigeria. Roughly 50% of managers in Kenya and 70% in Uganda were doctors (with a medical degree or a specialist Masters in Medicine qualification) compared to 1% in Nigeria and 16% in SA. South African DHMs reported the highest number of MPH or MSc degrees, almost 39% compared to just under 10% in Kenya, 7.4% in Uganda and 0.5% in Nigeria. Over 80% of DHMs interviewed in all four countries were members of a professional association.
Table 1. Characteristics of district managers interviewed in each country.
As the countries differ it was important to understand how DHMs perceived their own jobs. We, therefore, explored DHMs’ job satisfaction using a 5-part Likert scale. This is presented as an average out of five (five being very satisfied) in . Respondents were asked to rate their degree of satisfaction with their job overall, their salary, their current working conditions, their supervisor (to whom they report), their relationship with their colleagues and their profession independent of their present job. The question on satisfaction with salary was excluded in error from the questionnaire in Uganda. In both Kenya and Nigeria, DHMs reported their relationship with colleagues as satisfactory and rated it the highest, followed by being satisfied with their profession; they were least satisfied with their salaries. This was similar in Uganda in that they too rated their relationship with their colleagues and their profession as most satisfying, but they were least satisfied with their current working conditions. In South Africa, DHMs rated their job in general and their relationship with their colleagues the highest and their salary and current working conditions were rated the least satisfying. There were similarities across the four countries where relationships with colleagues and their profession and or job being satisfying.
Table 2. District health managers’ assessment of their jobs.
Again, to explore if there was any homogeneity among DHMs, they were asked what they found most rewarding and most demotivating about their jobs (). Responses to these open-ended questions were coded after the data were collated. This provided an opportunity to understand, within each national context, the factors that motivate and discourage DHMs who are important linchpins in health system functioning in many African countries. The percentages show the proportion of DHMs in each country that spontaneously mentioned each factor. Across all four countries, the opportunity to provide leadership and effect change emerged as the most (or second most in Nigeria) rewarding. In Uganda, 100% of DHMs reported this spontaneously while in Kenya 85% and in South Africa 74% reported this as motivating. In Nigeria, ‘being part of a team’ was what DHMs enjoyed the most about their jobs, with just under 67% giving this response. In Nigeria, this was followed by leadership and the opportunity to effect change and ‘benefitting and working with communities’ with 44.4% reporting this as motivating. ‘Being part of the team’ was also the second most rewarding part of the job in both Kenya and Uganda. In South Africa, the space to innovate was the second most important motivating factor for DHMs followed by benefitting and working with communities at just under 52% and 42% respectively. There were thus some similarities in what DHMs found motivating.
The factors that demotivate DHMs () were more varied across the countries than the factors that motivate them. Kenyan DHMs reported the greatest range of issues though limited financial resources were mentioned most often (by 82% of respondents) followed by staff shortages mentioned by 28% of respondents. In Nigeria, three factors that demotivated DHMs were mentioned: lack of support from leadership (69.2% of respondents), bureaucracy (31%) and limited financial resources (23%). South African DHMs also reported a range of demotivating factors. The most frequently reported was lack of support from leadership reported by 53% of DHMs, followed by limited financial resources (43%), while the degree of delegation of authority was demotivating for 30% of respondents. In Uganda, limited financial resources was the most reported demotivating factor (73%) followed by staff shortages (27%).
To assess the commonality between the experience of the DHMs in our survey with other DHMs in other LMICs, DHMs were presented with fifteen different options (listed in ) that have been reported to affect the work performance of DHMs. They were asked to choose the top five factors that affected them and to rank these five from the most to least important. presents the weighted average of their cumulative ranked top five choices with 1 being the most important obstacle and 15 being the least important. Too much work featured in the top three for all four countries. Inadequate salary was the top choice in Kenya and Uganda but ranked as fourth and seventh for Nigeria and South Africa, respectively. Inadequate physical infrastructure ranked as the top obstacle in South Africa and was ranked second in Kenya and Uganda but ranked only 14th in Nigeria. Nigerian managers ranked inadequate training as the most important obstacle.
Table 3. Rank of factors affecting performance at work by country.
A major aim of this study was to assess the relevance of a set of activities to improve agency among DHM. The DHMs surveyed were asked to select and rank their top five activities from a list. Additional options, outside of those that we specifically wanted to test, were included in the survey and we also provided an opportunity for DHMs to include other interventions. In , we present the weighted ranks of the activities chosen by the DHMs. For Nigeria, South Africa and Uganda, the highest-ranked activity was to employ someone to support primary care staff with record reviews by compiling and analysing monthly statistics. Undertaking a study tour to understand how another district worked was highly ranked; first choice for Kenya, second choice for South African and Uganda, and third choice for Nigeria. DHMs in all four countries ranked joining an African Regional District Health Managers’ Association in their top five.
Table 4. District manager’s scoring (sum of ranks) of activities they would like to undertake to improve job satisfaction and patient care (1 = highest rank).
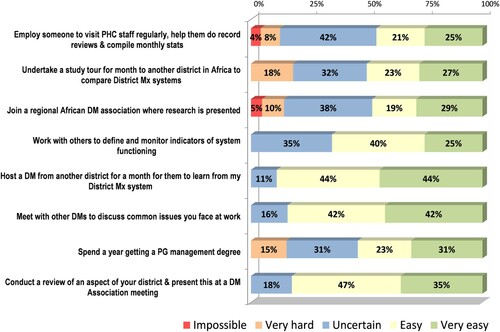
We asked DHMs for their views on the feasibility of carrying out the proposed activities that they ranked highly (their first five choices). The results are summarised in where the data are summarised as impossible (I), possible (P) or easy (E) to implement. Very few of the activities seemed impossible to DHMs to implement, except for spending a year getting a post-graduate management degree in Uganda where one third of DHMs categorised this as impossible. This activity was considered easy to implement by over 50% of DHMs in South Africa and Nigeria, and 27% in Kenya. The activities thought to be most feasible to implement were hosting a DHM from another district, meeting with other DHMs to discuss common issues faced at work, and conducting a review of an aspect of the district to present at a DHM association meeting.
Table 5. Percentage of DHMs agreeing that proposed activities are Impossible (I), Possible (P) or Easy (E).
In , we pooled the data from all four countries addressing only those activities that we hypothesised would recognise and motivate DHM to give an estimate of the collective rather than country-specific views on the feasibility of the inter-related activities. The data suggest that a Sub-Saharan Africa initiative to improve the performance of DHMs in decentralised health systems would be possible.
Discussion
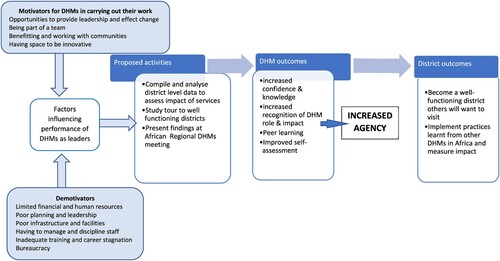
This study investigated the acceptability and feasibility of a set of inter-related regional African activities to promote agency among DHMs. provides a conceptual framework showing linkages between the factors influencing the performance of DHMs as leaders and proposed activities for change.
Figure 2. Conceptual framework showing the linkage between factors influencing teh performance of DHMs and proposed activities for change.
For regional activities to be relevant they need to be acceptable and feasible in diverse contexts and to a range of DHMs. We tested this in four countries in Africa that have different characteristics in how their health services are organised and in who becomes a DHM. It is vital to avoid imposing a one-size-fits-all solution to the variety of experiences in different contexts. Instead, the responses that DHMs would generate through the processes proposed here exploits the various circumstances across the region and enables DHMs to share learning with each other. This proposed approach specifically recognises that diversity and enhances the richness of experience. The concept of districts and DHMs varied amongst the four countries. The Nigerian respondents were to some extent outliers in that they were younger, with less training and fewer higher qualifications; only 10% of the Nigerian sample had a post-secondary education qualification. However, Nigerian CHOs, as well as being nurses or midwives, have two years of additional training which includes management training though we were not able to document the degree to which the training included management skills. In addition, this training is not certificated. In the other countries included in this study, almost all DHMs had some post-secondary degree. All DHMs in Uganda are now required to have an MPH, which many study for after appointment (Egger & Ollier, Citation2006). Apart from those with a Masters in Public Health (MPH) that may or may not include health management skills, it is not clear that they received any management training. Even if there is some management training included in these qualifications or additional training, it is not clear that it adequately equips DHMs with the skills required to manage health services that are fraught with urgent, competing demands. Other differences included the poor representation of women as DHMs except in South Africa, that they were predominantly doctors in Uganda and Kenya but nurses in South Africa and CHOs in Nigeria. Their average age and period of service as DHMs also differed somewhat. Nonetheless, all those interviewed played management and oversight roles in health service delivery in a defined geographical area – in other words, they would be eligible and appropriate to participate in the activities we were testing.
There were also commonalities amongst them. The DHMs included in this study said they were motivated by being able to innovate, leading and effecting change. They identified health system inadequacies, lack of planning and leadership, bureaucracy, financial and staff shortages as holding them back and compromising their ability to develop and lead initiatives to improve health system functioning. Thus, in spite of differences between the various countries, there were similarities in what motivated and frustrated them and they ranked the possible interventions similarly enough and considered a regional intervention to be feasible. We argue that running this at a regional level will elevate the status of DHMs and allow for inter-country learning.
Participants were offered a set of possible activities which included those we wanted to test plus others as well as allowing for additional suggestions that they could generate themselves. Our aim here was to attempt to offer a range of possible activities so that we did not bias them towards our suggestions, albeit that they were based on formative research in each country.
The highest rank was given to a solution to better manage district health information by employing someone to visit facilities regularly to assist health staff with record reviews and analysis of monitoring statistics to allow for the local understanding of performance, challenges and outcomes. This has the potential to enhance context-specific solutions and innovation, promote local ownership of health interventions and potentially increase motivation to implement changes. DHMs also proposed working with others to define indicators of health system functioning for which data would be collected on an on-going basis. These activities would require capacity development of decision-makers to use the data, such as the use of decision support tools, analysis and presentation of data at research meetings, and peer exchange (Henriksson et al., Citation2017; Kawonga et al., Citation2013; Wickremasinghe et al., Citation2016). Our envisaged African Regional District Health Managers Association meeting would provide such a forum.
The top five inter-related activities identified by DHMs included learning tours to other districts, exchange visits between districts and joining a regional African DHM association where locally generated district research is presented at an annual meeting. Discussion of common issues with other DHMs also had some support. Learnerships and exchanges could be organised for DHMs to visit identified well-functioning districts and centres of excellence in the same or different countries. Such ‘sabbaticals’ provide opportunities for enquiry, reflection and rejuvenation which could improve the motivation and confidence of DHMs, learning from peers, observing good practices and promoting cross-fertilisation of ideas. The aim of this activity would be to validate local knowledge and innovation and to counter the notion that solutions are mainly found outside Africa. DHMs would learn how to identify those aspects of successful health systems that could be adapted for their own context, and motivate them to exercise agency by taking action to implement learning once they return. The aim of learning visits would be to observe good practice and management rather than providing services, so logistical problems related to professional registration should not arise.
Participants ranked highly the development of a regional African DHM association that held an annual meeting at which DHMs would present operational research projects, successful problem-solving exercises and clinical audits, thereby demonstrating local use of district health data. Through these meetings, the attributes that make some districts successful in achieving their goals and provide high-quality care to communities would be publicised and celebrated. The association would give recognition to district management and promote professionalisation of the management process. While this may be similar to the Institute of Healthcare Managers in South Africa, functioning since 2003, which offers a possible example, its membership is mainly from the private sector and it is not clear to what extent it promotes these concepts of professionalism (Egger & Ollier, Citation2006).
While upstream factors such as the degree of authority delegated to DHMs still has to change, nonetheless, there are examples where DHMs have successfully led changes that offer experiences and lessons to share. Ad-hoc learning visits and learning networks have featured in other research projects and have been successful in getting district staff to advocate for change in some settings (Egger & Ollier, Citation2006). In Mozambique, teams of mentors were deployed to build capacity for DHMs by equipping them with skills in planning, priority-setting and problem-solving. Indicators of success were that more district mentoring visits took place, there was greater transparency in district spending and more of the workforce achieved advanced career development (Edwards et al., Citation2015). In Tanzania, researchers noted that the success of a community-based health finance scheme depended on the personal initiatives of DHMs. They recommended that an arrangement where well-performing districts shared good practices with other districts may improve overall uptake of the scheme and emphasised the importance of horizontal relationships and networking in decentralised health systems (Kigume & Maluka, Citation2019; Maluka, Citation2013).
DHMs who can demonstrate their ability to lead may inspire confidence and force change from the bottom-up. The leadership role required of DHMs is to create a conducive environment for learning, change and innovation implementation, through the motivation of frontline health workers, and mediating between strategic goals and day-to-day activities (Birken et al., Citation2012; Nzinga et al., Citation2013). Peer learning between DHMs presents an opportunity to develop this. Motivational systems to encourage managers to be competent in their jobs, peer feedback, mentoring and coaching and sharing interventions to improve quality have demonstrated positive outcomes (Egger & Ollier, Citation2006; Nzinga et al., Citation2013). Management-led quality improvements through a structured system of engagement of managers have also improved quality (Birken et al., Citation2012).
The proposed multi-faceted inter-related activities tested in this study include a regional DHMs annual research meeting using local district data and study tours across the continent where DHMs could visit a well-functioning district for learning purposes. Providing a space for DHMs and DHMTs collectively to analyse and review what they do and how they do it may improve DHMs’ confidence and ability to act as change agents within their districts. Using the local health systems data generated by district staff could facilitate self-reflection and prompt local problem-solving and action – that is, evidence-based agency. They would be enabled to exercise their decision space, defined as the extent to which DHMs can make choices or exercise authority over health system functions currently constrained by central level priority-setting (Bossert & Beauvais, Citation2002; Henriksson et al., Citation2017).
The activities tested in this study would benefit DHMTs and other health cadres as well as DHMs and promote health systems development more generally. It would recognise management of health services as a significant, distinct and valued task, providing opportunities for professionals with management expertise to provide training relevant to DHMs in Africa. Management training that is practical and oriented to problem-solving approaches could be provided through a range of in-service activities such as exchange visits and short courses run through a regional DHM association or offered at the proposed annual regional meetings. While attending further training and getting a higher degree such as a DrPH (Doctorate in Public Health) may be desirable for some DHMs and can be pursued, many African DHMs would not qualify for such a course (Agyepong et al., Citation2018). A system-wide, rather than an individual-oriented approach, that facilitates tacit and peer learning and that can reach a greater number of DHMs may have a greater impact on health care services.
Limitations and reflection
The data presented here was collected in 2010. There have been significant changes in the policy environment since then especially in Kenya and South Africa. In this paper, we argue that despite these improvements, the pace of change has been slow and uneven and that processes that enable DHMs from diverse contexts to develop their own interventions will lead to more sustainable and enhanced quality of care. We, therefore, assert that our analysis based on this data is still relevant and useful.
It is reasonable to ask how this set of inter-related activities differs from the imposed outsider top-down health systems interventions that we criticise in the introduction of this paper. While none of us was district managers at the time this research was conducted, we are all African residents working in Africa in African health systems. We do not see our proposal as an intervention with a set of actions that need to be followed by DHMs. Rather we are proposing a process that could incentivise district managers to use and analyse their own data. We believe that by using their own data they will generate various, varied and appropriate interventions and that, by definition, these interventions would be generated from the bottom-up. Because such interventions would be based on local data generated by people working in districts, they would be context-specific and more sustainable. This is fundamentally different from programmes imposed by national or international players commented on here.
Conclusions
Investments that incentivise DHMs to use and analyse their own data to present at regional meetings, where they would actively participate in an adult learning environment, will facilitate bottom-up decision-making and allow context-specific interventions to emerge from African DHMs. Donors and national governments indicate that they want to build sustainable, good quality health systems in Africa, especially if these interventions are evidence-based and will lead to stewardship at all levels in the health system. They should be encouraged to fund processes that enable DHMs to decide for themselves and to learn from each other. The activities proposed here could potentially facilitate such district-lead country-level achievements. This should be tested and monitored for impact to promote universal access to quality care within diverse environments and structures.
Acknowledgments
The authors gratefully acknowledge the district health managers who participated in this study. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors thank the African Population Health Research Centre, Nairobi, Kenya for managing this grant.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Aberese-Ako, M., Agyepong, I., & van Dijk, H. (2018). Leadership styles in two Ghanaian hospitals in a challenging environment. Health Policy and Planning, 33(suppl_2), ii16–ii26. https://doi.org/10.1093/heapol/czy038
- Agyepong, I. A., Lehmann, U., Rutembemberwa, E., Babich, S. M., Frimpong, E., Kwamie, A., Olivier, J., Teddy, G., Hwabamungu, B., & Gilson, L. (2018). Strategic leadership capacity building for Sub-Saharan African health systems and public health governance: A multi-country assessment of essential competencies and optimal design for a Pan African DrPH. Health Policy and Planning, 33(suppl_2), ii35–ii49. https://doi.org/10.1093/heapol/czx162
- Agyepong, I. A., Sewankambo, N., Binagwaho, A., Coll-Seck, A. M., Corrah, T., Ezeh, A., Fekadu, A., Kilonzo, N., Lamptey, P., Masiye, F., Mayosi, B., Mboup, S., Muyembe, J., Pate, M., Sidibe, M., Simons, B., Tlou, S., Gheorghe, A., Legido-Quigley, H., … Piot, P. (2017). The path to longer and healthier lives for all Africans by 2030: The Lancet Commission on the future of health in sub-Saharan Africa. The Lancet, 390(10114), 2803–2859. https://doi.org/10.1016/S0140-6736(17)31509-X
- Binagwaho, A., & Ghebreyesus, T. (2019). Primary healthcare is cornerstone of universal health coverage. BMJ, 365, l2391. https://doi.org/10.1136/bmj.l2391
- Birken, S. A., Lee, S. Y. D., & Weiner, B. J. (2012). Uncovering middle managers’ role in healthcare innovation implementation. Implementation Science, 7(1), 1–12. https://doi.org/10.1186/1748-5908-7-28
- Black, D. (1976). Partial justification of the Borda count. Public Choice, 28(1), 1–15. https://doi.org/10.1007/BF01718454
- Blecher, M. S., Davén, J., Harrison, S., Fanoe, W., Ngwaru, T., Matsebula, T., & Khanna N. (2019). National Health Insurance: vision, challenges, and potential solutions. In: T. Moeti, A. Padarat (eds). South African health review. Health Systems Trust. https://journals.co.za/doi/pdf/10. 10520/EJC-1d2aa54be5
- Bonenberger, M., Aikins, M., Akweongo, P., Bosch-Capblanch, X., & Wyss, K. (2015). What do district health managers in Ghana use their working time for? A case study of three districts. PLoS One, 10(6), 1–15. https://doi.org/10.1371/journal.pone.0130633
- Bossert, T., & Beauvais, J. (2002). Decentralization of health systems in Ghana, Zambia, Uganda and the Philippines: A comparative analysis of decision space. Health Policy and Planning, 17(1), 14–31. https://doi.org/10.1093/heapol/17.1.14
- Bradley, E. H., Taylor, L. A., & Cuellar, C. J. (2015). Management matters: A leverage point for health systems strengthening in global health. International Journal of Health Policy and Management, 4(7), 411–415. https://doi.org/10.15171/ijhpm.2015.101
- Daire, J., & Gilson, L. (2014). Does identity shape leadership and management practice? Experiences of PHC facility managers in Cape Town, South Africa. Health Policy and Planning, 29(suppl 2), ii82–ii97. https://doi.org/10.1093/heapol/czu075
- Dwicaksono, A., & Fox, A. (2018). Does decentralization improve health system performance and outcomes in low-and middle-income countries? A systematic review of evidence from quantitative studies. The Milbank Quarterly, 96(2), 323–368. https://doi.org/10.1111/1468-0009.12327
- Edwards, L. J., Moisés, A., Nzaramba, M., Cassimo, A., Silva, L., Mauricio, J., Wester, C. W., Vermund, S. H., & Moon, T. D. (2015). Implementation of a health management mentoring program: Year-1 evaluation of its impact on health system strengthening in Zambézia province, Mozambique. International Journal of Health Policy and Management, 4(6), 353–361. https://doi.org/10.15171/ijhpm.2015.58
- Egger, D., & Ollier, E. (2006). Making health systems work, working paper no 8. Managing the health Millennium Development Goals - The challenge of management strengthening: Lessons from three countries. Geneva. http://www.who.int/management/countrycasestudies.pdf.
- Fetene, N., Canavan, M. E., Megentta, A., Linnander, E., Tan, A. X., Nadew, K., & Bradley, E. H. (2019). District-level health management and health system performance. PLoS One, 14(2), 1–9. https://doi.org/10.1371/journal.pone.0210624
- Filerman, G. (2003). Closing the management competence gap. Human Resources for Health, 1(1), 7. https://doi.org/10.1186/1478-4491-1-7
- Fonn, S., Ray, S., & Blaauw, D. (2011). Innovation to improve health care provision and health systems in sub-Saharan Africa, promoting agency in mid-level workers and district managers. Global Public Health, 6(6), 657–668. https://doi.org/10.1080/17441692.2010.489905
- Fusheini, A., & Eyles, J. (2016). Achieving universal health coverage in South Africa through a district health system approach: Conflicting ideologies of health care provision. BMC Health Services Research, 16(1), 1–11. https://doi.org/10.1186/s12913-016-1797-4
- Heerdegen, A. C. S., Gerold, J., Amon, S., Agyemang, S. A., Aikins, M., & Wyss, K. (2020). How does district health management emerge within a complex health system? Insights for capacity strengthening in Ghana. Frontiers in Public Health, 8(July), 1–11. https://doi.org/10.3389/fpubh.2020.00270
- Henriksson, D., Ayebare, F., Waiswa, P., Peterson, S. S., Tumushabe, E. K., & Fredriksson, M. (2017). Enablers and barriers to evidence based planning in the district health system in Uganda; perceptions of district health managers. BMC Health Services Research, 17(1), 1–11. https://doi.org/10.1186/s12913-017-2059-9
- Henriksson, D. K., Peterson, S. S., Waiswa, P., & Fredriksson, M. (2019). Decision-making in district health planning in Uganda: Does use of district-specific evidence matter? Health Research Policy and Systems, 17(1), 1–11. https://doi.org/10.1186/s12961-019-0458-6
- Kawonga, M., Blaauw, D., & Fonn, S. (2012). Aligning vertical interventions to health systems: A case study of the HIV monitoring and evaluation system in South Africa. Health Research Policy and Systems, 10(1), 1–13. https://doi.org/10.1186/1478-4505-10-2
- Kawonga, M., Blaauw, D., & Fonn, S. (2016). The influence of health system organizational structure and culture on integration of health services: The example of HIV service monitoring in South Africa. Health Policy and Planning, 31(9), 1270–1280. https://doi.org/10.1093/heapol/czw061
- Kawonga, M., Fonn, S., & Blaauw, D. (2013). Adminstrative integration of vertical HIV monitoring and evaluation into health systems: A case study from South Africa. Global Health Action, 6(19252), 157–168. https://doi: 10.3402/gha.v6i0.19252
- Kigume, R., & Maluka, S. (2019). Decentralisation and health services delivery in 4 districts in Tanzania: How and why does the use of decision space vary across districts? International Journal of Health Policy and Management, 8(2), 90–100. https://doi.org/10.15171/ijhpm.2018.97
- Kwamie, A., Dijk, H. v., & Agyepong, I. A. (2014). Advancing the application of systems thinking in health: Realist evaluation of the leadership development programme for district manager decision-making in Ghana. Health Research Policy and Systems, 12(1), 1–12. https://doi.org/10.1186/1478-4505-12-29
- Loh, E. (2015). How and why medically-trained managers undertake postgraduate management training. Journal of Health Organization and Management, 29(4), 438–454. https://doi.org/10.1108/JHOM-10-2013-0233
- Maluka, S. O. (2013). Why are pro-poor exemption policies in Tanzania better implemented in some districts than in others? International Journal for Equity in Health, 12(1), 1–9. https://doi.org/10.1186/1475-9276-12-80
- Mccollum, R., Limato, R., Otiso, L., Theobald, S., & Taegtmeyer, M. (2018). Health system governance following devolution : Comparing experiences of decentralisation in Kenya and Indonesia. BMJ Global Health, 3(e000939), 1–11. https://doi.org/10.1136/bmjgh-2018-000939
- Muchekeza, M., Chimusoro, A., Gombe, N. T., Tshimanga, M., & Shambira, G. (2012). District health executives in Midlands province, Zimbabwe: Are they performing as expected? BMC Health Services Research, 12(1), https://doi.org/10.1186/1472-6963-12-335
- Mutale, W., Vardoy-Mutale, A., Kachemba, A., Mukendi, R., Clarke, K., & Mulenga, D. (2017). Leadership and management training as a catalyst to health system strengthening in low-income settings: Evidence from implementation of the Zambia Management and Leadership course for district health managers in Zambia. PLoS One, 12(7), e0174536. https://doi.org/10.1371/journal.pone.0174536
- Muthathi, I. S., & Rispel, L. C. (2020). Policy context, coherence and disjuncture in the implementation of the ideal clinic realisation and maintenance programme in the Gauteng and Mpumalanga provinces of South Africa. Health Research Policy and Systems, 18(1), 1–15. https://doi.org/10.1186/s12961-020-00567-z
- Ndavi, P. M., Ogola, S., Kizito, P. M., & Johnson, K. (2009). Decentralizing Kenya’s health management system: An evaluation. Kenya Working Papers No.1.
- Nzinga, J., Mbaabu, L., & English, M. (2013). Service delivery in Kenyan district hospitals – What can we learn from literature on mid-level managers? Human Resources for Health, 11(1), 1. https://doi.org/10.1186/1478-4491-11-10
- South African National Department of Health. (2017). White paper on national health insurance. Pretoria. http://www.health.gov.za/index.php/nhi?download=2257:white-paper-nhi-2017.
- Tetui, M., Hurtig, A. K., Ekirpa-Kiracho, E., Kiwanuka, S. N., & Coe, A. B. (2016). Building a competent health manager at district level: A grounded theory study from Eastern Uganda. BMC Health Services Research, 16(1), 1–13. https://doi.org/10.1186/s12913-016-1918-0
- Tetui, M., Zulu, J. M., Hurtig, A. K., Ekirapa-Kiracho, E., Kiwanuka, S. N., & Coe, A. B. (2018). Elements for harnessing participatory action research to strengthen health managers’ capacity: A critical interpretative synthesis. Health Research Policy and Systems, 16(1), 1–14. https://doi.org/10.1186/s12961-018-0306-0
- WHO. (2007). Building leadership and management capacity in health. www.who.int/management/FrameworkBrochure.pdf.
- Wickremasinghe, D., Hashmi, I. E., Schellenberg, J., & Avan, B. I. (2016). District decision-making for health in low-income settings: A systematic literature review. Health Policy and Planning, 31(suppl 2), ii12–ii24. https://doi.org/10.1093/heapol/czv124