ABSTRACT
Mobility, access to transport and healthcare play a crucial part in healthy ageing. However, these often posechallenges for older adults in the global South. This study applies the three concepts of ‘motility’ (access, competence and appropriation), to explore transport inequalities and barriers to access healthcare services for older adults in Bengaluru, India. The paper draws on interviews with sixty adults, aged 50 years and over, residing in urban Bengaluru. A semi-structured in-depth interview guide was employed to explore the transport inequalities. Applying thematic analysis, we present the mobility and transport barriers to access healthcare. Restricted access to healthcare services due to unavailable and unaffordable transportation resulted in missed appointments, delayed care and deterioration of health conditions. To cope with the barriers, older adults often visited less specialised clinics for regular check-ups and those with financial constraints resorted to self-medication. These actions further deteriorated health and led to adverse health outcomes. Our findings suggest that integrated health and transport policies must be designed to ensure equitable access to transportation services. Enabling older adults to have more independent lives and improve access to preventive healthcare is essential for better health outcomes.
Background
As populations age, action must be taken to ensure that people can age healthily and enjoy a good quality of life in later life (United Nations, Citation2017). Public transportation ensures access to essential services and helps older adults stay socially connected to their communities. With limited transportation options older people have to forego some of their travel needs to make only essential trips (Luiu & Tight, Citation2021; Meijering, Citation2021). Therefore, it is important to provide sustainable transportation services, which are inclusive and enable participation in daily activities. In line with that, the sustainable development goal (SDG) 11, intends to make cities and human settlements inclusive, safe, resilient and sustainable, with the target of SDG 11.2 specifically catering to older adults, women, children and people with disabilities (United Nations, Citation2021).
As most (older) people do not live closer to healthcare facilities, using transportation to access them is crucial. In this paper, access to healthcare refers to the physical access to a healthcare facility for getting treatment. For older adults living in the urban periphery [‘urban periphery’ refers to the edge of the city farthest from the centre, but technically a part of the city (Geneletti et al., Citation2017)], availability of transportation may be scarce (Novek & Menec, Citation2014) and a lack of integrated public transport (Aziz et al., Citation2018) or not having access to alternative transport modes can result in expensive and exhausting trips involving multiple modes of transport (Wallace et al., Citation2005; Wolfe et al., Citation2020). Such inequalities in accessing reliable transportation services can lead to missed appointments (Ramlucken & Sibiya, Citation2018), delayed treatment resulting in worsening health conditions and hospital admissions. Often, healthcare expenditures in countries such as India are several times higher than their monthly income, resulting in catastrophic health expenditures (Bhan et al., Citation2017; Syed et al., Citation2013; Wolfe et al., Citation2020). The inability to access timely medical attention could lead to significant stress, anxiety and psychological burden for older adults (Hadley Strout et al., Citation2016). The lack of transportation, poverty and family support may force older adults to depend on traditional healers, unlicensed medical practitioners and over-the-counter medicines (HelpAge International, Citation2002; Kullanit & Taneepanichskul, Citation2018). Such inadequate treatment options could lead to poor health outcomes.
The World Health Organisation’s (WHO) age-friendly cities framework includes transportation as one of the key domains, enabling mobility of older adults (World Health Organization, Citation2021). However, public transportation in India is reported to be inadequate for older adults (Tsang, Citation2012; Villena-Sanchez & Boschmann, Citation2022). Inappropriate behaviour of transport personnel and passengers, gender discrimination and ageism, affect older adults’ access to essential services resulting in social exclusion and widening transport inequalities (Jahangir et al., Citation2022). Having accessible and inclusive transportation modes will enable older persons to carry out day-to-day activities independently, improving healthcare accessibility and overall health (Musselwhite, Citation2022).
The current study was undertaken in Bengaluru, which is the capital city of Karnataka, India. It is the third most populous city in India and the fifth most populous urban area, larger than many European countries. The current estimated population of Bengaluru is about 13,607,800 (World Population Review, Citation2023). This has made it challenging for the urban local bodies to provide adequate infrastructure. Consequently, the public transport system has not been able to keep up with increasing transportation demand (Knight Frank India Private Limited, Citation2021; Nayka & Sridhar, Citation2019). Likewise, there are gaps in the healthcare system, which is provided by a mix of public (government) and private hospitals. Healthcare at public hospitals is free of cost for individuals from very low-income groups (Planning Commission, Citation2013). However, a shortage of staff and, a lack of medicines and diagnostic services push many to use the services from private hospitals, which are expensive, or to postpone their visit to the hospital (Yellapa et al., Citation2017). The unavailability of affordable and quality healthcare services in their locality requires people to travel long distances in a difficult and often disjointed transport system. A scoping review in Southeast Asia identified barriers to accessing healthcare from the service providers’ point of view such as lack of availability of skilled healthcare staff, geographic location of the facility, operating hours of the healthcare facilities, expensive healthcare services and perceptions of older adults about their health condition and healthcare services (Mohd Rosnu et al., Citation2022). However, the transport-related accessibility of an individual has not been explored in the South Asian context for older adults’ access to healthcare services. Hence, this study was conducted to understand the transportation barriers in Bengaluru, how participant characteristics such as gender, income, disability and geographical location interacted with transportation barriers that limited older adults’ access to healthcare and how they negotiated access to healthcare services.
Transport as a missing link to healthcare access
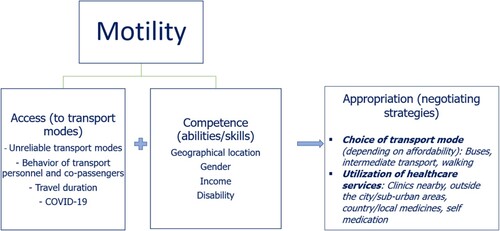
In developed and a few developing countries, including India, research on ‘access to healthcare’ generally focuses on availability and affordability of services, geographical accessibility, where the locations of service providers and users were factors influencing access to healthcare (Jacobs et al., Citation2012; Kyriopoulos et al., Citation2014). In this paper, we use the concept of motility, proposed by Kaufmann and colleagues (2004) to understand an individual’s mobility potential and the ability she/he has to transform that potential to travel. Motility is defined as ‘how an individual or group takes possession of the realm of possibilities for mobility and builds on it to develop personal projects’ (Flamm & Kaufmann, Citation2006; Kaufmann et al., Citation2004). It includes (i) access, (ii) competence and (iii) appropriation. ‘Access’ is the range of options available based on place, time, and contextual features (e.g. personal vehicles, public transport). ‘Competence’ relates to acquired and organisation skills and abilities of an individual to plan activities. ‘Appropriation’ refers to what an individual does with access and skills. Motility (potential mobility) when combined with movement (actual mobility) has been shown to influence the well-being of older adults (Cuignet et al., Citation2020). The literature indicates that being mobile could help older adults access healthcare services, which would enable better health outcomes (de Vos et al., Citation2013). For example, an older adult who is able to access information about the timings and availability of transport modes can plan travel at her/his convenience. This will make them feel more independent and provide greater travel opportunities, resulting in greater well-being. However, there could be situations in which older adults are unable to use different transport modes due to factors such as physical limitations, gender and financial constraints. Rurality, poverty and poor transportation are associated with limited access to healthcare for older adults in the USA (Cohen, Citation2021). Similarly, in India, age and gender influenced older adults’ eye care-seeking behaviour (Barman & Mishra, Citation2020).
The key concepts that inform the conceptual framework in this paper are accessibility to transport services, the ability of an individual to access transport services and negotiating strategies to access healthcare, which are adapted from the main concept of ‘Motility’. The three elements of ‘Motility’ have not been explored from the perspective of older adults with respect to accessing healthcare facilities in the Asian context. Therefore, in this study, we explore the barriers faced by older adults when accessing different modes of transport and examine how various factors, such as gender, disability, income and geographical location interact with their ability to access transport modes. Lastly, we identify the strategies used by older adults to overcome the existing barriers to reach healthcare facilities.
Methodology
Operational definitions
Disability in this paper refers to physical impairments that substantially limit the activities and participation of an individual in the community (Rohwerder, Citation2015). In our research, public transport refers to bus and metro services. Intermediate public transport sometimes known as paratransit, refers to ‘road vehicles used on hire for flexible passenger transportation, which do not follow a fixed time schedule. They may or may not follow a fixed route’ (Ponnuswamy & Victor, Citation2012) [e.g. autorickshaw and cab (regular/app-based)]. Personal vehicles refer to motorised two- or four-wheelers, e.g. privately owned motorcycles or cars.
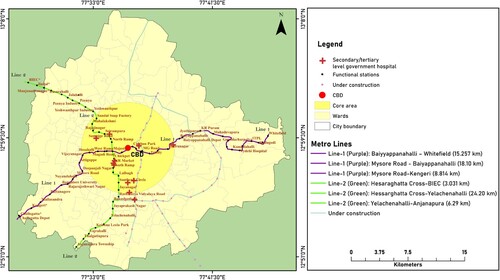
Setting: The study was conducted in Bengaluru, a rapidly growing metropolitan city in the southern part of India. depicts the study site indicating the core and peripheral areas, metro routes and location of the secondary/tertiary level care public health care settings.
Figure 1. Map of Bengaluru indicating the study sites, location of public healthcare setting and metro routes.
Participant profile: To capture the diverse experiences, we tried to include older adults (>50 years) from different socio-economic statuses, residential locations, employment statuses, living arrangements and religions. Fifty years and above was considered since many working-class people in the pre-retirement stage, begin to make changes with respect to their occupations and mobility behaviour based on their health conditions (Bloom et al., Citation2021). The socio-demographic and economic characteristics of participants are given in . A detailed participant profile is given in Appendix 1.
Table 1. Participant characteristics.
Participants were recruited initially through the researcher’s contacts and with the help of Non-Governmental Organisations (NGOs) such as HelpAge India and Hasirudala, which work with older adults and low-income garbage collectors, and thereafter by snowballing. The NGOs helped low-income older adults with healthcare check-ups and other needs during the COVID-19 pandemic. They introduced the researcher to older adults (over the telephone), thereafter the researcher contacted the older adult at a convenient time set by them. They were given a full description of the research, allowed to ask questions and were asked for their willingness to participate if they were eligible. The interview date was scheduled after obtaining consent.
Data collection: Data collection was carried out between June and December 2020 by the lead author. A semi-structured in-depth interview guide (see supplementary file) was developed and refined to improve comprehension after conducting pilot interviews (e.g. as the interviews were conducted during the COVID-19 pandemic, for questions on their activities outside the house the researcher had to inform participants to share their experiences before the pandemic. This applied to most questions because the participants were inclined to speak about the lockdown that was imposed). The COVID-19 pandemic halted the process of in-person interviews completely and hence researchers across the globe had to shift to remote methods of data collection (Lupton & Lewis, Citation2021, Citation2022). Among the 64 participants approached, four of them did not respond on the scheduled interview date after agreeing to participate. Sixty participants consented and participated in the study. Telephone interviews were recorded using the mobile phone’s in-built voice recorder after obtaining consent from the participant. Notes were taken during the interview. Interviews ranged between 40 and 90 min. To capture the diverse experiences of older adults across different categories such as geographical location, socio-economic classes, gender and physical abilities, we interviewed participants until we reached data saturation at the 60th interview.
Data management: Interviews were conducted in English, Kannada and Tamil languages. Recorded interviews were transcribed and translated into English. The data were analysed using NVIVO version 12. The coding of interviews was done by the lead author in consultation with one of the co-authors, who is also the principal investigator of the project. A two-stage coding cycle was undertaken. Initially, deductive codes were developed based on the conceptual framework and inductive codes from the data themselves (Hennink et al., Citation2020). Key concepts from the conceptual framework are availability, ability to access transport, negotiating strategy and socio-demographic factors such as income, gender, geographical location and disability which are interlinked with the other concepts. The inductive codes were the behaviour of transport personnel, average distance to the hospital, travel duration and the impact of COVID-19. In the second cycle, different codes with similar attributes were grouped under code families to develop themes and sub-themes related to transport barriers that limited the uptake of transport services and the negotiating strategies developed by older adults to access healthcare (see ).
Table 2. List of codes.
Results
Our findings reveal that different transport modes were available for older adults such as public, intermediate and personal transport. However, they were often unable to access their preferred mode of transport. In section 1, we explore the transport barriers faced by older adults, followed by section 2 highlighting the personal characteristics of older adults that affect their ability to use the available transport modes and section 3 covers the strategies used by older adults to overcome the transport system and personal barriers to negotiate access to healthcare. depicts the barriers to accessing transport modes to reach healthcare facilities.
1. Barriers limiting uptake of transport services to access healthcare
This section reveals that the access to different transport services to reach healthcare facilities depended on the availability of transport services, travel duration behaviour of transport personnel and passengers and the COVID-19 pandemic.
1.1 Availability/unreliable transport modes
Participants reported that they often had to wait for 15–60 min, sometimes even longer, to catch a bus to reach the healthcare facility. Crowded buses during peak hours were difficult to board, and the reduced frequency of services during the afternoon increased their waiting time. Lack of information about bus schedules resulted in uncertainty, making it difficult for them to plan hospital visits. Therefore, public transport was considered unreliable in the case of hospital visits for acute care conditions.
Particularly, those who lived in the urban periphery faced difficulty accessing timely bus facilities to go to the hospital, thus increasing their travel time to the hospital and back home.
Earlier I used to go in bus to buy medicines. Now I don't even do that … It is nearly 20 kilometres from home … It would take six hours easily. We won't get buses on time; we have to wait. (Ahmed, 78, male)
Once we had to go for my eye surgery to the hospital. We had the appointment at a particular time. So based on that … I was booking for the cab. But both the cabs cancelled, and they did not come. (Channesh, 62, male)
Actually, I do not do the booking. I am not used to it (booking cabs via apps). My wife does it, so we go in it. I don't know how to do all that. I don't even use Android mobile phone; I use normal simple phone only. (Venkatesh, 60, male)
I have to take an auto and go to Nayandahalli metro station and from there I take metro and reach, again I will take an auto to reach the hospital. (Channesh, 62, male)
1.2 Travel duration
Reaching the healthcare facility involved using multiple modes of transport that increased the travel time. If they had to use public transport, participants had to walk to the bus or metro station, depending on family members or intermediate transport. The walking distance to the bus stop/metro rail station as reported by participants ranged between 0.5 and 2 kilometres.
I use auto or bus to go to metro station. From there to Vijayanagar metro station, if I get down it (the clinic) is close by only. Some half a kilometre. (Ravi, 82, male)
… my son used to drop me till the Byppanahalli metro station and from there I used to take the metro and get down at Majestic … I used to take two buses and go till MG Road (for homeopathy clinic) … and while returning I used to take a bus from there till Shivaji Nagar and then another bus from there to Kammanahalli. (Sarah, 63, female)
1.3 Behaviour of transport personnel and passengers
Rude and disrespectful behaviour and ageist remarks made by transport personnel and co-passengers, insufficient time to board and sit in the bus, not stopping at the bus stop or close to the kerb, and climbing the high steps, discouraged older people from using buses.
I get in and stand all the while. There is seating arrangement for senior citizens, but they do not give place … When I am tired it is usually very difficult to stand. What to do? Conductors can help but they won't. (Sandhya, 73, female)
They always ask, so always we have argument, especially when we are outside city then they will not put meter. (Anupamma, 66, female)
Transport staff are not very well trained. They should be sensitised … Their transport staff should be trained sufficiently to handle various section of the population. (Rathnakar, 58, female)
1.4 COVID-19 pandemic and increasing inequalities
The COVID-19 pandemic added to the challenges of bus users and brought to light the already existing inequalities that older adults face in accessing healthcare due to transportation barriers. In areas with very limited bus services before the pandemic, there were absolutely no buses available once restrictions came in, which resulted in missing their routine check-ups.
He was supposed to go in April. Because of corona he could not go … doctor said you don’t come, you continue the same medicines. Only thing he is not able to take the diagnostic tests. (Suganti, 63, female)
Now because of covid metro is also not working so if we have to go to hospital, we will go here only nearby for the routine diabetes follow up check-up. My son will take me and go. Auto will be there but … I already told right these auto drivers they charge as they want. (Channesh, 62, male)
About going to hospital, I have not been able to consult the doctor for this leg pain … It is very painful sometimes and I am unable to sleep. (John, 65, male)
2. Ability to access transport modes
The inability of older adults to afford different transport modes, their poor physical health, gender (read women) and living on the periphery of the city increased inequalities in accessing transport modes. Those on a lower income usually reside in the urban periphery, as the rent/lease is affordable. However, this affected their access to transport to travel to essential services such as healthcare. A 66-year-old participant, Ratna, living with her husband (unwell) and son (not working), resides in the urban periphery due to affordable house rent and closeness to the workplace so that she can walk to work. She works as an English teacher at the nearby college where she is paid INR 150 (approximately US$ 2)/ hour. At present, she has no income because the college is closed and is financially supported by her well-wishers for basic needs. She suffers from diabetes mellitus and also underwent surgery for hernia during the COVID-19 pandemic. She must go to the city to access healthcare services for herself and her husband who is also suffering from a chronic illness. She faces difficulty in accessing buses near her house. She cannot take the auto everywhere because she has to save some money to buy medicines. She mostly walks to the bus stop near her house and if the bus is not available, sometimes takes an auto to the next bus stop near the main junction and takes the bus. Since her husband cannot travel, she must visit his previous workplace to claim partial medical insurance to pay off his medical bills. This process is very exhausting due to the lack of direct public transport and adds to the financial burden for her at this age when she herself has health issues.
Rent is less and the lease is also less in this area. … But buses are not very regular … It’s very difficult to get a bus here … and if I don't get a bus, I take an auto from my area … 30 rupees (less than US$ 1) they take and from there I always take bus. And I walk everywhere you know. Expensive everything.
Being a lady, I did not face a problem in the daytime … Evening and night only … I used to avoid coming late … sometimes when it got late, I have felt … men come and sit in ladies’ seats also, it is not good. At such times I don’t feel very secure in the bus. (Shalini, 55, female)
Not prefer to walk. I have to walk. For every little thing I can't, my medical expense is more … So, I have to think, whether to spend on auto for little distance or let me walk slowly. (Ratna, 66, female)
3. Negotiating strategies to access healthcare services
This section uncovers how older adults adapted to existing challenges and developed coping strategies for accessing healthcare services. The appropriation of a transport mode to access healthcare services was influenced by healthcare needs (emergency or routine check-ups), distance to healthcare facilities and financial status. Participants visited the doctor once or twice a month, whereas a few visited once a year for a regular check-up. For chronic conditions (e.g. diabetes) they preferred visiting a clinic nearby to avoid navigating long distances through chaotic traffic in the city. They could not spend too much time and money commuting to a bigger health facility unless it was necessary.
Nazeema, a 60-year-old tailor who lives with her family, walks to the mobile clinic arranged by an NGO, which provides weekly check-ups and free medications. Due to financial constraints, she walks to the clinic to access the free medical services.
I walk and go … I can take auto but then to take auto I need money also right … money problem is there and so I go by walk only and get medicines and come.
For homoeopathy, I had to change three buses. I had to go to Banashankari and from there had to go to Jayanagar … But have to change three buses.
I use Uber or Ola. It is convenient when we have to go to hospitals or any other occasions where time is a factor, we can’t keep waiting for bus which is not frequent here … I feel cab is better.
We have no other point public transport to avail for health care facility … Most of the times it is in case of emergency. You always go with either … a hired cab or with personal transportation.
Buses are available, but the timings are not proper … So only 4–5 of us came together and hired a car and we went there … If there was bus till there, then I would have taken bus obviously. Car is more costly right. Bus charges in BTS (Bangalore Transport Service) will be less only. (Nagesh, 68, male)
I have one allergy and I had wounds all over. Some good person got me a medicine it has come down. I have visited so many places, hospitals, medicines for that. It has not cured, since last 6–7 months it has reduced. They have given me country medicine. With use it has come down. (Nirmala, 76, female)
And one of my friends has a medical store … I was working as the bus-body builder, even he worked with me at that time. Later he opened the medical store … if I go to them and ask any medicines for any problem that I have then they will give me medicines for that. (Sreenath, 60, male)
See for me itself 1 tablet is costly, it really used to help me to control my diabetes … because it is costly, from three months I stopped. (Rebecca, 65, female)
Discussion and implications
In this paper, the concept of ‘motility’ aids in discussing the challenges older adults face in gaining access to transport modes to visit healthcare facilities, the skills (abilities) they have to use the available modes and strategies (appropriation) to overcome these challenges. It was found that most older adults accessed healthcare facilities to access preventive healthcare services. We observed that access to transport modes to reach healthcare facilities was not the same for all older adults.
Older adults wanted to use public transport but could not rely on it due to the unavailability and uncertainty of services. In middle-income groups, accessing healthcare by personal vehicle or intermediate transport was not a financial burden. One of the reasons was that some of the older adults in this group were insured for healthcare. They also had a regular pension which aided in hiring transport services or a driver. Low-income older adults, with no health insurance, chose bus services with reasonable fares, used multiple modes of transport or resorted to delaying hospital visits. This highlights the disparities in transport access among different income groups while accessing healthcare services. Similarly, in African and high-income countries, studies examined how socio-economic factors influenced older adults’ choices of transport to healthcare (de Witte et al., Citation2013; Ipingbemi, Citation2010; Oduro Appiah et al., Citation2020; Varela et al., Citation2019). Restricted access to healthcare due to unaffordable and unavailable transport modes can result in delays in seeking care and deterioration of existing health conditions (Hadley Strout et al., Citation2016).
Older adults with lower incomes lived in the urban periphery for affordable housing. Public transport was scarce in these areas, pushing them to depend on expensive intermediate transport delaying timely access to health care. Similar findings were reported in other high-income and low-income countries (Kotavaara et al., Citation2021; Varela et al., Citation2019). Therefore, it is important to strengthen public transport services to the urban peripheries and provide intermediate transport with subsidised fares to areas where public transport cannot reach. Barriers to accessing metro rail services across income groups included limited connectivity to all locations and higher fares compared to other public transport modes. Evidence from the Global North has shown that providing free rides and fare concessions in public transport increased the utilisation of public transport among older adults (Mah & Mitra, Citation2017; Reinhard et al., Citation2018). Fare concessions for older adults in buses already exist in Bengaluru; however, it is recommended that this provision be explored for the metro rail services. Furthermore, this study highlighted that the safety of older women was not sufficient in any transportation modes after it was dark. Even in high-income countries where public transport could be easily accessed, older women found it difficult to participate in social life due to fear of crime while using public transport (Nordbakke, Citation2013). Our findings recommend the need to improve safety measures for older women while accessing transport modes.
The lockdown, which was imposed to curb the spread of COVID-19 infection, resulted in a lack of transportation services (Ahmed et al., Citation2020; Geldsetzer et al., Citation2020). Although the government issued directives for tele-consultation facilities across different hospitals, it was not very effective for older adults from lower income groups due to the lack of internet/technology and the ability to use it (Hoffer-Hawlik et al., Citation2020; Seifert, Citation2020). Therefore, during such emergencies, healthcare should be brought to the community, especially for those living in the urban periphery and low-income groups.
This study also explored the strategies used by older adults to adapt to the transport inequalities they faced to access healthcare services. They preferred facilities nearby for preventive care services to avoid commuting through congested roads. Since a comprehensive care was not available at the private clinic, they had to access a bigger healthcare facility for emergency conditions. Hence, they had to depend on personal or intermediate modes of transport. However, this was not affordable for older adults from lower-income groups. Additionally, an increased distance and travel duration to healthcare facilities resulted in poor health outcomes (e.g. delay in follow-up visits) (Kelly et al., Citation2016). Due to the aforementioned transportation barriers, older adults opted for self-medications or local/country medicines, which they perceived to be less expensive. This could lead to more complications if the underlying ailment was not diagnosed on time resulting in delayed diagnosis and financial burden for further treatment. Our findings were congruent with a study conducted in the US, which indicated that individuals from lower-income groups experienced delays in receiving care due to transportation barriers (Acquah et al., Citation2022). Therefore, it is vital to have efficient transport services to reach healthcare facilities in difficult-to-reach areas.
This study contributes to the literature by providing an understanding of how transportation barriers have impeded older adults’ access to healthcare and how they have been able to negotiate access to healthcare in the face of transportation barriers. It focuses on the multi-dimensional aspects of transportation services, such as availability, affordability and acceptability, which have not been explored in-depth by previous literature in the South Asian context. The findings from this study should be interpreted with care due to the limitation that participants were geographically located in different zones of Bengaluru, hence all participants may not have faced issues to access transportation.
Conclusion
Older adults primarily visited healthcare facilities for preventive care services. Routine hospital visits are important for them to lead healthy lives. It is important to ensure they can access transport modes at their convenience to reach the hospital and avail of necessary services. The fact that they do not want to use public transport indicates that the transportation system is not suitable for them. Public transport connectivity to the urban periphery is very sparse or not available making it difficult for them to access health services. This draws our attention towards the need for other options, such as affordable intermediate public transport in these locations, which will provide door-to-door services. Providing equitable access to public transport will help older adults be independent and make use of preventive healthcare services for better health outcomes.
Ethics approval and consent to participate
All procedures were performed in compliance with relevant laws and institutional guidelines and the appropriate institutional committee(s) have approved them. Ethical approval was obtained from Utrecht University (Geo-L-19294) and the Institute for Social and Economic Change (DPA/Ethic.Com/2020/343). We obtained informed consent from the participants before beginning the interview. We used pseudonyms for the names of participants in the text.
Availability of data and materials
Data will be available with the corresponding author on request.
Supplemental Material
Download MS Word (17 KB)Supplemental Material
Download PDF (490 KB)Supplemental Material
Download MS Word (31.3 KB)Acknowledgements
The authors would like to acknowledge the financial support from the funding agency Dutch Research Council (NWO W 07.30318.003) and Utrecht University, the Netherlands, to carry out the research activities. We would also like to thank all the NGOs (who were the gatekeepers in the community) and the participants who took part in the research.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Acquah, I., Hagan, K., Valero-Elizondo, J., Javed, Z., Butt, S. A., Mahajan, S., Taha, M. B., Hyder, A. A., Mossialos, E., Cainzos-Achirica, M., & Nasir, K. (2022). Delayed medical care due to transportation barriers among adults with atherosclerotic cardiovascular disease. American Heart Journal, 245, 60–69. https://doi.org/10.1016/j.ahj.2021.11.019
- Ahmed, S. A. K. S., Ajisola, M., Azeem, K., Bakibinga, P., Chen, Y.-F., Choudhury, N. N., Fayehun, O., Griffiths, F., Harris, B., Kibe, P., Lilford, R. J., Omigbodun, A., Rizvi, N., Sartori, J., Smith, S., Watson, S. I., Wilson, R., Yeboah, G., Aujla, N., … Yusuf, R. (2020). Impact of the societal response to COVID-19 on access to healthcare for non-COVID-19 health issues in slum communities of Bangladesh, Kenya, Nigeria and Pakistan: Results of pre-COVID and COVID-19 lockdown stakeholder engagements. BMJ Global Health, 5(8). https://doi.org/10.1136/bmjgh-2020-003042
- Aziz, A., Nawaz, M. S., Nadeem, M., & Afzal, L. (2018). Examining suitability of the integrated public transport system: A case study of lahore. Transportation Research Part A: Policy and Practice, 117, 13–25. https://doi.org/10.1016/j.tra.2018.08.003
- Barman, D., & Mishra, M. (2020). How does eye care seeking behaviour change with increasing age and visual impairment? Intersectional analysis of older adults in the Indian Sundarbans. BMC Geriatrics, 20(1), 71. https://doi.org/10.1186/s12877-020-1438-y
- Bhan, N., Madhira, P., Muralidharan, A., Kulkarni, B., Murthy, G., Basu, S., & Kinra, S. (2017). Health needs, access to healthcare, and perceptions of ageing in an urbanizing community in India: A qualitative study. BMC Geriatrics, 17(1). https://doi.org/10.1186/s12877-017-0544-y
- Bloom, D. E., Sekher, T. V., & Lee, J. (2021). Longitudinal aging study in India (LASI): New data resources for addressing aging in India. Nature Aging. https://doi.org/10.1038/s43587-021-00155-y
- Cohen, A. (2021). The challenges of intersectionality in the lives of older adults living in rural areas with limited financial resources. Gerontology & Geriatric Medicine, 7. https://doi.org/10.1177/23337214211009363
- Cuignet, T., Perchoux, C., Caruso, G., Klein, O., Klein, S., Chaix, B., Kestens, Y., & Gerber, P. (2020). Mobility among older adults: Deconstructing the effects of motility and movement on wellbeing. Urban Studies, 57(2). https://doi.org/10.1177/0042098019852033
- de Vos, J., Schwanen, T., van Acker, V., & Witlox, F. (2013). Travel and subjective well-being: A focus on findings, methods and future research needs. Transport Reviews, 33(4). https://doi.org/10.1080/01441647.2013.815665
- de Witte, A., Hollevoet, J., Dobruszkes, F., Hubert, M., & Macharis, C. (2013). Linking modal choice to motility: A comprehensive review. Transportation Research Part A: Policy and Practice, 49. https://doi.org/10.1016/j.tra.2013.01.009
- Flamm, M., & Kaufmann, V. (2006). Operationalising the concept of motility: A qualitative study. Mobilities, 1(2). https://doi.org/10.1080/17450100600726563
- Geldsetzer, P., Reinmuth, M., Ouma, P. O., Lautenbach, S., Okiro, E. A., Bärnighausen, T., & Zipf, A. (2020). Mapping physical access to health care for older adults in sub-saharan Africa and implications for the COVID-19 response: A cross-sectional analysis. The Lancet Healthy Longevity, 1(1), e32–e42. https://doi.org/10.1016/S2666-7568(20)30010-6
- Geneletti, D., La Rosa, D., Spyra, M., & Cortinovis, C. (2017). A review of approaches and challenges for sustainable planning in urban peripheries. Landscape and Urban Planning, 165, 231–243. https://doi.org/10.1016/j.landurbplan.2017.01.013
- Hadley Strout, E., Fox, L., Castro, A., Haroun, P., Leavitt, B., Ross, C., Sayan, M., Delaney, T., Platzer, A., Hutchins, J., & Carney, J. K. (2016). Access to transportation for chittenden county Vermont older adults. Aging Clinical and Experimental Research, 28(4), 769–774. https://doi.org/10.1007/s40520-015-0476-3
- HelpAge International. (2002). Gender and transport for older people. HelpAge International. https://www.helpage.org/silo/files/gender-and-transport-for-older-people.pdf.
- Hennink, M., Hutter, I., & Bailey, A. (2020). Qualitative research methods. SAGE Publications Limited.
- Hoffer-Hawlik, M. A., Moran, A. E., Burka, D., Kaur, P., Cai, J., Frieden, T. R., & Gupta, R. (2020). Leveraging telemedicine for chronic disease management in low- and middle-income countries during COVID-19. Global Heart, 15(1). https://doi.org/10.5334/gh.852
- Ipingbemi, O. (2010). Travel characteristics and mobility constraints of the elderly in Ibadan, Nigeria. Journal of Transport Geography, 18(2). https://doi.org/10.1016/j.jtrangeo.2009.05.011
- Jacobs, B., Ir, P., Bigdeli, M., Annear, P. L., & van Damme, W. (2012). Addressing access barriers to health services: An analytical framework for selecting appropriate interventions in low-income Asian countries. Health Policy and Planning, 27(4), 288–300. https://doi.org/10.1093/heapol/czr038
- Jahangir, S., Bailey, A., Hasan, M. U., Hossain, S., Helbich, M., & Hyde, M. (2022). “When I need to travel, I feel feverish”: Everyday experiences of transport inequalities among older adults in Dhaka, Bangladesh. The Gerontologist, 62(4), 493–503. https://doi.org/10.1093/geront/gnab103
- Kaufmann, V., Bergman, M. M., & Joye, D. (2004). Motility: mobility as capital. International Journal of Urban and Regional Research, 28(4). https://doi.org/10.1111/j.0309-1317.2004.00549.x
- Kelly, C., Hulme, C., Farragher, T., & Clarke, G. (2016). Are differences in travel time or distance to healthcare for adults in global north countries associated with an impact on health outcomes? A systematic review. BMJ Open, 6(11), e013059. https://doi.org/10.1136/bmjopen-2016-013059
- Knight Frank India Private limited. (2021). Bengaluru urban infrastructure report – 2020. https://content.knightfrank.com/research/2142/documents/en/bengaluru-urban-infrastructure-report-2020-india-urban-infrastructure-report-7671.pdf.
- Kotavaara, O., Nivala, A., Lankila, T., Huotari, T., Delmelle, E., & Antikainen, H. (2021). Geographical accessibility to primary health care in Finland – Grid-based multimodal assessment. Applied Geography, 136, 102583. https://doi.org/10.1016/j.apgeog.2021.102583
- Kullanit, A., & Taneepanichskul, N. (2018). Transportation barriers on healthcare utilization among elderly population living in Mahasarakham Province, Thailand. Journal of Health Research, 31(2), 233–238. https://he01.tci-thaijo.org/index.php/jhealthres/article/view/114558.
- Kyriopoulos, I.-I., Zavras, D., Skroumpelos, A., Mylona, K., Athanasakis, K., & Kyriopoulos, J. (2014). Barriers in access to healthcare services for chronic patients in times of austerity: An empirical approach in Greece. International Journal for Equity in Health, 13(1), 54. https://doi.org/10.1186/1475-9276-13-54
- Luiu, C., & Tight, M. (2021). Travel difficulties and barriers during later life: Evidence from the national travel survey in England. Journal of Transport Geography, 91, 102973. https://doi.org/10.1016/j.jtrangeo.2021.102973
- Lupton, D., & Lewis, S. (2021). Learning about COVID-19: A qualitative interview study of Australians’ use of information sources. BMC Public Health, 21(1), 662. https://doi.org/10.1186/s12889-021-10743-7
- Lupton, D., & Lewis, S. (2022). Coping with COVID-19: The sociomaterial dimensions of living with pre-existing mental illness during the early stages of the coronavirus crisis. Emotion, Space and Society, 42, 100860. https://doi.org/10.1016/j.emospa.2021.100860
- Mah, S., & Mitra, R. (2017). The effects of a free bus program on older adults travel behaviour: A case study of a Canadian suburban municipality. Case Studies on Transport Policy, 5(3). https://doi.org/10.1016/j.cstp.2017.05.003
- Meijering, L. (2021). Towards meaningful mobility: A research agenda for movement within and between places in later life. Ageing and Society, 41(4), 711–723. https://doi.org/10.1017/S0144686X19001296
- Mohd Rosnu, N. S., Singh, D. K. A., Mat Ludin, A. F., Ishak, W. S., Abd Rahman, M. H., & Shahar, S. (2022). Enablers and barriers of accessing health care services among older adults in South-East Asia: A scoping review. International Journal of Environmental Research and Public Health, 19(12), 7351. https://doi.org/10.3390/ijerph19127351
- Musselwhite, C. (2022). A research agenda on transport and health and public buses: More research on the buses please!. Journal of Transport & Health, 24, 101355. https://doi.org/10.1016/j.jth.2022.101355
- Nayka, S., & Sridhar, K. S. (2019). Determinants of Intra Urban Mobility: A Study of Bengaluru.
- Nordbakke, S. (2013). Capabilities for mobility among urban older women: Barriers, strategies and options. Journal of Transport Geography, 26. https://doi.org/10.1016/j.jtrangeo.2012.10.003
- Novek, S., & Menec, V. H. (2014). Older adults’ perceptions of age-friendly communities in Canada: A photovoice study. Ageing and Society, 34(6), 6. https://doi.org/10.1017/S0144686X1200150X
- Oduro Appiah, J., Agyemang-Duah, W., Peprah, C., Adei, D., Peprah, P., & Fordjour, A. A. (2020). Transportation barriers to formal healthcare utilisation and associated factors among poor older people under a social protection programme in Ghana. Journal of Transport & Health, 19, 100965. https://doi.org/10.1016/j.jth.2020.100965
- Planning Commission, G. O. I. (2013). Twelfth five year plan 2012-2017 social sectors, Volume-III. Sage Publications.
- Ponnuswamy, S., & Victor, (Late) D. J. (2012). Intermediate public transport. In Urban transportation: Planning, operation and management (First edition). McGraw-Hill Education. https://www.accessengineeringlibrary.com/content/book/9781259002731/chapter/chapter12.
- Ramlucken, L., & Sibiya, M. N. (2018). Frequency and reasons for missed appointments of outpatient mental health care users in the uMgungundlovu district. Curationis, 41(1). https://doi.org/10.4102/curationis.v41i1.1835
- Reinhard, E., Courtin, E., van Lenthe, F. J., & Avendano, M. (2018). Public transport policy, social engagement and mental health in older age: A quasi-experimental evaluation of free bus passes in England. Journal of Epidemiology and Community Health, 72(5). https://doi.org/10.1136/jech-2017-210038
- Rohwerder, B. (2015). Disability inclusion: Topic guide. In Birmingham, UK: GSDRC, University of Birmingham.
- Seifert, A. (2020). The digital exclusion of older adults during the COVID-19 pandemic. Journal of Gerontological Social Work, 63(6–7), 674–676. https://doi.org/10.1080/01634372.2020.1764687
- Syed, S. T., Gerber, B. S., & Sharp, L. K. (2013). Traveling towards disease: Transportation barriers to health care access. Journal of Community Health, 38(5). https://doi.org/10.1007/s10900-013-9681-1
- Tsang, M. (2012). Connecting and caring: Innovations for healthy ageing. Bulletin of the World Health Organization, 90(3). https://doi.org/10.2471/BLT.12.020312
- United Nations. (2017). World Population Ageing 2017 – Highlights.
- United Nations. (2021). Department of economic and social affairs: Sustainable development. https://sdgs.un.org/goals/goal11.
- Varela, C., Young, S., Mkandawire, N., Groen, R. S., Banza, L., & Viste, A. (2019). Transportation barriers to access health care for surgical conditions in Malawi a cross sectional nationwide household survey. BMC Public Health, 19(1). https://doi.org/10.1186/s12889-019-6577-8
- Villena-Sanchez, J., & Boschmann, E. E. (2022). A scoping review of the daily mobilities of older adults in the global south. The Canadian Geographer / Le Géographe Canadien, 66(1), 119–131. https://doi.org/10.1111/cag.12736
- Wallace, R., Hughes-Cromwick, P., Mull, H., & Khasnabis, S. (2005). Access to health care and nonemergency medical transportation. Transportation Research Record: Journal of the Transportation Research Board, 1924(1), 76–84. https://doi.org/10.1177/0361198105192400110
- Wolfe, M. K., McDonald, N. C., & Holmes, G. M. (2020). Transportation barriers to health care in the United States: Findings from the national health interview survey, 1997–2017. American Journal of Public Health, 110(6), 815–822. https://doi.org/10.2105/AJPH.2020.305579
- World Health Organization. (2021). The WHO age-friendly cities framework. World Health Organization. https://extranet.who.int/agefriendlyworld/age-friendly-cities-framework/.
- World Population Review. (2023). Bangalore population 2023. 2023 World Population Review. https://worldpopulationreview.com/world-cities/bangalore-population.
- Yellapa, V., Devadasan, N., Krumeich, A., Pant Pai, N., Vadnais, C., Pai, M., & Engel, N. (2017). How patients navigate the diagnostic ecosystem in a fragmented health system: A qualitative study from India. Global Health Action, 10(1), 1350452. https://doi.org/10.1080/16549716.2017.1350452