1. Introduction
Obesity in childhood and adolescence has increased worldwide and is being considered a public health issue [Citation1]. Obesity is associated with a chronic proinflammatory state and many comorbidities, including, metabolic syndrome (MS) and nonalcoholic fatty liver diseases (NAFLD) [Citation2,Citation3]. Enlarged adipose tissue is a consequence of multifactorial conditions such as genetic and lifestyle factors including the increase in ultra-processed and high caloric food consumption and a decrease in physical activity [Citation4,Citation5].
The expansion of adipose tissue promotes dysregulation of adipokine action, increasing the secretion of proinflammatory (i.e. leptin, resistin, plasminogen activator inhibitor-1, vistatin, angiotensin, tumor necrosis factor-alpha, interleukin 6) and concomitant reduction the anti-inflammatory adipokines like (adiponectin and interleukin 10). This pro-inflammatory state is considered key to the development of comorbidities related to obesity, such as MS [Citation6].
The World Health Organization (WHO) defines MS as a pathological condition characterized by excessive abdominal obesity, insulin resistance, hypertension, and hyperlipidemia and its high prevalence around the world has today become a truly global challenge [Citation1,Citation7]. In fact, in adolescents with obesity, the prevalence of MS can reach up to 60%, which may disrupt its control in long-term weight loss interventions, with insulin resistance and visceral fatty being strong predictors [Citation8].
Furthermore, the hyperleptinemic state is a common factor present in obesity in adolescents. The hyperleptinemic state is associated with disruption of neuroendocrine regulation of energy balance, atherosclerosis in early stage of the life, impairment on lung function and depression symptoms. In addition, it may impair the effects of interdisciplinary weight loss approach in the long term considering the pediatric population [Citation9–12].
Inversely, the hypoadiponectinemia present in obesity can be reversed after leptin concentration was normalized with approximately 10% of weight loss. It is suggested that the balance between leptin and adiponectin may orchestrate the impact of weight loss therapy in adolescents with obesity and MS. In fact, previously, our research team showed that the adiponectin/leptin ratio is more effective as a biomarker of inflammation than these adipokines itself and should be considered in clinical practice [Citation13–15]. Healthcare professionals must know what is behind the obesity phenotype in order to achieve reasonable goals in each patient and to define what strategy in each area should be used in order to improve not just body weight but body composition, inflammation profile, and metabolic disorders.
Importantly, it has been shown that the impact of weight loss therapy in adolescents with MS occurs as a dependent manner considering of the presence of low or high number of altered parameters. Individuals with MS might need a longer time of multidisciplinary therapy to obtain similar results to those who do not have MS and to normalize the parameters that are altered such as blood pressure, dyslipidemia, insulin resistance, and so on [Citation14]. Thus, this needs to be observed by the interdisciplinary team to find the better approach to treat this population.
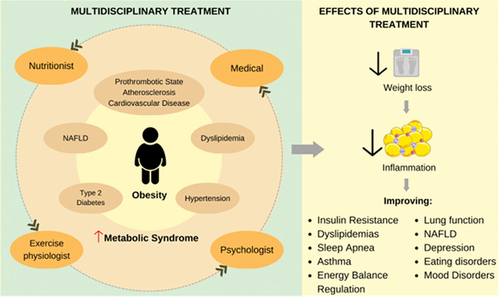
In the past 30 years an effort to understand the pathophysiology of obesity, MS and other co-morbidities in adolescents with obesity was developed by our research team and others. It was shown that this pediatric population present a constellation of altered parameters and conditions including insulin resistance, dyslipidemias, sleep apnea, asthma, lung function, NAFLD, depressive symptoms, eating disorders, together, contributing to a poor quality of life. On the other hand, the purposed multidisciplinary approach in the long term, including clinical, psychological, nutritional, and exercise approach was effective to reduce all the above-mentioned disorders, contributing to enhance the control of energy balance; inflammatory state, improving the quality of life and avoiding the development of yo-yo effects and many co-morbidities [Citation2,Citation3,Citation9–12,Citation14,Citation16,Citation17].
The presence of many co-morbidities coexisting with obesity and MS related to pediatric population lead to our understanding that the best approach to treat these diseases is holistic, including medical professionals, psychologists, nutritionists, and exercise physiologists all working together (). Pediatricians and endocrinologists have an important role in diagnosing and treating present illnesses of the patient as well guiding the multidisciplinary team regarding the global health goals of patients; nutritionists must identify inappropriate eating habits and guide children and family members on how is the best way to achieve progressive changes in food habits, by nutritional education sections, as well as to establish individual and family nutritional goals; psychologists should identify the main symptoms of emotional conditions that can be triggers for eating disorders and treat (during individual or group sections) the main issues regarding binomial emotion and food; the exercise physiologist must promote negative energy balance by increasing physical exercise and physical activity, taking into account the child’s preferences and possibilities encouraging the family to become more physically active. Although each area needs to establish their own goals for the patient, the patient must be seen in a holistic manner, and the multidisciplinary team must interact to promote a one-language approach.
Figure 1. The inflammatory state resulting from the expansion of adipose tissue in obesity is the key factor for the development of metabolic complications such as type 2 diabetes (DM2), hypertension, dyslipidemia, nonalcoholic fatty liver steatosis (NAFLD), atherosclerosis, and consequently increases the risk of developing the Metabolic Syndrome. The multidisciplinary treatment in long term, including clinical, psychological, nutritionist and exercise physiologist can contribute to enhance the inflammatory state, control of energy balance, improving many comorbidities and consequently improving the quality of life.
The main targets in the pediatric population are the patient itself, family members, school, and communities. Obesity and MS have multiple etiologies, thus, offering health care to children without enrolling parents/primary caregivers responsible for their nutrition or without the government provide public health measures to ensure food security is not enough. Therefore, governmental and non-governmental actions need to be involved as a prevention measure.
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Additional information
Funding
References
- WHO: Obesity and overweight. World Health Organization; 2021 Jun 9 [cited 2023 Mar 24]. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- de Piano A, Tock L, Carnier J, et al. Negative correlation between neuropeptide Y/agouti-related protein concentration and adiponectinemia in nonalcoholic fatty liver disease obese adolescents submitted to a long-term interdisciplinary therapy. Metabolism. 2010 May;59(5):613–619.
- Dâmaso AR, de Piano A, Campos RM, et al. Multidisciplinary approach to the treatment of obese adolescents: effects on cardiovascular risk factors, inflammatory profile, and neuroendocrine regulation of energy balance. Int J Endocrinol. 2013;2013:541032. doi: 10.1155/2013/541032
- Katzmarzyk PT, Barreira TV, Broyles ST, et al. Relationship between lifestyle behaviors and obesity in children ages 9-11: results from a 12-country study. Obesity (Silver Spring). 2015 Aug;23(8):1696–1702.
- Corgosinho FC, Almeida SS, Tock L, et al. LEPR polymorphism may affect energy balance during weight loss among Brazilians obese adolescents. Neuropeptides. 2017 Dec;66:18–24.
- Saltiel AR, Olefsky JM. Inflammatory mechanisms linking obesity and metabolic disease. J Clin Invest. 2017 Jan 3;127(1):1–4. doi: 10.1172/JCI92035
- Saklayen MG. The global epidemic of the metabolic syndrome. Curr Hypertens Rep. 2018 Feb 26;20(2):12. doi: 10.1007/s11906-018-0812-z
- Graf C, Ferrari N. Metabolic syndrome in children and adolescents. Visc Med. 2016;32(5):357–362. doi: 10.1159/000449268
- Leão da Silva P, de Mello MT, Cheik NC, et al. Reduction in the leptin concentration as a predictor of improvement in lung function in obese adolescents. Obes Facts. 2012;5(6):806–820. doi: 10.1159/000345840
- Sanches PL, de Mello MT, Elias N, et al. Hyperleptinemia: implications on the inflammatory state and vascular protection in obese adolescents submitted to an interdisciplinary therapy. Inflammation. 2014 Feb;37(1):35–43.
- Carvalho-Ferreira JP, Masquio DC, da Silveira Campos RM, et al. Is there a role for leptin in the reduction of depression symptoms during weight loss therapy in obese adolescent girls and boys? Peptides. 2015 Mar;65:20–28.
- Kravchychyn ACP, Campos RMDS, Corgosinho FC, et al. The long-term impact of high levels of alpha-melanocyte-stimulating hormone in energy balance among obese adolescents. Ann Nutr Metab. 2018;72(4):279–286. doi: 10.1159/000488005
- Dâmaso AR, de Piano A, Sanches PL, et al. Hyperleptinemia in obese adolescents deregulates neuropeptides during weight loss. Peptides. 2011 Jul;32(7):1384–1391.
- Masquio DC, de Piano A, Campos RM, et al. The role of multicomponent therapy in the metabolic syndrome, inflammation and cardiovascular risk in obese adolescents. Br J Nutr. 2015 Jun 28;113(12):1920–1930. doi: 10.1017/S0007114515001129
- Ferreira YAM, Kravchychyn ACP, Vicente SECF, et al. Influence of magnitude of weight loss on Adipo/lep ratio in adolescents with obesity undergoing multicomponent therapy. Cytokine. 2020 Jul;131:155111.
- Roche J, Corgosinho FC, Isacco L, et al. A multidisciplinary weight loss intervention in obese adolescents with and without sleep-disordered breathing improves cardiometabolic health, whether SDB was normalized or not. Sleep Med. 2020 Nov;75:225–235.
- Gallè F, Valerio G, Daniele O, et al. Multidisciplinary treatment for childhood obesity: a two-year experience in the Province of Naples, Italy. Children (Basel). 2022 Jun 4;9(6):834. doi: 10.3390/children9060834
