ABSTRACT
This article unites different disciplinary debates on ‘southern innovation’, ‘theory from the South’, and ‘decolonisation of knowledge’ in order to discuss existing understandings around the role of Africa in the production of health-related knowledge, public health policy, and medical innovation. Arguing that high-income countries have much to learn from the global South when it comes to health-related knowledge and practices, we propose an interdisciplinary research approach to uncovering and examining African contributions to global health, drawing on an ongoing collaborative project funded by the Swiss National Science Foundation. We present four empirical case studies concerning drug development, healthcare systems, and urban planning to critically enquire into both historical and contemporary transcontinental knowledge circulation and learning potentials, as much as cases of forgetting and silencing. On this basis, we argue that ‘learning from the South’ must mean more than transplanting quick and cheap technological fixes to serve societies in the global North, but rather recognising the vast contributions that Africans have made to global epistemologies, without losing sight of the asymmetries inherent in South–North knowledge exchanges. Lessons learned might apply to fields other than those discussed here and go far beyond ‘reverse innovation’.
Introduction
In August 2020, Foreign Policy magazine published its ‘COVID-19 Global Response Index’. Upon its release, the index, which ranks countries’ responses to the unfolding coronavirus disease 2019 (COVID-19) pandemic, saw Senegal as the second top-listed country. Senegal was lauded for swift official action, which included the mobilisation of experiences and infrastructures built up in the course of dealing with previous epidemics, as well as the rapid roll-out of free nation-wide testing and the development of innovative diagnostics. In particular, the government was recognised for its effective and transparent public communication on infection rates and containment strategies (De Sam Lazaro, Citation2020; Foreign Policy, Citation2021).Footnote1 In fact, as Tilley (Citation2020) has argued for the period between January and November 2020, ‘African nations, peoples, and pan-African organisations did better with COVID-19 than any other regions of the world,’ but these success stories have not resonated widely.Footnote2 The COVID-19 pandemic's unexpected, at least partial inversion of established correlations between national wealth and global prestige on the one hand, and disease burden and effective public health responses on the other, has raised questions about the locus of health-related knowledge and innovation, and – in a somewhat more critical vein – the willingness of ‘advanced’ and ‘industrialised’ nations to learn from so-called less developed countries in this regard (Lancet, Citation2020; Samarajiva, Citation2020; WHO, Citation2020).
Our piece contributes to such reconsiderations around the directionality of health-related knowledge transfer. We argue that the global North has much to learn from the global SouthFootnote3 – and African countries in particular – regarding health-related knowledge, surveillance, and public health responses, as well as medical innovations – a point which remains at best coloured and at worst obscured by prejudices, asymmetries, and disciplinary blind spots. However, ‘learning from Africa’, we argue, does not mean naively celebrating ‘reverse’ or ‘frugal innovations’ – concepts which themselves reify understandings of Africa as defined by scarcity. Rather, African contributions to global health need to be approached with an eye to empirical cases, investigated historically, and examined from an interdisciplinary perspective. This article introduces a constellation of ongoing interdisciplinary research projects reflecting this approach.
Africa and the production of health-related knowledge and innovation
Existing scholarly and policy discourse on innovation has been based on the (tacit) understanding that developments – including health-related knowledge, public health policy, and medical innovation – typically occur in the global North, while countries in the global South are passive and needy recipients. Such actual and perceived asymmetries have come under increasing scrutiny, especially in the social sciences. Under the umbrella term ‘theory from the South’, scholars have highlighted the role of the global South as a site of knowledge production and innovation. Comaroff and Comaroff (Citation2012) have proposed that ‘Euro-America is evolving toward Africa’, pointing out that African experiences with poverty, corruption, and ethnic conflict make the continent a ‘source of theory and explanation for world historical events’ (p. 113). On a more optimistic and empowering note, scholars such as Mavhunga (Citation2017), Osseo-Asare (Citation2014), and Connell (Citation2007), among others, have researched the South's contributions to globally circulating bodies of knowledge, including medicine, philosophy, sociology, and technology. Such contributions have often gone unacknowledged or even been actively silenced, as Ndlovu-Gatsheni (Citation2018), among others, has insisted, pointing to the need for ‘epistemological decolonisation’ (p. 3). In many regards, Southern theorists re-engage with prominent thinkers of the era of decolonisation, such as Léopold Sédar Senghor, Kwame Nkrumah, and Julius Nyerere, who argued that not only legal and political systems, but also knowledge itself had to be decolonised, insisting – to various degrees – on specifically African modes of knowledge systems (Adesina, Citation2021; Biney, Citation2011; Bjerk, Citation2017; Rabaka, Citation2015).
Calls for decolonisation have also arisen in recent debates around global health. The 2020 ‘Global Health 50/50 Report’, for instance, shows that more than 70% of the leaders in the sample of 200 global health organisations are men, 80% of whom are nationals of high-income countries (HICs) (Global Health 50/50, Citation2020). The report concludes that the current system is ‘neither fair nor fit-for-purpose’, stipulating that ‘the health and well-being of people around the world will benefit from – and require – diverse leadership’ (p. 10). On a more technical level, public health scholars have adopted the concept of ‘reverse innovation’ – a term derived from the fields of business management and commercial product innovation – to identify the potential of products and technical developments from the global South for markets in the global North (Crisp, Citation2014; Govindarajan & Trimble, Citation2012; Immelt et al., Citation2009; Zinsstag et al., Citation2019). Debates around ‘reverse innovation’ in global health from the late 2000s signalled an emerging acknowledgement that HICs have much to learn from low- and middle-income countries (LMICs) in terms of health-related knowledge, practices, and products, and that ideas emanating from LMICs could potentially instigate healthcare transformation.Footnote4 Health practitioners were urged to seek out southern innovations – from products and technologies to health financing and governance – from which northern countries may benefit (Crisp, Citation2010; Skopec et al., Citation2019; Syed et al., Citation2013).
However, debates around ‘reverse innovation’ reveal the difficulties associated with the recognition of southern innovations. Harris et al. (Citation2016, Citation2020) have argued that, while the term has a certain ‘marketing currency’, its association with low-income contexts often carries a negative association with poverty and poorer quality. Furthermore, disagreement abounds about the appropriate definition of a ‘reverse innovation’, with varying emphases on the phases of ideation, development, testing, and implementation (Von Zedtwitz et al., Citation2015). Further, uncovering such innovations may be challenging, as they are often localised solutions which are not typically documented (Skopec et al., Citation2019).Footnote5 More fundamentally, some worry that ‘reverse innovation’ still invokes an ostensibly normative directionality of knowledge transfer from the West to the rest of the world (Lokugamage et al., Citation2019; Skopec et al., Citation2019). Additionally, by suggesting a simple South–North directionality, the concept continues to limit knowledge exchange to a transfer between two distinct loci instead of accounting for multiple influences (Harris et al., Citation2016).
Other fields related to public health are also seeing the emergence of critical debates around traditional North–South knowledge transfers. Urban planners are critically reassessing the ideas and practices informing urban planning approaches. Based on planning traditions emanating from Western Europe and the United States of America, these have often been simplistically transferred to, or imposed upon, southern contexts through processes of colonialism and globalisation (Watson, Citation2009). As a result, urban planning systems have facilitated the social and spatial exclusion of the poor, and undermined environmental sustainability. This has stimulated a new emphasis on the importance of ‘situated’ planning practices (Watson, Citation2009, p. 187) in response to the specific social, spatial, economic, and environmental contexts for which they are intended. Scholars such as Njoh (Citation2016) have highlighted the potential of applying indigenous knowledge to address current public health and urban planning challenges, particularly through more participatory processes. Participatory planning and development approaches developed locally in the global South have indeed been adopted by Western European cities (Sintomer et al. Citation2008). In recent years, urban planners have more confidently expressed the potential of northern cities to learn from southern counterparts as they increasingly face similar challenges of economic competition, poverty, social exclusion, territorial fragmentation, and climate change. Bolay et al. (Citation2016) hence argue for a new perspective on ‘slums’ that characterises southern cities as ‘potential pool[s] of solutions’ for problems faced by city-dwellers everywhere (p. 3).
Studying southern knowledge and innovation
To a large degree, existing studies on innovation and transnational knowledge flows remain restricted to closely related disciplines. The research project entitled ‘African contributions to global health: Circulating knowledge and innovations’, funded by the Swiss National Science Foundation (SNSF) and based at the University of Basel, the Swiss Tropical and Public Health Institute (Swiss TPH), and the École Polytechnique Fédérale de Lausanne (EPFL), recognises that a single discipline cannot provide sufficient orientation in analysing the intercontinental (non-)circulation of knowledge over time. The project unites scholars and PhD candidates with expertise in African history, epidemiology, environmental engineering, health economics, pharmaceutical medicine, public health, and urban planning. Thus, it offers an example of how researchers from the humanities, health sciences, and application-oriented fields may come togetherFootnote6 to identify and examine emerging health-related ideas, approaches, and practices; investigate how health-related knowledge is produced and circulates, and how innovation works in practice; and study the factors that enable or hamper knowledge exchange in a fair and equitable way.
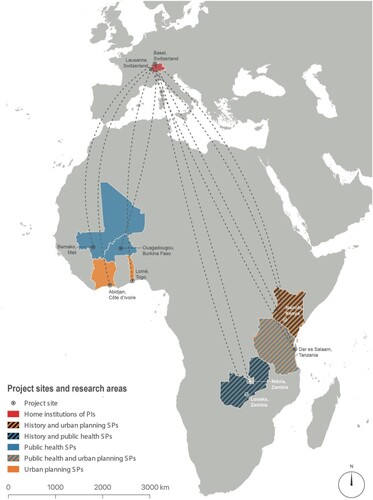
Our research team consists of a principal investigator, two co-applicants, two postdoctoral researchers, four PhD candidates and over 15 project partners. We study ‘African contributions to global health’ in the sense of bodies of knowledge, applications, or technologies that were shaped by African actors – medical personnel, experts, and local populations – or that emerged through international cooperation in specific settings in Africa () and that are (potentially) decisive for questions of health on a much broader scale. Taking account of the contingent, situated, but multidirectional nature of knowledge communication, we investigate scientific knowledge as much as knowledge developed or applied in everyday situations. Focusing on circulation and flows allows us to avoid centre/periphery tropes and essentialising notions of knowledge having a distinct geographic origin. Instead, we ask how knowledge travels, under which conditions innovations occur, and highlight the asymmetries that have restricted the production and circulation of health-related knowledge.
Figure 1. Map showing countries and study sites of the ‘African contributions to global health: Circulating knowledge and innovations’ project (PIs: principal investigators; SPs: subprojects).
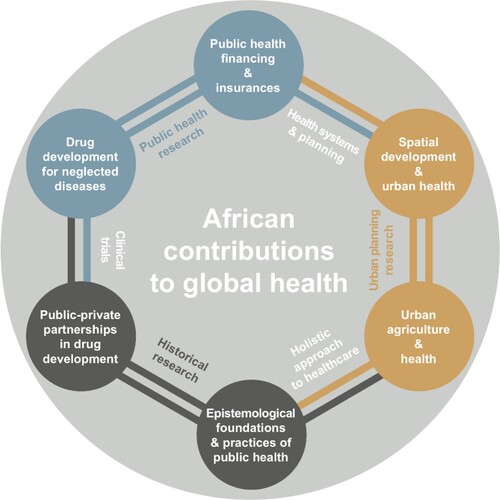
This project connects disciplines with diverse methodological foundations and paradigms, each offering unique contributions (). Historical investigation, based on archival research and oral history, can yield insights into factors which enabled or constricted mutual learning, including questions of power relations and social norms. We seek to challenge the current presentist bias in discussions on innovation that ignore long-standing historical evidence of cross-cultural knowledge circulation. Yet, a historical approach does more than celebrating ‘lessons from the past’. Contributing conceptually to overall understandings of knowledge circulation and innovation, historians are wary of invoking the term ‘innovation’, as few ideas are truly new, and what might be termed ‘innovation’ does not necessarily have the positive connotations that underlie existing research. In fact, historians have discussed rather sinister cases of colonial learning, including medical research based on human experimentation (Graboyes, Citation2014; Tilley, Citation2016). The notion of the colonies as ‘laboratories of modernity’ (Rabinow, Citation1989) has been widely explored in historical research (Anderson, Citation1995; Eckart, Citation2002), which has, however, also reflected critically on the fact that colonial power structures enabled European actors to conduct experiments that would have been difficult or impossible to carry out at home (Phillips, Citation2006).Footnote7 Historical examination of ‘innovation’, pointing to the often implicitly teleological narratives attached to it, can highlight cases of failure, and show how the term served to distinguish supposedly ‘dynamic’ western civilisation from the ‘backward’ South.
Figure 2. Interdisciplinary connections in the ‘African contributions to global health: Circulating knowledge and innovations’ project.
Despite the postulation of ‘reverse innovation’ as a key trend in public health – and, indeed, global health – existing research on South–North innovation in healthcare is piecemeal. Public health research in Africa and Europe has remained largely disconnected from each other, whilst the actual occurrence and global applicability of southern innovations is still in its infancy. This project utilises the breadth of public health science to expand this field in empirical and conceptual terms. Looking beyond medical treatments and technologies – typical foci of those seeking ‘reverse innovations’ – we investigate knowledge production and exchange in relation to models of drug development and healthcare financing. In the long run, these may offer promising insights for struggling healthcare sectors in the global North.
Urban planning and public health emerged simultaneously in nineteenth century Europe as closely intertwined fields with shared goals, such as the elimination of poverty and control of infectious diseases. However, these fields have become largely disconnected. Recently, spatial methods have received attention again in public health (Auchincloss et al., Citation2012), and urban planners have started to re-emphasise health concerns – yet examinations of the relation between the built environment and issues of human health are largely focused on North America and Europe (Giles-Corti et al., Citation2016; Sallis et al., Citation2016). Also, there is little interdisciplinary collaboration in many LMICs (Coburn, Citation2004; Njoh, Citation2016), not least due to the administrative divisions between authorities of urban planning and public health. This project contributes to the expansion of integrated analyses and solutions, thereby contributing to the advancement of recent approaches in urban planning that seek to better fulfil the needs of individuals in LMICs (Bolay et al., Citation2016; Chenal, Citation2014a; Citation2014b; Healey, Citation1998).
Utilising the analytical power and methodologies of these respective fields, our overarching goal is to develop an interdisciplinary perspective on health and innovation from an Africanist viewpoint. To demonstrate these arguments, the following section introduces the research agendas and some preliminary results of four out of a total of six ongoing case studies.
Case studies
Drug development
Over the past five decades, the process of developing new drugs has become increasingly complex, more expensive, and more global (Avorn, Citation2015; DiMasi et al., Citation2015, Citation2016). The escalation of costs is compounded by the significant attrition rate during pre-clinical and clinical development, in which only about one in nine molecules entering clinical trials will eventually become a marketed drug (DiMasi, Citation2001, Citation2002; DiMasi et al., Citation2010; Grabowski et al., Citation2002). Drug development and clinical trials are subject to extensive regulations by national authorities and regulatory bodies. Managing clinical trials and ensuring data quality has become a major task, which is reflected in an annual 10% growth of the market for contract research organisations (CROs) carrying out clinical trials. The resulting costs of goods pose a challenge to health priorities and systems. For diseases endemic in the global South (e.g. malaria), the pressure to economise has led to significant innovation in the efficiency and work organisation of drug development and the ways in which knowledge is generated. Two subprojects, taking different approaches, thematise questions around drug development.
The first, led by historian Tanja Hammel, focuses on the antimalarial agent mefloquine. In the wake of World War II, the World Health Organization (WHO) emerged as a major player in mitigating the effects of so-called tropical diseases. However, it was not until 1974 – with the creation of its Special Programme for Research and Training in Tropical Diseases (TDR) – that WHO started to take cautious steps towards collaborating with the pharmaceutical industry in drug development. TDR also marked a key move by WHO to study tropical diseases in endemic areas. Research centres were established across the globe, including on the Zambian Copperbelt in Ndola, and clinical trials on a variety of tropical diseases were conducted at the centre. These were an early example of the now well-established model of public-private partnership (PPP) and offer a window into practices of collaboration between public institutions and the private sector.
From the mid-1970s, numerous antimalarial agents were tested at Ndola's Tropical Diseases Research Centre (TDRC). Interest in mefloquine arose amid growing scientific concern about the emergence of resistance to older commonly used antimalarial drugs, such as chloroquine. Thus, clinical trials conducted in Ndola involved testing the efficacy of mefloquine compared to chloroquine in double-blind randomised controlled trials. The results generated by TDRC staff were forwarded to WHO headquarters in Geneva and the pharmaceutical company Hoffmann-La Roche (commonly known as Roche) in Basel, Switzerland.
Led and staffed by African, mostly Zambian nationals – a measure intended to forestall the post-independence exodus of Zambian scientists to the global North – the research centre at Ndola soon became a TDR showpiece, visited and admired by tropical medicine experts from across the world. This generation of Zambian pharmacologists and medical practitioners demonstrated that research on malaria and other endemic tropical diseases could and should be researched in endemic areas. Scientists from the centre travelled around the world, presenting their research at scientific meetings and conferences. The WHO presented Ndola as evidence of productive cooperation between public and private, as well as global and local partners. However, as Hammel's ongoing research has shown, the situation on the ground was not always this positive. The institution faced staff shortages and encountered resistance from local communities who did not want to participate in trials which they believed rendered them guinea pigs for European drugs. Moreover, development processes did not proceed as planned, and no large-scale phase III trial was ever conducted for the mefloquine-based drug Lariam®. Nevertheless, based on clinical trials conducted in Ndola and elsewhere in the global South, Lariam® gained official regulatory approval. As Zambian voices had warned, the drug did not benefit local communities in malaria endemic areas but was mainly sold as prophylaxis for travellers from the global North. In fact, some countries in the global South – such as India – did not approve Lariam®.
This subproject starts to uncover and assess the transcontinental forms of knowledge production and circulation that PPPs entailed, with particular attention to the role of Africans – researchers, medical staff, and study participants – in these often ambiguous processes. Hammel collaborates with Zambian health economist Felix Mwenge based in Lusaka and Nigerian anthropologist Osuolale Joseph Ayodokun based in Ibadan. While Hammel conducts archival research in Swiss archives of WHO and Roche, and interviews former Roche employees involved in TDR, Mwenge is scrutinising archives in Ndola and interviewing contemporary witnesses of the TDR programme. Ayodokun has conducted archival research in Lagos and Ibadan, traced interview partners and co-conducted interviews with Hammel. Their preliminary findings reveal the historical emergence of PPPs in drug development, including their forms of governance, and the uneven power relations and experiences characterising such partnerships. This provides insight into alternative models of drug development, which are today globally prevalent, with their roots in contexts such as the TDRC in Ndola.
A second subproject investigates contemporary alternative models of drug development. The high cost and complexity of drug development has a particularly adverse impact on the field of neglected tropical diseases (NTDs), as the return on investment through sales for drugs are modest, even though the need is high (Trouiller et al., Citation2002). As a result, this field has seen the emergence of product development partnerships (PDPs). Eric Nébié, a Burkina Faso-trained physician with a specialisation in tropical medicine and vaccinology, compares organisational and operational modalities of the conventional HICs’ pharmaceutical track with these models used in LMICs.
PDPs are not-for-profit organisations operating as small think tanks collaborating with academia, biotech, and pharmaceutical companies. They usually focus on a single disease or a limited set of diseases by bringing together experts in that particular field. The cost of drug development in such models can be as little as 20% of that incurred during conventional pharmaceutical models (Maxmen, Citation2016). Recent cost-optimised development of drugs for human African trypanosomiasis, a deadly NTD, testifies to the success of strong African-based collaborations between PDP, industry, academia, and national disease control programmes. This highlights the capabilities of knowledge generation in the global South. Among other success stories of innovations in drugs chemistry, the Drug Discovery and Development Centre (H3D) in South Africa has developed the most advanced in-house African compound being tested in phase II against malaria using a new target (Chibale et al., Citation2021), with the potential to address growing antimalarial resistance.
Given the success of PDP-style drug development, policymakers have started to discuss whether this model may be generalisable, particularly for medicines against rare (orphan) diseases in the North, but also as a means of accelerating or reducing costs for treating non-neglected diseases (Avorn, Citation2015; Carter et al., Citation2016; Maxmen, Citation2016; Tomaras & Dunman, Citation2015). By scrutinising PDPs and comparing these with more conventional models, this subproject seeks to pinpoint sources of over-expenditure and cost-saving mechanisms respectively, in order to identify saving prospects in pharma-based research as well as possible shortcomings in PDP-led trials. To compare clinical operations processes, Nébié works in the context of, and observes, clinical trials conducted in Burkina Faso, Mali, and Switzerland. This is supplemented by semi-structured interviews with key actors at both clinical trial sites and on sponsors’ side, enquiring into factors characterising different research models such as trial implementation, trial governance and organisation, trial documentation, ethical and regulatory aspects, quality control and quality assurance, project management, and digitalisation of clinical research. He also gathers quantitative data through an online survey of investigators and sponsor teams. Given the potential of clinical development approaches with PDPs, Africa is well positioned as a major driver of drug-related knowledge generation and circulation from the South to the North. Nébié's preliminary results suggest that there is room for rendering clinical development of drugs more efficient through leaner approaches in terms of governance, trial management, quality approaches (risk assessment), and supply chain management, particularly in pharma-sponsored clinical trials. The novel frames of collaborative drug development approaches involving pharma, PDPs, and academia such as the West African Network for Anti-Malarial Drugs (WANECAN 2) provide an opportunity for a mutual learning in clinical trials.
Healthcare systems and innovations
Given the constant pressure to improve health systems performance as well as their dependence on external support for health expenditure, African states have essentially become the global testing ground for health systems reforms. Despite severely limited resources and an almost 100% increase in population between 1990 and 2015 for the subcontinent overall, many African countries have done remarkably well in improving their health systems as well as key health indicators. Such improvements have led, for instance, to an over 50% reduction in child mortality over this 25-year period (UN Inter-agency Group for Child Mortality Estimation, Citation2018). Particularly over the past 20 years, a range of innovative healthcare and financing models emerged (Chahed et al., Citation2014; Senkubuge et al., Citation2014). While many studies investigate individual reforms, there is a paucity of systematic data on the impact of these large-scale experiments. As a result, the potential that these experiences have for providing important insights into global health questions has so far been overlooked.
Public health specialist Doris Osei Afriyie is generating evidence of the impact of health insurance schemes in LMICs with case studies pursued in Tanzania and Zambia. Her research also attempts to assess the potential implications of the findings in LMICs for higher-income countries. Health insurance schemes have been used increasingly as a strategy to make progress towards Universal Health Coverage (UHC). Spurred by Sustainable Development Goal (SDG) 3, target 3.8 – that is, ‘achiev[ing] universal health coverage, including financial risk protection, access to quality essential health-care services, and access to safe, effective, quality and affordable essential medicines and vaccines for all’ – several African countries have started to implement comprehensive health insurance reforms. Their goal is to reduce the financial burden on patients and improve access to quality of care regardless of an individual's ability to pay.
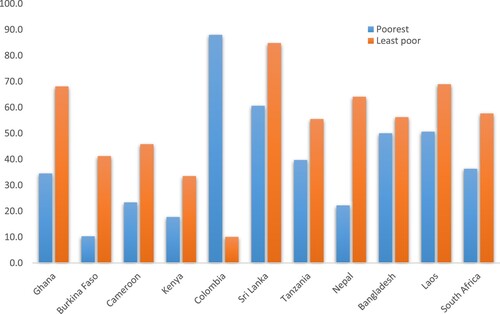
In her research, Osei Afriyie combines systematic review of evidence on the impact of these health insurance schemes with in-depth investigations. Evidence from her systematic review found that, on average, better-off households are more likely to enrol in health insurance schemes compared to poor households despite pro-poor policies by schemes in LMICs () (Osei Afriyie et al., Citation2022). Some of the challenges faced by current schemes, particularly those implemented in Africa, were identification of the poorest and the most vulnerable population groups (Marwa et al., Citation2013; Umeh, Citation2017) as well as management and implementation of schemes at sub-national levels (Maluka, Citation2013). The only country where health insurance was higher for poor households was Colombia. Indeed, Colombia had a means-proxy testing approach to identify eligible individuals through their established social service beneficiaries’ identification system. The evidence from this review shows that despite governments’ best efforts, insurance programmes often fail to reach those that need it the most; a lesson that is valuable for LMICs and HICs alike.
Figure 3. Health insurance enrolment rates (in percentage) for the poorest and least poor in low- and middle-income countries.
Osei Afriyie's investigations in Tanzania and Zambia focus on the countries’ national health insurance. Tanzania was one of the first countries to promote health insurance through the launch of its National Health Insurance Fund (NHIF) in 1998. Despite low registration fees and major government efforts, insurance currently covers less than 10% of the population (Maluka & Bukagile, Citation2014). In collaboration with researchers at the Ifakara Health Institute (IHI) in Dar es Salaam, Osei Afriyie and her team seek to better understand the impact of Tanzania's NHIF on quality care. The study includes targeted community and stakeholder interviews, specifically with local and national leaders. Similar interviews were conducted in Lusaka, Zambia. While Zambia and Tanzania share many health systems characteristics, the Zambian government only passed its national health insurance bill in 2018, making it a productive comparative case to Tanzania. Working with partners at the University of Zambia, Osei Afriyie investigates the political and financial implications of this policy to assess the likely impact on quality of care for all Zambians. The newly established national health insurance scheme is the first exposure of most Zambians to health insurance, a field which is regularly subject to reform. Osei Afriyie's study therefore also seeks to better understand the relationship between the perception of health system quality and health insurance enrolment.
As these findings and comparative analyses on African health reforms are drawn together, they will be assessed for their global resonance by comparing recent health reform trends in OECD countries with parallel developments on the African continent. Debates around health systems financing are increasingly discussed in HICs, which face a number of similar challenges and pursue the same goal of providing cost-effective, high-quality healthcare.
A further subproject examines healthcare systems from an urban planning perspective. Historically, urban planning has been closely linked with public health, notably in African cities. During the colonial period, urban planning was geared towards creating healthy settlements that would allow European administrators, missionaries, and settlers to live in a ‘hostile’ setting (Njoh, Citation2008; Silva, Citation2015). During the twentieth century, however, the two fields were progressively disconnected. Globally, urban planning became increasingly influenced by capital accumulation (Harvey, Citation2003), while public health efforts progressively focused on microbiology and individual-level healthcare based on a curative approach, paying less attention to environmental determinants of health (Susser & Susser, Citation1996). In Kenya during the decades following independence, for instance, ‘a disproportionate share of spending has focused on curative, hospital-based health care’ leading to a ‘cost-ineffective health care delivery system which allows people to fall sick, then tries to cure them’ (Government of Kenya, Citation2013, p. 14).
Following from this observation, Brazilian architect Vitor Pessoa Colombo seeks to examine how the health status of urban residents correlates with their living environment. To gain a deeper understanding of environmental determinants of health in African cities, he is mapping health facilities, water, sanitation and hygiene (WASH) networks, and comparing their spatial distribution to that of cases of diarrhoeal diseases. The latter remain amongst the main causes of death worldwide, especially in Africa (GBD Citation2018; Diarrhoeal Disease Collaborators, Citation2018), and can be used as a proxy indicator of the quality of access to WASH services (Clasen et al., Citation2014). The study uses readily available open access data and combines quantitative spatial analyses conducted at different geographic scales, and thus relies on ecological analyses at city scale and cross-sectional household surveys at neighbourhood scale (Pessoa Colombo et al., Citation2022).
The subproject focuses on Abidjan, Côte d’Ivoire, and Nairobi, Kenya, and is conducted in close collaboration with local partners at the Centre Suisse de Recherches Scientifiques en Côte d’Ivoire (CSRS, Abidjan) and the Kenyan Medical Research Institute (KEMRI, Nairobi). The two cities have experienced rapid population growth, which took place within a poor development framework, creating complex housing production and settlement patterns, as well as public health challenges (Chenal et al., Citation2009; Owuor & Mbatia, Citation2012). At the same time, innovative WASH solutions can be found in the two cities that deserve further scientific inquiry. For instance, in Nairobi value-chain strategies have been applied to sanitation systems, to attain sustainable and safe maintenance of amenities (Auerbach, Citation2016). Additionally, in both cities, the utilities responsible for water distribution have implemented tailored interventions to extend water services to the urban poor (Drabble et al., Citation2018; Marin et al., Citation2009).
Assessing the impacts of such interventions on the risk of diarrhoeal diseases can be particularly informative to urban planners worldwide, notably in the global South. With over 1 billion urbanites living in ‘slums’ (UN-Habitat, Citation2020), transitional and more affordable solutions are urgently needed across the globe (Hutton & Varughese, Citation2016). In this sense, the use of subsidy schemes and non-networked solutions for water and sanitation services, as seen in Abidjan and Nairobi, are important case studies for planners to understand how to palliate the lack of access to basic services in impoverished urban settlements.
Conclusions: Opportunities and limits of cooperative research
A project that seeks to study innovation and knowledge communication from an Africanist perspective centrally depends on partners based in Africa. ‘African contributions to global health: Circulating knowledge and innovations’ involves different forms of collaboration with African researchers and institutions, some of whom, particularly the CSRS, were involved from the moment of setting the agenda of our project proposal.Footnote8 We also planned joint scientific conferences and stakeholder meetings in the main project sites – Abidjan, Dar es Salaam, Lusaka, and Nairobi – in order to bring different parties together and discuss our findings with diverse audiences. Thus far, however, most of our broader physical engagements have been stalled due to the COVID-19 pandemic, and international scientific exchanges have been largely restricted to online events.Footnote9 Thus, in addition to the restrictions on African involvement imposed through the funding format itself, which stipulates that project staff have to be employed at a Swiss academic institution, our project bears witness of how exposure, personal risk, and mobility restrictions related to COVID-19 exacerbate global asymmetries in scientific exchange. Ironically, therefore, the asymmetries of knowledge production and circulation that are the subject of our research are at least partly echoed in the ways in which our own project has evolved so far.
This article has called for a critically nuanced and historically grounded investigation into African contributions to global health through an interdisciplinary inquiry of health-related knowledge, practices, and applications emanating from Africa. In this regard, we are seeking to contribute to, as well as critique, ongoing debates on innovations from the South and their policy implications. While a recent New Yorker article celebrated ‘reverse innovation’, advocating the broader use of ‘[c]heap and simple medical devices’ already used in southern countries (Vanderbilt, Citation2019), Southerners who ‘do more with less’ are not necessarily content with doing so. To be sure, it is no coincidence that the recent revelation that the ‘often extravagant “North” has something to learn from innovations that emerged from resource-challenged settings’ (Syed et al., Citation2013, p. 1) emerged amid the 2008/2009 financial crisis, the imperatives of austerity and the growth of ageing societies. Reverse innovation must not become a modern version of the ‘double standards’ that shaped the colonial history of medicine in Africa (Tilley, Citation2016, p. 746), implying that cheaper, poorer quality is good enough for Africa – and by extension – poorer people in the global North. Moreover, as Pessoa Colombo's case study shows, in many regards, a South-South – rather than South–North – axis in knowledge circulation, connecting similarly structured political economies, may at times be even more relevant to questions of innovation.
Learning from the global South implies more than adopting simple and cheap technological fixes. Instead, it means recognising the vast contributions that Africans – be it prominent pan-Africanist thinkers of the decolonisation era and of today, or ‘ordinary’ farmers, healers, tradespeople, or mothers – have made to global epistemologies, without losing sight of the fact that South–North knowledge exchanges have also been inhibited and southern contributions silenced.
Ethical clearance
Eric Nébié submitted his subproject to the Ethics Committee of Northwestern and Central Switzerland (EKNZ) (registration number Req-2020-01364). It received an exemption statement since the interviewees are clinical research professionals and the subjects discussed covered managerial topics only. Hence, the project was considered to be outside the Swiss Human Research Act. Ethical approvals were obtained from the Comité national d’éthique in Mali under the registration number N°2021/14/CE/USTTB and the Comité éthique pour la recherche en santé (CERS) in Burkina Faso under the deliberation number N°2020-12-281. Individual written informed consent was obtained from all the participants. Tanja Hammel and Felix Mwenge obtained ethical clearance through the Biomedical Research Ethics Committee, University of Zambia (ref. no. 1198-2020) for their request to do research at the TDRC archive in Ndola and conduct interviews on the basis of the obtained data. Doris Osei Afriyie obtained ethical clearance from the University of Zambia Social Sciences and Humanities Ethical Clearance Committee (HSSREC-2020-SEP-012) and authority to conduct research from the National Health Research Authority (NHRA00018/15/10/2020). In Tanzania, she obtained ethical clearance from the Institutional Review Board of the Ifakara Health Institute (IHI/IRB/No: 6-2021) and the National Institute for Medical Research (NIMR/HQ/R.8a/Vol.IX/3684). In addition, she obtained ethical clearance from the EKNZ in Switzerland (AO_2020-00029). Vitor Pessoa Colombo obtained ethical clearance from the Kenya Medical Research Institute (KEMRI/RES/7/3/1) and authority to conduct research from the National Commission for Science, Technology & Innovation (NACOSTI/P/21/10921). In Côte d’Ivoire, he obtained clearance from the Comité national d’éthique des sciences de la vie et de la santé (ref. no. 005-22/MSHPCMU/CNESVS-km). He also obtained ethical clearance from EPFL (decision no. 068-2020).
Acknowledgement
The authors thank Sophie Irion at the University of Basel for her assistance in preparing the technical aspects of this paper.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes
1 Foreign Policy continued to update the list. In the March 2021 update, Senegal again occupied the second and Ghana the fifth position. Of course, African countries also faced and continue to face difficulties in combating COVID-19, and official action was hardly uniformly positive: see James et al. (Citation2021).
2 See also South African scientists’ pioneering and long unacknowledged role in detecting the Omicron variant (Harding, Citation2022).
3 ‘Global South’ has gained traction in the past 15 years as a critical concept for analysing patterns of wealth and power across different spatial scales. Although it is typically used in contradistinction with ‘global North’, it is more than simply a geographical shorthand – rather, it is primarily a political economy characterisation for examining localised struggles and experiences in relation to geopolitical relationships (see, for example, Clarke, Citation2018; Dados & Connell, Citation2012; Mahler, Citation2017). It is in this manner that we invoke ‘global South’ in this article – with specific reference to African countries, embedded in histories of colonial subjugation, ‘development’ and globalisation – to examine the dynamics of health-related knowledge.
4 See the series on reverse innovation launched by Globalization and Health in 2013, reviewed by Harris et al. (Citation2020).
5 Skopec et al. (Citation2019) note the Centre for Health Market Innovations and the WHO Compendium for Technologies for Global Health as databases which seek to document innovations from LMICs.
6 Further examples of interdisciplinary studies of health include the ‘Global Health Histories’ project established by the WHO in 2004 (https://www.who.int/global_health_histories/en/); the incorporation of anthropologists and historians into the activities of traditionally ‘hard science’-focused institutions such as the Institute Pasteur, Swiss TPH, and the London School of Hygiene and Tropical Medicine (LSHTM); and the emergence of the field of historical epidemiology (Giles-Vernick & Webb, Citation2013; Webb, Citation2014, Citation2015).
7 On contemporary debates on African populations as global guinea pigs, see Flint (Citation2020).
8 Eleven principles set out by the Swiss Commission for Research Partnerships with Developing Countries (Citation2012).
9 This includes launching an online discussion series ‘Global Health Africa: Interdisciplinary conversations on knowledge production and circulation’ with project partners and stakeholders as guest speakers. See https://www.globalhealthafrica.ch/
References
- Adesina, J. (2021). Dismantling and transcending colonialism’s legacy. The Elephant, https://www.theelephant.info/op-eds/2021/02/19/dismantling-and-transcending-colonialisms-legacy/
- Anderson, W. (1995). Excremental colonialism: Public health and the poetics of Pollution. Critical Inquiry, 21(3), 640–669. https://doi.org/10.1086/448767
- Auchincloss, A. H., Gebreab, W. Y., Mair, C., & Diez Roux, A. V. (2012). A review of spatial methods in epidemiology, 2000-2010. Annual Review of Public Health, 33(1), 107–122. https://doi.org/10.1146/annurev-publhealth-031811-124655
- Auerbach, D. (2016). Sustainable sanitation provision in urban slums–the Sanergy case study. In D. Auerbach (Ed.), Broken pumps and promises (pp. 211–216). Springer.
- Avorn, J. (2015). The $2.6 billion pill — methodologic and policy considerations. New England Journal of Medicine, 372(20), 1877–1879. https://doi.org/10.1056/NEJMp1500848
- Biney, A. (2011). The political and social thought of Kwame Nkrumah. Palgrave Macmillan.
- Bjerk, P. (2017). Julius Nyerere. Ohio University Press.
- Bolay, J.-C., Chenal, J., & Pedrazzini, Y. (2016). Learning from the slums for the development of emerging cities. Springer International Publishing.
- Carter, P. H., Bernt, E. R., DiMasi, J. A., & Trusheim, M. (2016). Investigating investment in biopharmaceutical R&D. Nature Reviews Drug Discovery, 15(10), 673–674. https://doi.org/10.1038/nrd.2016.104
- Chahed, M., Arfa, C., Patcharanarumol, W., Thammatacharee, J., & Ibañez, C. (2014). Monitoring and evaluating progress towards Universal Health Coverage in Tunisia. PLoS Medicine, 11(9), e1001729. https://doi.org/10.1371/journal.pmed.1001729
- Chenal, J. (2014a). Les villes africaines en attente de modèle. Metropolitiques.eu. https://metropolitiques.eu/Les-villes-africaines-en-quete-de.html
- Chenal, J. (2014b). The West African city: Urban space and models of urban planning. EPFL Press.
- Chenal, J., Pedrazzini, Y., & Kaufmann, V. (2009). Quelques rues d’Afrique. Observation et gestion de l’espace public à Abidjan, Dakar et Nouakchott. Les éditions du LASUR.
- Chibale, K., Wicht, K. J., & Woodland, J. G. (2021). Medicinal chemistry out of Africa. Journal of Medicinal Chemistry, 64(15), 10513–10516. https://doi.org/10.1021/acs.jmedchem.1c01183
- Clarke, M. (2018). Global South: What does it mean and why use the term? Global South Political Commentaries. https://onlineacademiccommunity.uvic.ca/globalsouthpolitics/2018/08/08/global-south-what-does-it-mean-and-why-use-the-term/#:~:text=Drawing%20on%20the%20work%20of,and%20peoples%20negatively%20impacted%20by.
- Clasen, T., Prüss-Üstun, A., Mathers, C. D., Cumming, O., Cairncross, S., & Colford Jr, J. M. (2014). Estimating the impact of unsafe water, sanitation and hygiene on the global burden of disease: Evolving and alternative methods. Tropical Medicine & International Health, 19(8), 884–893. https://doi.org/10.1111/tmi.12330
- Coburn, J. (2004). Confronting the challenges in reconnecting urban planning and public health. American Journal of Public Health, 94(4), 541–546. https://doi.org/10.2105/AJPH.94.4.541
- Comaroff, J., & Comaroff, J. (2012). Theory from the South: Or, how Euro-America is evolving toward Africa. Anthropological Forum, 22(2), 113–131. https://doi.org/10.1080/00664677.2012.694169
- Connell, R. (2007). Southern theory: The global dynamics of knowledge in social science. Polity.
- Crisp, N. (2010). Turning the world upside down: The search for global health in the 21st century. CRC Press.
- Crisp, N. (2014). Mutual learning and reverse innovation – where next? Globalization and Health, 10(14). https://doi.org/10.1186/1744-8603-10-14.
- Dados, N., & Connell, R. (2012). The global south. Contexts, 11(1), 12–13. https://doi.org/10.1177/1536504212436479
- De Sam Lazaro, F. (2020). ‘With few resources, Senegal emerges as a leader in the fight against COVID-19’, PBS, 18 December. https://www.pbs.org/newshour/show/with-few-resources-senegal-emerges-as-a-leader-in-the-fight-against-covid-19.
- DiMasi, J. A. (2001). Risks in new drug development: Approval success rates for investigational drugs. Clinical Pharmacology & Therapeutics, 69(5), 297–307. https://doi.org/10.1067/mcp.2001.115446
- DiMasi, J. A. (2002). The value of improving the productivity of the drug development process. PharmacoEconomics, 20(3), 1–10. https://doi.org/10.2165/00019053-200220003-00001
- DiMasi, J. A., Feldman, L., Seckler, A., & Wilson, A. (2010). Trends in risks associated with new drug development: Success rates for investigational drugs. Clinical Pharmacology & Therapeutics, 87(3), 272–277. https://doi.org/10.1038/clpt.2009.295
- DiMasi, J. A., Grabowski, H. G., & Hansen, R. W. (2015). The cost of drug development. New England Journal of Medicine, 372(20), 1972. https://doi.org/10.1056/NEJMc1504317
- DiMasi, J. A., Grabowski, H. G., & Hansen, R. W. (2016). Innovation in the pharmaceutical industry: New estimates of R&D costs. Journal of Health Economics, 47, 20–33. https://doi.org/10.1016/j.jhealeco.2016.01.012
- Drabble, S., Mugo, K., & Renouf, R. (2018). A journey of institutional change: Extending water services to Nairobi’s informal settlements. Water & Sanitation for the Urban Poor (WSUP). PDF Document. https://www.wsup.com/insights/a-journey-of-institutional-change-extending-water-services-to-nairobis-informal-settlements/.
- Eckart, W. (2002). The colony as laboratory: German sleeping sickness campaigns in German East Africa and in Togo, 1900-1914. History & Philosophy of the Life Sciences, 24(1), 69–89. https://doi.org/10.1080/03919710210001714323
- Flint, K. (2020). “Africa isn’t a testing lab”: Considering COVID vaccine trials in a history of biomedical experimentation and abuse. Journal of West African History, 6(2), 126–140. https://doi.org/10.14321/jwestafrihist.6.2.0126
- Foreign Policy. (2021). ‘The COVID-19 Global Response Index’, published 5 August 2020, updated 25 January 2021. https://globalresponseindex.foreignpolicy.com/.
- GBD 2016 Diarrhoeal Disease Collaborators. (2018). Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Infectious Diseases, 18(11), 1211–1228. https://doi.org/10.1016/S1473-3099(18)30362-1
- Giles-Corti, B., Vernez-Moudon, A., Reis, R., Turrell, G., Dannenberg, A. L., Badland, H., Foster, S., Lowe, M., Sallis, J. F., Stevenson, M., & Owen, N. (2016). City planning and population health: A global challenge. Lancet, 388(10062), 2912–2924. https://doi.org/10.1016/S0140-6736(16)30066-6
- Giles-Vernick, T., & Webb, J. A. (2013). Global health in Africa: Historical perspectives on culture, epidemiology, and disease control. Ohio University Press.
- Global Health 50/50. (2020). The global health 50/50 report 2020: Power, Privilege and priorities. London.
- Government of Kenya. (2013). Kenya Population Situation Analysis. Government of Kenya and United Nations Population Fund (UNFPA). https://www.unfpa.org/sites/default/files/admin-resource/FINALPSAREPORT_0.pdf
- Govindarajan, V., & Trimble, C. (2012). Reverse innovation: Create far from home, win everywhere. Harvard Business Review Press.
- Grabowski, H., Vernon, J., & DiMasi, J. A. (2002). Returns on research and development for 1990s new drug introductions. PharmacoEconomics, 20(3), 11–29. https://doi.org/10.2165/00019053-200220003-00002
- Graboyes, M. (2014). Introduction: Incorporating medical research into the history of medicine in East Africa. International Journal of African Historical Studies, 47(3), 379–398.
- Harding, A. (2022). Was South Africa ignored over mild Omicron evidence? BBC News, 20 January; https://www.bbc.com/news/world-africa-60039138.
- Harris, M., Dadwal, V., & Syed, S. B. (2020). Review of the reverse innovation series in Globalization and Health – where are we and what else is needed? Globalization and Health, 16(26), 1–4. https://doi.org/10.1186/s12992-020-00555-6
- Harris, M., Weisberger, E., Silver, D., Dadwal, V., & Macinko, J. (2016). That’s not how the learning works – the paradox of reverse innovation: A qualitative study. Globalization and Health, 12(1), 36. https://doi.org/10.1186/s12992-016-0175-7
- Harvey, D. (2003). The right to the city. International Journal of Urban and Regional Research, 27(4), 939–941. https://doi.org/10.1111/j.0309-1317.2003.00492.x
- Healey, P. (1998). Building institutional capacity through collaborative approaches to urban planning. Environment and Planning A: Economy and Space, 30(9), 1531–1546. https://doi.org/10.1068/a301531
- Hutton, G., & Varughese, M. (2016). The costs of meeting the 2030 Sustainable Development Goal targets on drinking water, sanitation, and hygiene. The World Bank. https://elibrary.worldbank.org/doi/abs/10.1596K8543.
- Immelt, J., Govindarajan, V., & Trimble, C. (2009). How GE is disrupting itself. Harvard Business Review, 87(October), 56–65.
- James, W., McClelland, A., Stanberry, L. R., Thompson, L. R., & White, L. (2021). Epidemic/pandemic response in Africa: COVID-19 in Egypt, Ethiopia, Kenya, Nigeria and South Africa. Institute for Social and Economic Research and Policy (ISERP).
- Lancet. (2020). Editorial: COVID-19 in Africa: No room for complacency. Lancet, 395(10238), 1669. https://doi.org/10.1016/S0140-6736(20)31237-X
- Lokugamage, A. U., Douglas, C., Gishen, F., & Fyfe, M. V. (2019). Reverse innovation, power imbalances, language, and avoiding cultural appropriation. BMJ, 367, 17003. https://doi.org/10.1136/bmj.l7003
- Mahler, A. G. (2017). Global south. Oxford bibliographies in literary and critical theory, ed. O’Brien, E. Oxford University Press.
- Maluka, S. O. (2013). Why are pro-poor exemption policies in Tanzania better implemented in some districts than in others? International Journal for Equity in Health, 12(1), 80. https://doi.org/10.1186/1475-9276-12-80
- Maluka, S. O., & Bukagile, G. (2014). Implementation of community health fund in Tanzania: Why do some districts perform better than others? International Journal of Health Planning and Management, 29(4), e368–e382. https://doi.org/10.1002/hpm.2226
- Marin, P., Ouayoro, E., Fall, M., & Verspyck, R. (2009). Un partenariat réussi pour l’eau en Côte d’Ivoire: Leçons tirées de 50 ans de gestion privée efficace. http://documents1.worldbank.org/curated/en/451011468243908787/pdf/517700BRI0Box310Gridlines1501French.pdf.
- Marwa, B., Njau, B., Kessy, J., & Mushi, D. (2013). Feasibility of introducing compulsory community health fund in low resource countries: Views from the communities in Liwale district of Tanzania. BMC Health Services Research, 13(298). https://doi.org/10.1186/1472-6963-13-298.
- Mavhunga, C. (2017). What do science, technology, and innovation mean from Africa? MIT Press.
- Maxmen, A. (2016). Busting the billion-dollar myth: How to slash the cost of drug development. Nature, 536(7617), 388–390. https://doi.org/10.1038/536388a
- Ndlovu-Gatsheni, S. (2018). Introduction. Seek ye epistemic freedom first. In S. J. Ndlovu-Gatsheni (Ed.), Epistemic freedom in Africa: Deprovincialization and decolonization (pp. 1–41). Routledge.
- Njoh, A. J. (2008). Colonial philosophies, urban space, and racial segregation in British and French colonial Africa. Journal of Black Studies, 38(4), 579–599. https://doi.org/10.1177/0021934706288447
- Njoh, A. J. (2016). Urban planning and public health in Africa: Historical, theoretical and practical dimensions of a continent’s water and sanitation problematic. Routledge.
- Osei Afriyie, D., Krasniq, B., Hooley, B., Tediosi, F., & Fink, G. (2022). Equity in health insurance schemes enrollment in low and middle-income countries: A systematic review and meta-analysis. International Journal for Equity in Health, 21(1), 21. https://doi.org/10.1186/s12939-021-01608-x
- Osseo-Asare, A. D. (2014). Bitter roots: The search for healing plants in Africa. Chicago University Press.
- Owuor, S., & Mbatia, T. (2012). Nairobi. In S. B. Bekker, & G. Therborn (Eds.), Capital cities in Africa: Power and powerlessness (pp. 120–141). HSRC Press.
- Pessoa Colombo, V., Chenal, J., Koné, B., Bosch, M., & Utzinger, J. (2022). Using open-access data to explore relations between urban landscapes and diarrhoeal diseases in Côte d’Ivoire. International Journal of Environmental Research and Public Health, 19(13), 7677. https://doi.org/10.3390/ijerph19137677
- Phillips, R. (2006). Sex, politics and empire: A postcolonial geography. Manchester University Press.
- Rabaka, R. (2015). The negritude movement. W.E.B. Du Bois, Leon Damas, Aime Cesaire, Leopold Senghor, Franz Fanon, and the evolution of an insurgent idea. Lexington Books.
- Rabinow, P. (1989). French modern: Norms and forms of the social environment. MIT Press.
- Sallis, J. F., Bull, F., Burdett, R., Frank, L. D., Griffiths, P., Giles-Cortis, B., & Stevenson, M. (2016). Use of science to guide city planning policy and practice: How to achieve healthy and sustainable future cities. Lancet, 388(10062), 2936–2947. https://doi.org/10.1016/S0140-6736(16)30068-X
- Samarajiva, I. (2020). ‘The overwhelming racism of COVID coverage’, Indica.ca, 10 September. https://indi.ca/the-overwhelming-racism-of-covid-coverage-78e37e4ce6e8.
- Senkubuge, F., Modisenyane, M., & Bishaw, T. (2014). Strengthening health systems by health sector reforms. Global Health Action, 7(1), 23568. https://doi.org/10.3402/gha.v7.23568
- Silva, C. N. (2015). On planting and planning. The making of British colonial cities. Planning Perspectives, 30(4), 675–678. https://doi.org/10.1080/02665433.2015.1063323
- Sintomer, Y., Herzberg, C., & Röcke, A. (2008). Participatory budgeting in Europe: Potentials and challenges. International Journal of Urban and Regional Research, 32(1), 164–178. https://doi.org/10.1111/j.1468-2427.2008.00777.x.
- Skopec, M., Issa, H., & Harris, M. (2019). Delivering cost effective healthcare through reverse innovation. BMJ, 367(November 14), 16205. https://doi.org/10.1136/bmj.l6205
- Susser, M., & Susser, E. (1996). Choosing a future for epidemiology: I. Eras and paradigms. American Journal of Public Health, 86(5), 668–673. https://doi.org/10.2105/AJPH.86.5.668
- Swiss Commission for Research Partnerships with Developing Countries (KFPE). (2012). ‘A guide for transboundary research partnerships, 11 principles’, 3rd edition, https://portal-cdn.scnat.ch/asset/4d8372ee-27d7-558a-b9db-77bf409ceef4/KFPE-11P-7Q-3d2018?b=370a2788-58f3-581e-85d7-2418b87c662e&v=8ef687bc-7b14-5a4f-ad9e-bf494cddc1d7_0&s=gLwVbtPON190F6auadVe-DPd_IOknFA_pssGzeBGB68h8nfbZIcnUaztPkFbUOKFef8V2 w2-5NzkK61J2WEdN4JXXheHl2gX1f6cLTTro8WFmDkhlKvHQjqRQDZdPmPo3whl0-P3PWWEWWinhvJ5h WLGC5hYwVTAPC0kLEC-F7g
- Syed, S. B., Dadwal, V., & Martin, G. (2013). Reverse innovation in global health systems: Towards global innovation flow. Globalization and Health, 9(1), 36. https://doi.org/10.1186/1744-8603-9-36
- Tilley, H. (2016). Medicine, empires, and ethics in colonial Africa. AMA Journal of Ethics, 18(7), 743–753. https://doi.org/10.1001/journalofethics.2016.18.7.mhst1-1607
- Tilley, H. (2020). COVID-19 across Africa: Colonial hangovers, racial hierarchies, and medical histories. Journal of West African History, 6(2), 155–179. https://doi.org/10.14321/jwestafrihist.6.2.0155
- Tomaras, A. P., & Dunman, P. M. (2015). In the midst of the antimicrobial discovery conundrum: An overview. Current Opinion in Microbiology, 27, 103–107. https://doi.org/10.1016/j.mib.2015.08.005
- Trouiller, P., Olliaro, P., Torreele, E., Orbinski, J., Laing, R., & Ford, N. (2002). Drug development for neglected diseases: A deficient market and a public-health policy failure. Lancet, 359(9324), 2188–2194. https://doi.org/10.1016/S0140-6736(02)09096-7
- Umeh, C. A. (2017). Identifying the poor for premium exemption: A critical step towards Universal Health Coverage in sub-Saharan Africa. Global Health Research and Policy, 2(1), 2. https://doi.org/10.1186/s41256-016-0023-6
- UN-Habitat. (2020). World Cities Report 2020. United Nations Human Settlements Programme, Nairobi. Available at: https://unhabitat.org/World%20Cities%20Report%202020.
- UN Inter-agency Group for Child Mortality Estimation. (2018). Levels and trends in child mortality report 2017, UN, Geneva.
- Vanderbilt, T. (2019). Reverse innovation’ could save lives. Why aren’t we embracing it? The New Yorker, 4(February). https://www.newyorker.com/science/elements/reverse-innovation-could-save-lives-why-isnt-western-medicine-embracing-it.
- Von Zedtwitz, M., Corsi, S., Søberg, P. V., & Frega, R. (2015). A typology of reverse innovation. Journal of Product Innovation Management, 32(1), 12–28. https://doi.org/10.1111/jpim.12181
- Watson, V. (2009). ‘The planned city sweeps the poor away … ’: Urban planning and 21st century urbanisation. Progress in Planning, 72(3), 151–193. https://doi.org/10.1016/j.progress.2009.06.002
- Webb, J. L. (2014). The long struggle against malaria in tropical Africa. Cambridge University Press.
- Webb, J. L. (2015). The historical epidemiology of global disease challenges. Lancet, 385(9965), 322–323. https://doi.org/10.1016/S0140-6736(15)60108-8
- WHO. (2020). ‘COVID-19 spurs health innovation in Africa’, 29 October. https://www.afro.who.int/news/covid-19-spurs-health-innovation-africa.
- Zinsstag, J., Pelikan, K., Hammel, T., Tischler, J., Flahault, A., Utzinger, J., & Probst-Hensch, N. (2019). Reverse innovation in global health. Journal of Public Health and Emergency, 3(2), 2–2. https://doi.org/10.21037/jphe.2018.12.05
