ABSTRACT
Distinct from quantifying the economic sequelae of tuberculosis (TB) in adults, data are scarce regarding lived experiences of youth and their caregivers seeking and sustaining TB treatment in low income communities. Children ages 4–17 diagnosed with TB and their caregivers were recruited from rural and semi-urban northern Tanzania. Using a grounded theory approach, a qualitative interview guide was developed, informed by exploratory research. Twenty-four interviews were conducted in Kiswahili, audio-recorded and analyzed for emerging and consistent themes. Dominant themes found were socioemotional impacts of TB on households, including adverse effects on work productivity, and facilitators and obstacles to TB care, including general financial hardship and transportation challenges. The median percentage of household monthly income spent to attend a TB clinic visit was 34% (minimum: 1%, maximum: 220%). The most common solutions identified by caregivers to mitigate adverse impacts were transportation assistance and nutrition supplementation. To end TB, healthcare systems must acknowledge the total financial burden shouldered by low wealth families seeking pediatric TB care, provide consultations and medications locally, and increase access to TB-specific communal funds to mitigate burdens such as inadequate nutrition.
Trial registration: planned sub-study of the registered prospective study, NCT05283967.
Trial registration: ClinicalTrials.gov identifier: NCT05283967.
Background
A disease disproportionately impacting low wealth and resource scarce communities, tuberculosis (TB) has the potential to entrap individuals and families in a vicious poverty-disease cycle as a result of exorbitant out-of-pocket health expenditures, both direct (i.e. consultations, medicines, hospitalization, transportation costs) and indirect (i.e. lost wages). Within the End TB Strategy, the World Health Organization advocates to reduce the catastrophic costs from TB, defined as ‘total costs borne by patients in tuberculosis treatment, exceeding a given threshold (e.g. 20%) of the household’s annual pre-TB income’ (World Health Organization, Citation2022a; World Health Organization, Citation2022b).
To date, numerous studies focused on the catastrophic burden of TB on individuals and households have been informed by cost-of-illness surveys, income data, regression models and other statistical analyses with the goal of quantifying the economic sequelae of TB disease (Barter et al., Citation2012; Brinda et al., Citation2014; Getahun et al., Citation2016; Madan et al., Citation2015; Mhalu et al., Citation2019; Njagi et al., Citation2018; Prasanna et al., Citation2018; Stracker et al., Citation2019; Tanimura et al., Citation2014; Ukwaja et al., Citation2013a; Ukwaja et al., Citation2013b). However, prior studies of catastrophic costs focus primarily on the household unit and adult wage earners, and fail to incorporate the perspectives of and impacts on youth affected by TB. The present study broadens the scope of that approach by exploring the lived experiences and personal testimonies of Tanzanian children living with TB and their caregivers and contextualises these findings within the sustained financial impacts.
Methods
Theoretical framework and thematic analysis
Using a grounded theory approach for data collection and analysis (Glaser & Strauss, Citation2017), and qualitative interviews as primary source material, the principal aims were to understand both the tangible and intangible impacts of pediatric TB illness on rural and semi-urban households in two municipalities. Qualitative methods were used to probe the sociocultural and behavioral contexts of TB and to understand children’s and caregivers’ health care experiences (Foley & Timonen, Citation2015). Researchers also hoped to learn how to better tailor interventions to hard-to-reach and vulnerable populations in Tanzania who are disproportionately impacted by the disease.
In deductive (theory-driven) research, pre-established theoretical hypotheses are tested by way of data collection. In a grounded theory (data-driven) approach, the inverse is true. Our research team sought to generate theoretical insights as themes emerged from the data in the qualitative interview transcripts. A grounded theory approach allowed for the emergence of themes and priorities identified by participants themselves, which we had not necessarily anticipated at the outset of the research study. We conducted thematic analyses on the interview transcriptions; for example, we examined responses to the question of how daily life changed having a sick child in the household, and explored how lower wealth families strategized ways to obtain transportation fare when money was scarce (Chapman et al., Citation2015). Emerging themes are presented in the results section with supporting reflections and testimonies from participants. Quantitative statistics are presented for descriptive purposes to frame further the sociocultural context.
Study setting and participants
This qualitative study of the impact of childhood TB was embedded within a larger pharmacokinetics study of children aged 4–17 enrolled at two sites: Haydom Lutheran Hospital, a regional referral hospital located in a rural area of the Manyara region; and Kilimanjaro Christian Medical University College, an academic medical center in the municipality of Moshi, Kilimanjaro region.
Participants were included from the larger cohort via convenience sampling (Guest et al., Citation2006; Small, Citation2009). Children and their caregivers who were conversant in Kiswahili were enrolled to include a representative sample of the children with TB from the two catchment areas, including both the younger (4–10) and older (11–17) participants, with equal representation of genders. Fewer children were enrolled from the Moshi site due to delayed onset of study enrollment. All participants were recruited during face-to-face encounters and conversations.
Study design
By way of a semi-structured guide [Additional File 1], adults’ and children’s perceptions were explored regarding their understandings of TB; patterns of daily life in the household before and during a child’s illness; the reactions of relatives and community members to a child’s disease; potential barriers and facilitators to care; and other related topics. The U.S. and Tanzanian research teams designed the guide in a collaborative, culturally-informed and iterative process prior to launching the study. Mock interviews were conducted among team members to refine questions; however, the guide was not pilot tested with participants. Given the age range of participants and the children’s ability and/or inclination to engage, responses were expected to vary and thus the interview guide was largely tailored toward the parent/caregiver, with additional child-directed questions interspersed throughout. Adult participants were asked what additional information, resources or support would be helpful for a family affected by TB.
Data collection
All interviews, which ranged from 25 to 45 min in duration, were conducted in Kiswahili by DM, SL, PM and PM and audiotaped in private rooms on the premises of the research hospitals. Researchers included an assistant nurse officer, a medical doctor, a registered nurse and a doctoral student with a master’s degree in social work. All had extensive experience providing clinical care to persons living with TB and participating in international research studies and clinical trials focused on infectious disease. Two researchers were male and two were female. Three interviewers who worked in clinical TB care participated in a three-day intensive training on qualitative research methods delivered by a local social scientist; a fourth had advanced academic training in qualitative methods and global infectious diseases research. Interviewers established rapport with participants prior to the study encounter by way of introductions and discussing the research opportunity with them during their child’s pharmacokinetic study visits to the research hospital. Only the children, their caregivers and family members and the researchers were present during interviews. Some researchers chose to take discrete field notes during or immediately after the interviews. Audio files were transcribed by CM, DA, PM, RG, SL, DK, MS and PM and translated to English by DA, PM, RG, SL, MS and PM. The transcripts were then imported into Dedoose for coding and thematic analysis [Version 9.0 (2021); SocioCultural Research Consultants, LLC, Los Angeles, CA] (Deterding & Waters, Citation2021). A preliminary codebook was developed by DA, KPG, MG, PM and SL using the aforementioned grounded theory, an inductive process which reflexively interrogates the positionality of the researcher and foregrounds participants’ voices and accounts in the analysis.
Analysis
At least two members of the coding team coded the first 12 transcripts, after which thematic saturation was reached (Hennink et al., Citation2017). The final codebook [see abridged version as Appendix] was applied to all interviews, with all five aforementioned team members coding the final 12 transcripts independently. Researchers not native to Tanzania continuously probed lexical and cultural nuances in consultation with Tanzanian colleagues who were fluent in Kiswahili to ensure valid interpretations of the text. Discrepancies were resolved via discussions with the full team to enhance analytic dependability (Morse et al., Citation2002). Participants did not review the final versions of the transcripts, in part due to the infrequency of clinic visits, transportation burden and distance from the research facilities. To date, they have not provided feedback on our team’s findings. Reporting complies with Consolidated Criteria for Reporting Qualitative Research guidelines (Tong et al., Citation2007). In addition to performing qualitative analysis, families were also asked about finances including average earnings and expenditures incurred including time and money on TB-related issues; frequencies and medians are reported. Potential solutions offered are described using simple frequencies.
Rigor
The study team employed rigorous techniques to render the research credible, transferable and dependable (Cypress, Citation2017). While the research team used a streamlined semi-structured interview guide, researchers probed for additional information and allowed the participants to guide the conversation when possible. Participants’ words are used in the final manuscript and U.S.-based researchers debriefed regularly with their Tanzanian counterparts to confirm interpretations of the interview transcripts to ensure meaning was not lost in translation or misconstrued. The team was reflexive and considered how positionality, status and/or preconceptions of the interviewers inevitably affected the research encounter. We used the same data collection methods across different demographic groups and geographical locations (i.e. Haydom, Moshi). Finally, we describe the specific purpose of the study, how and why participants were selected, and provide a detailed description of our research methods, interpretation and presentation of the findings.
Ethics
The study was approved by institutional review boards at the National Institute of Medical Research in Tanzania, and the University of Virginia. The larger cohort from which the participants were drawn was registered with clinicaltrials.gov, NCT05283967. Written consent was obtained from guardians and assent from all children 7–17 years of age prior to participation in the study.
Results
Twenty-four participants were enrolled, including four recruited from Moshi and 20 from Haydom; two interviews were completed by the child alone (ages 10 and 15), while the remainder had input from child/caregiver dyads. Demographic characteristics are detailed in . Study participants hailed from 19 villages across northern Tanzania, representing 10 different tribes and six languages. Emerging themes presented here include (1) socioemotional impacts; (2) a broadened scope of financial impacts; and (3) facilitators and barriers to pediatric TB treatment.
Table 1. Participant demographic characteristics.
Socioemotional impact on children
Nearly half (n = 11, 46%) of participants reported that their TB illness or their child’s TB illness had a detrimental impact on relationships with their peers and classmates. A 10 year-old girl shared her experience with bullying at school. ‘People are afraid,’ she recounted:
They are saying that I will infect them. Then you will find you do not have anyone to play with. You are alone. They run away from you … Then [someone said], ‘This one may be sick. Don’t stay near her.’ Sometimes they even create words; they scold me and you will find I do not have any one to play with. They say, ‘Your mother doesn’t like you to be like this.’ I just go and stay inside. I do my [homework] questions. When I am tired, I just go to sleep, but I usually feel lonely.
She has been out of school for three months now and she does not play. She is silent all the time. She is a person of stress. She does not want to stay with her peers when they are playing. She feels angry and it is normal to her.
‘Where is he? What is he suffering from?’ Even during mealtimes, they keep asking
This is because they love him. They love playing with him.
Similarly, the father of a 14 year-old boy recalled that when his son fell ill with tuberculosis, village youth would come to their home on weekends to visit the boy:
The children who used to play on the same [soccer] teamstarted complaining that they have lost their striker, as the striker is at home, sick. His team was affected so much that it broke up. His school team also broke up, as they depended on him.
Socioemotional impact on caregivers
Fourteen (64%) of caregivers or children themselves reported feeling varying degrees of sadness, uncertainty, disappointment and shock upon learning of their TB diagnosis or their child’s TB diagnosis. Four participants shared that they were initially unfamiliar with TB, especially its presentation in children, who they did not believe were susceptible to the disease. The older brother of a 13 year-old girl described his reaction:
I felt bad. How can it be that the child has TB? We used to hear about tuberculosis in adults, since they smoke, they ingest chemicals. I felt hurt; that is why I had to bring her [to the hospital]. It is not a good thing for a young child to have tuberculosis. It was a new thing to me. It surprised us a lot as a family. How can a young child have this problem?
The first eagerness is to know what you are suffering from, even if you were told it is a disease that people might be afraid of. But it is also a joy to know what you are suffering from because you are sure. ‘I have TB.’ So, knowing that I have TB, I am sure that I will be treated. I was happy to find out that my child suffered from TB. She will get treatment rather than just taking regular medications without knowing what she is suffering from.
Socioemotional impact on siblings
Nine caregivers reported that the sick child’s siblings were affected emotionally by the disease. ‘They did not receive this incidence with pleasure,’ explained the mother of a 12 year-old boy. ‘After it happened, they accepted it. They cannot change it. The joy they always had diminished.’ Others described how having a child with TB shifted a heavier chore burden onto healthy siblings, who missed interacting with their playmate and ultimately resigned themselves to completing a greater share of ‘heavy’ tasks, such as fetching water for the household, in their fellow’s absence. When asked how other children in the home reacted to their seven year-old brother’s illness, one guardian responded:
With sadness! They have been affected a great deal, as they expected to be with him, playing with him, seeing him around, but due to the illness, he cannot socialize with them. They have been asking questions, why they do not see him regularly. They expected him to be there so that they play and be happy together … They used to work together but currently, they do not. They feel so sad about this.
Socioemotional impact on neighbors
Seventeen (71%) of caregivers and children described maintaining altruistic and mutually beneficial relationships with other villagers following the child’s tuberculosis diagnosis. Neighbors prayed for children’s healing, provided moral support to the affected families, visited sick children regularly and encouraged parents and guardians to adhere to their child’s prescribed medication regimen to ensure their recovery. Some neighbors helped the affected families with everyday farming and livestock chores while the parents or caregivers tended to their sick child. An eight year-old boy said of his neighbors, 'They give me hope.’ They tell me, ‘Don’t worry. It is a disease which can be cured.’
Neighbors demonstrated solidarity with the mother of a four year-old boy with TB by providing holistic support during the child’s illness: emotional, material and adherence-related. ‘They indeed come to my house advising me that I should keep courage,’ related the mother.
There are others – you will find them coming home and even bringing drinking water or money. They advise me, ‘As you've been instructed from the hospital, don’t miss giving the child the medication.’ Others say to me, ‘You tell me the day you are attending hospital. I will contribute something, even if it could be a little.’
Five caregivers reported that their child’s relationship with village children worsened after initiating TB treatment, largely due to others’ fears of becoming infected. Children as young as five years-old were shunned by their peers because of their diagnosis. The mother of a kindergartener shared that her son ‘doesn't play much with his teammates because they separate him a lot of the time. He is playing by himself. He is not getting out.’
Broadened scope of financial impact: Financial hardship separate from medical expenditures
Twenty-one (88%) of all participant households (100% of those from HLH) engaged in some degree of agricultural activities at home. Three parents/caregivers in Moshi made a living performing temporary work some seven hours away in the capital city of Dar es Salaam, driving motorcycle taxis, through entrepreneurship and pastry making. Self-reported estimates of household monthly income are described in .
Table 2. Family monthly income, TB expenditures and roundtrip travel time.
Three (13%) of caregivers or children themselves indicated a general sense of financial hardship independent of TB-related medical expenditures. Most, however, felt confident that they could ‘find’ or borrow money from trusted friends, relatives or neighbors in an emergency. Adolescents in particular experienced the household’s financial stress. A 10 year-old girl interviewed in Moshi related her family’s predicament. The child’s mother, a university graduate, had a steady office job until the child’s grandmother fell sick; the mother subsequently quit her job in order to care for the grandmother. The child’s father had traveled to Dar es Salaam for temporary work, but was often without money. The child confessed that some days, ‘We don’t have anything to eat, so we keep porridge in the flask. If there is a day that mother has no money, she will go to the shop to borrow. Then, later, when she gets money, she will come to pay.’
Another participant interviewed in Haydom, whose daily income was dependent on selling her cows’ milk, felt a sense of shame or stigma associated with her low wealth status.
Having no money becomes a big challenge because you are supposed to attend the clinic, and sometimes you do not have the money. When you go to someone to borrow, due to your financial status, [the person] feels like you will not even be able to return the money.
Broadened scope of financial impact: Impact to caregivers’ occupation
Twenty-two caregivers described their child’s TB disease and associated expenditures as having a direct negative impact on work productivity, income and/or household finances. Some caregivers found themselves postponing day work obligations to retrieve anti-TB medications from the dispensary on a weekly basis; still others quit their jobs entirely to stay home with their sick child. One participant described how she had to abandon a small business selling fish when her five year-old daughter fell severely ill with TB. ‘I could not go [fishing] anymore,’ she recalled. ‘I was struggling to find which hospital to go to, as she was becoming weaker.’
Adolescent children who contributed to the household economy also abandoned many of their previous work duties after acquiring TB. One 14 year-old boy earned 9,000 shillings each Saturday making sacks of charcoal and would help his family plow fields during the rainy season. The boy’s father shared:
Since he became ill, he cannot work. He could sometimes fetch water; he cannot even carry a bucket right now. He currently herds cattle only. On the weekends, he helps with cattle herding, as there is no heavy work in grazing cattle.
This is because there is only one bus to here. Therefore, when you go for medication, you cannot turn back earlier. You wait until evening when the bus is heading back … The income we were earning is now being used as bus fare to attend TB clinics [and] for food.
For the past two weeks, I have stopped [my regular work activities] to look after my child’s health. Responsibilities change because now you have no information about the disease and you are not prepared for it, but it has come. You must fight with it. Because as they say, ‘you can find money, but not a person.’
Facilitators and barriers to pediatric TB treatment: Effort required to obtain diagnosis
Prior to traveling to Haydom or Moshi, 19 (79%) of caregivers or children themselves indicated that they had sought healing for their child or in the case of children interviewed with TB that their families had sought healing for them, from at least one additional site of care, including dispensaries (n = 10), private or district hospitals (n = 8), local health clinics (n = 5), and traditional healers and household herbal remedies (n = 4). Nine caregivers reported a barrier of frequenting two or more places for their child’s treatment before establishing TB care at the hospital in Haydom or the academic medical center in Moshi. While numerous participants spoke of witchcraft as a commonly held belief in their village, all shared that they did not personally subscribe to this interpretation of bodily disease.
Five (21%) of caregivers or children themselves reported traveling directly to the clinics in Haydom or Moshi as a first healthcare touchpoint after noticing their child was ill, including two who were within walking distance. Another mother and child pair spent two hours on their roundtrip motorcycle taxi journey to Haydom. One father who sought immediate care for his 10-year-old son at the hospital in Haydom journeyed 6 h roundtrip by bus on clinic visit days. Despite the distance, he explained, ‘We knew if we went to Haydom Lutheran Hospital, we would get reliable treatment, as the hospital has advanced diagnostic equipment.’ Other parents and guardians echoed these sentiments, highlighting the dependable treatment options and sophisticated tests available to their children at the hospital as desirable services.
Facilitators and barriers to pediatric TB treatment: Transportation and clinic attendance
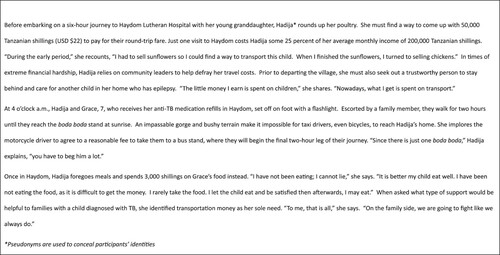
Fourteen caregivers identified transportation as a barrier to their child’s TB care. Five caregivers reported often lacking sufficient funds to defray roundtrip travel expenses on the day of their clinic appointment, requiring creative strategies to come up with the money. Some families lived in villages so distant from the hospital or dispensary that only one transport vehicle regularly serviced their village. The grandmother of a seven year-old girl related her experience embarking on an arduous overnight journey to Haydom, haggling with price gouging boda boda (motorcycle taxi) drivers and enduring hunger, all in the interest of safeguarding her young granddaughter’s health [].
Figure 1. Legend: Case study of detailed day in life of one family impacted by childhood tuberculosis. Boda boda = motorcycle taxi.
Six participants described infrastructure challenges as impediments to traveling to Haydom from their respective villages. ‘In the rainy season,’ explained a mother from a village some 4 h away from Haydom, ‘the buses do not make the trip.’ She paid motorcycle drivers 40,000 shillings (USD $17.32) to travel with her 11 year-old daughter to TB clinic appointments. When vehicles have access to the village, roundtrip bus fare costs only 4,000 (USD $1.73). The guardian of a seven year-old boy faced similar barriers. ‘As we live far,’ they explained,
We spend a lot of money on transport. The other challenge is sometimes the bus, as there is only one; so, sometimes you find it full or had already left. Therefore, we incur extra costs by taking a motorcycle so that we do not miss the clinic.
Mostly for our setting, support would probably be a fast means of transport, even if it were a nice bicycle for traveling. That would be a relief. It would be a fast means of transport compared to any other type, especially for us who live in the wilderness. Traveling by bicycle would make you arrive much earlier, as there is a shortcut to [the hospital in Haydom]. When you find out your child is sick and you have a means of transport, it would serve a lot.
I would advise that you should move your offices to the villages. When you move your offices to the village, you would diagnose many patients, even others who are not brought for treatment. You will see things out there … if you shift your offices to the villages. You will face these challenges.
Facilitators and barriers to pediatric TB treatment: Nutrition
Another barrier to supporting a child with TB through their treatment course was the higher household expenditures on and need for diversity of food. Five caregivers discussed the need to purchase special foods that were more compatible with anti-TB medications or to satisfy their sick child’s cravings. When a 14 year-old boy initiated treatment, his father explained:
Our food in the village did not go with these medications. Sometimes the child would tell you he feels like having a soup, while sometimes, it is not there, requiring chicken eggs. Sometimes he would say he likes fried foods, which are not there. Fruits are not there.
Sometimes the child needed a change in food. When you cook a certain food, he does not like it; he would want a different kind of food that was not there … For example, he would say he wants to eat ugali with beef. You prepare him that food, but when it is ready, he will not eat it as requested; instead, he will just eat a little bit.
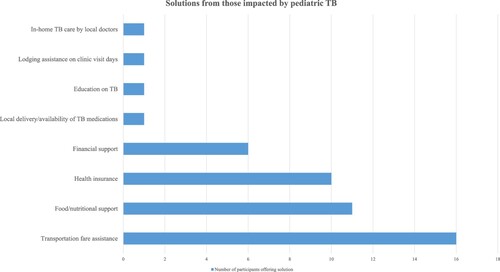
Solutions from those impacted by pediatric TB
All adult participants were asked what additional information, resources or support would be helpful for a family after their child was first diagnosed with TB and means to avert catastrophic cost. The majority indicated transportation fare as a solution and nearly half indicated nutritional supplementation and support, while the remainder of responses are illustrated in . Common ideas reflected those that could be included in social welfare programs, but others could be implemented at the institutional or individual health care worker level, such as home visits, medication delivery systems, and TB education.
Discussion
We report a grounded theory informed qualitative study exploring the socioemotional, interpersonal and financial impacts of childhood and adolescent TB on rural and semi-urban households in two Tanzanian municipalities. Moreover, we aimed to build upon the catastrophic costs argument by giving primacy to the voices and lived experiences of persons directly and indirectly affected by TB, thereby broadening the discussion to include nonmonetary impacts of the disease. Our findings demonstrate the significant toll that TB exacts on the emotional well-being of both sick and healthy children alike, as well as their caregivers. Ill and healthy children all suffer the effects of fractured relationships, leading to loneliness and isolation among the children with TB, and longing for normalcy among children who are well. Fear of contagion among classmates and neighbors leads to bullying, anger, and social withdrawal, highlighting the pervasiveness of TB-related stigma. However, in the face of adversity, families exhibited resilience in adhering to their children’s treatment course and found relief in securing a specific diagnosis and treatment plan. Others were buoyed by the support of neighbors, friends, relatives and health care workers. However, socioeconomic deprivation and transportation barriers continued to place a palpable strain on the majority of families, both semi-urban and rural alike.
The literature, though focused largely on adult populations, shines light on the pivotal role of social support in achieving TB medication adherence and treatment completion (Nirmal et al., Citation2022; Wen et al., Citation2020). Social support and accompaniment throughout the TB treatment cascade and the provision of child and adolescent friendly services have been shown to facilitate early diagnosis, promote optimal medication adherence, reduce stigma and enhance emotional wellbeing (George et al., Citation2021; Das et al., Citation2021). Robust patient-centered support systems serve to combat treatment fatigue, depression, low morale and lack of trust in medications among vulnerable populations living with TB and other comorbidities (Paz-Soldán et al., Citation2013). Implementing social welfare programs at the policy-level (i.e. counseling, psychosocial interventions, nutritional support, family support, family-centered care) would be important drivers of successful treatment outcomes among children impacted by TB in Tanzania. At the time of this publication, nutritional support programs in Tanzania are limited to people with drug-resistant TB and children with moderate/severe acute malnutrition. A safety net for remaining youth affected by TB is urgently needed.
Our findings align with previous work documenting the multiple intersecting challenges that preclude access and adherence to otherwise free medications for low wealth children and adults living with TB in sub-Saharan Africa (Chileshe & Bond, Citation2010; Sullivan et al., Citation2017; Samuelsen et al., Citation2013; Verhagen et al., Citation2010). This study fills a gap in the research by shedding light on the impact of TB on relationships, social interactions, and work. It also highlights the specific support needs identified by families themselves. The current system of care for rural and semi-urban families impacted by pediatric TB in Tanzania does not appear to meet the population’s needs. Thus, we summarise the systematic changes identified in this study as priorities to provide equitable care to all families []. The need for frequent visits for refills poses a major strain on families. While this may be alleviated for some in the future with the adoption of the four-month shorter course regimen for non-extensive TB disease (Turkova et al., Citation2022), future work should aim to eliminate completely the family burdens of travel for medication refills alone. Food and nutritional support were also offered as a solution. Although childhood malnutrition is common in our study regions, this concept has been reported by others receiving TB care in Tanzania (Kilale et al., Citation2022). Enhanced nutritional interventions for poor communities have even been recently modeled as highly cost-effective for preventing TB incidence and TB related mortality (Sinha et al., Citation2022).
Table 3. Key themes preventing comprehensive TB care generated from impacted families among a predominantly rural, low wealth population in a TB endemic region of Tanzania with suggested recommendations at the local, institutional and national levels.
An East African nation with a population of over 62 million people, the United Republic of Tanzania is one of 30 countries with the highest projected TB burden worldwide (World Health Organization, Citation2022c). In 2020, an estimated 133,000 people in Tanzania developed TB disease; among them, 22,000 (17%) children (United Republic of Tanzania TB dashboard, Citation2022). National surveys implemented between 2016 and 2020 show that nearly half of all people living with TB and their households faced catastrophic costs (World Health Organization, Citation2022). We found that despite having TB treatment provided free of charge, many families incurred additional medical-related costs during the diagnostic evaluation, and those affected families called attention to possible solutions such as creation of communal village-based emergency funds, direct cash transfers, or further cost mitigation by a universal health insurance policy. Encouragingly, community engagement strategies have proven particularly successful in implementing the country’s National Strategic Plan for TB and improving disease detection efforts and treatment outcomes (World Health Organization, Citation2022c). Therefore, infrastructure and past practices exist to enact new programs to support impacted families and caregivers of children with TB.
Limitations include interviews conducted solely in Kiswahili and therefore may not have reflected the lived experiences of families who are not conversant in the national language. Given the age range included in the parent study, this work does not specifically represent the views of younger children <4 years of age and their families. Since only four participants were recruited through the academic medical center in Moshi, data were insufficient to make semi-urban versus rural catchment area comparisons. Lastly, interviews may be affected by reflexivity and the inherent biases of the researchers. Despite these limitations, the data presented here provide the real-life experiences and reflections of children and their families affected by TB. Ongoing work locally includes home visits to enhance TB screening and research on unconditional cash transfers to facilitate overall engagement in TB care.
Conclusion
Addressing household- and system-level obstacles to TB treatment and care is crucial to improving health outcomes, as is the provision of person- and community-centered TB care (Furin et al., Citation2020; Pai & Furin, Citation2017; Zarocostas, Citation2019). Our findings suggest these programs should confer additional social protections to vulnerable families in the form of national health insurance to offset diagnostic evaluation costs, and direct cash transfer or other interventions to facilitate access to care, nutritional support, and to offset prohibitive transportation costs.
Ethics approval and consent to participate
The study was approved by institutional review boards at the National Institute of Medical Research in Tanzania and the University of Virginia. The larger cohort from which the participants were drawn is registered with clinicaltrials.gov, NCT05283967. Written consent was obtained from guardians and assent from all children 7–17 years of age prior to participation in the study.
Availability of data and materials
All data are available upon request from the corresponding author.
Competing interests
The Authors declare that there is no conflict of interest.
Consent for publication
All authors have given consent for publication.
Authors contributions
Study design by KPG, TAT, SKH, CV, EM. Study management by EM, HP, BM. Audio files were transcribed by CM, DA, PM, RG, SL, DK, MS and PM and translated to English by DA, PM, RG, SL, MS and PM. A codebook was developed by DA, KPG, MG, PM and SL. Analysis was performed by KPG, SKH, TAT. Funding obtained by SKH, CV, YX. Writing of manuscript by KPG, SKH, TAT. All authors read and approved the final manuscript.
Supplemental Material
Download PDF (369.6 KB)Acknowledgements
The study team expresses gratitude to all participating families of children impacted by tuberculosis.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Barter, D. M., Agboola, S. O., Murray, M. B., & Bärnighausen, T. (2012). Tuberculosis and poverty: the contribution of patient costs in sub-Saharan Africa – A systematic review. BMC Public Health, 12(1), https://doi.org/10.1186/1471-2458-12-980
- Brinda, E. M., Andrés, A. R., & Enemark, U. (2014). Correlates of out-of-pocket and catastrophic health expenditures in Tanzania: Results from a national household survey. BMC International Health and Human Rights, 14(5). https://doi.org/10.1186/1472-698X-14-5
- Chapman, A. L., Hadfield, M., & Chapman, C. J. (2015). Qualitative research in healthcare: An introduction to grounded theory using thematic analysis. Journal of the Royal College of Physicians of Edinburgh, 45(3), 201–205. https://doi.org/10.4997/jrcpe.2015.305
- Chileshe, M., & Bond, V. A. (2010). Barriers and outcomes: TB patients co-infected with HIV accessing antiretroviral therapy in rural Zambia. AIDS Care, 22(sup1), 51–59. https://doi.org/10.1080/09540121003617372
- Cypress, B. S. (2017). Rigor or reliability and validity in qualitative research. Dimensions of Critical Care Nursing, 36(4), 253–263. https://doi.org/10.1097/DCC.0000000000000253. PMID: 28570380.
- Das, M., Mathur, T., Ravi, S., Meneguim, A. C., Iyer, A., Mansoor, H., Kalon, S., Hossain, F. N., Acharya, S., Ferlazzo, G., Isaakidis, P., & Thakur, H. P. (2021). Challenging drug-resistant TB treatment journey for children, adolescents and their care-givers: A qualitative study. PLoS One, 16(3), e0248408. https://doi.org/10.1371/journal.pone.0248408
- Deterding, N. M., & Waters, M. C. (2021). Flexible coding of in-depth interviews: A twenty-first-century approach. Sociological Methods & Research, 50(2), 708–739. https://doi.org/10.1177/0049124118799377
- Foley, G., & Timonen, V. (2015). Using grounded theory method to capture and analyze health care experiences. Health Services Research, 50(4), 1195–1210. https://doi.org/10.1111/1475-6773.12275
- Furin, J., Loveday, M., Hlangu, S., Dickson-Hall, L., le Roux, S., Nicol, M., & Cox, H. (2020). “A very humiliating illness”: A qualitative study of patient-centered Care for Rifampicin-Resistant Tuberculosis in South Africa. BMC Public Health, 20(1), 1–11. https://doi.org/10.1186/s12889-019-8035-z
- George, L. S., Rakesh, P. S., Sunilkumar, M., Vijayakumar, K., Kunoor, A., & Kumar, V. A. (2021). TB patient support systems in Kerala: A qualitative analysis. Indian Journal of Tuberculosis, 68(1), 9–15. https://doi.org/10.1016/j.ijtb.2020.11.005
- Getahun, B., Wubie, M., Dejenu, G., & Manyazewal, T. (2016). Tuberculosis care strategies and their economic consequences for patients: The missing link to end tuberculosis. Infectious Diseases of Poverty, 5(1), 93. https://doi.org/10.1186/s40249-016-0187-9
- Glaser, B. G., & Strauss, A. L. (2017). The discovery of grounded theory: Strategies for qualitative research. Routledge.
- Guest, G., Bunce, A., & Johnson, L. (2006). How many interviews are enough? Field Methods, 18(1), 59–82. https://doi.org/10.1177/1525822X05279903
- Hennink, M. M., Kaiser, B. N., & Marconi, V. C. (2017). Code saturation versus meaning saturation. Qualitative Health Research, 27(4), 591–608. https://doi.org/10.1177/1049732316665344
- Kilale, A. M., Pantoja, A., Jani, B., Range, N., Ngowi, B. J., Makasi, C., … Ershova, J. (2022). Household solid waste management practices and perceptions among residents in the East Coast of Malaysia. BMC Public Health, 22(1), 1–10. https://doi.org/10.1186/s12889-021-12274-7
- Madan, J., Lönnroth, K., Laokri, S., & Squire, S. B. (2015). What can dissaving tell US about catastrophic costs? Linear and logistic regression analysis of the relationship between patient costs and financial coping strategies adopted by tuberculosis patients in Bangladesh, Tanzania and Bangalore, India. BMC Health Services Research, 15(1), https://doi.org/10.1186/s12913-015-1138-z
- Mhalu, G., Hella, J., Mhimbira, F., Said, K., Mosabi, T., Mlacha, Y. P., Schindler, C., Gagneux, S., Reither, K., de Hoogh, K., Weiss, M. G., Zemp, E., & Fenner, L. (2019). Pathways and associated costs of care in patients with confirmed and presumptive tuberculosis in Tanzania: A cross-sectional study. BMJ Open, 9(4), e025079. https://doi.org/10.1136/bmjopen-2018-025079
- Morse, J. M., Barrett, M., Mayan, M., Olson, K., & Spiers, J. (2002). Verification strategies for establishing reliability and validity in qualitative research. International Journal of Qualitative Methods, 1(2), 13–22. https://doi.org/10.1177/160940690200100202
- Mpagama, S. G., Ezekiel, M. J., Mbelele, P. M., Chongolo, A. M., Kibiki, G. S., de Guex, K. P., & Heysell, S. K. (2020). Gridlock from diagnosis to treatment of multidrug resistant tuberculosis (MDR-TB) in Tanzania: Patients’ perspectives from a focus group discussion. BMC Public Health, 20(1), 1–10. https://doi.org/10.1186/s12889-020-09774-3
- Nirmal, A., Kuzmik, A., Sznajder, K., Lengerich, E., Fredrick, N. B., Chen, M., Hwang, W., Patil, R., & Shaikh, B. (2022). ‘If not for this support, I would have left the treatment!': Qualitative study exploring the role of social support on medication adherence among pulmonary tuberculosis patients in Western India. Global Public Health, 17(9), 1945–1957. https://doi.org/10.1080/17441692.2021.1965182
- Njagi, P., Arsenijevic, J., & Groot, W. (2018). Understanding variations in catastrophic health expenditure, its underlying determinants and impoverishment in Sub-Saharan African countries: A scoping review. Systematic Reviews, 7(1), 136. https://doi.org/10.1186/s13643-018-0799-1
- Pai, M., & Furin, J. (2017). Tuberculosis innovations mean little if they cannot save lives. eLife, 6, e25956. https://doi.org/10.7554/eLife.25956
- Paz-Soldán, V. A., Alban, R. E., Jones, C. D., & Oberhelman, R. A. (2013). The provision of and need for social support among adult and pediatric patients with tuberculosis in Lima, Peru: A qualitative study. BMC Health Services Research, 13(1), 290. https://doi.org/10.1186/1472-6963-13-290
- Prasanna, T., Jeyashree, K., Chinnakali, P., Bahurupi, Y., Vasudevan, K., & Das, M. (2018). Catastrophic costs of tuberculosis care: A mixed methods study from Puducherry, India. Global Health Action, 11(1), 1477493. https://doi.org/10.1080/16549716.2018.1477493
- Samuelsen, H., Tersbøl, B. P., & Mbuyita, S. S. (2013). Do health systems delay the treatment of poor children? A qualitative study of child deaths in rural Tanzania. BMC Health Services Research, 13(1), 1–10. https://doi.org/10.1186/1472-6963-13-67
- Sinha, P., Lakshminarayanan, S. L., Cintron, C., Narasimhan, P. B., Locks, L. M., Kulatilaka, N., … Hochberg, N. S. (2022). Nutritional supplementation would be cost-effective for reducing tuberculosis incidence and mortality in India: The Ration Optimization to Impede Tuberculosis (ROTI-TB) model. Clinical Infectious Diseases, 75(4), 577–585. https://doi.org/10.1093/cid/ciab1033
- Small, M. L. (2009). `How many cases do I need?' need?’ On science and the logic of case selection in field-based research. Ethnography, 10(1), 5–38. https://doi.org/10.1177/1466138108099586
- Stracker, N., Hanrahan, C., Mmolawa, L., Nonyane, B., Tampi, R., Tucker, A., West, N., Lebina, L., Martinson, N., & Dowdy, D. (2019). Risk factors for catastrophic costs associated with tuberculosis in rural South Africa. The International Journal of Tuberculosis and Lung Disease, 23(6), 756–763. https://doi.org/10.5588/ijtld.18.0519
- Sullivan, B. J., Esmaili, B. E., & Cunningham, C. K. (2017). Barriers to initiating tuberculosis treatment in sub-Saharan Africa: A systematic review focused on children and youth. Global Health Action, 10(1), 1290317. https://doi.org/10.1080/16549716.2017.1290317
- Tanimura, T., Jaramillo, E., Weil, D., Raviglione, M., & Lönnroth, K. (2014). Financial burden for tuberculosis patients in low- and middle-income countries: A systematic review. European Respiratory Journal, 43(6), 1763–1775. https://doi.org/10.1183/09031936.00193413
- Tong, A., Sainsbury, P., & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357. https://doi.org/10.1093/intqhc/mzm042
- Turkova, A., Wills, G. H., Wobudeya, E., Chabala, C., Palmer, M., Kinikar, A., … Crook, A. M. (2022). Shorter treatment for nonsevere tuberculosis in African and Indian children. New England Journal of Medicine, 386(10), 911–922. https://doi.org/10.1056/NEJMoa2104535
- Ukwaja, K. N., Alobu, I., Abimbola, S., & Hopewell, P. C. (2013a). Household catastrophic payments for tuberculosis care in Nigeria: Incidence, determinants, and policy implications for universal health coverage. Infectious Diseases of Poverty, 2(1), 21. https://doi.org/10.1186/2049-9957-2-21
- Ukwaja, K. N., Alobu, I., Lgwenyi, C., & Hopewell, P. C. (2013b). The high cost of free tuberculosis services: Patient and household costs associated with tuberculosis care in Ebonyi State, Nigeria. PloS One, 8(8), e73134. https://doi.org/10.1371/journal.pone.0073134
- United Republic of Tanzania TB dashboard. (2022). Retrieved February 1, 2022, from Stoptb.org website: https://www.stoptb.org/static_pages/TZA_Dashboard.html.
- Verhagen, L. M., Kapinga, R., & van Rosmalen-Nooijens, K. A. W. L. (2010). Factors underlying diagnostic delay in tuberculosis patients in a rural area in Tanzania: A qualitative approach. Infection, 38(6), 433–446. https://doi.org/10.1007/s15010-010-0051-y
- Wen, S., Yin, J., & Sun, Q. (2020). Impacts of social support on the treatment outcomes of drug-resistant tuberculosis: A systematic review and meta-analysis. BMJ Open, 10(10), e036985. https://doi.org/10.1136/bmjopen-2020-036985
- World Health Organization. (2022). Retrieved February 1, 2022, from who.int website: https://cdn.who.int/media/docs/default-source/documents/tuberculosis/engage-tb-tanzania-case-study-2cfe6b1bf-8efd-481b-b659-e2a889e90b97.pdf?sfvrsn=f8c2028a_1&download=true.
- World Health Organization (a). (2022). Retrieved February 1, 2022, from who.int website: https://www.who.int/tb/publications/patient_cost_surveys/en/.
- World Health Organization (b).. (2022). The end TB strategy. Retrieved March 16, 2022, from who.int website: https://www.who.int/teams/global-tuberculosis-programme/the-end-tb-strategy.
- World Health Organization (c). (2022). Global tuberculosis report 2021. Retrieved February 1, 2022, from who.int website: https://www.who.int/publications/i/item/9789240037021.
- Zarocostas, J. (2019). Nandita Venkatesan: A voice of hope for tuberculosis survivors. The Lancet, 393(10178), 1277. https://doi.org/10.1016/S0140-6736(19)30582-3