1. Introduction
Sexual health is a fundamental component of human health, which is important to many people and their partners, and is therefore highly relevant to clinical care. Despite this, sexual health typically receives little attention in the routine care of non-communicable conditions.
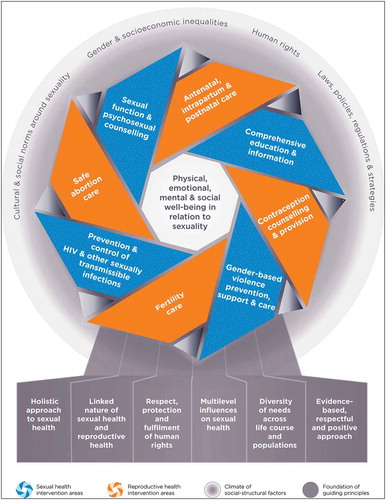
The World Health Organization (WHO) defines sexual health as ‘… a state of physical, emotional, mental and social well-being in relation to sexuality; it is not merely the absence of disease, dysfunction or infirmity’ [Citation1]. WHO defines sexuality as ‘a central aspect of being human throughout life encompassing sex, gender identities and roles, sexual orientation, eroticism, pleasure, intimacy, and reproduction. Sexuality is experienced and expressed in thoughts, fantasies, desires, beliefs, attitudes, values, behaviors, practices, roles, and relationships. While sexuality can include all of these dimensions, not all of them are always experienced or expressed. Sexuality is influenced by the interaction of biological, psychological, social, economic, political, cultural, legal, historical, religious, and spiritual factors’ [Citation1]. WHO recently released a framework which presents eight intervention areas for the inter-related concepts of sexual and reproductive health () [Citation2]. Importantly, the new framework emphasizes the link between sexual health and reproductive health and that these are important and lifelong components of wellbeing.
Figure 1. WHO framework for operationalizing sexual health and its linkages to reproductive health.
Reprinted from World Health Organization: Sexual health and its linkages to reproductive health: an operational approach. Geneva: World Health Organization; 2017. License: CC BY-NC-SA 3.0 IGO.
Health-care practitioners (HCPs) who manage individuals with inflammatory arthritis are familiar with the multidimensional (and often multidisciplinary) care these individuals frequently require over many decades [Citation3]. In addition to musculoskeletal impairments, HCPs often need to address concurrent issues including associated co-morbidities (e.g. elevated cardiovascular risk), psychological impacts (e.g. depression) and functional limitations (e.g. diminished work participation). In providing holistic care, HCPs need to be adept at taking a sexual history and discussing sexual and reproductive health issues or concerns. This is highlighted by recent examples of clinical encounters from the first author’s consultant rheumatology practice:
a young man with suspected reactive arthritis needing diagnosis and treatment of a sexually transmitted disease, and counseling about how to prevent recurrent infections;
a young woman with newly diagnosed rheumatoid arthritis needing advice about initiation and continuation of effective contraception in preparation for methotrexate treatment;
a young woman with established rheumatoid arthritis requesting pre-pregnancy counseling including discussion of fertility, conception, and management of her arthritis during pregnancy and breastfeeding;
a middle-aged man taking leflunomide for psoriatic arthritis with a sudden dramatic rise in hepatic enzymes, who tested positive for recently acquired Hepatitis B from an unprotected sexual encounter.
2. Why should practitioners take a sexual history and explore sexual health, and in whom?
As outlined by WHO, sexual health is relevant to all patients regardless of gender, sexual orientation or level of disability. The clinical scenarios provided above are just a few examples of why taking a sexual history is frequently relevant in patients with auto-immune disease, either at the first consultation or during subsequent encounters. Protection against sexually transmitted infections (STIs) and issues surrounding fertility, contraception, pregnancy, and post-natal care are all important topics; however, this editorial focuses on sexual dysfunction in patients with auto-immune disease.
For patients and HCPs, sexual dysfunction and intimate relationship concerns are potentially difficult or sensitive topics to raise and discuss openly. Evidence suggests these issues are relatively common among people with inflammatory arthritis. In a systematic review of 55 studies from Europe, the Middle East, North America, Africa, Oceania and South America, examining patients aged 20 to 69 years with conditions including rheumatoid arthritis, scleroderma, ankylosing spondylitis, systemic lupus erythematosus and Sjogren’s syndrome, we identified consistent evidence of inflammatory arthritis negatively impacting intimate relationships and sexual function for both genders, at a higher proportion than their otherwise healthy peers [Citation4].
The limited information available suggests that patients are reluctant to raise the topic of sexual dysfunction but do nonetheless express the desire to speak about it with an HCP, with a preference shown for their treating doctor [Citation5]. In order to identify sexual problems and appropriately engage other practitioners, HCPs need to raise sexual function in a sensitive manner and discuss the patient’s concern in enough detail to determine the nature and impact of the problem and the likely contributors to the experience. For instance, a woman with severe degenerative hip disease following years of poorly controlled rheumatoid arthritis describing sexual difficulty due to an inability to abduct her hips may be best served by a referral to a physiotherapist and/or orthopedic surgeon. In contrast, sexual dysfunction due to fatigue and lowered libido may be addressed through referral to a relationship therapist or sexual counselor.
3. Causes of sexual dysfunction in inflammatory arthritis
It is likely that any discussion about sexual dysfunction will reveal multiple factors contributing to the experience, consistent with the WHO model. Scrutiny of the six qualitative studies included in our systematic review [Citation4] demonstrated that sexual function was affected by pain or the anticipation of pain, reduced joint mobility, negative body image, reduced sexual desire, erectile dysfunction and fatigue, along with the same stressors that affect the general population such as stress (including stress related to the illness itself along with the financial implications of having a chronic illness) and other general life concerns. Compromised intimate relationships were frequently reported. Although in some cases acceptance and understanding of the impact that inflammatory arthritis had on sexual function served to strengthen the bond between partners, others found that their partners poorly understood the impact of inflammatory arthritis on their ability to engage in intercourse, creating tension and fear in relationships. Despite the sexual dysfunction associated with inflammatory arthritis, women in particular often felt pressured to maintain a normal sex life. Given that sexual dysfunction is likely to be multifactorial, it follows that management of the sexual dysfunction will require a combination of interventions, provided by a variety of clinicians.
4. Barriers to the optimal management of sexual health in patients with inflammatory arthritis
Patients may be reluctant to raise the issue of sexual dysfunction due to embarrassment and may require encouragement to do so. HCPs may lack the confidence, training, skills and peer support required to address this deeply personal and complex issue. They may also believe the patient would consider it an unwelcome, intrusive or inappropriate topic of discussion. Furthermore, the taking of a sexual history requires adequate time and privacy and may require the partner or a chaperone (depending on the gender of the HCP and the patient) to be present. This may be challenging to facilitate in a busy clinical practice or hospital setting. Different HCPs may take different approaches depending on their own level of comfort, the clinical setting, the specific clinician–patient interaction, and the supports available. Approaches may include providing general information in the waiting room for patients to access, directing the patient to a brochure or web-based information which includes suggested actions, referral to psychologist, sex therapist or other appropriate HCP, or scheduling a dedicated appointment with the patient and their partner to discuss and manage the issues identified.
5. What can we do?
We can start by raising awareness of this issue. Increased awareness among HCPs including doctors, physiotherapists, occupational therapists, and rheumatology nurses would ideally occur in parallel with skills-based competencies development for interested clinicians on how to (a) raise, (b) discuss, and (c) manage sexual dysfunction. An Internet search reveals numerous helpful guides on the taking of a sexual history (e.g. www.cdc.gov/std/treatment/sexualhistory.pdf; https://pmj.bmj.com/content/80/946/444); however, many are focused more on determining and reducing risk of STIs than on sexual dysfunction per se, suggesting a lack of attention to this aspect of holistic care.
Prevention and management of sexual dysfunction goes hand-in-hand with our other efforts to reduce the long-term morbidity associated with inflammatory arthritis. This includes efforts to obtain optimum control of disease activity from early in the disease course to arrest joint destruction/deformity, address any psychological problems, and ensure physical fitness and functional joint mobility, including mobility for intercourse. We need to be aware of medications which can impact sexual function (such as many of the commonly used anti-depressants) and avoid them if possible, or at a minimum warn patients of the risk and provide education around minimizing the impact. Along the management continuum, the involvement of intimate partners can be used to facilitate their understanding of the potential impact of inflammatory arthritis on sexual function; this may in turn improve within-relationship communication and prevent relationship breakdown. Many patients with life-long conditions such as inflammatory arthritis may also benefit from self-management courses. Integration of sexual health, including sexual dysfunction, into these courses and associated resources may be helpful, delivered online or face-to-face.
Our review demonstrated high heterogeneity in outcome measurement tools relating to sexual dysfunction [Citation4]. Incorporating standardized tools for measuring sexual function in patients with inflammatory arthritis within measures of disease activity and self-reported function would serve to highlight the importance of sexual health in the overall health of the patient and capture arthritis management outcomes more comprehensively. The Oswestry Disability Questionnaire, for example, includes an item of sexual function in the context of low back related-disability [Citation6].
6. Conclusion
Sexual dysfunction is a common problem among patients with inflammatory arthritis and contributes to morbidity. Within long-term care, we suggest HCPs consider an assessment of sexual health and implementation of strategies to optimize sexual health as an integral part of their management.
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Additional information
Funding
References
- World Health Organization. Defining sexual health: report of a technical consultation on sexual health, 28-31 January 2002, Geneva. Geneva: World Health Organization; 2006.
- World Health Organization. Sexual health and its linkages to reproductive health: an operational approach. Geneva: World Health Organization; [accessed 2019 Aug 5]. Available from: https://www.who.int/reproductivehealth/publications/sexual_health/sh-linkages-rh/en/;.
- Segan JD, Briggs AM, Chou L, et al. Patient-perceived health service needs in inflammatory arthritis: a systematic scoping review. Semin Arthritis Rheum. 2017;47:765–777.
- Restoux LJ, Dasariraju SR, Ackerman IN, et al. A systematic review of the impact of inflammatory arthritis on intimate relationships and sexual function. Arthritis Care Res. 2019; (Epub ahead of print). doi:10.1002/acr.23857.
- Josefsson KA, Gard G. Sexual health in patients with rheumatoid arthritis: experiences, needs and communication with health care professionals. Musculoskeletal Care. 2012;10:76–89.
- Fairbank JC, Pynsent PB. The oswestry disability index. Spine (Phila Pa 1976). 2000;25:2940–2952.
