ABSTRACT
Globally, anaemia prevails as a public health issue, being also a concern in Mozambique, where about two-thirds of children 6–59 months of age are affected by this condition. We carried out this study to estimate anaemia prevalence and evaluate structural determinants and haematological parameters association among children aged 6–59 months attending pediatric inpatient and outpatient services in a Quaternary Health Facility in Maputo City Province, Mozambique. We collected data from 637 inpatients or outpatients who attended pediatric consultations at the Maputo Central Hospital. The overall rate of anaemia in children aged 6–59 months was 62.2% (396/637), with 30.9% moderate anaemia (197/637), 23.9% mild anaemia (152/637), and 7.4% severe anaemia (47/637). Among our study participants, critical factors for anaemia were those concerning the age group, child´s caregiver schooling, malaria and size of the liver.
Introduction
Anaemia is a condition characterised by a reduction in the red blood cell count or the concentration of haemoglobin (Sharman, Citation2000). It has significant adverse health consequences contributing to the increased morbidity from infectious diseases and unfavourable impacts on social and economic development (World Health Organization [WHO] & UNICEF, Citation2017; Sharman, Citation2000). Anaemia in children under five, based on the concentrations of haemoglobin in the blood, is classified as mild (10g/dL ≤ Hb ≤ 10.9g/dL), moderate (7g/dL ≤ Hb ≤ 9.9g/dL), and severe (Hb < 7.0g/dL) (Melku et al., Citation2018; WHO, Citation2011). Moderate and severe anaemia is associated with the deterioration of both physical and cognitive development in children (Ngnie-Teta et al., Citation2007). Severe anaemia, in particular, carries a high ‘hidden’ morbidity and mortality, occurring months after initial diagnosis and treatment, and is a contributing factor for overall under-five mortality (Melku et al., Citation2018). Microcytic iron deficiency anaemia is also a common cause of childhood anaemia and is associated with impaired cognitive and intellectual performance, motor development, coordination, language development, and academic performance (Demaret et al., Citation2017; Sharman, Citation2000; Wang, Citation2016).
In 2019, global anaemia prevalence was 39.8% ((95% uncertainty interval (UI) 36.0%, 43.8%)) in children aged 6–59 months, equivalent to 269 million children with anaemia (WHO, Citation2021). Over 60.2% of children aged 6–59 months in the African region were affected by anaemia in the same year (WHO, Citation2021). Thus, anaemia prevails as a global public health issue and is also a concern in Mozambique, where about two-thirds of children 6–59 months of age are affected (Muhajarine et al., Citation2021; Picolo et al., Citation2019). From 2015 to 2018, studies showed that anaemia prevalence rates increased for Mozambican children aged 6–59 months, from 61.2% to 78.8% (Ministério da Saúde [MISAU] & INS, Citation2015; MISAU et al., Citation2015; United Nations Children’s Fund [UNICEF], Citation2021; Zaba et al., Citation2021). Recent evidence shows that rates of child anaemia have remained high at 63.8%, affecting primarily Mozambican children 6–23 months living in poorer households (MISAU et al., Citation2015; Picolo et al., Citation2019).
Anaemia is far from trivial and is associated with a decreased quality of life, worse outcomes even in non-critically ill patients, and increased healthcare resource utilisation (Demaret et al., Citation2017). Patients admitted to hospitals are at risk of becoming anaemic from blood loss, nutritional issues, or chronic disease (Hamid et al., Citation2021). Despite the existence of some studies on anaemia in children aged 6–59 months in Mozambique and Maputo City and Maputo’s Province, many are either outdated or mainly focused on household-level and community-level data or malaria and HIV (Cambaza, Citation2013; Chemane et al., Citation2021; Duffy et al., Citation2020; Moraleda et al., Citation2017; Muhajarine et al., Citation2021; Picolo et al., Citation2019). A study by Moraleda et al. (Citation2017) reported that iron deficiency, undernutrition, malaria, and HIV are the main factors associated with anaemia in hospitalised Mozambican preschool children. In 2016, a study in a hospitalised cohort of HIV-infected and HIV-exposed uninfected children aged 6–59 months reported a high prevalence of anaemia (Duffy et al., Citation2020).
Estimating anaemia prevalence in the hospital setting can help improve clinical management, the provision of services, and intervention strategies planning for anaemia care management in children aged 6–59 months (Tesfay et al., Citation2021). Nonetheless, while community-level-based studies bring evidence of childhood anaemia prevalence and associated factors, hospital-level-based studies conducted until now often report only anaemia prevalence lacking possible associated risk factors (Chemane et al., Citation2021). Thus, eventually contributing to the continuity of in-care health facility gaps linked to poor anaemia management of cases. We carried out this study to estimate anaemia prevalence and evaluate structural determinants and haematological parameters association among children aged 6–59 months attending pediatric inpatient and outpatient services in a Quaternary Health Facility in Maputo City Province, Mozambique. Thus, evidence generated by this research will contribute to a better understanding of anaemia among this population group and help to improve and guide nutrition-specific strategies and policies, also clinical management at the health facility level. Preliminary findings of this research were presented previously as a meeting oral pitch presentation at the 15th European Public Health Conference 2022 on 12 November 2022 (Maulide Cane et al., Citation2022).
Materials and methods
Study design and setting
From August 2020 to August 2022, we collected secondary data from inpatients or outpatients who attended pediatric consultations at the ‘Maputo Central Hospital (HCM)’ – a quaternary health facility in Maputo City Province. Mozambique’s health facilities are hierarchically organised into primary, secondary, tertiary, and quaternary levels to ensure a comprehensive referral system and continuum of care. Typically, tertiary and quaternary health facilities are provincial or regional referral hospitals (generally located in densely populated urban areas) (Fernandes et al., Citation2023). The Pediatrics Department of Maputo Central Hospital is a reference at the national level that integrates ten services: intensive care, pediatric emergency, surgery, infants, hemato-oncology, general illnesses, infectious diseases, pneumology, neonatology, outpatient consultations, and has the following subspecialties: cardiology, neurology, nephrology, hemato-oncology, and pulmonology (Departamento de Pediatria [DP], Citation2023).
Selection and description of participants
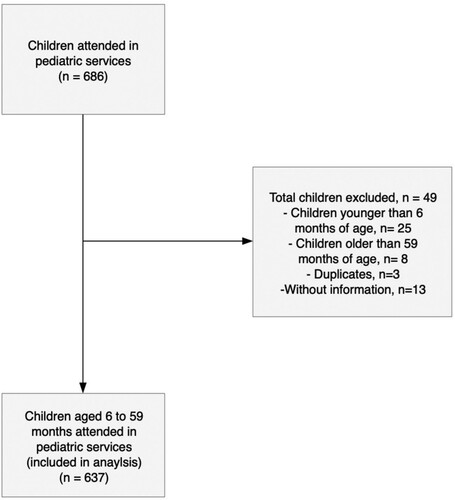
The sample universe was the Pediatrics Department of Maputo Central Hospital. All medical records of children aged 6–59 months who attended pediatric consultations during the period´s study were included (census approach). In total, 637 children attending these pediatric consultations and that complied with the study criteria were selected (see , Supplementary Table 1). Inclusion criteria were: a child aged between six and 59 months. Exclusion criteria were: a child who does not have a haemoglobin (Hb) determination or who has carried a haemoglobin determination out of the period covered by the study; a child younger than six months; a child older than 59 months. Children under five have anaemia when the haemoglobin concentration is below 11.0 g/dL at sea level (see Supplementary Table 1). The cut-off values for anaemia in children aged 6–59 months, based on haemoglobin levels, were: mild (10g/dL ≤ Hb ≤ 10.9g/dL), moderate (7g/dL ≤ Hb ≤ 9.9g/dL), and severe (Hb < 7.0g/dL) (WHO, Citation2011). Children were categorised by age as follows: 6–11 months, 12–23 months, and 24–59 months (MISAU et al., Citation2015; MISAU & INS, Citation2015; UNICEF, Citation2021b).
Data collection
We collected data from clinical records, child’s health cards, consultation registration books, and monthly summary records. A pre-tested electronic questionnaire (Kobo Toolbox [Kobo], Citation2023) was used to compile information on sociodemographics, health status, and nutritional variables. The questionnaire, prepared in Portuguese, included four sections that dealt with (i) sociodemographic characteristics, (ii) anthropometric characteristics, (iii) feeding practices and therapeutic diet, and (iv) health status. Data collectors received training on study objectives, ethics, and data collection procedures – including a pilot day. Data collection was closely monitored and supervised by investigators. To ensure good data quality, we performed double data entry and compared the information in physical records (paper-based form) and the electronic questionnaire. Data cleaning was performed to verify frequency, consistency, and missed values, and any errors identified were corrected.
Data analysis
Data was analysed using SPSS 28.0 software (International Business Machine Corporation [IBM Corp], We performed descriptive statistics Citation2021), (frequencies, cross-tabulations) and measures of association (Cramer’s V, Phi, and contingency coefficient) to describe study participants and determine anaemia prevalence. We estimated the odds ratio and associated confidence intervals (CI 95%) using logistic regression models. Primarily, we examined the association between the independent variables and anaemia using bivariate logistic regression. Subsequently, we included variables with a p-value less than 0.05 in the adjusted multiple logistic regression model (Hsieh et al., Citation1998; Ranganathan et al., Citation2017). The anaemia (has anaemia = Hb < 11.0g/dL; without anaemia = Hb ≥ 11.0g/dL) was considered a dependent variable in the model. Gender, age, residence area, province, child’s caregiver schooling, breastfeeding, complementary feeding, type of breastfeeding, porridge intake, family meals, eating practices, mid-upper arm circumference (MUAC), malaria, human immunodeficiency virus (HIV), COVID-19, glucose level, urine testing, vomiting, cough, pale conjunctiva, and size of the liver were analysed as independent variables in the model.
Results
Socio-demographic characteristics
A total of 637 children aged 6–59 months attended the pediatric services. The majority of participants were male (354/637; 55.6%), aged between 24–59 months (288/637; 45.2%), and lived in rural areas (370/637; 58.1%) (see ; Supplementary Table 2).
Table 1. Socio-demographic characteristics of children aged 6–59 months at Maputo Central Hospital, PAMC, August 2020-August 2022.
Nutritional and health characteristics
summarises the nutritional and health characteristics of the children. More than half of the children (334/637; 52.4%) received breastfeeding, and 47.4% (302/637) received complementary foods. About 14.4% (92/637) had exclusive breastfeeding, while 36.1% (230/637) received breastfeeding simultaneously with complementary feeding. Out of the 637 children, 33 (5.2%) were at risk of acute malnutrition, 68 (10.7%) had malaria, 25 (3.9%) had HIV, 15 (2.4%) had COVID-19, and 25 (3.9%) had urinary tract infections. The overall prevalence of anaemia in children aged 6–59 months was 62.2% (396/637), with 30.9% moderate anaemia (197/637), 23.9% mild anaemia (152/637), and 7.4% severe anaemia (47/637).
Table 2. Nutritional and health characteristics of children aged 6–59 months at Maputo Central Hospital, PAMC, August 2020-August 2022.
Sociodemographic, nutritional, and health parameters associated with anaemia
Anaemia in children aged 6–59 months was associated with age, child’s caregiver schooling, complementary feeding, malaria or HIV, cough and size of the liver (p < 0.05) in the bivariate logistic regression analysis. At the same time, age, child´s caregiver schooling, malaria and size of the liver remained significant in the multivariable logistic regression analysis (p < 0.05). Children aged 6–11 months are more prone to have anaemia than children from other age groups (OR = 2.39; CI 95% = 1.37–4.16). Children whose caregivers have no schooling (OR = 3.07; CI 95% = 1.37–6.89) or with a primary (OR = 2.71; CI 95% = 1.23–5.98) or secondary (OR = 1.96; CI 95% = 1.07–3.60) level of education are also more likely to have anaemia. Malaria (OR = 3.56; CI 95% = 1.63–7.77) and the size of the liver (OR = 10.57; CI 95% = 1.36–81.95) are also factors with a crucial role in anaemia (see ).
Table 3. Analysis of factors associated with anaemia in children aged 6–59 months at Maputo Central Hospital, PAMC, August 2020-August 2022.
Discussion
In this study, we described the magnitude of anaemia in children aged 6–59 months who attended Maputo Central Hospital and evaluated its association with structural and haematological parameters. We observed a high prevalence of anaemia among children aged 6–59 months of 62.2% (CI 95% = 2.6–3.0%) in children aged 6–59 months. This prevalence is higher than 40% and is considered a severe public health problem (WHO, Citation2011, Citation2023). Our findings are similar to those of Mavale et al. (Citation2000), who reported a high prevalence of anaemia (68.7%) in infants attending Alto-Mae and Xipamanine health centres in Maputo city.
Our findings also corroborate with a previous study by Duffy et al. (Citation2020) that showed a high anaemia prevalence (88%) in cohorts of HIV-infected and HIV-exposed uninfected children aged 6–59 months admitted to hospitals in Maputo and Zambezia provinces in Mozambique. We found a higher prevalence of anaemia than that reported by other authors in Uganda (58.8%) (Kuziga et al., Citation2017), Angola (53.8%) (Gasparinho et al., Citation2022), Northeast (52.2%) and Southern Ethiopia (13.2%) (Aliyo & Jibril, Citation2022; Fentaw et al., Citation2023), Bangladesh (49.4%) (Chisti et al., Citation2022), Lebanon (33.2%) (Salami et al., Citation2018) and China (8.8%) (Li et al., Citation2020). However, it was lower than that found in Tanzania (69.1%) (Khatib & Joho, Citation2022) and Pakistan (63.7%) (Khan et al., Citation2021). Compared to our findings, previously mentioned studies show a difference in anaemia prevalence that might be due to the geographical/seasonal variability of risk factors and the cultural and socioeconomic characteristics of the populations, as noted by Melku et al. (Citation2018).
Although addressing micronutrient deficiencies in children under 59 months of age is one of the highest priorities in the Mozambican health sector (Boletim da República [BR], Citation2021; Amaro, Citation2019), current strategies may still be inadequate, and more efforts are needed to address anaemia. ´Homemade food fortification with multi-nutrient powder´ (MNP) is one of the responses to micronutrient deficiencies, including iron, adopted by the Mozambican Ministry of Health in 2015 (MISAU, Citation2022). However, it faces systematic stock-outs limiting the supply of all required doses to children. As such, in 2021 was reported that only 9.0% of children (7.021 out of 410.684) had received the first dose of MNP and failed to receive the second and third doses of MNP (MISAU, Citation2022). Ensuring a strong and resilient health system able for timely delivery of MNP supplementation to children under five through the reinforcement of human resources logistic management skills can contribute to reducing the anaemia burden.
We found an association between anaemia and age, caregiver schooling, malaria, and liver size. This association of anaemia with malaria was also observed in previous studies (Duffy et al., Citation2020; Moraleda et al., Citation2017; Muhajarine et al., Citation2021), highlighting the need for more monitoring. Foreseeable, the association between anaemia and the liver size reported by us is also in good agreement with previous findings in the literature (Divya et al., Citation2020; Muhe et al., Citation2000; White, Citation2018; Yurdakök et al., Citation2008). Anaemia commonly develops rapidly in acute malaria, and the liver and spleen enlarge rapidly (White, Citation2018), explaining the results found in our study.
The current study shows that children aged 6–11 months are more prone to suffer anaemia than their peers – this is consistent with previous findings in Ethiopia and China (Fentaw et al., Citation2022; Li et al., Citation2020). Possible explanations for these results may be related to the – age at which complementary foods are given to the children. As suggested by several authors (Csölle et al., Citation2022; Miniello et al., Citation2021, Citation2017), the age of introduction of complementary feeding might also be critically important if infants are not fed properly, with an external source of iron, which might be associated with childhood anaemia. In our study, the exact time age´s introduction of complementary foods to the children evaluation couldn´t be carried out due to the unavailability of information (not featured in the clinical data collection charts/tools). Such limitations may be considered in further research, ensuring a better understanding of the age-time of complementary foods introduction and its relationship with anaemia in this setting.
In line with our findings, children whose caregivers have a lower level of education may be more exposed to the risk of anaemia than those whose caregivers have a higher level of education, which is well documented in studies conducted in Ethiopia (Gebereselassie et al., Citation2020; Melku et al., Citation2018; Regassa et al., Citation2023) and Tanzania (Khatib & Joho, Citation2022). Some authors suggested that health education strengthening caregivers’ scientific nutrition knowledge can be carried on during the prevention and treatment of maternal anaemia during pregnancy (Li et al., Citation2020). In addition, our results highlight the importance of increasing educational interventions for caregivers whose children are intruded to complementary foods- helping to improve feeding practices and contributing to the management of anaemia.
Although we observed a slightly higher prevalence of anaemia among boys comparing girls and those children living in rural areas compared to urban areas, we found no association between anaemia and gender or residence area. Even so, that does not imply that gender may not play a role in anaemia´s occurrence. Some authors argue that marked urban-rural anaemia prevalence variation may indicate the importance of targeting specific areas or districts (Ncogo et al., Citation2017). Several studies reported the higher prevalence of anaemia in children who are males is linked to a higher growth rate in boys as they have higher iron body requirements, often not supplied by the diet (Elmardi et al., Citation2020; Tesema et al., Citation2021; Zuffo et al., Citation2016). However, evidence for the role of these factors in anaemia in Mozambican children remains weak and warrants further research.
Strengths and limitations
As far as we know, this was the first study with a large sample size that attempted to evaluate the determinants associated with the prevalence of anaemia in children aged 6–59 months in this specific setting. Therefore, our study can contribute to filling the gap in the evidence/literature on this topic and improve ongoing interventions related to the prevention and management of anaemia in children aged 6–59 months. We are aware that our study may have some limitations. The first limitation is that we could not identify the exact age at which complementary foods were introduced to children – as this information is not available in clinical records, child health cards, consultation registers, and monthly summary records. The second limitation is that information on the child’s intestinal parasitosis is unavailable, remaining poorly captured by the data collection tools used in this study. Therefore, we could not compare the risk of anaemia in children concerning the introduction of complementary feeding at different ages and intestinal parasitosis. These limitations highlight the difficulty of collecting data in this quaternary setting – where there are still no electronic records and the conditions for archiving physical charts/records are often inadequate or inappropriate. The third limitation is that a few variables presented a high proportion of missing values (above 15%), namely, porridge intake, family meals intake, eating practices, MUAC, COVID-19, urine testing and glucose. However, such variables did not enter into the multivariate logistic regression model. Thus, the model obtained was not affected.
Conclusion
Our findings provide evidence of factors associated with the prevalence of anaemia in children aged 6–59 months of age. More than half of the children were anaemic, demonstrating that anaemia prevails as a severe public health problem, particularly in this setting. Among our study participants, key – factors for anaemia were age, caregiver schooling, malaria and size´s liver. To tackle anaemia, a set of multisectoral efforts should take place targeting the improvement of management for timely delivery of homemade fortification by the Ministry of Health, the continuous monitoring of children who have malaria by the health practitioners, the reinforcement of educational interventions among caregivers whose children are introducing complementary foods by nutritionists and health practitioners, as well as, the strengthening of strategic community interventions adapted to the local context and aimed at reducing food insecurity, particularly during economic, environmental and public health emergencies.
Ethical considerations
This study was conducted following the Helsinki Declaration and approved by the Institutional Committee of Bioethics in Health of the Faculty of Medicine/Maputo Central Hospital (CIBS FM&HCM/004/2020). This research is also a sub-study – that integrates the study protocol on the same topic (PAMC, Ref. Of0110/CC/2020).
Contributors
Conceptualization: RMC, IC, and LV; Methodology: RMC, IC, and LV; Data collection: RMC, LL, and EP; Coordination of data collection on site: RMC; Formal Analysis: RMC and YK; Investigation: RMC and YK; Resources: RMC; Data Curation: RMC, YK and MPG; Writing-Original Draft Preparation: RMC; Writing – Review and Editing: RMC, YK, IC, and LV; Visualization: RMC; Supervision: IC and LV. All authors have read and agreed to the published version of the manuscript.
Supplemental Material
Download ()Acknowledgements
We thank Paulino da Costa, Faizana Amad, Eugenia Macassa, Nocita da Natividade Macuacua, Amélia Guambe, Rosita Agostinho Baloi Cossa, Vasco Muchanga, Lidia Maungue, Henrique Afonso Mondlane, Silvia Panunzi and Luzia Gonçalves. We also thank the staff of the Pediatrics Department of Maputo Central Hospital. This work is dedicated to Tamim Merzouki (deceased).
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Aliyo, A., & Jibril, A. (2022). Anemia and associated factors among under five year old children who attended bule hora general hospital in West Guji zone, Southern Ethiopia. Journal of Blood Medicine, 13, 395–406. https://doi.org/10.2147/JBM.S363876
- Amaro M. (2019). Accelerating progress in micronutrient deficiencies in Mozambique: A Ministry of Health perspective. Maternal & Child Nutrition, 15(S1), e12707. https://doi.org/10.1111/mcn.12707
- Boletim da República. (2021). Política de Saúde e a Estratégia da Sua Implementação (Resolução n.° 13/2021:Serie N72). Gazettes Africa. Retrieved April 17, 2023, from https://gazettes.africa/archive/mz/2021/mz-government-gazette-series-i-dated-2021-04-16-no-72.pdf
- Cambaza E. (2013). Estudo dos níveis de hemoglobina e prevalência de anemia em adultos da Cidade de Maputo. Accademos Saúde Pública, Nutrição e Alimento, 1-31.https://www.academia.edu/3738800/Hemoglobina_e_Anemia_em_Adultos_da_Cidade_de_Maputo
- Chemane, E., Wale, C., Macamo, R., Machanhane, R., Cassy, A., & Sitoe N. (2021). Caracterização Hemato-linfocitária em Crianças Infectadas por Malária. Revista Moçambicana de Ciências de Saúde, 7(1). https://pesquisa.bvsalud.org/portal/resource/pt/biblio-1343979
- Chisti, M. J., Kawser, C. A., Rahman, A. S. M. S. B. S, Afroze, F., Shahunja, K. M, Shahrin, L., Sarmin, M., Nuzhat, S., Rahman, A. E., Alam, T., Parvin, I., Mahmuda, M. S. T., Mamun, G. M. S, Shaima, S. N., Faruque, A. S. G., & Ahmed, T. (2022). Prevalence and outcome of anemia among children hospitalized for pneumonia and their risk of mortality in a developing country. Scientific Reports, 12(1), 10741. https://doi.org/10.1038/s41598-022-14818-2
- Csölle, I., Felső, R., Szabó, É, Metzendorf, M. I., Schwingshackl, L., Ferenci, T., & Lohner, S. (2022). Health outcomes associated with micronutrient-fortified complementary foods in infants and young children aged 6-23 months: A systematic review and meta-analysis. The Lancet Child & Adolescent Health, 6(8), 533–544. https://doi.org/10.1016/S2352-4642(22)00147-X
- Demaret, P., Karam, O., Tucci, M., Lacroix, J., Behal, H., Duhamel, A., Lebrun, F., Mulder, A., & Leteurtre, S. (2017). Anemia at pediatric intensive care unit discharge: Prevalence and risk markers. Annals of Intensive Care, 7(1), 107. https://doi.org/10.1186/s13613-017-0328-8
- Departamento de Pediatria. (2023). Hospital Central de Maputo. https://www.hcm.gov.mz/
- Divya, K. K., Avabratha, K. S., Shenoy, V. K., & Anand, K. V. (2020). Efficacy of site of pallor to detect anemia and its correlation with etiology in under five children. International Journal of Contemporary Pediatrics, 8, 160–164. https://doi.org/10.18203/2349-3291.ijcp20205429
- Duffy, C., Kenga, D. B., Gebretsadik, T., Maússe, F. E., Manjate, A., Zaqueu, E., Fernando, H. F., Green, A. F., Sacarlal, J., & Moon, T. D. (2020). Multiple concurrent illnesses associated with anemia in HIV-infected and HIV-exposed uninfected children aged 6-59 months, hospitalized in Mozambique. The American Journal of Tropical Medicine and Hygiene, 102(3), 605–612. https://doi.org/10.4269/ajtmh.19-0424
- Elmardi, K. A., Adam, I., Malik, E. M., Ibrahim, A. A., Elhassan, A. H., Kafy, H. T., Nawai, L. M., Abdin, M. S., & Kremers, S. (2020). Anaemia prevalence and determinants in under 5 years children: Findings of a cross-sectional population-based study in Sudan. BMC Pediatrics, 20(1), 538. https://doi.org/10.1186/s12887-020-02434-w
- Fentaw, W., Belachew, T., & Andargie, A. (2023). Anemia and associated factors among 6 to 59 months age children attending health facilities in Kombolcha town, Northeast Ethiopia: A facility-based cross-sectional study. BMC Pediatrics, 23(1), 209. https://doi.org/10.1186/s12887-023-04031-z
- Fernandes, Q., Augusto, O., Machai, H., Pfeiffer, J., Carone, M., Pinto, N., Carimo, N., Ramiro, I., Gloyd, S., & Sherr, K. (2023). Scrutinizing human resources for health availability and distribution in Mozambique between 2016 and 2020: A subnational descriptive longitudinal study. Human Resources for Health, 21(1), 33. https://doi.org/10.1186/s12960-023-00815-7
- Gasparinho, C., Gonçalves, M. H., Chissaque, A., Silva, G. L., Fortes, F., & Gonçalves, L. (2022). Wasting, stunting, and anemia in Angolan children after deworming with albendazole or a test-and-treat approach for intestinal parasites: Binary longitudinal models with temporal structure in a four-Arm randomized trial. Nutrients, 14(11), 2185. https://doi.org/10.3390/nu14112185
- Gebereselassie, Y., BirhanSelassie, M., Menjetta, T., Alemu, J., & Tsegaye, A. (2020). Magnitude, severity, and associated factors of anemia among under-five children attending Hawassa university teaching and referral hospital, Hawassa, Southern Ethiopia, 2016. Anemia, 7580104. https://doi.org/10.1155/2020/7580104
- Hamid, M., Naz, A., Alawattegama, L. H., & Steed, H. (2021). The prevalence of anaemia in a district general hospital in the United Kingdom. Cureus, 13(5), e15086. https://doi.org/10.7759/cureus.15086
- Hsieh, F. Y., Block, D. A., & Larsen, M. D. (1998). A simple method of sample size calculation for linear and logistic regression. Statistics in Medicine, 17(14), 1623–1634.
- IBM Corp. (2021). Ibm SPSS statistics for windows (version 28.0). IBM Corp.
- Khan, L., Zafar, F., & Iqbal, M. (2021). Anemia among hospitalized children – A study based on occurrence, morphology and associated factors. Pakistan Journal of Medicine and Dentistry, 10(03), https://doi.org/10.36283/PJMD10-3/006
- Khatib, A. H., & Joho, A. A. (2022). Prevalence of anaemia and caregivers’ knowledge, practice and attitude towards its prevention among under-fives in Zanzibar, Tanzania: A cross-sectional study. International Journal of Africa Nursing Sciences, 16, 100416. https://doi.org/10.1016/j.ijans.2022.100416
- Kobo. (2023). KoboToolBox: Kobo collect app (Version 1.30.1). The Kobo Organization.
- Kuziga, F., Adoke, Y., & Wanyenze, R. K. (2017). Prevalence and factors associated with anaemia among children aged 6 to 59 months in Namutumba district, Uganda: A cross-sectional study. BMC Pediatrics, 17(25). https://doi.org/10.1186/s12887-017-0782-3
- Li, H., Xiao, J., Liao, M., Huang, G., Zheng, J., Wang, H., Huang, Q., & Wang, A. (2020). Anemia prevalence, severity and associated factors among children aged 6–71 months in rural Hunan Province, China: A community-based cross-sectional study. BMC Public Health, 20(1), 989. https://doi.org/10.1186/s12889-020-09129-y
- Maulide Cane, R., Keita, Y., Varandas, L., & Craveiro, I. (2022). Anemia in children aged 6 to 59 months attending a quaternary health facility in Maputo, Mozambique. European Journal of Public Health, 32(Suppl. 3), ckac129.697. https://doi.org/10.1093/eurpub/ckac129.697
- Mavale, S., Albuquerque, O., Mondlane, R., & Guerra, A. (2000). Prevalência de anemia numa população infantil da cidade de Maputo. Act Pedriatr Port, 1(31), 33–39.
- Melku, M., Alene, K. A., Terefe, B., Enawgaw, B., Biadgo, B., Abebe, M., Muchie, K. F., Kebede, A., Melak, T., & Melku, T. (2018). Anemia severity among children aged 6–59 months in Gondar town, Ethiopia: A community-based cross-sectional study. Italian Journal of Pediatrics, 44(1), 107. https://doi.org/10.1186/s13052-018-0547-0
- Miniello, V. L., Verga, M. C., Miniello, A., Di Mauro, C., Diaferio, L., & Francavilla, R. (2021). Complementary feeding and iron status: “The unbearable lightness of being” infants. Nutrients, 13(12), 4201. https://doi.org/10.3390/nu13124201
- Ministério da Saúde. (2022). Relatório Anual do Programa de Nutrição. MISAU.
- Ministério da Saúde, Instituto Nacional de Estatística, & ICF. (2015). Inquérito de Indicadores de Imunização, Malária e HIV/SIDA em Moçambique 2015. Maputo, Moçambique. Rockville, Maryland, EUA: MISAU, INS, INE & ICF. The DHS Program. Retrieved April 17, 2023, from https://dhsprogram.com/pubs/pdf/AIS12/AIS12.pdf
- Ministério da Saúde, & Instituto Nacional de Saúde. (2015) Inquérito Nutricional a Crianças de 0 a 24 Meses de Idade, Adolescentes e Mulheres em Idade Fértil nas Províncias de Niassa, Cabo Delgado e Nampula, 2015. Maputo, Moçambique: MISAU & INS. HCM-UCLA. Retrieved April 17, 2023, from https://ped-hcm-ucla.weebly.com/uploads/8/0/6/0/80607382/15-8-18_inquerito_nutricao.pdf
- Moraleda, C., Aguilar, R., Quintó, L., Nhampossa, T., Renom, M., Nhabomba, A., Acácio, S., Aponte, J. J., Nhalungo, D., Achtman, A. H., Schofield, L., Martins, H., Macete, E., Alonso, P. L., & Menéndez, C. (2017). Anaemia in hospitalised preschool children from a rural area in Mozambique: A case control study in search for aetiological agents. BMC Pediatrics, 17(1), 63. https://doi.org/10.1186/s12887-017-0816-x
- Muhajarine, N., Adeyinka, D. A., Matandalasse, M., & Chicumbe, S. (2021). Inequities in childhood anaemia at provincial borders in Mozambique: Cross-sectional study results from multilevel Bayesian analysis of 2018 National Malaria Indicator Survey. BMJ Open, 11(12), e051395. https://doi.org/10.1136/bmjopen-2021-051395
- Muhe, L., Oljira, B., Degefu, H., Jaffar, S., & Weber, M. W. (2000). Evaluation of clinical pallor in the identification and treatment of children with moderate and severe anaemia. Tropical Medicine & International Health, 5(11), 805–810. https://doi.org/10.1046/j.1365-3156.2000.00637.x
- Ncogo, P., Romay-Barja, M., Benito, A., Aparicio, P., Nseng, G., Berzosa, P., Santana-Morales, M. A., Riloha, M., Valladares, B., & Herrador, Z. (2017). Prevalence of anemia and associated factors in children living in urban and rural settings from Bata District, Equatorial Guinea, 2013. PLoS One, 12(5), e0176613. https://doi.org/10.1371/journal.pone.0176613
- Ngnie-Teta, I., Receveur, O., & Kuate-Defo, B. (2007). Risk factors for moderate to severe anemia among children in Benin and Mali: Insights from a multilevel analysis. Food and Nutrition Bulletin, 28(1), 76–89. https://doi.org/10.1177/156482650702800109
- Picolo, M., Barros, I., Joyeux, M., Gottwalt, A., Possolo, E., Sigauque, B., & Kavle, J. A. (2019). Rethinking integrated nutrition-health strategies to address micronutrient deficiencies in children under five in Mozambique. Maternal & Child Nutrition, 15(S1), e12721. https://doi.org/10.1111/mcn.12721
- Ranganathan, P., Pramesh, C. S., & Aggarwal, R. (2017). Common pitfalls in statistical analysis: Logistic regression. Perspectives in Clinical Research, 8(3), 148–151. https://doi.org/10.4103/picr.PICR_87_17
- Regassa, R., Duguma, M., Belachew, T., & Tamiru, D. (2023). Environmental enteropathy and anaemia status among under-five children, in slum areas of Jimma Town, Ethiopia. Pediatric Health, Medicine and Therapeutics, 14, 33–43. https://doi.org/10.2147/PHMT.S387747
- Salami, A., Bahmad, H. F., Ghssein, G., Salloum, L., & Fakih, H. (2018). Prevalence of anemia among Lebanese hospitalized children: Risk and protective factors. PLoS One, 13(8), e0201806. https://doi.org/10.1371/journal.pone.0201806
- Sharman, A. (2000). Anemia testing in population-based surveys: General information and guidelines for country monitors and program managers. ORC Macro.
- Tesema, G. A., Worku, M. G., Tessema, Z. T., Teshale, A. B., Alem, A. Z., Yeshaw, Y., Alamneh, T. S., & Liyew, A. M. (2021). Prevalence and determinants of severity levels of anemia among children aged 6-59 months in sub-Saharan Africa: A multilevel ordinal logistic regression analysis. PLoS One, 16(4), e0249978. https://doi.org/10.1371/journal.pone.0249978
- Tesfay, F., Gebregerges, A., Gebrehiwot, H., Hailekiros, H., Girmay, L., Bekuretsion, H., Gebrezigher, G., Gebremariam, G., & Teklehaimanot, G. (2021). Anemia among children living with HIV/AIDS on HAART in Mekelle Hospital, Tigray regional state of northern Ethiopia – a cross-sectional study. BMC Pediatrics, 21(1), 480. https://doi.org/10.1186/s12887-021-02960-1
- United Nations Children's Fund. (2021a). A Situação das Crianças em Moçambique 2021. Resumo de Relatório. Maputo, Moçambique: UNICEF. Retrieved April 17, 2023, from https://www.unicef.org/mozambique/media/4491/file/A%20Situa%C3%A7%C3%A3o%20das%20Crian%C3%A7as%20em%20Mo%C3%A7ambique%202021.pdf
- United Nations Children's Fund. (2021b). Technical Notes from the background document for country consultations on the 2021 edition of the UNICEF-WHO-World Bank Joint Malnutrition Estimates SDG Indicators 2.2.1 on stunting, 2.2.2a on wasting and 2.2.2b on overweight. UNICEF Data. Retrieved April 20, 2023, from https://data.unicef.org/resources/jme-2021-country-consultations/
- Wang, F., Liu, H., Wan, Y., Li, J., Chen, Y., Zheng, J., Huang, T., & Li, D. (2017). Age of complementary foods introduction and risk of anemia in children aged 4–6 years: A prospective birth cohort in China. Scientific Reports, 7(1). https://doi.org/10.1038/srep44726
- Wang, M. (2016). Iron deficiency and other types of anemia in infants and children. American Family Physician, 93(4), 270–278.
- White, N. J. (2018). Anaemia and malaria. Malaria Journal, 17(1), 371. https://doi.org/10.1186/s12936-018-2509-9
- World Health Organization. (2011). Vmnis: Vitamin and mineral nutrition information system. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Geneva, Switzerland: WHO. Retrieved April 20, 2023, from https://apps.who.int/iris/bitstream/handle/10665/85839/WHO_NMH_NHD_MNM_11.1_eng.pdf
- World Health Organization. (2021) Anaemia in women and children WHO Global Anaemia estimates, 2021 Edition Global anaemia estimates in women of reproductive age, by pregnancy status, and in children aged 6-59 months. Geneva, Switzerland: WHO. Retrieved April 20, 2023, from https://www.who.int/data/gho/data/themes/topics/anaemia_in_women_and_children
- World Health Organization. (2023). Nutrition landscape information system (Nlis). Anaemia. Nutrition and nutrition-related health and development data. Geneva, Switzerland: WHO. Retrieved April 20, 2023, from https://www.who.int/data/nutrition/nlis/info/anaemia
- World Health Organization & United Nations Children's Fund. (2017). Global Nutrition Monitoring Framework: Operational guidance for tracking progress in meeting targets for 2025. Geneva, Switzerland: WHO & UNICEF. Retrieved April 20, 2023, from http://www.who.int/nutrition/publications/operational-guidance-GNMF-indicators/en/
- Yurdakök, K., Güner, S. N., & Yalçin, S. S. (2008). Validity of using pallor to detect children with mild anemia. Pediatrics International, 50(2), 232–234. https://doi.org/10.1111/j.1442-200X.2008.02565.x
- Zaba, T., Buene, D., Famba, E., & Joyeux, M. (2021). Factors associated with acute malnutrition among children 6-59 months in rural Mozambique. Maternal & Child Nutrition, 17(1), e13060. https://doi.org/10.1111/mcn.13060
- Zuffo, C. R., Osório, M. M., Taconeli, C. A., Schmidt, S. T., da Silva, B. H., & Almeida, C. C. (2016). Prevalence and risk factors of anemia in children. Jornal de Pediatria, 92(4), 353–360. https://doi.org/10.1016/j.jped.2015.09.007