ABSTRACT
This study examines the recovery experiences of students at a university college in the Netherlands during an outbreak of COVID-19 in the spring of 2022. University policy was based on the conception of COVID-19 as short-term, with a defined recovery timeline. Despite perceptions that young people face lower risks for prolonged recovery, our study reveals a different reality.
Among 36 students with COVID-19, twelve experienced symptoms for over one month. Ten semi-structured interviews revealed heterogenous recovery experiences: good, mild, moderate, and difficult. We also explored how diverse recoveries interacted with academic work. Lingering symptoms ranged from smell loss to brain fog and prolonged fatigue.
The unpredictability of recovery made it difficult to attribute symptoms to COVID-19 or academic work pressure. In the context of expectations to resume academic work, some students failed to recognise their ongoing struggles. An absence of conversation regarding recovery in a demanding academic environment renders diverse recovery experiences invisible. Our findings emphasise the need for a broader conceptualisation of COVID-19 recovery amongst young people and call for further research exploring the interaction between students’ illness experiences and the fast-paced academic environment.
Sustainable Development Goals:
Introduction
Prologue
February 2022. Three weeks into on-campus teaching and my class is half empty. To not further burden teachers we are supposed to only offer in-class education, but how to have group presentations when only one group member is still in class is beyond me. Rescheduling takes more energy than offering a hybrid option. Students are anxious about missing class and ask me how they can catch up. I want them to take time to be ill. I am tired. I started teaching three weeks ago just coming out of quarantine from a COVID-reinfection. Or was it a resurgence of the primary infection? I am not sure. I got COVID-19, very mild symptoms, got better, ill again, slightly less mild, and better. I am tired but that’s probably the intensity of teaching just after recovery (Teacher at a university college, second author).
February 2022. Two months after my COVID-19 infection and I am sicker than ever. Before my infection, I was an active and healthy 20-year-old. Though I am no longer infectious, the virus has taken a greater toll on my body than I ever expected. I cannot stand without my heart racing out of my chest, and I cannot walk any distance without gasping for breath. I have difficulty making it through class as I am unable to lie down and struggle to breathe through my mask. Most of all, I have no energy for my studies and instead of aiming for top marks as I usually do, I aim to just get through the semester.
December 2023. As two months turned into two years, my symptoms have changed, but COVID-19 has never really let go of me. Those around me announce that the pandemic ‘is over’, but I feel the effect of COVID-19 in my body every day. I still face extreme fatigue that limits my studies. With my whole life ahead of me, I wonder if I ever will feel how I did before my infection (Former student at a university college, first author).
As a teacher and a former student at a university college in the Netherlands, we both have managed uncertain illness trajectories in academic settings and had very different COVID-19 experiences. While JK as a teacher was seeing the effects of COVID-19 on students’ well-being, TM, as a student, had to manage the uncertainty of prolonged recovery in combination with keeping up with academia. These complementary perspectives sparked our interest in understanding the diverse recovery experiences of university students at a university college in the Netherlands, an academic environment characterised by excellence, a high workload, and mandatory attendance.
In the Netherlands, university students have experienced diverse COVID-19 recoveries. At the time of the study, the risk of severe symptoms and long-term disability for young people was perceived as low (Saxena et al., Citation2021; Zimmermann et al., Citation2022), except for people with pre-existing conditions (including co-morbidities) (Berghs, Citation2021) and COVID-19 was portrayed as a mundane, flu-like condition (Brown, Citation2020).
Prolonged recoveries amongst university students at the time of the study were reported through case studies such as those printed in student newsletters. Students with a mild initial infection described their post-COVID recovery as highly debilitating. International students unfamiliar with the Dutch healthcare system and lacking family support nearby faced heightened difficulties navigating COVID-19 recovery (van Dijk, Citation2021).
Studies focusing on university students highlighted the significant impact of the pandemic on students’ mental and physical well-being worldwide (Du et al., Citation2021; Plakhotnik et al., Citation2021; Reyes-Portillo et al., Citation2022). During lockdown and remote teaching and learning, students’ sleeping patterns, eating habits, and physical exercise deteriorated (Copeland et al., Citation2021; Du et al., Citation2021; Gallè et al., Citation2020). Remote teaching and learning contribute to social isolation and loneliness, lack of motivation, and dropouts (Tan, Citation2020). However, the diverse recovery experiences of COVID-19 in this population received minimal attention.
Recent studies indicate that adolescents and young adults can also face prolonged and challenging recoveries from COVID-19, even after an initial mild acute phase (Hageman, Citation2021). A heterogeneity of recovery trajectories has also been documented, ranging from straight-forward recuperation to prolonged illness (Berghs, Citation2022). Since the start of the COVID-19 pandemic, however, Dutch public health policy has centred around a linear conception of COVID-19 illness, emphasising a brief acute symptomatic phase followed by recovery within 14 days of the onset of symptoms and a clear distinction between acute and recovered states (Ajbar et al., Citation2021). Following this conceptualisation, university policy highlighted safety measures, quarantine guidelines, and information on acute infections. Information on prolonged recovery or long COVID was absent.
In this context, we examined the interplay between students’ illness and recovery experiences and academic work culture. This study was conducted as lockdown measures were easing, with many students experiencing their first COVID-19 infection.
Background: uncertain recoveries
Acute or long-COVID?
In early 2022 the paradigm around the COVID-19 pandemic shifted from a threat to an ordinary flu-like condition. The relaxing of pandemic control measures, including the reopening of in-person higher education, resulted in a surge of Omicron infections in the Netherlands (RIVM, Citationn.d.). This marked a significant moment in the pandemic’s timeline, with many simultaneously experiencing illness and heterogeneous recoveries (Berghs, Citation2021; Mahase, Citation2020).
In the context of the COVID-19 pandemic, uncertainty has been particularly triggered by prolonged recovery experiences. These experiences, referred to as ‘long COVID’ or post-acute sequelae of SARS-CoV-2, encompass a range of conditions that are challenging to capture in a distinct diagnosis (CDC, Citation2023; Mahase, Citation2020). Brown and O’Brien describe long COVID as an episodic health condition, characterised by fluctuating and unpredictable clusters of multidimensional symptoms that negatively affect well-being, daily activities, work, and social inclusion (Brown & O’Brien, Citation2021, p. 1). The lived experiences of patients with long COVID highlight symptoms that come and go inconsistently (Russell et al., Citation2022).
Symptoms of long COVID include fatigue, brain fog, neurologic dysfunction, cardiac symptoms, autonomic dysfunction, and chronic pain (CDC, Citation2023). Estimates suggest that approximately 12.7% of individuals who develop a COVID-19 infection have symptoms related to this infection three months later (Ballering et al., Citation2022). Furthermore, the incidence of long COVID appears to differ depending on the COVID-19 variant, with more cases reported for the Delta variant (17.7%) compared to the Omicron variant (10%) (de Bruijn et al., Citation2023). There is evidence that individuals with certain comorbidities, such as chronic obstructive pulmonary disorder or fibromyalgia, might face a heightened risk for long COVID (Subramanian et al., Citation2022).
Current diagnostic criteria used by public health institutions differ in their definition of long COVID. The World Health Organization (WHO) defines long COVID as symptoms occurring in individuals with a probable or confirmed, and in some cases, asymptomatic history of COVID-19, usually appearing three months after the onset of COVID-19 and persisting for at least two months without an alternative diagnosis (WHO, Citation2021). In contrast, the Centers for Disease Control and Prevention (CDC) sets the minimum symptom duration at four weeks (CDC, Citation2022). The Dutch National Institute for Public Health and the Environment (RIVM) describes long COVID as ‘long-term symptoms’ that ‘persist for several weeks, but could last for several months’ (RIVM, Citation2021).
Lingering symptoms blur the line between infection and recovery (Russell et al., Citation2022). While diagnostic criteria signal the existence of symptoms beyond four weeks, the variety in long COVID definitions leaves patients uncertain about the origin and progression of symptoms and effective remedies (Moretti et al., Citation2022). Patients are stuck in a state of uncertainty because they qualify as having long COVID according to some criteria while still being within a ‘normal’ recovery according to other definitions. This raises the question of how the prevailing framing of COVID-19 as an acute illness, in combination with unclear diagnostic criteria for long COVID shaped student experiences of lingering symptoms.
Uncertainty in illness and recovery
In making sense of a (chronic) illness trajectory, uncertainty results from questions about what symptoms mean, the effects of the illness on daily life, and what the future holds (Becker & Kaufman, Citation1995). Uncertainty in illness experience arises from a not-knowing, an inability to give meaning to an illness-related event, triggered by the unpredictability of symptoms, course of illness, and/or a lack of clarity about prognosis (Mishel, Citation1988). The processing of uncertainty is also contextual, influenced by institutional structures and conditions (Rangarajan & Daneshfar, Citation2022) As documented for difficult-to-diagnose conditions, biomedical authoritative frameworks provide legitimacy to symptoms, and the absence of these frameworks can lead to isolation (Nettleton, Citation2006; Rosenberg, Citation2002; Ware, Citation1992). Long COVID is recognised as a ‘patient-made’ illness; in the absence of biomedical authoritative frameworks, patient activism has allowed for the (medical) recognition of the heterogeneity and persistence of symptoms of long COVID (Callard & Perego, Citation2021; Rushforth et al., Citation2021; Russell et al., Citation2022). The linear public health model of COVID-19 as mild and acute for young populations holds an inherent promise of rapid recovery. The COVID-19 pandemic challenges this promise of recovery (Berghs, Citation2021, Citation2022). As in other post-viral syndromes (Proal & VanElzakker, Citation2021) what constitutes recovery is a spectrum (Bal et al., Citation2014). The concept of recovery is further complicated by the potential for reinfection and the presence of different COVID-19 strains. Rather than seeing cure or recovery as an endpoint, Berghs recommends addressing the heterogeneous experiences of cure (or recovery) itself (Berghs, Citation2022).
This study aimed to contribute to debates around COVID-19 recovery within a ‘not-at-risk’ population. Moreover, it aimed to shed light on the interplay between students’ illness and recovery experiences and academic work culture, and how uncertainty stems from this interplay.
Research context and methods
Setting
This study was conducted at a university college (UC) in the Netherlands, where UCs are separate institutes embedded in a university. UCs are characterised by a focus on interdisciplinarity, creativity, uniqueness, and excellence. While simultaneously rewarding and demanding, the neoliberal focus on continuous performance and assessment has been associated with insecurity among students (Bal et al., Citation2014). The college has a strict attendance policy, allowing a maximum of two absences per class every eight weeks. This setting, although not representative of the broader Dutch university system, offers a good case study to explore the connections between illness and recovery experiences and values like productivity. The UC offers a three-year honours bachelor’s degree in liberal arts and sciences. It hosts around 600 students, 400 of whom live on campus. The student population is diverse, representing approximately 45 nationalities mostly 18-22-year-olds, sharing similar higher education experiences. Approximately 70–75% of the student body is female.
During the pandemic from March 2020 to September 2021, the college shifted to remote teaching and learning, followed by a hybrid teaching and learning model until February 2022 when on-campus teaching and learning resumed. To accommodate the challenges posed by the COVID-19 pandemic, the college temporarily adjusted its attendance policy, allowing up to four absences until September 2022. Hybrid classes were discouraged from February 2022 onwards. The transition to on-campus teaching and learning coincided with the Omicron variant wave in the Netherlands, which began in late November 2021. The college experienced its largest outbreak in February/March 2022.
Research methodology
Design
This qualitative case study was designed to critically examine the prevailing assumption at the time of study that young students quickly recover from COVID-19. The study was set up as a qualitative case study with a narrative methodology. It combined a descriptive survey with semi-structured interviews and visual elicitation (see supplementary files).
The survey included 18 questions capturing experienced symptoms, recovery duration, and academic experience. The survey was distributed to all students enrolled at the college at the time of the study (600 students). Branching logic in the survey limited survey completion to only students who had experienced COVID-19. The survey was distributed via the primary student communication channels at the UC (Microsoft Teams and WhatsApp) in May 2022 after a delayed ethics review by the university’s institutional review board. Because May is exam month, the response rate was low; only 47 students filled out the survey, and 36 of these were eligible for survey completion and analysis. Demographic data on age, gender, and nationality were not collected: students had a similar age range, the gender balance was uneven, and data on nationality were deemed an identifying risk.
Students were recruited via the survey. Those interested were asked to contact the study team for an interview. This strategy ensured voluntary participation, allowing students to carefully consider sharing personal stories with researchers.
The semi-structured interviews aimed to prompt narrative descriptions of illness experiences, highlighting how participants navigated disruption and sought normalcy (Becker, Citation1997, p. 197), and experienced recovery within the academic work culture.
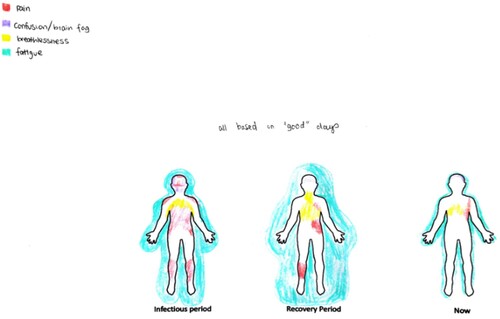
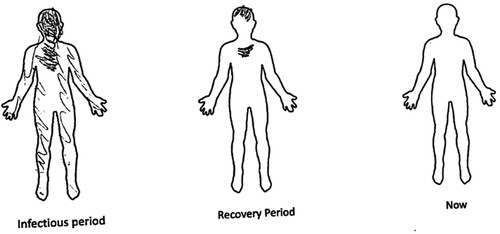
To facilitate the reflexive articulation of students’ illness trajectories and bodily experiences (Gastaldo et al., Citation2018), students were requested to fill out a body map depicting the location and severity of symptoms during illness, recovery, and current state. The body maps were used to explore similarities or disparities between narratives and visuals provided by the student, which were discussed. Students also completed a social support diagram at the beginning of the interview, which was used to visualise types and intensity of support during the acute and recovery phase (see supplementary files).
Participant-driven photo-elicitation was employed to understand student representations of their COVID-19 illness and recovery (Cleland & MacLeod, Citation2021). Students provided a photograph after the interview accompanied by a description. All interviews and visuals were anonymised.
This study was a student-driven project, involving a team of five students trained interdisciplinarily in Global Health, including the first author, under the guidance of a college staff member (second author). Students who voluntarily contacted the team signed an informed consent form. The student team conducted the interviews in a private space and stored data in an encrypted file to protect participant privacy. The second author, a college staff member, was only given participants’ pseudonyms, to protect participants’ privacy in future classroom settings. All participants are referred to by their pseudonyms in the results section.
Analysis process
An explicit aim of the analysis of the survey data was to map the study findings onto public health categories of acute COVID-19. In doing so the study aimed to critically examine public health claims that young people recovered quickly, against anecdotal evidence that recovery experiences at the college were heterogeneous. Following guidelines of RIVM, CDC, and WHO in January 2022, recommending a ten-day isolation period for symptomatic individuals following a positive test and a five-day period for asymptomatic individuals (CDC, Citation2022; RIVM, Citation2022; WHO, Citation2022), the research team defined ‘acute’ COVID-19 infection as symptoms within a 10-day window period and ‘recovery time’ as the duration between the onset of COVID-19 symptoms and the restoration to pre-COVID-19 health. Survey respondents who remained symptomatic for four weeks or longer, regardless of the severity of symptoms, were classified as experiencing a ‘prolonged recovery’, following CDC/RIVM criteria for long COVID (CDC, Citation2022; RIVM, Citationn.d.).
In doing the analysis the research team reflected on how their own heterogeneous experiences, ranging from not having had COVID-19 to a long COVID diagnosis, influenced their interpretations. After transcribing interviews, the research team collectively coded each interview, using a mix of topic list-derived codes (illness experience, recovery experience, academic work culture, social support) and inductive coding. We then executed a thematic analysis. The five research team members discussed coding once to reflect on varying interpretations of the analysis and together formulated overarching themes that reflected patterns of meaning across the data (Braun & Clarke, Citation2021, Citation2022; Glaser & Strauss, Citation2017). While the study was not designed using principles of reflexive thematic analysis (RTA) as outlined by Braun & Clarke, it resembled the process of RTA (Braun & Clarke, Citation2021).
Based on this analysis, the central theme of uncertainty was formulated. Other themes included ‘making sense of a novel illness’, ‘uncertain recoveries’, and ‘keeping up’ [with academia]. In the results section, these themes form the headings. Within the theme ‘uncertain recoveries’ the research team decided to present and categorise the interviews into four distinct recovery experiences: good recovery, mild recovery, moderate recovery, and difficult recovery. This categorisation of experiences was based on the duration and impact of symptoms on daily life and academic functioning. The survey findings were used to provide a bigger picture or context to the compared interviews.
Results
We identified three main themes: Making sense of a novel illness, uncertain recovery, and ‘keeping up’.
Making sense of a novel illness
Observing the body
Most students experienced COVID-19 between December 2021 and February 2022, when they returned to the UC for the spring semester (see ), where they followed Dutch COVID-control regulations.
Table 1. Demographic data of interviewed participants.
A main theme across the data was the novelty of the first COVID-19 experience. Students framed COVID-19 as novel and borrowed from different reference frameworks to make sense of their bodily experiences. Students mentioned symptoms such as fatigue, cough, headaches, sore throats, fever, shortness of breath, and muscle aches and pains and likened these to illnesses they had experienced, such as the flu. Students also drew on familiar bodily sensations to comprehend their novel COVID-19-related experiences. One student describing severe muscle pains likened it to the discomfort of sitting with bent legs in a car all day.
Other symptoms were novel (brain fog, headaches, chest pain, shortness of breath, muscle pains, intestinal pains, and loss of smell, or taste). The novelty was also in the rapid onset of symptoms, such as loss of taste, as Tim explained: ‘It came on very suddenly. And, you know, I think I was drinking tea. I was like, wait a minute. This is just hot.’
When reference frameworks were lacking, as in the case of bodily experiences that were unlike anything students had ever felt before, anxiety and uncertainty resulted. Laura said:
When you would move your eyes from one side to the other, that would hurt. A very specific headache that I had never had before … my peripheral vision was kinda limited like you could not really look to the sides because that hurt. Yeah … And I had never had that before.
Others, dealing with pre-existing conditions such as diabetes and asthma experienced interactions between COVID-19 and their health conditions. Emily noted how COVID-19 interfered with her diabetes, leading to increased insulin resistance, which was ‘mentally draining’.
Feelings of isolation
In the acute phase, quarantine was also a novel experience. Feelings of isolation were related to both the physical and social isolation of quarantine in dorm rooms or off-campus apartments. Students mentioned hearing sounds in the hallway without being able to participate, and being anxious because they were unable to go home to their families. Aside from feeling isolated, students also described challenges in self-care in the infectious phase, such as difficulty in eating and cooking, and struggling with household chores like dishes, laundry, and cleaning. Sophie said: ‘It was a bit of a struggle sometimes because my family could not physically help me, and a lot of my close friends who normally would be more supportive also had COVID-19 at the same time.’
Students distinguished between social and practical support. In the acute phase, support was offered by family, friends, and academic staff. Friends and dorm mates mostly provided practical support. Rose said:
I had a couple of my floormates who did groceries for me, which was super nice of them (…) they did leave some food at my door when it was someone’s birthday, but not because I had asked them to, just because they thought it would be nice to share.
Photographs 3 and 4, a vase of flowers sent by family and a snow globe reminding the student of home, represent feelings of isolation away from loved ones during the infectious period ( and ).
Both the support diagrams and the photographs represented the acute phase of the illness. The support diagrams showed that support dwindled after the acute phase. In some support diagrams, only academic staff were mentioned as support during recovery. This indicates the conceptualisation of COVID-19 as an acute illness, not just by students but also by their support network. When students’ recovery took longer and they were uncertain about the duration of symptoms and where to find support, they felt isolated.
Uncertain recovery
A second theme in our analysis included uncertain recovery. This theme was featured in both the survey and the interviews. While the survey defined long COVID as symptoms persisting beyond four weeks (CDC, Citation2022), 39% of the respondents indicated they were uncertain whether their symptoms qualified as long COVID-19, and 8% indicated experiencing long COVID-19 according to this definition (See ). These 8% reported symptoms such as fatigue, brain fog, shortness of breath/difficulty breathing, difficulty sleeping, muscle aches/pains, chest pain, and loss of taste/smell.
Table 2. Time spent ill in both recovered and non-recovered survey students at the time of the survey.
Uncertainty about having long COVID was related to recovery experiences. We used the survey to understand how student experiences of recovery mapped onto the official RIVM conceptualisation of COVID-19, which structured the institutional policy at the college. Descriptive statistics from the survey showed diverse recovery experiences. In our survey of 36 students who had contracted COVID-19, 32 provided recovery information. Among these respondents, twenty (63%) had recovered, while 12 (37%) remained unrecovered at the time of the survey. Among the 63% recovered, most (16 out of 20) had no symptoms after 10 days, which was considered ‘normal’. Among the 12 unrecovered students, 10 students experienced symptoms longer than one month. Five students were still experiencing symptoms after three months.
Thematic analysis of the interviews showed four recovery experiences based on the severity of symptoms and duration: good recovery, mild recovery, moderate recovery, and difficult recovery.
Good recovery
Interviewed students experiencing a good recovery had no remaining symptoms after the infectious period (10 days from symptom onset). Students with good recovery who were interviewed described the symptoms of COVID-19 as mild. Joseph said:
After five days, my major symptoms were gone, I was not infectious. I was feeling OK. I just had a little bit of a stuffy nose, and I would say [that] took around three more days. So in total, like eight days, I would say. And I recovered completely.
These students experienced what one described as a ‘regular flu’ with symptoms consisting of fever, runny nose, sore throat and headache, and some novel symptoms. COVID-19 did not have lingering consequences beyond their quarantine period. While uncertainty did not pertain to physical recovery, quarantine and the inability to attend class led to uncertainty and anxiety. One student described quarantine as a valuable experience in the academic environment, learning to be comfortable with being non-productive.
Mild recovery
Students experiencing a mild recovery had some symptoms that took longer to resolve, but these symptoms did not significantly impact daily life. Two interviewed students (Zoe and Rose) experienced lingering symptoms, such as feeling out of breath for about a week following acute COVID-19 infection (Rose) and losing sense of smell (Zoe). While Zoe’s sense of smell had not returned over 1.5 years after her COVID-19 episode, it did not seriously impact her daily life despite not regaining full function. Zoe expressed ambivalent chagrin: ‘Well, it’s kind of frustrating ‘cause I know that everything, like, works. Yeah, my nose can smell, and my brain just can’t understand what’s going on. But it’s just like the connection between both doesn’t work’.
Students with a good and mild recovery framed the experience of COVID-19 in terms of impact on their daily lives (particularly social life) during acute infection, emphasising isolation, the inability to leave their apartments, and missing out on ‘normal’ life.
Moderate recovery
Students who experienced moderate recoveries had some symptoms that lingered and impacted their daily functioning and academic work. Two interviewed students, Tim and Maria, had moderate recoveries. Both had lost their stamina and struggled with fatigue and concentration. Reflecting on his recent episode of flu, Tim felt that he recovered much more slowly from COVID-19, although his actual illness was much milder than the flu:
This was dramatic ‘cause I’ve been sick before, and I’ve had lots of respiratory things that made it more difficult to go back to football and to biking and everything but given the fact that the COVID experience was not as bad as the flu … [with] COVID there was really this drop off afterward.
I think people kept telling me it [academic troubles] might have been COVID [related]. I didn’t really start to think of that until … Um … . Actually, I don’t know that I ever kind of really thought of it that way. But it was something other people would say: ‘Well, no wonder you’re struggling’.
Difficult recovery
Students experiencing a difficult recovery reported long-lasting symptoms that significantly hindered daily functioning. Four students (Emily, Sophie, Iris, and Grace) described a difficult recovery, with symptoms extending for over a month or not yet resolved at the time of the interview.
Grace described getting sick more often since having had COVID-19 and going to the doctor for multiple infections. She was unsure whether to attribute this to having had COVID-19. Emily, who experienced extreme fatigue during her acute phase, and mentioned ‘sleeping like 14 hours a day’, also grappled with interactions with her diabetes. Describing her situation, she said: ‘I’ll hit a low in terms of energy, no matter how well I’ve slept the night before’. Emily further reported a lingering cough that continued for over a month and significantly disrupted her daily life, although it eventually resolved. Frustrations over the unpredictability of symptoms were common in this group of students. Sophie stated:
Fatigue can be a really big problem. What is also hard is that not every day is the same. Some days I have a lot more energy than other days. I really have to check in with myself before I leave the house or do a lot [depending] on what type of day it is going to be.
I can’t really stand for long periods of time, and other ‘normal’ slightly exhausting events are also not really possible. For example, before COVID, it would have been fine to go out once every weekend or work out, but now I can’t really do those things anymore.
As time progressed, students were unclear whether their physical symptoms had subsided (they described good days and bad days), and whether their physical symptoms were related to COVID-19 or another cause. Uncertainty was related to resuming normal activities (such as exercise) and a fear that their normal routine would exhaust them. The body maps juxtaposed with the narratives also showed ambiguity. Iris, for example, did not draw lingering symptoms in her body map. When she was asked to talk about the body map () and her current symptoms, she said:
I mean, I’m still struggling with, yeah, focusing on tasks, especially like studying a long text. Which also could be quite frustrating at times because I was able to do this. Now it’s taking me so much longer to read, so that was quite frustrating, and also just … it made me more tired as well.
‘Keeping up’
A third theme in the analysis, ‘Keeping up’, related to the interplay between COVID-19 infection and academic performance, and featured in both the survey (22% of the surveyed students reported severe difficulties in academic performance) and the interviews.
Fear of falling behind
This UC has an intensive curriculum and a high workload of about 56 hours a week. Prolonged illness and catching up with assignments may result in a real possibility of failing a course. While students mentioned reducing workload and missing content, they felt physically able to resume working after quarantining. Students with lingering symptoms did struggle to return to their previous academic standards, where ‘things started to pile up’. One student called it a ‘ricochet effect just throughout the block in the semester’ and felt ‘constantly behind’. Iris experienced lingering fatigue and brain fog, which affected her academic performance:
Especially reading from my computer screen was very hard […] just needed a lot of breaks in between, losing my focus a lot more often than before, so then just took a lot more time. And then also knowing it took a lot more time, it was just difficult to find motivation.
Staff leniency
Students had varied experiences with teacher support. Some professors checked in, granted extensions, and provided resources such as allowing online participation in class or providing supplementary material to aid in catching up. Students particularly appreciated clear communication on the consequences of absences due to COVID-19. One student described confusion regarding attendance policy and the maximum number of absences as a significant source of stress during her illness. Maria, however, felt reassured as the professor had clearly outlined expectations during the initial class,
That taking care of your body was, like, a valid reason not to come to class – and I know that sounds very obvious, but I think sometimes it’s like … it gets missed out, like ‘oh I only have like two skips, I have to come, I have to come, or else I’m gonna fail,’ and it was very much like, ‘No, chill, you’re gonna be OK.’
I had professors reach out asking how I was doing. And that felt nice because it made me feel like I was being seen and made it easier to ask them if I did actually need help […] I might have been less inclined to ask for an extension and more inclined to force myself to finish the work even when I shouldn’t have if they hadn’t reached out.
The perceived need to keep up is related to the visibility of COVID-19 at the college. During the Omicron outbreak, when multiple students per class were quarantined, COVID-19 was visible, but as cases subsided and expectations resumed, students still recovering faced challenges. Grace said:
During COVID, they were all kind of equal; the policy was the same, I guess. But later, if I mentioned I was not feeling well or anything like that they would not always take it as an excuse not to come to class. They would say: ‘That’s just not part of the policy. If you don’t have COVID, you come to class’.
Discussion
Students’ narratives highlight the heterogeneity of COVID-19, both in symptoms and recovery experiences, underscoring that COVID-19 recovery among young people is not always straightforward. One-third of the students in our study might meet the technical criteria of long COVID. However, among the students meeting these definitions, symptoms and recovery experiences and their impact on daily life vary greatly. Students themselves were hesitant to label their symptoms as long COVID. The survey showed prolonged recoveries. While ten of 36 students reported symptoms after one month, and five of these after three months, only four students identified as having long COVID. Amongst those four, two suffered from co-morbidities. Perhaps students who know what living with chronic illness entails are better able to recognise prolonged health struggles.
Although long COVID serves as a valuable concept in terms of patient advocacy (Callard & Perego, Citation2021; Rushforth et al., Citation2021; Russell et al., Citation2022), our study shows its limitation in understanding the illness experiences of students. It encompasses such a wide array of symptoms that it does not provide a meaningful framework for students to make sense of their experiences (Mishel, Citation1988).
Several aspects of COVID-19 triggered uncertainty. The first derives from experiencing a novel illness in which the recovery experience was unpredictable, and symptoms were unfamiliar. The narratives show how students grappled with understanding this new illness by comparing symptoms to those of familiar illnesses like flu, the common cold, or other viral infections. Students also used metaphors and similes to describe bodily sensations. In this process, students acquired new ‘illness knowledge’. Uncertainty led to hypervigilance; one-third of students tested while symptom-free because of a ‘feeling’. For both students with short and long recoveries, uncertainty related to the duration and progression of symptoms (Becker & Kaufman, Citation1995; Hänsch et al., Citation2017; Mishel, Citation1988). Rushforth et al. highlight that long COVID disrupts the ‘chronology’ of expected illness (Rushforth et al., Citation2021). Students’ narratives indicated a lack of acknowledgement of prolonged or uncertain recovery: students felt hesitant to connect their struggles to COVID-19.
Secondly, we found that students felt unable to process uncertainty over recovery experiences within the fast-paced academic environment, where expectations implied a swift return to academic life following the acute phase. Some students in our study recognised and reflected on their symptoms only after voicing or visualising their recovery experiences through their narrative, body map, photograph, or support circle diagram, allowing for a ‘reclamation and reimagination of the self’ (Sakalys, Citation2003). During interviews, students such as Tim and Iris, who considered themselves recovered, noticed discrepancies between their drawing and their narrative. Others, like Sophie, described the interview as a therapeutic moment, allowing them to process experiences and recognise lingering symptoms (Rushforth et al., Citation2021). Uncertainty can also prompt learning experiences (Mishel, Citation1990), as with Joseph, who expressed gratitude for discovering under quarantine the value of stepping off productivity’s treadmill. Our findings show that without space to narrate uncertainty, the heterogeneity of COVID-19 remains invisible and increases anxiety.
The diverse experiences of students recovering from COVID-19 at this UC reflect pressures around productivity. The impact of lingering symptoms on academic performance, exercise, and social life changed the course of students’ everyday lives. Becker’s suggestion that narrative allows people to reflect and struggle with what their own culture deems to be normal in comparison to their own lived experience (Becker, Citation1997) is especially relevant. The norm at this UC is to work hard and get a lot done quickly. Regardless of recovery, ten days of absence sets students back; slower-than-expected recuperation causes additional stress in their recovery trajectories.
Given the considerable number of students struggling weeks or months following their infection, we need to rethink the approaches of institutes of higher education towards COVID-19 recovery. Many students did not process their illness in the demanding academic setting. These student experiences urge us to consider how cultural values around (academic) productivity shape illness and recovery and to take seriously what it means to support and recognise students in academia if ‘cure is partial’ (Venkat, Citation2021).
In 2024, amidst the portrayal of the pandemic ‘coming to an end’, it’s crucial to have accessible information and resources to support recovering students. Beyond discussions of long COVID, this study relates to broader debates and recommendations for inclusivity in higher education. We include the following points for reflection:
Universities should foster broader faculty conversation about uncertain recoveries’ impact on academic performance, including problems with concentration, and lingering fatigue. Prior studies indicate that faculty might show less understanding towards ‘invisible disability,’ including those resulting from chronic health issues like long COVID (Hamilton et al., Citation2023)
Beyond institutional support, our study shows the important role of academic staff in how students cope with uncertain recoveries. Reaching out and creating an adaptive teaching environment significantly reduces student stress. Visibility and recognition are core to effective support (Hamilton et al., Citation2023). Empathetic teacher-student relations with clear communication are central to student wellbeing and relieving COVID-19 stress (Balkundi & Frederick, Citation2024; Douwes et al., Citation2023; Riva et al., Citation2020).
Current disability accommodations often follow a medical model, placing responsibility on the student (Nieminen, Citation2023). While most students at the UC felt supported by staff, creating an adaptive environment relied on individual staff members. Therefore, adaptive education should be a university-led initiative rather than relying on individual professors.
Limitations
This study has several limitations. The study’s setting within a UC limits its generalisability towards the Dutch student university population.
The low response rate limits our ability to report on the scale of prolonged recovery at this UC. To address this, we reconceptualised the study as a case study of diverse recovery experiences among students and used it to advocate for more research on varied recovery experiences in this age group and the interplay between academic work culture and illness experience.
A second limitation related to recruitment, which relied on self-selection of participants. This likely resulted in a selection bias towards students who wanted to share their stories and relatively more students who had experienced prolonged recovery.
Conclusion
In this study, we contrasted the public health narrative of COVID-19 as an acute infection with a heterogeneity of recovery experiences amongst university students. As students were not seen as a risk group for serious complications from COVID-19 infection, university policies were geared towards containment and reopening of the university. Our study shows diverse recovery experiences, with a third of those surveyed experiencing a recovery period of over one month and five students still unrecovered after three months. Uncertainty was an overarching theme, related to the novelty of symptoms, the uncertainty of recovery, and keeping up with academics in the fast-paced schedule of the university. Framing COVID-19 as an acute viral infection obscures the multiple realities of COVID-19 recovery at universities. This is particularly relevant under the current RIVM and university policy, where COVID-19 is seen as largely passed. This invisibilises the struggles of students experiencing prolonged recoveries from COVID-19.
Declaration of competing interest
The authors report there are no competing interests to declare.
Supplemental Material
Download MP4 Video (217.2 MB)Supplemental Material
Download PDF (291.5 KB)Acknowledgements
First, we would like to thank all study participants for their time and for entrusting us with their personal experiences. Karolina Kneller, Marieke Dohrmann, Sterre Geenen, and Tuva Bühler co-labored with us in developing and conducting the interviews, the creation of the survey, and the writing of the initial research report on which this article is based. Our sincere appreciation goes to the anonymous reviewers of this article and Andrew Gebhardt for their constructive comments.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Ajbar, A., Alqahtani, R. T., & Boumaza, M. (2021). Dynamics of an SIR-based COVID-19 model with linear incidence rate, nonlinear removal rate, and public awareness. Frontiers in Physics, 9, 1–13. https://doi.org/10.3389/fphy.2021.634251.
- Bal, E., Grassiani, E., & Kirk, K. (2014). Neoliberal individualism in Dutch universities: Teaching and learning anthropology in an insecure environment. Learning and Teaching, 7(3), 46–72. https://doi.org/10.3167/latiss.2014.070303
- Balkundi, S., & Fredrick, S. S. (2024). Students’ perceptions of COVID-19 stress and internalizing problems: Is social support a buffer? Contemporary School Psychology, 28(1), 3–14. https://doi.org/10.1007/s40688-023-00457-5
- Ballering, A. V., van Zon, S. K. R., Olde Hartman, T. C., & Rosmalen, J. G. M. (2022). Persistence of somatic symptoms after COVID-19 in the Netherlands: An observational cohort study. The Lancet, 400(10350), 452–461. https://doi.org/10.1016/S0140-6736(22)01214-4
- Becker, G. (1997). Disrupted lives: How people create meaning in a chaotic world. University of California Press.
- Becker, G., & Kaufman, S. R. (1995). Managing an uncertain illness trajectory in old age: Patients’ and physicians’ views of stroke. Medical Anthropology Quarterly, 9(2), 165–187. https://doi.org/10.1525/maq.1995.9.2.02a00040
- Berghs, M. (2021). Who gets cured? COVID-19 and developing a critical medical sociology and anthropology of cure. Frontiers in Sociology, 5, 1–5. https://doi.org/10.3389/fsoc.2020.613548
- Berghs, M. (2022). Let’s get back to normal? COVID-19 and the logic of cure. Frontiers in Sociology, 7, 1–11. https://doi.org/10.3389/fsoc.2022.782582.
- Braun, V., & Clarke, V. (2021). Can I use TA? Should I use TA? Should I not use TA? Comparing reflexive thematic analysis and other pattern-based qualitative analytic approaches. Counselling and Psychotherapy Research, 21(1), 37–47. https://doi.org/10.1002/capr.12360
- Braun, V., & Clarke, V. (2022). Conceptual and design thinking for thematic analysis. Qualitative Psychology, 9(1), 3–26. https://doi.org/10.1037/qup0000196
- Brown, P. (2020). Studying COVID-19 in light of critical approaches to risk and uncertainty: Research pathways, conceptual tools, and some magic from Mary Douglas. Health, Risk & Society, 22(1), 1–14. https://doi.org/10.1080/13698575.2020.1745508
- Brown, D. A., & O’Brien, K. K. (2021). Conceptualising long COVID as an episodic health condition. BMJ Global Health, 6(9), e007004. https://doi.org/10.1136/bmjgh-2021-007004
- Callard, F., & Perego, E. (2021). How and why patients made long COVID. Social Science & Medicine, 268, 113426:1–5. https://doi.org/10.1016/j.socscimed.2020.113426.
- CDC. (2022). Ending isolation and precautions for people with COVID-19: Interim guidance. Centers for Disease Control and Prevention. Retrieved May 15, 2023, from https://www.cdc.gov/coronavirus/2019-ncov/hcp/duration-isolation.html.
- CDC. (2023). Long COVID or post-COVID conditions. Centers for Disease Control and Prevention. Retrieved May 15, 2023, from https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html.
- Cleland, J., & MacLeod, A. (2021). The visual vernacular: Embracing photographs in research. Perspectives on Medical Education, 10(4), 230–237. https://doi.org/10.1007/S40037-021-00672-X
- Copeland, W. E., McGinnis, E., Bai, Y., Adams, Z., Nardone, H., Devadanam, V., Rettew, J., & Hudziak, J. J. (2021). Impact of COVID-19 pandemic on college student mental health and wellness. Journal of the American Academy of Child and Adolescent Psychiatry, 60(1), 134–141.e2. https://doi.org/10.1016/j.jaac.2020.08.466
- de Bruijn, S., van Hoek, A. J., Mutubuki, E. N., Knoop, H., Slootweg, J., Tulen, A. D., Franz, E., van den Wijngaard, C. C., & van der Maaden, T. (2023). Lower prevalence of post-COVID-19 condition following Omicron SARS-CoV-2 infection. medRxiv, https://doi.org/10.1101/2023.04.05.23288157
- Douwes, R., Metselaar, J., Pijnenborg, G. H. M., & Boonstra, N. (2023). Well-being of students in higher education: The importance of a student perspective. Cogent Education, 10(1), 2190697. https://doi.org/10.1080/2331186X.2023.2190697
- Du, C., Zan, M. C. H., Cho, M. J., Fenton, J. I., Hsiao, P. Y., Hsiao, R., Keaver, L., Lai, C.-C., Lee, H., Ludy, M.-J., Shen, W., Swee, W. C. S., Thrivikraman, J., Tseng, K.-W., Tseng, W.-C., Almotwa, J., Feldpausch, C. E., Folk, S. Y. L., Gadd, S., … Tucker, R. M. (2021). Health behaviors of higher education students from 7 countries: Poorer sleep quality during the COVID-19 pandemic predicts higher dietary risk. Clocks & Sleep, 3(1), 12–30. https://doi.org/10.3390/clockssleep3010002
- Gallè, F., Sabella, E. A., Ferracuti, S., De Giglio, O., Caggiano, G., Protano, C., Valeriani, F., Parisi, E. A., Valerio, G., Liguori, G., Montagna, M. T., Romano Spica, V., Da Molin, G., Orsi, G. B., & Napoli, C. (2020). Sedentary behaviors and physical activity of Italian undergraduate students during lockdown at the time of COVID−19 pandemic. International Journal of Environmental Research and Public Health, 17(17), 6171. https://doi.org/10.3390/ijerph17176171
- Gastaldo, D., Rivas-Quarneti, N., & Magalhaes, L. (2018). Body-map storytelling as a health research methodology: Blurred lines creating clear pictures. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research, 19(2), https://doi.org/10.17169/FQS-19.2.2858
- Glaser, B. G., & Strauss, A. L. (2017). The discovery of grounded theory: Strategies for qualitative research. Routledge.
- Hageman, J. R. (2021). Long COVID-19 or post-acute sequelae of SARS-CoV-2 infection in children, adolescents, and young adults. Pediatric Annals, 50(6), e232–e233. https://doi.org/10.3928/19382359-20210519-02
- Hamilton, P. R., Hulme, J. A., & Harrison, E. D. (2023). Experiences of higher education for students with chronic illnesses. Disability & Society, 38(1), 21–46. https://doi.org/10.1080/09687599.2021.1907549
- Hänsch, V., Kroeker, L., & Oldenburg, S. (2017). Uncertain future(s) perceptions on time between the immediate and the imagined. Swiss Journal of Sociocultural Anthropology, 22, 4–17. https://doi.org/10.36950/tsantsa.2017.22.7342
- Mahase, E. (2020). Long COVID could be four different syndromes, review suggests. BMJ, 371, m3981. https://doi.org/10.1136/bmj.m3981
- Mishel, M. H. (1988). Uncertainty in illness. Image: The Journal of Nursing Scholarship, 20(4), 225–232. https://doi.org/10.1111/j.1547-5069.1988.tb00082.x
- Mishel, M. H. (1990). Reconceptualization of the uncertainty in illness theory. Image: The Journal of Nursing Scholarship, 22(4), 256–262. https://doi.org/10.1111/j.1547-5069.1990.tb00225.x
- Moretti, C., Collaro, C., Terzoni, C., Colucci, G., Copelli, M., Sarli, L., & Artioli, G. (2022). Dealing with uncertainty. A qualitative study on the illness’ experience in patients with long-COVID in Italy. Acta Bio-Medica: Atenei Parmensis, 93(6), e2022349. https://doi.org/10.23750/abm.v93i6.14059
- Nettleton, S. (2006). ‘I just want permission to be ill’: Towards a sociology of medically unexplained symptoms. Social Science & Medicine, 62(5), 1167–1178. https://doi.org/10.1016/j.socscimed.2005.07.030
- Nieminen, J. H. (2023). Unveiling ableism and disablism in assessment: A critical analysis of disabled students’ experiences of assessment and assessment accommodations. Higher Education, 85(3), 613–636. https://doi.org/10.1007/s10734-022-00857-1
- Plakhotnik, M. S., Volkova, N. V., Jiang, C., Yahiaoui, D., Pheiffer, G., McKay, K., Newman, S., & Reißig-Thust, S. (2021). The perceived impact of COVID-19 on student well-being and the mediating role of the university support: Evidence from France, Germany, Russia, and the UK. Frontiers in Psychology, 12(642689), 1–13. https://doi.org/10.3389/fpsyg.2021.642689.
- Proal, A. D., & VanElzakker, M. B. (2021). Long COVID or post-acute sequelae of COVID-19 (PASC): An overview of biological factors that may contribute to persistent symptoms. Frontiers in Microbiology, 12(698169), 1–24. https://doi.org/10.3389/fmicb.2021.698169.
- Rangarajan, R., & Daneshfar, S. (2022). Processing uncertainty during COVID-19: A collaborative autoethnography of two stranded international Ph.D. Students. In B. Cahusac De Caux, L. Pretorius, & L. Macaulay (Eds.), Research and teaching in a pandemic world (pp. 37–57). Springer Nature Singapore.
- Reyes-Portillo, J. A., Masia Warner, C., Kline, E. A., Bixter, M. T., Chu, B. C., Miranda, R., Nadeem, E., Nickerson, A., Ortin Peralta, A., Reigada, L., Rizvi, S. L., Roy, A. K., Shatkin, J., Kalver, E., Rette, D., Denton, E., & Jeglic, E. L. (2022). The psychological, academic, and economic impact of COVID-19 on college students in the epicenter of the pandemic. Emerging Adulthood, 10(2), 473–490. https://doi.org/10.1177/21676968211066657
- Riva, E., Freeman, R., Schrock, L., Jelicic, V., Ozer, C.-T., & Caleb, R. (2020). Student wellbeing in the teaching and learning environment: A study exploring student and staff perspectives. Higher Education Studies, 10(4), 103. https://doi.org/10.5539/hes.v10n4p103
- RIVM. (2021). Long COVID study. National Institute for Public Health and the Environment. Retrieved May 15, 2023, from https://www.rivm.nl/coronavirus-covid-19/onderzoek/long-covid.
- RIVM. (2022). COVID-19 quarantine and isolation. National Institute for Public Health and the Environment. Retrieved May 15, 2023, from https://www.rivm.nl/en/coronavirus-covid-19/quarantine-and-isolation.
- RIVM. (n.d.). Long COVID. National Institute for Public Health and the Environment. Retrieved June 14, 2023, from https://www.rivm.nl/en/coronavirus-covid-19/long-covid.
- Rosenberg, C. (2002). The tyranny of diagnosis: Specific entities and individual experience. 80(2), 237–260. https://doi.org/10.1111/1468-0009.t01-1-00003
- Rushforth, A., Ladds, E., Wieringa, S., Taylor, S., Husain, L., & Greenhalgh, T. (2021). Long COVID – The illness narratives. Social Science & Medicine, 286, 114326. https://doi.org/10.1016/j.socscimed.2021.114326
- Russell, D., Spence, N. J., Chase, J.-A. D., Schwartz, T., Tumminello, C. M., & Bouldin, E. (2022). Support amid uncertainty: Long COVID illness experiences and the role of online communities. SSM - Qualitative Research in Health, 2, 100177. https://doi.org/10.1016/j.ssmqr.2022.100177
- Sakalys, J. A. (2003). Restoring the patient’s voice: The therapeutics of illness narratives. Journal of Holistic Nursing, 21(3), 228–241. https://doi.org/10.1177/0898010103256204
- Saxena, S., Skirrow, H., & Wighton, K. (2021). Should the UK vaccinate children and adolescents against COVID-19? BMJ, 374, n1866. https://doi.org/10.1136/bmj.n1866
- Subramanian, A., Nirantharakumar, K., Hughes, S., Myles, P., Williams, T., Gokhale, K. M., Taverner, T., Chandan, J. S., Brown, K., Simms-Williams, N., Shah, A. D., Singh, M., Kidy, F., Okoth, K., Hotham, R., Bashir, N., Cockburn, N., Lee, S. I., Turner, G. M., … Haroon, S. (2022). Symptoms and risk factors for long COVID in non-hospitalized adults. Nature Medicine, 28(8), 1706. https://doi.org/10.1038/s41591-022-01909-w
- Tan, C. (2020). The impact of COVID-19 on student motivation, community of inquiry and learning performance. Asian Education and Development Studies, 10(2), 308–321. https://doi.org/10.1108/AEDS-05-2020-0084
- van Dijk, T. (2021). For many students, Long COVID is a big problem. TU Delft. Retrieved May 15, 2023, https://www.delta.tudelft.nl/article/many-students-long-covid-big-problem.
- Venkat, B. J. (2021). At the limits of cure. Duke University Press.
- Ware, N. (1992). Suffering and the social construction of illness: The delegitimation of illness experience in chronic fatigue syndrome. Medical Anthropology Quarterly, 6(4), 347–361.
- WHO. (2021). A clinical case definition of post COVID-19 condition by a Delphi consensus, 6 October 2021. World Health Organization. Retrieved May 15, 2023, from https://www.who.int/publications-detail-redirect/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021.1.
- WHO. (2022). Coronavirus disease (COVID-19): Home care for families and caregivers. World Health Organization. Retrieved May 15, 2023, from https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-covid-19-home-care-for-families-and-caregivers.
- Zimmermann, P., Pittet, L. F., & Curtis, N. (2022). Long COVID in children and adolescents. BMJ, 376(o143), 1–2. https://doi.org/10.1136/bmj.o143.