Euthyroidism can be postulated to be comprised of biochemical euthyroidism and clinical euthyroidism [Citation1]. It would naturally be anticipated that these states would generally coexist, but this does not seem to be the case universally. This dichotomy presents a challenge for the treating physician and the patient affected by hypothyroidism.
If the definition of euthyroidism is a serum TSH within the reference interval established in individuals free of thyroid disease [Citation2], then this is generally an achievable goal, albeit not achieved in all treated patients, and requiring ongoing adjustments in thyroid hormone dosage [Citation3]. There is some recent evidence that a TSH at goal is being achieved in 80% of treated patients [Citation4], compared with closer to 60% in prior studies (reviewed in [Citation5]). If euthyroidism also encompasses free thyroxine (FT4) and total triiodothyronine (T3) levels within reference intervals established in those free of thyroid disease, this is potentially more problematic as levothyroxine (LT4) treatment tends to produce high-normal or elevated FT4 concentrations and low-normal or low T3 concentrations [Citation6–8]. The ‘holy grail’ of euthyroidism, however, is likely to be the perfect balance of thyroid hormones at a cellular level [Citation9,Citation10], which has been most thoroughly investigated in animal models [Citation11,Citation12].
Patients with untreated overt hypothyroidism can have multiple signs and symptoms which are well-described [Citation1]. In addition to the anticipated changes in the integument, temperature regulation, cardiorespiratory functioning, and the reproductive system, there can be neurocognitive dysfunction, anxiety, and depression. For example, neurocognitive testing and questionnaires assessing depression show deficits in patients with untreated hypothyroidism (average TSH levels 44.8 mIU/L), which correlates with altered gray matter morphology and altered functional MRI findings in the brain [Citation13]. Broadly, such changes are reversed with the treatment of hypothyroidism [Citation1].
Clinical euthyroidism, thus, could encompass the normalization of multiple parameters [Citation1]. These parameters could include signs such as heart rate and weight, other biomarkers of thyroid status, such as lipid profile, ferritin, sex hormone-binding globulin, and angiotensin converting enzyme levels, and also normalization of patient-reported symptoms [Citation14–16]. Presumably these would be mediated through a normal gene expression profile in multiple relevant tissues.
However, vital signs and measures such as body weight are very nonspecific. In addition, biomarkers of thyroid status, such as lipid profile, ferritin, sex hormone-binding globulin, and angiotensin converting enzyme levels are notoriously insensitive to subtle changes in thyroid hormone levels, and their relationship with other parameters associated with thyroid status has not been well studied. Genes profiles in various tissues can generally only be assessed in animal models [Citation17], with blood being the only easily accessible tissue in humans [Citation18]. Unfortunately, clinical euthyroidism, based on patient-reported symptoms or patient satisfaction, is not guaranteed even if the TSH is normal [Citation19,Citation20]. The relationship between FT4 and T3 and patient satisfaction with therapy is unclear, not seemingly related to thyroid hormone levels or dose in some studies [Citation21–23], and related to higher dose in other analyses [Citation24].
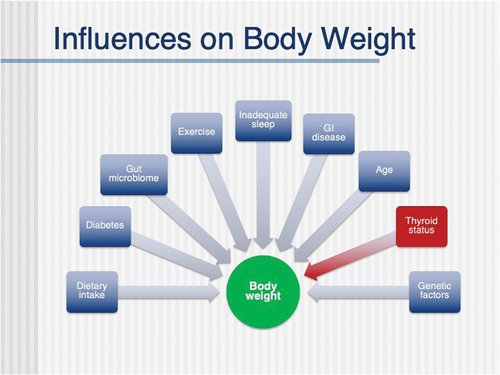
Chief among the concerns of patients being treated for hypothyroidism are the following unresolved signs and symptoms: weight gain, fatigue, and difficulty with memory and concentration (frequently described as brain fog) [Citation25,Citation26] (see ). Other concerns such as hair loss, decreased physical ability, need for increased sleep, dry skin, body aches, and increased cold sensitivity are perhaps less frequent. It is clear that these complaints are not rectified by a normal TSH, or even a TSH in the lower part of the normal range [Citation21,Citation22,Citation27,Citation28].
Table 1. Quotes from patients with normal TSH levels about their hypothyroidism (slightly modified to preserve anonymity).
Based on the thyroid hormone profile differences between endogenous euthyroidism and levothyroxine-treated patients with a normal TSH (lower T3, higher FT4), a multitude of trials of ‘combination therapy’ have been conducted (reviewed in [Citation9]). These trials involve adding liothyronine (LT3) to LT4 therapy and have had various limitations, but thus far have not clearly shown improvement in quality of life or performance and cognition with combination therapy. Some themes emerging from these trials, however, include that combination therapy may be more beneficial in the subgroup of patients who are most symptomatic while taking LT4 monotherapy [Citation29,Citation30] and in those that have less residual endogenous thyroid function [Citation31], that patients may prefer T3 doses that result in iatrogenic hyperthyroidism [Citation32,Citation33], and a placebo effect may be seen [Citation34,Citation35]. Better designed trials that are either underway or planned may clarify whether combination therapy delivered in a particular manner does ameliorate most symptoms of hypothyroidism in the majority of symptomatic patients.
However, an additional challenge in addressing the symptoms of patients with treated hypothyroidism is correctly identifying the underlying cause of the symptoms [Citation36]. It is understandable that a patient being treated for hypothyroidism attributes their symptoms to lack of resolution of the symptoms of hypothyroidism [Citation36]. However, this may not necessarily be the case. For example, with respect to the common complaint of weight gain, this could certainly be due to hypothyroidism, but multiple other reasons could be primary or contributing causative factors. Such factors might include insufficient exercise, excessive caloric intake, inadequate sleep and genetic influences (see ). Clearly, if any symptom is not actually due to sub-optimally treated hypothyroidism, then it will not resolve with manipulation of thyroid hormone dose.
Similarly, and along these same lines, certain symptoms may lead to patients being screened for and diagnosed with hypothyroidism, without these symptoms being due to hypothyroidism [Citation37]. A recent study surveyed patients with treated hypothyroidism, including using a survey, the Patient Health Questionnaire-15, that is a screening tool for somatization disorder [Citation38]. Somatization disorder was present in 59% of the hypothyroid population compared with 7% of the general population. This study nicely illustrates the complexity of accurate attribution of symptoms and the overlap between symptoms caused by diverse conditions. Additionally, it could point to potential symptom relief by therapy for somatization disorders, rather than adjustment of thyroid hormone. For example, cognitive behavioral therapy has been shown to improve health-related quality of life [Citation39] and may potentially relieve brain fog [Citation26] in patients being treated for hypothyroidism.
In addition, synthetic combination therapy, the success of which has been so ardently hoped for, does not resolve the symptoms reported by patients [Citation38,Citation40,Citation41]. There may, however, even be a suggestion that combination therapy, achieved using desiccated thyroid extract, may be preferred by patients [Citation40], even though it also does not appear to fully ameliorate patient symptoms. In addition, the use of desiccated thyroid extract has been increasing over time [Citation42].
If symptoms are, in fact, due to flaws in therapy and failure to replicate endogenous euthyroidism, then the question is how can delivery of LT4, LT4/LT3 mixtures, or other treatments be more successful. Certainly, the adjustment of LT4 dosage does not seem to hold promise. Aiming for TSH values within particular sections of the normal range does not seem to improve parameters such as quality of life or body mass index [Citation21,Citation22,Citation27,Citation28]. Furthermore, such TSH goals do not provide a more physiologic serum thyroid profile, as they do not circumvent the high FT4 values that are generally achieved with LT4 therapy. Given that a percentage of patients treated with LT4 do not achieve a normal TSH, attention to normalization of TSH may at first consideration seem to be a ‘low-hanging fruit’ with respect to addressing residual symptoms. However, a recent study of patients filling their LT4 prescriptions, who were asked to complete a survey about their practices surrounding taking LT4 and their health-related quality of life, did not show any association between LT4 adherence, TSH values, and health-related quality of life [Citation43].
With respect to combination therapy, there do seem to be additional avenues to pursue such as selection of appropriate LT4/LT3 ratios, and more frequent administration of LT3 than once daily [Citation9]. However, perhaps the greatest promise may lie with extended-release T3 preparations which may better replicate normal thyroid physiology. Endogenous euthyroidism is associated with modest fluctuations of approximately 0.3 pmol/L in T3 levels during the course of the day [Citation44]. This compares with dramatic changes in T3 levels of approximate 1.6 pmol/L ng/dL or up to 40% with once daily T3 doses [Citation45].
Expert Opinion
In addition to better therapies, another need may also be to identify more refined means of monitoring therapy, in addition to TSH levels. FT4 levels vary with respect to the timing of LT4 and combined LT4/LT3 therapy. T3 concentrations may be more meaningful if extended-release T3 is being employed. Other novel thyroid hormone metabolites may also lend insight into thyroid status [Citation46]. Patient-reported outcomes may also be helpful [Citation9,Citation14,Citation47]. In the future, it may also be possible to examine gene profiles in accessible tissues. For example, gene profiles in blood cells such as leukocytes could be studied as a potential means to assess and guide thyroid hormone replacement.
Hopefully, the goal of achieving euthyroidism for all is within reach. However, this likely requires acknowledgment of the complexity of symptom etiology and resolution [Citation48]. Combination therapy will most likely not be either the primary approach or the only approach needed. Potentially it may be employed when needed, in conjunction with thyroid hormone optimization, attention to lifestyle issues, addressing medical comorbidities, regular exercise, and if needed, use of cognitive therapy, to name but a few approaches.
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Additional information
Funding
References
- Jonklaas J. Optimal thyroid hormone replacement. Endocr Rev. 2022;43(2):366–404. doi: 10.1210/endrev/bnab031
- Hollowell JG, Staehling NW, Flanders WD, et al. Serum TSH, T4, and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab. 2002;87(2):489–499. doi: 10.1210/jcem.87.2.8182
- Jonklaas J, Bianco, AC, Bauer, AJ, et al. Guidelines for the treatment of hypothyroidism: prepared by the American thyroid association task force on thyroid hormone replacement. Thyroid: Offic J Am Thyroid Association. 2014;24(12):1670–1751. doi: 10.1089/thy.2014.0028
- Bianco AC, Bao Y, Antunez Flores O, et al. Levothyroxine treatment adequacy and formulation changes in patients with hypothyroidism: a retrospective study of real-world data from the United States. Thyroid®. 2023;33(8):940–949. doi: 10.1089/thy.2022.0382
- Jonklaas J, Razvi S. Reference intervals in the diagnosis of thyroid dysfunction: treating patients not numbers. Lancet Diabetes Endocrinol. 2019;7(6):473–483. doi: 10.1016/S2213-8587(18)30371-1
- Jonklaas J, Davidson B, Bhagat S, et al. Triiodothyronine levels in athyreotic individuals during levothyroxine therapy. JAMA. 2008;299(7):769–777. doi: 10.1001/jama.299.7.769
- Gullo D, Latina A, Frasca F, et al. Levothyroxine monotherapy cannot guarantee euthyroidism in all athyreotic patients. PLoS One. 2011;6(8):e22552. doi: 10.1371/journal.pone.0022552
- Alevizaki M, Mantzou E, Cimponeriu AT, et al. Ist TSH ein geeigneter Indikator für eine adäquate Schilddrüsenhormon-Substitution? Wien Klin Wochenschr. 2005;117(18):636–640. doi: 10.1007/s00508-005-0421-0
- Jonklaas J, Bianco, AC, Cappola, AR, et al. Evidence-based use of levothyroxine/liothyronine Combinations in treating hypothyroidism: a consensus document. Thyroid: Offic J Am Thyroid Association. 2021;31(2):156–182. doi: 10.1089/thy.2020.0720
- Casula S, Ettleson MD, Bianco AC. Are we restoring thyroid hormone signaling in levothyroxine-treated patients with residual symptoms of hypothyroidism? Endocr Pract. 2023;29(7):581–588. doi: 10.1016/j.eprac.2023.04.003
- Werneck de Castro JP, Fonseca TL, Ueta CB, et al. Differences in hypothalamic type 2 deiodinase ubiquitination explain localized sensitivity to thyroxine. J Clin Invest. 2015;125(2):769–781. doi: 10.1172/JCI77588
- Jo S, Fonseca TL, Bocco BMLC, et al. Type 2 deiodinase polymorphism causes ER stress and hypothyroidism in the brain. J Clin Invest. 2019;129(1):230–245. doi: 10.1172/JCI123176
- Su W, Zhao L, Bao S, et al. Alterations in Gray matter Morphology and Functional Connectivity in adult patients with newly diagnosed untreated hypothyroidism. Thyroid®. 2023;33(7):791–803. doi: 10.1089/thy.2022.0476
- Cramon PK, Bjorner JB, Groenvold M, et al. Implementation of thyroid-related patient-reported outcomes in routine clinical practice. Front Endocrinol. 2022;13:1000682. doi: 10.3389/fendo.2022.1000682
- Zulewski H, Muller B, Exer P, et al. Estimation of tissue hypothyroidism by a new clinical score: evaluation of patients with various grades of hypothyroidism and controls. J Clin Endocrinol Metab. 1997;82(3):771–776. doi: 10.1210/jc.82.3.771
- Canaris GJ, Steiner JF, Ridgway EC. Do traditional symptoms of hypothyroidism correlate with biochemical disease? J Gen Intern Med. 1997;12(9):544–550. doi: 10.1046/j.1525-1497.1997.07109.x
- Feng X, Jiang Y, Meltzer P, et al. Thyroid hormone regulation of hepatic genes in vivo detected by complementary DNA microarray. Mol Endocrinol. 2000;14(7):947–955. doi: 10.1210/mend.14.7.0470
- Massolt ET, Chaker L, Visser TJ, et al. Serum microRNA profiles in athyroid patients on and off levothyroxine therapy. PLoS One. 2018;13(4):e0194259. doi: 10.1371/journal.pone.0194259
- Saravanan P, Chau W-F, Roberts N, et al. Psychological well-being in patients on ‘adequate’ doses of l-thyroxine: results of a large, controlled community-based questionnaire study. Clin Endocrinol (Oxf). 2002;57(5):577–585. doi: 10.1046/j.1365-2265.2002.01654.x
- Wekking EM, Appelhof BC, Fliers E, et al. Cognitive functioning and well-being in euthyroid patients on thyroxine replacement therapy for primary hypothyroidism. Eur J Endocrinol. 2005;153(6):747–753. doi: 10.1530/eje.1.02025
- Samuels MH, Kolobova I, Niederhausen M, et al. Effects of altering levothyroxine (L-T4) doses on quality of life, mood, and cognition in L-T4 treated subjects. J Clin Endocrinol Metab. 2018;103(5):1997–2008. doi: 10.1210/jc.2017-02668
- Samuels MH, Kolobova I, Niederhausen M, et al. Effects of altering levothyroxine dose on energy expenditure and body composition in subjects treated with LT4. J Clin Endocrinol Metab. 2018;103(11):4163–4175. doi: 10.1210/jc.2018-01203
- Eskelinen SI, Vahlberg TJ, Isoaho RE, et al. Associations of thyroid-stimulating hormone and free thyroxine concentrations with health and life satisfaction in elderly adults. Endocr Pract. 2007;13(5):451–457. doi: 10.4158/EP.13.5.451
- Akirov A, Fazelzad R, Ezzat S, et al. A systematic review and meta-analysis of patient preferences for combination thyroid hormone treatment for hypothyroidism. Front Endocrinol. 2019;10:477. doi: 10.3389/fendo.2019.00477
- Ettleson MD, Raine A, Batistuzzo A, et al. Brain fog in hypothyroidism: understanding the patient’s perspective. Endocr Pract. 2022;28(3):257–264. doi: 10.1016/j.eprac.2021.12.003
- Samuels MH, Bernstein LJ. Brain fog in hypothyroidism: what is it, how is it measured, and what can be Done about it. Thyroid: Offic J Am Thyroid Association. 2022;32(7):752–763. doi: 10.1089/thy.2022.0139
- Walsh JP, Ward LC, Burke V, et al. Small changes in thyroxine dosage do not produce measurable changes in hypothyroid symptoms, well-being, or quality of life: results of a double-blind, randomized clinical trial. J Clin Endocrinol Metab. 2006;91(7):2624–2630. doi: 10.1210/jc.2006-0099
- Boeving A, Paz-Filho G, Radominski, RB, et al. Low-normal or high-normal thyrotropin target levels during treatment of hypothyroidism: a prospective, comparative study. Thyroid: Offic J Am Thyroid Association. 2011;21(4):355–360. doi: 10.1089/thy.2010.0315
- Panicker V, Saravanan P, Vaidya B, et al. Common variation in the DIO2 gene predicts baseline psychological well-being and response to combination thyroxine plus triiodothyronine therapy in hypothyroid patients. J Clin Endocrinol Metab. 2009;94(5):1623–1629. doi: 10.1210/jc.2008-1301
- Shakir MKM, Brooks DI, McAninch EA, et al. Comparative effectiveness of levothyroxine, desiccated thyroid extract, and levothyroxine+Liothyronine in hypothyroidism. J Clin Endocrinol Metab. 2021;106(11):e4400–e4413. doi: 10.1210/clinem/dgab478
- DiStefano J, Jonklaas J. Predicting Optimal combination LT4 + LT3 therapy for hypothyroidism based on residual thyroid function. Front Endocrinol. 2019;10:746. doi: 10.3389/fendo.2019.00746
- Appelhof BC, Fliers E, Wekking EM, et al. Combined therapy with levothyroxine and liothyronine in two ratios, compared with levothyroxine monotherapy in primary hypothyroidism: a double-blind, randomized, controlled clinical trial. J Clin Endocrinol Metab. 2005;90(5):2666–2674. doi: 10.1210/jc.2004-2111
- Bunevicius R, Kažanavičius G, Žalinkevičius R, et al. Effects of thyroxine as compared with thyroxine plus triiodothyronine in patients with hypothyroidism. N Engl J Med. 1999;340(6):424–429. doi: 10.1056/NEJM199902113400603
- Clyde PW, Harari AE, Getka EJ, et al. Combined levothyroxine plus liothyronine compared with levothyroxine alone in primary hypothyroidism: a randomized controlled trial. JAMA. 2003;290(22):2952–2958. doi: 10.1001/jama.290.22.2952
- Saravanan P, Simmons DJ, Greenwood R, et al. Partial substitution of thyroxine (T4) with tri-iodothyronine in patients on T4 replacement therapy: results of a large community-based randomized controlled trial. J Clin Endocrinol Metab. 2005;90(2):805–812. doi: 10.1210/jc.2004-1672
- Jansen HI, Boelen A, Heijboer AC, et al. Hypothyroidism: the difficulty in attributing symptoms to their underlying cause. Front Endocrinol. 2023;14:1130661. doi: 10.3389/fendo.2023.1130661
- Bould H, Panicker V, Kessler D, et al. Investigation of thyroid dysfunction is more likely in patients with high psychological morbidity. Fam Pract. Fam Pract. 2012;29(2):163–167. doi: 10.1093/fampra/cmr059
- Perros P, Nagy EV, Papini E, et al. Hypothyroidism and somatization: results from E-Mode patient self-assessment of thyroid therapy, a cross-sectional, international online patient survey. Thyroid®. 2023;33(8):927–939. doi: 10.1089/thy.2022.0641
- Rezaei S, Abedi P, Maraghi E, et al. The effectiveness of cognitive- behavioral therapy on quality of life in women with hypothyroidism in the reproductive age: a randomized controlled trial. Thyroid Res. 2020;13(1):6. doi: 10.1186/s13044-020-00080-z
- Peterson SJ, Cappola, AR, Castro, MR, et al. An online survey of hypothyroid patients demonstrates prominent dissatisfaction. Thyroid: Offic J Am Thyroid Association. 2018;28(6):707–721. doi: 10.1089/thy.2017.0681
- Perros P, Hegedüs L, Nagy, EV, et al. The impact of hypothyroidism on satisfaction with care and treatment and everyday living: results from E-Mode patient self-assessment of thyroid therapy, a cross-sectional, international online patient survey. Thyroid: Offic J Am Thyroid Association. 2022;32(10):1158–1168. doi: 10.1089/thy.2022.0324
- Ettleson MD, Ibarra S, Wan W, et al. Demographic, healthcare access, and dietary factors associated with thyroid hormone treatments for hypothyroidism. J Clin Endocrinol Metab. 2023. doi:10.1210/clinem/dgad331.
- Mehuys E, Lapauw B, T’Sjoen G, et al. Investigating levothyroxine use and Its Association with thyroid health in patients with hypothyroidism: a community pharmacy study. Thyroid®. 2023;33(8):918–926. doi: 10.1089/thy.2023.0066
- Russell W, Harrison RF, Smith N, et al. Free triiodothyronine has a distinct circadian rhythm that is delayed but parallels thyrotropin levels. J Clin Endocrinol Metab. 2008;93(6):2300–2306. doi: 10.1210/jc.2007-2674
- Saravanan P, Siddique H, Simmons D, et al. Twenty-four hour hormone profiles of TSH, free T3 and free T4 in hypothyroid patients on combined T3/T4 therapy. Exp Clin Endocrinol Diabetes. 2007;115(4):261–267. doi: 10.1055/s-2007-973071
- Köhrle J, Lehmphul I, Pietzner M, et al. 3,5-T2—A janus-faced thyroid hormone metabolite exerts both canonical T3-mimetic endocrine and intracrine hepatic action. Front Endocrinol. 2019;10:787. doi: 10.3389/fendo.2019.00787
- Deshpande PR, Rajan S, Sudeepthi B, et al. Patient-reported outcomes: a new era in clinical research. Perspect Clin Res. 2011;2(4):137–144. doi: 10.4103/2229-3485.86879
- Mammen JS, Cooper DS. Symptoms in patients being treated for hypothyroidism: new data in a continuing controversy. Thyroid: Offic J Am Thyroid Association. 2023;33(8):887–889. doi: 10.1089/thy.2023.0307