ABSTRACT
Global health researchers often discount mutual learning and benefit to address shared health challenges across high and low- and middle-income settings. Drawing from a 30-year partnership called AMPATH that started between Indiana University in the US and Moi University in Kenya, we describe an innovative approach and program for mutual learning and benefit coined ‘reciprocal innovation.’ Reciprocal innovation harnesses a bidirectional, co-constituted, and iterative exchange of ideas, resources, and innovations to address shared health challenges across diverse global settings. The success of AMPATH in Kenya, particularly in HIV/AIDS and community health, resulted in several innovations being ‘brought back’ to the US. To promote the bidirectional flow of learning and innovations, the Indiana CTSI reciprocal innovation program hosts annual meetings of multinational researchers and practitioners to identify shared health challenges, supports pilot grants for projects with reciprocal exchange and benefit, and produces educational and training materials for investigators. The transformative power of global health to address systemic health inequities embraces equitable and reciprocal partnerships with mutual benefit across countries and communities of academics, practitioners, and policymakers. Leveraging a long-standing partnership, the Indiana CTSI has built a reciprocal innovation program with promise to redefine global health for shared wellbeing at a global scale.
Introduction
It is often assumed that global health partnerships primarily involve a unidirectional flow of expertise, innovation, and technology from high-income countries (HICs) to low- and middle-income countries (LMICs) (Packard, Citation2016). The assumption that wealthier countries have less to gain or that they have a claim on innovation, expertise, and technology when engaging in international partnerships discounts the potential for reciprocity and mutual benefit to both HICs and LMICs engaging in global health partnerships (Syed et al., Citation2013). Renewed attention to global health’s neocolonial tendencies and systemic inequities provides opportunities to critically examine practices and partnerships and for new paradigms to emerge that nurture bidirectional flows of knowledge and experience to promote global health equity (Horton, Citation2013; Kim et al., Citation2017).
Recent efforts to shift the paradigm in global health have sometimes employed the concept of ‘reverse innovation,’ originally developed in the field of business (Immelt et al., Citation2009), to highlight the potential benefits of health-related expertise, innovation, and technology flowing from lower to higher income settings (Syed et al., Citation2013; Syed et al., Citation2012). Over the past decade, numerous examples of reverse innovations in healthcare delivery have appeared in the literature, including technological innovations like mobile-based care platforms and methodological innovations in care delivery strategies (Harris et al., Citation2020). Examples of such activities include a community engagement strategy for patient safety in Baltimore, USA that was originally developed by the WHO’s African Partnerships for Patient Safety in sub-Saharan Africa (Ibe et al., Citation2018). In North Wales, UK, a primary care model and community health workforce was adapted from Brazil’s national primary care strategy (Johnson et al., Citation2013), while an organization in New York City, USA drew its inspiration for peer coaches and community health workers from Kenya (Singh, Citation2012). Finally, a model developed for primary prevention of cardiovascular disease in Nairobi, Kenya was adapted for immigrant communities in the Netherlands (van de Vijver et al., Citation2015).
Many health innovations and technologies developed in LMICs are applicable in HICs. Underserved populations in LMICs and HICs often face similar barriers to care due to being uninsured or underinsured, distance and transportation challenges to accessing healthcare particularly in rural areas, and health-related stigma. As such, interventions developed in LMICs to address these challenges could be effective, and cost-effective, in HICs. Care providers, practitioners, and policymakers in LMICs may utilize novel processes and interventions, particularly amidst resource and other constraints, to experiment and implement at scale (Syed et al., Citation2013), leading to many examples of ‘doing more with less’ (Ahmed et al., Citation2017). There are also challenges to reverse innovation in global health, including misperceptions about the quality and adaptability of innovations and technologies developed in LMICs, identifying good candidates for adaptation, and regulatory hurdles for adapting and implementing them in HICs, among other challenges (Bhattacharyya et al., Citation2017; Harris et al., Citation2017).
The reality that discoveries in LMICs are often discounted by implementers and policymakers in HICs clearly illustrates the need for a paradigm shift to harness the benefits of reverse innovation across settings. In addition, while the potential benefits to HICs from the flow of expertise, innovation, and technology from LMICs are clear (Syed et al., Citation2012), models of reverse innovation in global health may not fully capture the potential for mutual benefit and mutual learning that emerge from sustained, bidirectional partnerships across HICs and LMICs to address global and local health inequities (Crisp, Citation2014; Depasse & Lee, Citation2013; Harris et al., Citation2016). Building more equitable and reciprocal partnerships is essential to the future of global health (Koplan et al., Citation2009; Pai, Citation2020) and can work to address systemic and unequal power relations that disproportionately benefit both individual researchers and institutions in HICs. Researchers benefit through funding, research agendas, opportunities for training and career trajectory, and authorship on publications, while institutions stand to gain institutional infrastructure and capacity, reputational benefits that can lead to increased financial support, and access to more diverse study populations (Citrin et al., Citation2017; Crane, Citation2010; Crane et al., Citation2018; Gautier et al., Citation2018; Smith et al., Citation2014). At the broader level, societal benefits can also be gained through better health interventions, technologies, and methodologies that may improve population health.
Building on the concept of reverse innovation and drawing from a 30-year global health partnership between Indiana University in the US and Moi University in Eldoret, Kenya, in this paper we propose a new concept, ‘reciprocal innovation,’ that more explicitly harnesses a bidirectional, co-constitutive, and iterative exchange of resources, knowledge, and innovations among global health partners. We argue that reciprocal innovation is a transformative power for global health research to address systemic health inequities around the world that rests on equitable and reciprocal partnerships within and across countries and communities of academics, practitioners, and policymakers.
Reciprocal innovation: a new concept for global health partnership
Reciprocal innovation evolves the concept of reverse innovation and is defined by three characteristics: (1) global health partnership rooted in the values of reciprocity, mutual learning, and equity across partner institutions in HICs and LMICs, (2) a bi-directional and co-constituted approach to identifying shared health challenges across settings in long-term engagements, and (3) identification of high-quality innovations from global health partnerships for demonstration, replication, and dissemination in diverse settings, as demonstrated in . Reciprocal Innovation Model.
Figure 1. Reciprocal innovation model. Our ‘reciprocal innovation’ model in global health starts by engaging key US and international partners in a bidirectional process that identifies and prioritizes shared health challenges to be addressed and leads to delivering solutions through co-development of healthcare innovation and exchange of information.
Reciprocal innovation centres the values of reciprocity and equity in bilateral exchanges and partnerships in global health, which are increasing and increasingly being critically examined and documented (Harris et al., Citation2016). Relationships in global health that are truly reciprocal are more likely to lead to stronger and longer partnerships, better science, and developing, evaluating, and implementing effective health innovations in HIC and LMIC settings. Additionally, mutual learning allows for reciprocal innovation to evolve and expand more robustly with progressive improvements that have a considerable impact on both populations. This iterative process allows for flexibility to adapt innovations within the settings where they are implemented. Francis Collins, director of the US National Institutes of Health, affirmed the importance of reciprocal innovation in 2009 when he stated that, ‘Global health research should be a conversation with other countries not one in which the great United States tells the world what the answers are without listening to and learning from their experiences’ (Collins says global health is one of his top priorities, Citation2009).
Reciprocal innovation: lessons from the AMPATH partnership
The term reciprocal innovation was coined by the Indiana University (IU) Center for Global Health in 2018 and adopted by the Indiana Clinical and Translational Sciences Institute (CTSI) to capitalize on the collective experiences and strengths in global health research and to, in part, use them to inform the sharing and building of global collective knowledge, data, and innovations in research across Indiana and around the world. Significant inspiration for the concept was derived from IU's long-term partnership with Moi University, which today has grown into the Academic Model Providing Access to Healthcare (AMPATH). AMPATH is a unique and highly successful global health partnership representing over 30 years of collaboration between Moi University and Moi Teaching and Referral Hospital in Kenya and a consortium of North American academic institutions led by IU (Einterz et al., Citation2007). AMPATH was founded on the principles of equity, mutual benefit, and long-term commitment, with partners working across a tripartite mission of care, education, and research. In partnership with the Kenyan Government, AMPATH serves a population of 8 million people across western Kenya at more than 500 clinical sites, with comprehensive care programs in HIV/AIDS, oncology, chronic diseases, and maternal child health, among others, and pioneering population health and community-based approaches to care (Mercer et al., Citation2018). The partnership facilitates bilateral exchanges for Kenyan and North American faculty, residents, and students, and leverages academic partnerships to build critical clinical and research infrastructure in Kenya, train global health researchers, and conduct research to improve the health of under-served populations in Kenya and globally (Goodrich et al., Citation2021; Tierney et al., Citation2013; Turissini et al., Citation2020).
Two cases of ‘reciprocal innovation in action’
One example of ‘reciprocal innovation in action’ that was prompted by AMPATH’s efforts in building HIV/AIDS care systems in western Kenya was the response to an HIV outbreak that began among people using injection drugs in Scott County, Indiana in 2014. By 2016, 188 cases of HIV were diagnosed, resulting in a prevalence of 5% in Scott County, comparable to or exceeding prevalence estimates in many parts of Kenya. Other parallels between the HIV epidemic in Scott County and in western Kenya included that the impacted populations were predominately rural and socio-economically marginalized and that in both places HIV was a highly stigmatized disease. Mirroring the approaches taken from AMPATH, the Division of Infectious Diseases at Indiana University School of Medicine working under the auspices of the Indiana Department of Public Health and its partners established a comprehensive ‘one-stop shop’ HIV clinic fully integrated with other health and social services. The result was the rapid scale-up of HIV services that incorporated standardized HIV treatment algorithms and standardized visit documentation, which supported the provision of quality HIV care by physicians and mid-level providers not previously experienced in HIV care. As a result, by the end of 2015, among the 176 individuals known to be eligible for HIV treatment, 86% had been engaged in care (Janowicz, Citation2016).
A second case of ‘reciprocal innovation in action’ informed by AMPATH is the WeCare program in Indiana. In both Kenya and Indiana, maternal and infant mortality are significant public health concerns, with facility-based care models being inadequate to address maternal child healthcare needs, particularly for marginalized and uninsured populations. In Kenya, as well as in many global settings, community health workers (CHW) are central for delivering critical primary care services, education, referrals, and other social services. At AMPATH, several innovative models of CHW-delivered services were developed that have improved HIV/AIDS and maternal child healthcare and outcomes, including CHW-led, group-based care models that deliver healthcare as well as address the social determinants of health. Several of these innovations were taken back to Indiana and adapted to address high rates of infant mortality, significantly higher than the national average, through the WeCare program in Indiana (Litzelman et al. Citationin press; WeCare Indiana: Improving Maternal and Infant Health to Reduce Infant Mortality, n.a.). This program hires and trains CHW ‘coaches’ from the community to connect pregnant women and new mothers to health and social services and educates mothers on things like safe sleep practices and breastfeeding in the most underserved areas in Indianapolis. Underlying both the models of CHW-based care to improve maternal and child health at AMPATH in Kenya and WeCare in Indiana is recognizing and addressing the social determinants of health, including education, transportation, and poverty, among others, alongside healthcare needs.
Materials and methods
The remainder of this paper is a descriptive case study of establishing a reciprocal innovation global health program at the Indiana CTSI. We reflect on lessons learned and next steps for adopting a reciprocal innovation approach in global health to improve the health of underserved populations in Indiana, Kenya, and around the world.
Building a reciprocal innovation program at the Indiana CTSI
The Indiana CTSI Global Health Program was established in 2016 to address domestic and global health issues for underserved populations by bringing together research and expertise from three vibrant global health centres: IU Center for Global Health, University of Notre Dame Eck Institute for Global Health, and the Purdue University Institute of Inflammation, Immunology and Infectious Diseases. The Global Health Program is led by seven faculty at the three Indiana CTSI institutions, with expertise in infectious disease, infant and maternal health, non-communicable diseases, population health, community engagement, biology and chemistry. The program is supported by a full-time program manager to support program activities, including managing stakeholder meetings, overseeing the grants program, and creating educational resources for reciprocal innovation, which are described in more detail below. From 2016 to 2021, 30 grants totalling $610,000 have been awarded to investigators and their partners in the areas of infant and maternal health, infectious disease, access to healthcare, and chronic diseases. The CTSI Global Health Program also serves as a hub for investigators at Indiana CTSI and partner institutions in LMICs to access resources for reciprocal innovation, including informational videos and ‘how-to’ guides, and to network and collaborate at annual meetings
In 2018, the program underwent a transition to focus explicitly on reciprocal innovation. To support the transition from a more traditional global health program focused on health in LMIC to a reciprocal innovation program, we conducted an environmental scan to assess the available infrastructure and interest among partners and stakeholders in reciprocal innovation. Information gained from the environmental scan was used to organize an initial ‘stakeholder meeting’ that brought together Indiana CTSI institutions, researchers at partner institutions in LMICs, and members of local public health and community organizations. At this meeting, stakeholders identified and discussed health priorities in Indiana and in partner LMIC settings and potential areas for reciprocal innovation research and partnership. Using information from the environmental scan and the stakeholder meeting, a reciprocal innovation grants program and call for applications were created targeting areas for reciprocal innovation identified in the environmental scan and stakeholder meeting.
This unique approach, namely the environmental scan, stakeholder meetings, and grants program, to building and supporting reciprocal innovation is shown in . Reciprocal Innovation Process. The process continuously and explicitly engages local and global partners to identify shared health challenges and fosters research collaborations and partnerships to identify, test, and adapt shared solutions. Each of these steps in our approach is discussed in more detail below.
Figure 2. The Indiana CTSI process for identifying priority areas of opportunities for reciprocal innovation. In the first step of the process, stakeholders are identified through an ‘environmental scan’ that includes both ‘local’ and ‘global’ partners. This is followed by a Stakeholders Meeting whereby shared health priority areas are identified. This allows for the convergence of local and global partner priorities that are then used to inform a competitive reciprocal innovation grants program funded by the Indiana CTSI.
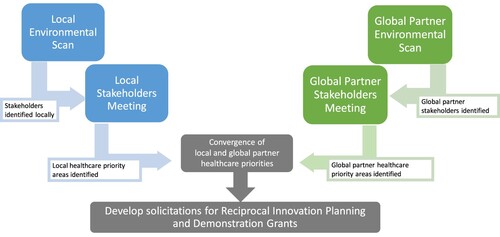
Environmental scan
The environmental scan was an essential ‘first step’ in building a reciprocal innovation grants program. The goal of the environmental scan was to engage stakeholders both in Indiana and internationally to: (1) gauge interest and understanding of the concept of reciprocal innovation, (2) catalogue the available infrastructure for reciprocal innovation, including existing partnership, (3) identify the critical challenges to moving forward the reciprocal innovation concept/process, and (4) begin to identify key health priorities both in Indiana and in our partner countries that might be amenable to addressing through a reciprocal innovation approach. The environmental scan also provided a roadmap to identify stakeholders and topics for the stakeholder meeting where global and local partners reviewed the challenges, priorities, and opportunities identified in environmental scans with the goal of developing priority investment areas for the Indiana CTSI’s Reciprocal Innovation and Grant Programs. The environmental scan was first done to gain perspective from both local and international partners so that implementers in each setting could identify and articulate their own challenges, priorities, and opportunities, and then come together to see where they overlap, and focus research efforts there.
An environmental scan of critical areas of need with key health stakeholders in Indiana and at the Indiana CTSI member institution’s key international partner sites was conducted over a six-month period with a special emphasis on the AMPATH partnership in Kenya. The first phase of the scan included interviews with 75 key stakeholders from IU, Purdue, Notre Dame, Indiana state government, local health practitioners, community groups, and long-standing LMIC partners. Semi-structured, in-person interviews were conducted to introduce the concept of reciprocal innovation, assess interest in reciprocal innovation, identify additional key stakeholders and start exploring critical health challenges, stakeholder priorities, and resources and opportunities. Interviewers provided written summaries of each interview to identify key themes. In follow-up to the preliminary stakeholder interviews, 121 Indiana-based and LMIC stakeholders were identified and invited to complete an online questionnaire to provide further input on how the reciprocal innovation program could best serve populations in Indiana and around the globe. Responses from Indiana stakeholders and LMIC stakeholders were tallied individually in order to analyse priorities, challenges, and barriers by country and compared with each other to identify commonalities. Overall, we found that the majority of stakeholders expressed support for the concept of reciprocal innovation and that they could identify several opportunities or candidates for a reciprocal innovation process to address health challenges in Indiana and in Kenya. Among identified barriers to reciprocal innovation the three most cited were 1) lack of funding, 2) challenges in gaining community acceptance of reciprocal innovation projects, and accessing relevant populations, and 3) the lack of protected time and qualified people to conduct reciprocal innovation.
Stakeholder meetings
Annual reciprocal innovation stakeholder meetings commenced in 2019 to disseminate the concept of reciprocal innovation, engage stakeholders in the reciprocal innovation process, and to identify key priorities and targets for reciprocal innovation. The first meeting in 2019 focused on Indiana stakeholders and priorities while the second meeting in 2020 focused on East Africa led by long standing partners at AMPATH in Kenya. A third meeting was held in 2021 to deepen connections between global and local investigators and provide support for the upcoming round of reciprocal innovation grants. At the first meeting, key stakeholders included researchers from Indiana CTSI institutions, the Indiana State Department of Health, and local organizations and used small groups to identify key health issues in Indiana and brainstorm potential topics for reciprocal innovation. Stakeholders identified the following priority areas for reciprocal innovation: 1) reducing chronic disease, 2) reducing substance abuse, 3) addressing infant and maternal health, and 4) strengthening access to healthcare. The second meeting focused on East African health priorities for reciprocal innovation, and due to the COVID-19 pandemic was held virtually in 2020. Key stakeholders attended from Moi University, Moi Teaching and Referral Hospital, Kenya Ministry of Health, Indiana CTSI institutions, and global health partners in the AMPATH consortium. Reciprocal innovation priorities identified by East African stakeholders were 1) mental health, 2) non-communicable diseases, 3) infectious disease, 4) infant and maternal health, and 5) access to quality healthcare, illustrating significant overlap and shared health challenges with those identified in Indiana. The third meeting in 2021 was a two-day virtual conference. The first day was a reciprocal innovation workshop where globally- and locally-focused investigators were broken into small groups to build relationships, share reciprocal innovation ideas, and get feedback from CTSI Global Health leadership on potential reciprocal innovation grant projects. The second day was a plenary session hosted by Dr. Roger Glass, Director of the Fogarty International Center and Associate Director for International Research at the US National Institutes of Health, followed by a panel discussion on the applications of reciprocal innovation and its role during global crises like COVID-19.
Results
Reciprocal innovation grants program
Based on the findings of the environmental scan and shared health priorities identified at the stakeholder meetings, a competitive reciprocal innovation grants program was established. Eligible applicants were investigators from an Indiana CTSI institution who had to either propose a plan to form or have an existing partnership with at least one investigator in an LMIC. While funding has been initially restricted to investigators at Indiana CTSI institutions, which represents a continued challenge of equity in global health funding opportunities, the requirement to either form a partnership with an international collaborator or to have a named international co-principal investigator as part of the proposal is intended to support the growth of collaborative and more equitable ‘local-global’ collaborative research teams.
The program established two types of grants - a reciprocal innovation planning grant of $10,000 for one year to support partnership development and project planning, and a reciprocal innovation demonstration grant of $50,000 for two years to conduct reciprocal innovation research activities. Planning grants support preliminary partnership development and project planning that will ideally provide the groundwork for reciprocal innovation projects. The CTSI Global Health Program felt that it was critical to support these early efforts to establish partnerships in reciprocal innovation since the concept and aims of the program were so new to many investigators. There are also few funding opportunities that are primarily focused on ‘relationship building’ for researchers, which we consider essential to building mutually beneficial and equitable international research teams. In many cases, these grants have supported travel to identify and build relationships with counterparts (both to Indiana for LMIC investigators and teams and to LMIC settings for Indiana investigators and teams), to identify shared research interests and priorities, and to plan for research grant applications.
Demonstration grants support existing global health research partnerships of the Indiana CTSI partner institutions to pilot implementation and assessment of innovations with a high potential to positively impact outcomes in the identified priority areas. The goal of the demonstration grant is to assist teams in generating pilot data for reciprocal innovation that can then be used to support additional extramural funding. For demonstration grants, the principal investigator in Indiana must have at least one co-principal investigator based at a LMIC institution with the expectation that these investigators are involved at all stages of the research process, from developing the proposal, to carrying out the research, to disseminating findings, and collaborating in future work.
Grant applications are reviewed by a selection committee. Planning grants are first reviewed by a member of the Indiana CTSI team, with expert review solicited as needed, including by international partners when appropriate. The demonstration grant reviews are conducted in a manner similar to an NIH study section review by a formal proposal review committee. The review committee is composed of members representing the Indiana CTSI institutions and international partners. The involvement of our international partners in the review and selection process for these awards continues to be an important aspect in the process of prioritizing innovations in a reciprocal way. The process was initially developed using tele and video-conferencing to engage reviewers. The creation of a robust selection process and team was a key feature of this process that was developed early in the creation of our pilot awards. This provides an important platform for supporting true reciprocity in this process and it is a feature that is not always present in the selection processes used by sponsors. It is worth highlighting this aspect as one of the key components of the reciprocal innovation process the Indiana CTSI established. Eventually, the Indiana CTSI program’s natural evolution as a model for reciprocal innovation will extend opportunities for international partners to lead the process.
One reciprocal innovation project supported by the Indiana CTSI program was adapting a technology to address drug safety in Malawi back to Indiana. In Malawi, weak drug regulatory environments contribute to high rates of adulterated or counterfeit pharmaceuticals, which can be dangerous to patients. Led by investigators at the University of Notre Dame in partnership with Malawian colleagues, a paper test card called the paper analytical device (PAD) was developed to detect adulterated antibiotics rapidly and inexpensively at the point of care. With support from the Indiana CSTI, these same investigators turned their attention to the problem of unregulated street drugs in the US and dangerous ‘cutting agents’ and other substances contributing to overdose deaths. The PAD technology was re-engineered to detect a wide range of dangerous substances often found in street drugs. The technology is being tested by harm reduction groups in Chicago who work with people who use drugs and empower them to identify particularly hazardous constituents (Chikowe et al., Citation2018; Lockwood et al., Citation2021; Lockwood et al., Citation2020).
Educational resources for reciprocal innovation
To increase awareness and support for the concept of reciprocal innovation, the Indiana CTSI Global Health Program created a series of videos and presentations on reciprocal innovation principles, the grants program, and previously funded projects. From our various interactions, we found that while global health investigators have strong connections to international partners in LMICs, they often are not well connected to locally-based researchers in Indiana. To support potential connections between locally- and globally-focused investigators, a Global Health Innovation Exchange was created as an online repository of reciprocal innovation projects. The repository is a living dashboard that is used to share updates on project progress, outcomes, and published materials. In addition to the repository, the annual reciprocal innovation stakeholder meetings provide further opportunities to link locally- and globally-focused researchers and foster the development of these partnerships. The program is also working to create additional educational modules for undergraduate and graduate students interested in public and global health, with a goal of increasing interest in reciprocal innovation, providing potential funding opportunities for graduate research projects, and increasing the pipeline of global health investigators harnessing reciprocal innovation approaches in their work.
Discussion
Lessons learned
Several lessons have emerged in establishing and building a program for reciprocal innovation at the Indiana CTSI. First, given that the concept of reciprocal innovation is new to investigators, there continues to be an important educational component to our program to define the core principles and scope of reciprocal innovation in global health. This has been especially important in our grants program to help ensure that applicants align their approach and activities with reciprocal innovation. To address this challenge, we created educational videos on the concept of reciprocal innovation and specifically outlined the types of projects and approaches supported by the grants program. We also provide mentorship and consultation for investigators on their applications and provide guidance on how to better tailor to a reciprocal innovation approach. While the mentorship and consultation process are time consuming for the program, it provides significant benefit in strengthening reciprocal innovation applications and fosters a new generation of investigators who are fluent in the concept of reciprocal innovation. Still, introducing new approaches and funding mechanisms to support reciprocal innovation has been challenging and time intensive.
Second, as noted above, US investigators in global health have strong partnerships with international collaborators, but often face significant challenges in identifying and partnering with investigators working domestically. Conversely, domestic community-embedded researchers are often unaware of the global health work being done by investigators at their own institution. Partnerships between these core groups of investigators are key components of reciprocal innovation. To support linkages between locally- and globally-focused researchers, we are developing a virtual platform to facilitate and foster collaborations between globally- and locally-focused investigators at Indiana CTSI institutions and international partners. We are in the process of creating a virtual commons that will be a meeting place to learn about reciprocal innovation approaches, present ongoing work in reciprocal innovation, and identify new areas and collaborations for reciprocal innovation. The continuous sharing of lessons learned and collaboration between globally- and locally-focused investigators alongside international partners in LMICs will leverage the power of developing, testing, and disseminating shared health solutions to shared health challenges.
Finally, we believe that our approach to reciprocal innovation provides a foundation from which to better identify and address systemic global health inequities, both at the level of health access and outcomes among populations across and within higher and lower income settings, as well as inequities in global health governance, funding, and research. We do not claim that this approach ‘solves’ any of these problems. However, by prioritizing meaningful and reciprocating relationships among researchers and communities across settings throughout all stages of the research process, it allows for areas of mutual benefit and reciprocity to emerge that can be leveraged to address inequities at various levels. Still, we recognize inequities in our own reciprocal innovation program, including access to grant funding and a review and leadership team that remains US-biased in terms of its construction, which we are working to address.
Plans for the future
The expansion goals for reciprocal innovation stretch both nationally and globally. To further connect global health and local researchers, the team’s long-term goal is to expand the Global Health Innovation Exchange by including investigators and projects from other clinical and translational science institutes, linking to other exchanges, and/or serving as a reference directory for interested global and local investigators. This would leverage the unique strengths of different institutions and increase opportunities for: 1) identifying investigators to partner in reciprocal innovation projects; 2) identifying internal and extramural funding opportunities; and 3) testing proof of concept that reciprocal innovation represents a powerful approach to research that can be successfully replicated at other institutions. Partner institutions and their investigators would have access to and contribute to building a variety of resources through the reciprocal innovation platform developed and piloted at the Indiana CTSI Global Health Program.
The Indiana CTSI has longstanding and strong international partnerships with investigators in Kenya. Although funded reciprocal innovation projects can and have taken place in different countries around the world, a majority of them are rooted in Kenya. To expand globally, we are working to identify and include other global partnerships and institutions in LMICs to engage in reciprocal innovation projects. As first steps, we have invited other global partners to attend annual stakeholder meetings, presented the concept of reciprocal innovation at academic conferences, and engaged leadership at AMPATH Consortium schools that have budding partnerships in Ghana, Mexico, and Nepal. Once these foundations of long-term commitment are built, we will be in a better position to extend beyond the north–south framework to include south-south and multilateral partnerships.
Finally, building support for reciprocal innovation requires recognizing and measuring the mutual benefits that are gained from such an approach in global health. Considering the current global COVID-19 pandemic and the crucial lessons being learned from international partnerships (Bump et al., Citation2021), it is difficult to justify not investing in such programs with the potential for bilateral gains and advances. Investments made are returned several-fold as new innovations and perspectives benefit all parties, as illustrated by our ‘reciprocal innovation in action’ cases. Compiling high quality evidence for mutual benefit and returns on investment on projects often funded by HICs are critical for sustained and increased funding in global health. This is one reason why we believe that research programs in reciprocal innovation have such an important role to play.
Conclusion
Reciprocal innovation represents a new approach to engaging partners in deep and mutually beneficial ways in global health partnerships that are more apt to addressing critical health needs. We recognize that the importance of investing to improve the health and security of our global population is also an opportunity to improve the health and security of our local community. As we grapple with the global COVID-19 pandemic, it continues to be evident that investments in health security on a global scale have direct implications in the health and wellbeing of local populations as well. What we have learned from these experiences is that a more equitable and bi-directional approach to global health partnerships will be essential to build stability through evidence-based interventions, new technological advancements, and novel healthcare delivery approaches. For example, members of the Community Health Impact Coalition advocated early in the COVID-19 pandemic for deploying CHWs to buffer the impact on the poor and vulnerable in LMIC who were being disproportionately affected by the pandemic. The US similarly identified disparities in the impact on vulnerable populations (Ballard et al., Citation2020). Heeding the Coalition’s recommendation to deploy CHW, research in Central Indiana demonstrated the positive impact CHW had on assisting vulnerable older adults stay connected to essential medical and social resources during the pandemic (Hodges et al., Citation2021). Global health equity priorities are also US health priorities and we have developed the Indiana CTSI reciprocal innovation approach and program to improve the efficiency and effectiveness of our global health investments through mutual benefit and a focus on equity.
Declaration of interest statement
The authors report there are no competing interests to declare.
Acknowledgements
The authors wish to acknowledge the founding director of the Indiana CTSI, Dr. Anantha Shekhar, whose support and encouragement helped catalyse the reciprocal innovation program described in this publication.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Ahmed, F., Ahmed, N., Briggs, T. W. R., Pronovost, P. J., Shetty, D. P., Jha, A. K., & Govindarajan, V. (2017). Can reverse innovation catalyse better value health care? The Lancet Global Health, 5(10), e967–e968. https://doi.org/10.1016/S2214-109X(17)30324-8
- Ballard, M., Bancroft, E., Nesbit, J., Johnson, A., Holeman, I., Foth, J., Rogers, D., Yang, J., Nardella, J., Olsen, H., Raghavan, M., Panjabi, R., Alban, R., Malaba, S., Christiansen, M., Rapp, S., Schechter, J., Aylward, P., Rogers, A., … Palazuelos, D. (2020). Prioritising the role of community health workers in the COVID-19 response. BMJ Global Health, 5(6), e002550. https://doi.org/10.1136/bmjgh-2020-002550
- Bhattacharyya, O., Wu, D., Mossman, K., Hayden, L., Gill, P., Cheng, Y. L., Daar, A., Soman, D., Synowiec, C., Taylor, A., Wong, J., von Zedtwitz, M., Zlotkin, S., Mitchell, W., & McGahan, A. (2017). Criteria to assess potential reverse innovations: Opportunities for shared learning between high- and low-income countries. Globalization and Health, 13(1), 4. https://doi.org/10.1186/s12992-016-0225-1
- Bump, J. B., Friberg, P., & Harper, D. R. (2021). International collaboration and COVID-19: What are we doing and where are we going? BMJ, 372, n180. https://doi.org/10.1136/bmj.n180
- Chikowe, I., Bliese, S. L., Lucas, S., & Lieberman, M. (2018). Amoxicillin quality and selling practices in urban pharmacies and drug stores of blantyre, Malawi. The American Journal of Tropical Medicine and Hygiene, 99(1), 233–238. https://doi.org/10.4269/ajtmh.18-0003
- Citrin, D., Mehanni, S., Acharya, B., Wong, L., Nirola, I., Sherchan, R., Gauchan, B., Karki, K. B., Singh, D. R., Shamasunder, S., Le, P., Schwarz, D., Schwarz, R., Dangal, B., Dhungana, S. K., Maru, S., Mahar, R., Thapa, P., Raut, A., … Maru, D. (2017). Power, potential, and pitfalls in global health academic partnerships: Review and reflections on an approach in Nepal. Global Health Action, 10(1), 1367161. https://doi.org/10.1080/16549716.2017.1367161
- Collins says global health is one of his top priorities. (July-August 2009). Washington, D.C. Global Health Matters Volume 8, Issue 4. Fogarty International Center. Available at: https://www.fic.nih.gov/NEWS/GLOBALHEALTHMATTERS/Pages/0809_collins.aspx.
- Crane, J. T. (2010). Unequal ‘partners’. AIDS, academia, and the rise of academic global health. Behamoth: A Journal of Civilisation, 3(3), 78–97. https://doi.org/10.1080/17441692.2017.1372504
- Crane, J. T., Andia Biraro, I., Fouad, T. M., & Boum, Y. (2018). The ‘indirect costs’ of underfunding foreign partners in global health research: A case study. Global Public Health, 13(10), 1422–1429. https://doi.org/10.1080/17441692.2017.1372504
- Crisp, N. (2014). Mutual learning and reverse innovation–where next? Globalization and Health, 10(1), 14. https://doi.org/10.1186/1744-8603-10-14
- Depasse, J. W., & Lee, P. T. (2013). A model for ‘reverse innovation’ in health care. Globalization and Health, 9(1), 40. https://doi.org/10.1186/1744-8603-9-40
- Einterz, R. M., Kimaiyo, S., Mengech, H. N., Khwa-Otsyula, B. O., Esamai, F., Quigley, F., & Mamlin, J. J. (2007). Responding to the HIV pandemic: The power of an academic medical partnership. Academic Medicine, 82(8), 812–818. https://doi.org/10.1097/ACM.0b013e3180cc29f1
- Gautier, L., Sieleunou, I., & Kalolo, A. (2018). Deconstructing the notion of “global health research partnerships” across northern and African contexts. BMC Medical Ethics, 19(Suppl 1), 49. https://doi.org/10.1186/s12910-018-0280-7
- Goodrich, S., Siika, A., Mwangi, A., Nyambura, M., Naanyu, V., Yiannoutsos, C., Spira, T., Bateganya, M., Toroitich-Ruto, C., Otieno-Nyunya, B., & Wools-Kaloustian, K. (2021). Development, assessment, and outcomes of a community-based model of antiretroviral care in western Kenya through a cluster-randomized control trial. JAIDS Journal of Acquired Immune Deficiency Syndromes, 87(2), e198–e206. https://doi.org/10.1097/QAI.0000000000002634
- Harris, M., Dadwal, V., & Syed, S. B. (2020). Review of the reverse innovation series in globalization and health - where are we and what else is needed? Globalization and Health, 16(1), 26. https://doi.org/10.1186/s12992-020-00555-6
- Harris, M., Macinko, J., Jimenez, G., & Mullachery, P. (2017). Measuring the bias against low-income country research: An implicit association test. Globalization and Health, 13(1), 80. https://doi.org/10.1186/s12992-017-0304-y
- Harris, M., Weisberger, E., Silver, D., Dadwal, V., & Macinko, J. (2016). That's not how the learning works - the paradox of reverse innovation: A qualitative study. Globalization and Health, 12(1), 36. https://doi.org/10.1186/s12992-016-0175-7
- Hodges, M., Butler, D. A. S., & Litzelman, D. (2021). The role of community health workers in assisting older adults during the COVID pandemic. Abstract presented at the American Geriatrics Society 2021 Virtual Annual Scientific Meeting, May 13–15, 2021, Virtual.
- Horton, R. (2013). Offline: Is global health neocolonialist? The Lancet, 382(9906), 1690. https://doi.org/10.1016/S0140-6736(13)62379-X
- Ibe, C. A., Basu, L., Gooden, R., Syed, S. B., Dadwal, V., Bone, L. R., Ephraim, P. L., Weston, C. M., Wu, A. W., & Baltimore, C. P. T. (2018). From kisiizi to Baltimore: Cultivating knowledge brokers to support global innovation for community engagement in healthcare. Globalization and Health, 14(1), 19. https://doi.org/10.1186/s12992-018-0339-8
- Immelt, J. R., Govindarajan, V., & Trimble, C. (October 2009). How GE is disrupting itself Harv Bus Rev.
- Janowicz, D. M. (2016). HIV transmission and injection drug use: Lessons from the Indiana outbreak. Topics in Antiviral Medicine, 24(2), 90–92. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6148928/
- Johnson, C. D., Noyes, J., Haines, A., Thomas, K., Stockport, C., Ribas, A. N., & Harris, M. (2013). Learning from the Brazilian community health worker model in North Wales. Globalization and Health, 9(1), 25. https://doi.org/10.1186/1744-8603-9-25
- Kim, J. U., Oleribe, O., Njie, R., & Taylor-Robinson, S. D. (2017). A time for new north–south relationships in global health. International Journal of General Medicine, 10, 401–408. https://doi.org/10.2147/IJGM.S146475
- Koplan, J. P., Bond, T. C., Merson, M. H., Reddy, K. S., Rodriguez, M. H., Sewankambo, N. K., & Wasserheit, J. N. & Consortium of Universities for Global Health Executive, B (2009). Towards a common definition of global health. The Lancet, 373(9679), 1993–1995. https://doi.org/10.1016/S0140-6736(09)60332-9
- Litzelman, D., Umoren, R. A., Inui, T. S., Griffin, W., Perkins, S. M., Moser, E. A. S., Wiehe, S. E., Roth, S., DeChant, P., & Swigonski, N. L. (In Press). Evaluation of a program to reduce infant mortality risk factors in central indiana. Journal of Health Care for the Poor and Underserved.
- Lockwood, T. E., Huynh, P., Richard, A., Sightes, E., Bailey, K., Ray, B., & Lieberman, M. (2021). Community overdose surveillance: Comparing substances collected from the death scene investigation to toxicology results. Drug and Alcohol Dependence, 224, 108722. https://doi.org/10.1016/j.drugalcdep.2021.108722
- Lockwood, T. E., Leong, T. X., Bliese, S. L., Helmke, A., Richard, A., Merga, G., Rorabeck, J., & Lieberman, M. (2020). Idpad: Paper analytical device for presumptive identification of illicit drugs. Journal of Forensic Sciences, 65(4), 1289–1297. https://doi.org/10.1111/1556-4029.14318
- Mercer, T., Gardner, A., Andama, B., Chesoli, C., Christoffersen-Deb, A., Dick, J., Einterz, R., Gray, N., Kimaiyo, S., Kamano, J., Maritim, B., Morehead, K., Pastakia, S., Ruhl, L., Songok, J., & Laktabai, J. (2018). Leveraging the power of partnerships: Spreading the vision for a population health care delivery model in western Kenya. Globalization and Health, 14(1), 44. https://doi.org/10.1186/s12992-018-0366-5
- Packard, R. M. (2016). A history of global health: Interventions into the lives of other peoples. Johns Hopkins University Press.
- Pai, M. (2020). Reciprocity in global health: here is how we can do better. Forbes Magazine.
- Singh, P. (2012). Bringing the concepts of peer coaches and local health workers from Africa to harlem. Health Affairs, 31(12), 2801–2802. https://doi.org/10.1377/hlthaff.2012.1109
- Smith, E., Hunt, M., & Master, Z. (2014). Authorship ethics in global health research partnerships between researchers from low or middle income countries and high income countries. BMC Medical Ethics, 15(1), 42. https://doi.org/10.1186/1472-6939-15-42
- Syed, S. B., Dadwal, V., & Martin, G. (2013). Reverse innovation in global health systems: Towards global innovation flow. Globalization and Health, 9(1), 36. https://doi.org/10.1186/1744-8603-9-36
- Syed, S. B., Dadwal, V., Rutter, P., Storr, J., Hightower, J. D., Gooden, R., Carlet, J., Bagheri Nejad, S., Kelley, E. T., Donaldson, L., & Pittet, D. (2012). Developed-developing country partnerships: Benefits to developed countries? Globalization and Health, 8(1), 17. https://doi.org/10.1186/1744-8603-8-17
- Tierney, W. M., Nyandiko, W. N., Siika, A. M., Wools-Kaloustian, K., Sidle, J. E., Kiplagat, J., Bell, A., & Inui, T. S. (2013). These are good problems to have … ”: establishing a collaborative research partnership in east Africa. Journal of General Internal Medicine, 28(3), 625–638. https://doi.org/10.1007/s11606-013-2459-4
- Turissini, M., Mercer, T., Baenziger, J., Atwoli, L., Einterz, R., Gardner, A., Litzelman, D., & Ayuo, P. (2020). Developing ethical and sustainable global health educational exchanges for clinical trainees: Implementation and lessons learned from the 30-year academic Model Providing access to healthcare (AMPATH) partnership. Annals of Global Health, 86(1), 137. https://doi.org/10.5334/aogh.2782
- van de Vijver, S., Oti, S., Moll van Charante, E., Allender, S., Foster, C., Lange, J., Oldenburg, B., Kyobutungi, C., & Agyemang, C. (2015). Cardiovascular prevention model from Kenyan slums to migrants in the Netherlands. Globalization and Health, 11(1), 11. https://doi.org/10.1186/s12992-015-0095-y
- WeCare Indiana: Improving maternal and infant health to reduce infant mortality. Regenstrief Institute, Indianapolis, USA. Available online at: https://www.regenstrief.org/projects/wecare-indiana/.
