ABSTRACT
This paper aims to discuss the relations between the built environment and the patient’s health, considering the context of the pandemic experienced since 2020. We assessed the results of a systematic literature review to create a theoretical framework. Based on that, we evaluated the performance of five diagnostic facilities sited in São Paulo, Brazil, during the occupation phase. These buildings share a similar design programme in a way that enables a systematic qualitative assessment. We organised the design requisites in a Table of Diagnostics and Recommendations. Based on the gathered evidence, we proposed reviewing the existing guidelines to promote healthier indoor environments. Among the leading design guidelines updates are issues regarding the management of contamination risk, such as the strategic planning of circulation routes, increasing outdoor air rates, and the specification of disinfection systems. We also present measures to promote healthiness and well-being for both patients and the medical team, including improving solar access to indoor environments and physical and visual access to the outdoors.
Introduction
Diagnostic facilities are not always a part of a hospital. However, these built environments share characteristics such as building complex systems and technical specifications for medical equipment, presenting high technological density. Consequently, design solutions that support multidisciplinary services should also be encouraged whenever possible.
Thus, these environments should be capable of accommodating equipment, which is often heavy and periodically replaced. In addition, the environment must be prepared to offer adequate conditions of use, both for the medical team and patients (van Hoof, Rutten, Struck, Huisman, & Kort, Citation2015).
Therefore, during the conceptual design phase of a healthcare facility, project requirements should consider the resilience of building environments and systems. It is essential to ensure that adequate changes are made in use and technologies, thus ensuring their building systems are constantly updated.
It is worth considering, for example, buildings that accommodate integrated health and social assistance services that have multifunctional rooms and where spaces and building systems may be easily changed/modified to support future demands. This approach is essential to ensure the building’s functionality during its service life. The building requisites can change quickly, such as those observed throughout 2020 and 2021, due to the pandemic caused by the Sars-Cov-2 virus (Houghton et al., Citation2020).
Another critical issue regarding diagnostic medical services is the ageing population worldwide, who are more likely to develop chronic diseases, such as cardiovascular conditions and cancer (Marquardt, Bueter, & Motzek, Citation2014; Villanueva et al., Citation2013; WHO, Citation2008, Citation2012). Therefore, we also shall consider increasing the demand for imaging-based screening examinations in portions that present a public health problem. Examples of these exams are magnetic resonance imaging, mammography, computed tomography scans, echocardiogram, and image-guided biopsy (ANS, Citation2019; OPAS/OMS, Citation2017).
Thus, understanding the impacts of extensive medical imaging equipment on the built environment is essential to identify the specific design requirements. A room dedicated to magnetic resonance imaging, for example, would address design requirements such as space constraints, structural loads, radiofrequency shielded enclosure, vibration mitigating solutions, and dedicated air conditioning and power systems. During the conception phase, the design team shall adopt solutions that allow the replacement and maintenance of heavy equipment. In addition to that, diagnostic imaging services may also include procedures such as biopsies. Thus, the imaging area operates as a platform for simultaneous invasive interventions and the use of anaesthesia.
Materials and methods
According to Yin (Citation2018), when a complex problem arises, it is essential to consider a systemic process to identify the main issues, the actors involved, and their interrelationships. In this scenario, adopting case studies may be valuable to the analysis process. Considering an exploratory approach, in a post-doctoral research context (França, Citation2019), we carried on building performance evaluations (BPEs) to healthcare facilities during the occupation phase to assess the adequacy of the design solutions during the operations phase. We considered the following methods for the research:
Systematic Literature Review (SLR);
analysis of building programming, construction typology, operation and maintenance data, as well as the healthcare facility requisites, to determine key evaluation aspects, considering applicable legislation (ANVISA, Citation2002) and standards (ABNT, Citation2013, Citation2020);
building technical inspection (including control devices, such as lighting, temperature, humidity, particles and external air sensors); photographic documentation; checklists; verification of as-builts and design requirement guidelines (2018 existing conditions); environmental and furniture functional assessment; and occupant flux mapping; and
passive observation, for occupant behavioural and flow evaluation purposes (therefore, without interaction between the researcher and the building occupants, in compliance with the best practices for research ethics) (Ono, Ornstein, Villa, & França, Citation2018).
We summarised the findings and recommendations in the Table of Diagnostics and Recommendations (Ono, França, & Ornstein, Citation2018). Then, considering the diagnostics, we proposed an update on design requirements based on the gathered evidence.
Systematic literature review
For the Systematic Literature Review (SLR), we followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Pati & Lorusso, Citation2018). shows the parameters and the results of the search.
Figure 1. SLR protocol. Source: the authors, based on (Pati & Lorusso, Citation2018).
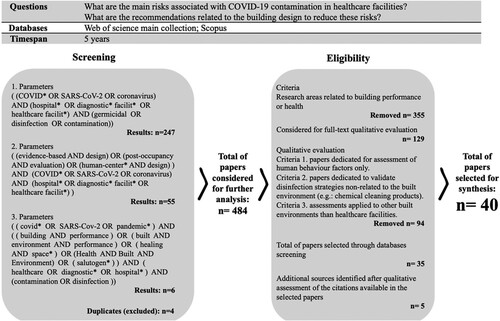
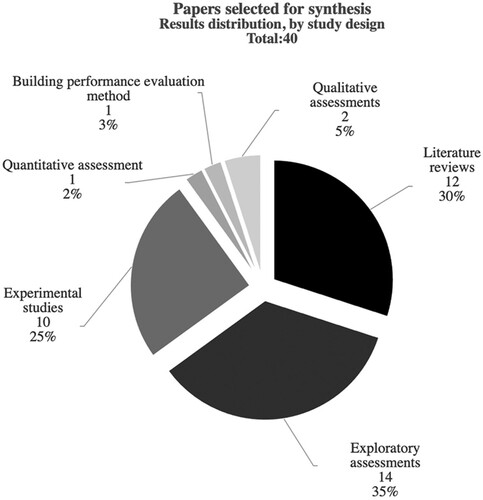
From a screening of 484 works, we selected 40 papers of interest in the context of our research. The exclusion criteria were: studies non-related to building performance or health care knowledge areas, articles dedicated to discussing strictly human behaviour disinfection strategies non-related to the built environment, such as the efficiency of chemical products and assessments applied to built environments non-related to healthcare facilities.
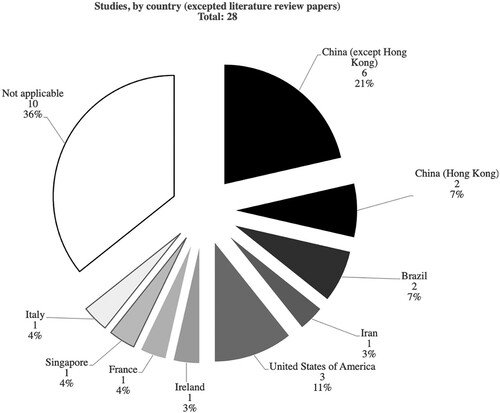
provides the distribution of the research gathered through the SLR, classified by study design. The selected papers were dedicated mainly to exploratory assessments (14; 35%), literature reviews (12; 30%) and experimental studies (10; 25%). shows that China housed the more significant number of screened studies (6; 21%) (Liu et al., Citation2020; Wang, Citation2021; Wang, Qiao, Zhou, & Yuan, Citation2020; Weng & Kau, Citation2021; Wu et al., Citation2020). followed by The United States of America (3;11%) (Gordon, Ward, Yao, & Lee, Citation2021; Redmond et al., Citation2021; Santarpia et al., Citation2020), Brazil (2; 7%) (Passos, Silveira, & Abrahão, Citation2021; Vicente et al., Citation2021) and Hong Kong, China (2; 7%) (Chan et al., Citation2020; Gormley, Aspray, Kelly, & Rodriguez-Gil, Citation2017).
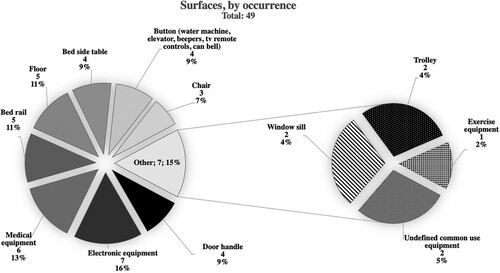
highlights the most frequently contaminated surfaces (considering the frequency of related results, not the number of contaminated surfaces). Other high contamination rates were related to electronic equipment (mobile phones, personal computers, tablets and other personal items) (Jerry, O’Regan, O’Sullivan, Lynch, & Brady, Citation2020; Noorimotlagh, Jaafarzadeh, Martínez, & Mirzaee, Citation2021; Peyrony et al., Citation2020; Santarpia et al., Citation2020; Vicente et al., Citation2021), medical equipment surfaces (such as ventilators, monitors, and X-ray devices) (6; 13%) (Gordon et al., Citation2021; Liu et al., Citation2020; Santarpia et al., Citation2020; Verderber, Gray, Suresh-Kumar, Kercz, & Parshuram, Citation2021; Wu et al., Citation2020), patient bed rails (5; 11%) (Chan et al., Citation2020; Jerry et al., Citation2020; Santarpia et al., Citation2020; Vicente et al., Citation2021; Wu et al., Citation2020) and floors (5; 11%) (Dargahi et al., Citation2021; Jerry et al., Citation2020; Passos et al., Citation2021; Peyrony et al., Citation2020; Redmond et al., Citation2021).
In addition, many studies verified contamination rates related to the toilet room, thus indicating their importance for contamination risk management (10; 25%) (Bedrosian et al., Citation2021; Chan et al., Citation2020; Choi et al., Citation2021; Dargahi et al., Citation2021; Ge et al., Citation2021; Gormley et al., Citation2017; Liu et al., Citation2020; Passos et al., Citation2021; Santarpia et al., Citation2020; Vicente et al., Citation2021).
The cleaning processes also seem to play an essential role in contamination management. For example, Vicente et al. (Citation2021) verified higher contaminated surfaces rates in primary care buildings than in hospital’s COVID wards, which may be related to less rigorous disinfection routines. Besides, Wu et al. (Citation2020) concluded that surfaces frequently touched both medical staff and patients, such as the buttons of water machines and elevators, were usually neglected during the disinfection processes.
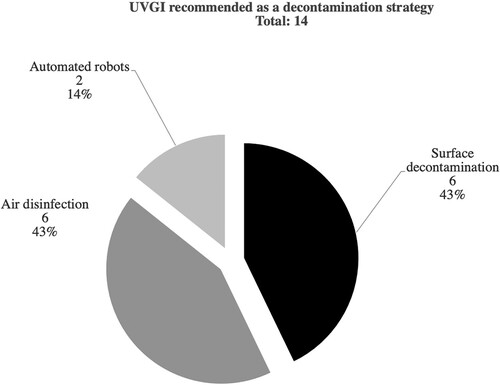
highlights the main recommendations that we verified concerning healthcare facilities design guidelines. The most frequent guidance for contaminations risk management were: the installation of UVGI systems (14; 33%), increasing air filtration efficiency (6; 14%), improving outdoor air rates (6; 14%), the spatial configuration to allow social distance between users (4; 10%), negative pressure and dedicated air conditioning systems in critical rooms (4; 10%), triage/circulation planning (2; 5%) and humidity control (2; 5%).
Figure 5. Design strategies to manage contamination risk, per frequency of occurrence. Source: the authors’ collection.
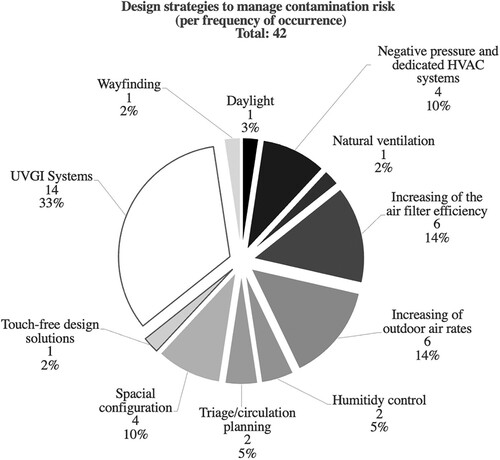
Among the recommendation regarding spatial configuration is separate contaminated, semi-contaminated and non-contaminated areas. In this context, it is essential to plan horizontal and vertical circulation to create separated dedicated circulation systems (Wang, Citation2021).
Avoiding crowding is an important measure to manage contamination. Zhou and Ji (Citation2021) conclude that the minimum distance between users in shared spaces shall be no less than 1,5 m. However, Noorimotlagh et al. (Citation2021) found a safety length of at least 2 m between the users. Both the recommendations surpass the physical distance of 1 m defined by the World Health Organization (WHO) <https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance>.
A relevant number of studies (14) concluded that ultraviolet germicidal inactivation (UVGI) systems should be an effective measure (). The selected studies were dedicated mainly to discuss ultraviolet lighting systems for air disinfection (6; 43%) (Bedrosian et al., Citation2021; Buonanno, Welch, Shuryak, & Brenner, Citation2020; Gordon et al., Citation2021; Hou, Pantelic, & Aviv, Citation2021; Morawska et al., Citation2020; Noorimotlagh et al., Citation2021), for surface disinfection (6; 43%) (Bedrosian et al., Citation2021; Chan et al., Citation2020; Heßling & Vatter, Citation2020; Messina et al., Citation2021; Ratnesar-Shumate et al., Citation2020; Sharafi, Ebrahimpour, & Nafez, Citation2021). In addition, 2 studies evaluated the use of automated robots for disinfection purposes (Diab-El Schahawi et al., Citation2021; Hu, Zhong, Li, Tan, & He, Citation2020).
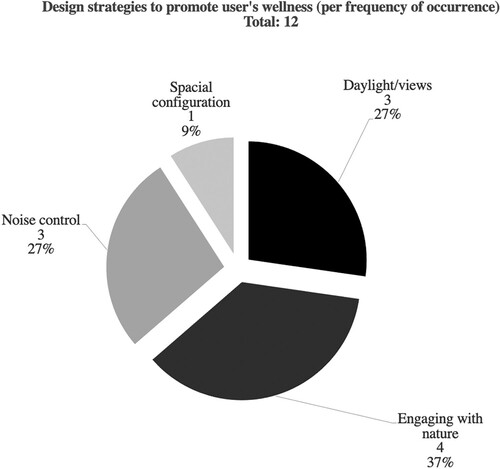
We also verified the importance of promoting wellness for patients and medical staff to reduce stress and anxiety. Considering that, the most frequent recommendations were engaging with nature (4; 37%) (Brambilla, Rebecchi, & Capolongo, Citation2019; Gola et al., Citation2020; Verderber et al., Citation2021; Wang, Citation2021), providing daylight and quality views to the outdoors (3; 27%) (Capolongo et al., Citation2020; Verderber et al., Citation2021; Wang, Citation2021), acoustic comfort (Capolongo et al., Citation2020; Gola et al., Citation2020; Verderber et al., Citation2021) and spacial configurations that promote privacy and family engagement (Verderber et al., Citation2021) ().
Case studies
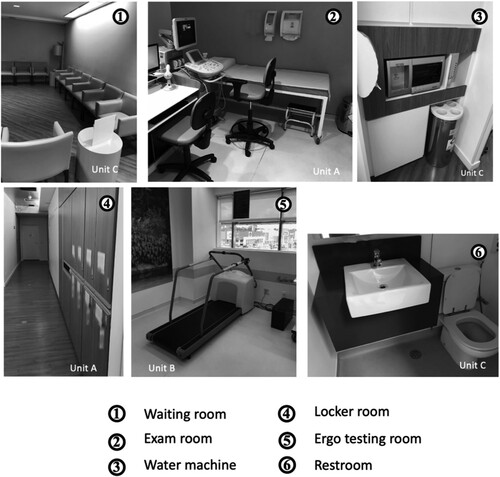
We defined for the diagnostic facilities selection the following criteria: the building must be a diagnostic should be designed, built and maintained as a diagnostic clinic, must be operated separated from any hospital operation, have a central air conditioning system and present an operational period longer than one year. Also, all of the units should provide complex medical imaging screening. In addition, the buildings share similar building programming and design guidelines that emphasise patient comfort to provide a ‘non-hospital atmosphere.’Footnote1 ().
Table 1. Operational characteristics of the selected case studies.
After analysing 144 (one hundred, forty-four) facilities in Brazil, we selected 5 (five) diagnostic clinics. The five buildings are located in Sao Paulo Expanded Metropolitan Area. We identified these healthcare units as Facilities A, B, C, D and EFootnote2 () for this study.
Table 2. Characteristics of building construction.
All of them provide imaging screening and clinical analysis testing services. Some examples of the available services are blood tests, urine tests, magnetic resonance, ergo stress testing and biopsies. In addition, the building programme defines independent testing areas according to the following approach: children’s health; women’s health; obstetrics; cardiology/neurovascular diseases; and check-up for tracking frequent diseases, such as tumours, metabolic, cardiovascular and infectious diseases. In all cases, the examinations occur in a sequence, and there is an integrated report to present the results of the tests.
Discussion
Designing for contamination risk management
Designing a healthcare facility requires multidisciplinary teams focused on developing a highly complex building programme. In this context, we should also take into account that project requirements can undergo rapid changes, such as those observed during 2020 due to the pandemic caused by the Sars-Cov-2 virus (Houghton et al., Citation2020), demanding improvements in the guidelines to mitigate risks of contaminating patients (Baker, Peckham, & Seixas, Citation2020).
According to the World Health Organization (WHO, Citation2020), coronavirus transmission is mainly through close contact with a contaminated person. However, people may come infected by aerosol transmission, especially if an infected person spends a long period with others in a crowded and poorly ventilated indoor space. Besides, contamination can happen when a person touches a contaminated surface or object, such as tables, doorknobs, or handrails, and then touches the nose, eyes or mouth.
A contamination prevention culture was a legacy of the global pandemic (Wu et al., Citation2020). Consequently, the most significant updates in design requirements have been an increase in natural ventilation and air change rates in waiting rooms and consulting rooms (Escombe, Ticona, Chávez-Pérez, Espinoza, & Moore, Citation2019). In this context, design strategies in planning circulation routes shall allow the efficient displacement of employees and supplies, avoid exposure to potential contaminating residues (Thomazoni, Citation2016), and minimise delays and waiting periods. In addition, patient triage must support separate circulation routes, thus creating clusters (Ierardi et al., Citation2020). Adopting strategies for disinfecting internal air and room surfaces is also fundamental to reduce contamination risks (see Subsection 2.1).
Among the available technologies for disinfection are ultraviolet germicidal irradiation (UVGI) lamps. The ultraviolet radiation is effective in deactivating not only the SARS-CoV-2 virus but also other respiratory pathogens, such as the Mycobacterium tuberculosis (Mphaphlele et al., Citation2015). Therefore, an alternative for interior spaces used by many people is to have a UVGI lighting system for permanent disinfection. For this purpose, the radiation wavelength of ∼286 nm could offer efficient virus deactivation (Gerchman, Mamane, Friedman, & Mandelboim, Citation2020).
Although ultraviolet radiation can be harmful to users, it is possible to provide UVGI directional lighting systems facing the ceiling above the user’s level (2.10 m). Another strategy is to install these features inside air conditioning recirculation devices (Buonanno et al., Citation2020; Kowalski, Citation2009; Miller, Citation2015; Mphaphlele et al., Citation2015). It is also possible to consider directional lighting systems facing the floor to disinfect surfaces in entrance areas. In such cases, the solution must include occupancy sensors to avoid exposing the user to UVC radiation (Heßling & Vatter, Citation2020; Kowalski, Citation2009; Mphaphlele et al., Citation2015; Sagripanti & Lytle, Citation2020).
Considering that the elderly represent a considerable portion of healthcare facility users and, at the same time, are more susceptible to developing severe conditions of infectious diseases (such as COVID-19), adopting measures of this nature is fundamental to mitigate the levels of risk to the health of the user.
Another issue worth mentioning is that many design requisites related to controlling other virus and bacteria transmission risks also apply to the Sars-CoV-2 risk management approach (Escombe et al., Citation2019; Fezi, Citation2020; Ramanathan et al., Citation2020). In addition, there is a recurrence of respiratory syndromes epidemic events since the Spanish influenza outbreak in 1918.
Among those events are the pandemic of influenza A, caused by the virus H1N1 (2009–2010), the pandemic caused by the betacoronavirus Sars-CoV (2002–2003) and the outbreak of the betacoronavirus MERS-CoV (2012) (Abdelrahman, Li, & Wang, Citation2020; WHO, Citation2017). Thus, the lessons learned during the Sars-CoV-2 pandemic shall promote the requirements update for designing healthcare facilities to mitigate the risks related to the virus transmission and prepare a healthcare built environment for future epidemic events.
Designing for healing
Building design solutions must meet a user’s needs and expectations (conscious and unconscious) (Codinhoto, Citation2017; Ono, Ornstein, et al., Citation2018). Thus, design solutions must meet requisites to promote positive impacts on the occupant’s health. The positive effects of a healthy built environment (HBE) are widely documented (Abdelaal & Soebarto, Citation2018; Prasad, Citation2017).
A Post-Occupancy Evaluation (POE) is an essential approach to understand the relations between a built environment and the occupants during the use phase (Mallory-Hill, Preiser, & Watson, Citation2012). This integrated approach shall include methods to access both technical data, for example, regarding the building systems performance and, on the other hand, carry on procedures to understand the effects of the built environment on the occupants’ behaviour and health. In addition, this integrated approach may include qualitative data gathered through observational evaluations, walkthroughs, focus groups discussions, interviews, and quantitative data obtained by applying surveys (Villa, Ono, França, & Ornstein, Citation2018).
The summarised results are essential to evaluate the effectiveness of the existing design solutions and support the review of future buildings’ design requirements that share the same typology, considering an evidence-based design framework (Brambilla, Lindahl, Dell’Ovo, & Capolongo, Citation2021; Villa et al., Citation2018).
As healthcare facilities shall provide support to patients on the recovery process, the assessment of healthcare facilities design requirements assume essential importance (Brambilla et al., Citation2021; Elf, Anåker, Marcheschi, Sigurjónsson, & Ulrich, Citation2020; Zhang, Tzortzopoulos, & Kagioglou, Citation2019).
Positive distraction, views to the natural environment, access to daylight, and adequate environmental comfort conditions may mitigate the sensation of pain and shorten the recovery phase by inducing individual experiences of positive feelings and developing relaxation. In this case, the built environment may perform a placebo effect by allowing the patient to stop paying attention to an injury and decreasing the transmission of pain impulses to the brain (Rehn & Schuster, Citation2017).
The proximity to the natural environment is essential due to the recent segregation between humans and nature, considering the evolutionary scale, as this process only intensified after the nineteenth century. As humans lived outside for a long time, they depend on environmental changes as triggers for their metabolism (such as light and temperature variations throughout days and seasons). For example, light exposure regulates melatonin and cortisol production, responsible for the sleep-wake cycle (Abdelaal & Soebarto, Citation2018).
As design requisites, HBEs incorporate several concepts of biophilia (Abdelaal & Soebarto, Citation2018; Mazuch, Citation2017) by providing nature environment stimuli in the built environment. Some of the design strategies may include sensorial richness, specification of natural finishes, offering contact with nature (gardens, plants, view windows, and water fountains) (Brambilla et al., Citation2019; Verderber et al., Citation2021; Wang, Citation2021). In addition, interpersonal distance (Redmond et al., Citation2021; Zhou & Ji, Citation2021).
Among the positive impacts of nature views through windows and access to gardens in healthcare facilities are blood pressure control, regulation of cortisol production, lower levels of pain, anxiety, and fatigue, and the reporting of greater satisfaction levels, both considering patients and health service providers (Bardenhagen, Rodiek, Nejati, & Lee, Citation2018; Momtaz, Citation2017; Reeve, Nieberler-Walker, & Desha, Citation2017).
Waiting areas are critical spaces because of the high circulation rates. The design solutions, in this case, may include layout arrangements and finishes that refers to residential environments, as well as warm colours and yellow lighting, to maintain a familiar and intimate scale. Among the design strategies are comfortable seats nearby windows, organised to allow social interaction and furniture arrangements that accommodate small groups, preferably close to a garden that may provide daylight and views (Capolongo et al., Citation2020; Jiang & Verderber, Citation2017).
Besides, there are design strategies for creating positive distraction opportunities aiming to produce beneficial effects on the patient’s emotional state, such as murals, framed art, decorative elements, image slideshows, digital or virtual reality devices, and trails through gardens (Andrade, Devlin, Pereira, & Lima, Citation2017).
On the other hand, inadequate design solutions may expose users to stressful experiences. For example, inadequate lighting levels or spatial configurations may increase the occurrence of medical errors and cause exposure to physical and biological contaminants, aspects related to risks to integrity for both patients and the medical team. By avoiding glare or reflections, adequate lighting levels are also a key factor to reduce risks related to medical errors by minimising physicians’ eye fatigue and ensuring accuracy during procedures (Zhang et al., Citation2019).
Thus, given the healthcare facility potential impact on the occupant’s health, design strategies must be user-centred (by meeting the needs of patients, companions, visitors, and healthcare service providers) to offer positive stimuli and mitigate occupants’ stress conditions (Carpman & Grant, Citation2016).
HBEs must also comply with the requirements to allow a patient to perform basic daily activities safely and with minimal assistance (DuBose, MacAllister, Hadi, & Sakallaris, Citation2018), including people with cognitive impairment, whether permanent or associated with any temporary health condition. Thus, wayfinding signage may include visible landmarks in a way that promotes location and orientation to allow a first time visitor to navigate the healthcare facility successfully, ensuring user’s autonomy (Brambilla et al., Citation2021).
Besides that, the design solutions must meet safety and promote universal design best practices and fall prevention. Patients subject to prolonged periods of fasting due to preparing for tests and undergoing exams that involve, for example, blood collection, sedation or physical efforts, are more susceptible to suffering from indisposition, dizziness or fainting. Furthermore, the elderly population represents an essential portion of diagnostic service users. At the same time, older patients are more likely to suffer from falls, whose risk of morbidity or sequelae increases proportionally to the age (WHO, Citation2018).
Results: current design guidelines and the necessity of updates
The research evaluated through the SLR indicates that a contaminated patient may easily contaminate both indoor air and surfaces around them. But differently than in COVID wards, which have rigorous protocols after a patient discharge and the infected patients are identified, primary care unities and diagnostic facilities have a higher circulation rate. Thus, in many cases, a contaminated patient may circulate throughout the facility without being identified.
As summarises (Subsection 2.1), there is an increased risk of a non-contaminated patient getting in touch with a surface in such cases. Thus, chairs, door handles, rails, elevators, and vending machines buttons may increase the risk for cross-contamination events.
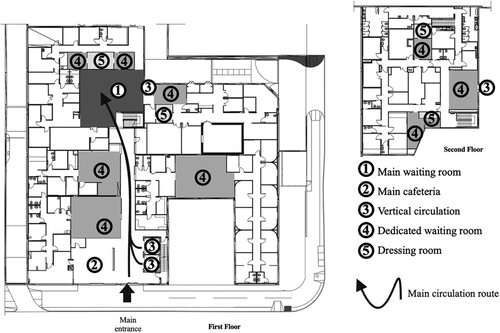
Moreover, these facilities usually have spaces that may have high circulation rates, such as waiting rooms, toilet rooms, elevators and cafeterias. presents examples of the room typology in the evaluated facilities.
The evaluated facilities comply with the following design requisites: positive distraction such as framed art, sculptures and murals (waiting areas, circulation, and cardiac stress testing rooms/imaging rooms), warm finishes, among them wooden furniture and wallpaper, warm electric light/ indirect light (waiting areas, circulation areas, and testing rooms) and acoustics and thermal comfort adequate levels.
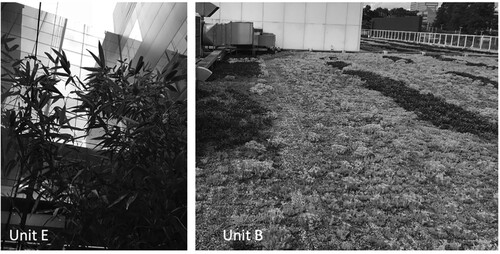
In addition, we verified views to the natural environment in cases A, B and E. Despite this, outdoor spaces were not accessible to users. Thus, we suggest a different approach for gardens. For example, front yards (Facilities B and E), courtyards (Facilities D and E), and green roofs (Facilities B and E) could be accessible to patients, aiming to provide natural ventilation, reducing contamination risk and encouraging relaxation (). Design strategies to reduce stress and anxiety are essential, especially during specialised diagnosis processes or chronic disease monitoring, requiring frequent visits and many tests each time.
In all case studies, air quality depended on ventilation and air conditioning mechanical systems. Moreover, the entrance, triage, cafeteria, and the main waiting area shared the same space, overlapping uses, and circulation flows (). These areas are critical spaces both for stress mitigation and contamination prevention due to the number of occupants in these spaces and the length of their permanence period.
Figure 10. Example of a map produced for circulation routes evaluation (Unit C). Source: the authors’ collection.
Regarding the study results, image screening rooms were considered critical due to temperature, humidity, and insulation specific requirements. Consequently, these air-conditioned spaces should not have windows for daylight or views. In these cases, design requirements must include positive distraction, warm lighting, and thermal comfort to reduce stress and anxiety. In addition, it is necessary to manage indoor air quality carefully. For example, rooms with high occupation rates may have UVGI disinfection systems above the user’s height, and inside the air handler devices should be considered for permanent use.
Entrances, horizontal and vertical circulation areas, locker/changing rooms, toilet rooms, stress testing rooms, an endoscopy area (Case A), cafeteria, waste rooms, custodial rooms, and air conditioning devices have a higher risk of contamination. Based on the presented SLR results, we determined the contamination risk for the spaces based on: length of stay, characteristics of the user’s flow nature, activity, airborne and surface contamination risk level, and user’s stress/anxiety risk level. shows the diagnostics and recommendations summary.
Table 3. Diagnostics and recommendations summary.
It would be possible to spend the waiting period in a multipurpose use with connection to outdoors and increased ventilation rates in the specific waiting area. The waiting room should preferably support nature proximity and offer many positive distraction features. The patient must have a snack with minimum dislocation, thus avoiding dislocations to a central cafeteria. They also shall have conditions to work online while waiting to be called. Design solutions shall minimise the use of elevators. If vertical transportation is necessary, it is essential to consider touch-free alternatives such as elevators that stop on a predetermined floor.
As proposed, the design solutions should support connectivity and not physical proximity to restrict the patient’s circulation to their specific testing areas.
Concluding remarks
Based on the study results, it is possible to identify design opportunities to reduce the levels of stress and anxiety of the users of diagnostic facilities, both patients and the medical team. Among them are the specification of natural finishes, warm lighting, and colours; positive stimuli and distractions; layout solutions that allow privacy and control of social interaction; and contact with nature through windows and access to gardens.
Natural ventilation strategies may be an essential strategy to increase outdoor air rates in indoor spaces. Among the solutions to promote air quality is the design of semi-open spaces with access to gardens.
Besides, digital communication is another strategy to reduce circulation overlaps. Triage planning must support the creation of clusters. If elevators are necessary, touch-free solutions may be an alternative. Finally, requirements should include UVGI lighting systems for surfaces and indoor air disinfection.
Limitations of the study
Limitations to this work include that the research identified during the LSR do not share normalised samples and testing methods. Besides, most studies consist of exploratory studies with limited sampling. Also, there is a lack of alignment in the data collected and the results from the surface contamination, stability, and disinfection protocols.
Thus, it would not be possible to carry on a quantitative analysis of the gathered evidence. Also, most of the verified experimental assessments demonstrated contamination within a hospitals’ indoor environment. Only a few discussed other healthcare facilities typologies.
Future developments
As an outspread of this study, future research shall adopt a quantitative approach when assessing indoor and outdoor spaces of diagnostic facilities. A quantitative analysis regarding air quality, for example, may contribute to complement the evidence that supports the decision-making process of coming facilities.
Contributions of the study
The present study highlights the importance of evidence-based design strategies related to contamination risk and well-being in non-hospital healthcare facilities. The results also suggest the importance of consolidating a biosecurity legacy to avoid future pandemic events; by planning adequate built environments that promote infection control.
The presented LSR results also show that there is a lack of research dedicated to this subject. It is a critical issue once primary care offers an essential part of a healthcare services system, thus impacting many people. Therefore, this paper presents a starting point for future research dedicated to consolidating performance requirements and recommendations for these facilities, which will support adequate and balanced design solutions.
Acknowledgement
We would like to thank the National Council for Scientific and Technological Development (CNPq) for the productivity grant number 304131/2020-2 awarded to the author Sheila Walbe Ornstein.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
Notes
1 Concentration of medical equipment and instruments.
2 The names and location of the healthcare facilities were omitted due to the confidentiality agreement signed between the researchers and the corporation.
References
- Abdelaal, M. S., & Soebarto, V. (2018). The death of modern hospital: Towards a restorative healthcare architecture. Proceedings of the 1st Annual Design Research Conference, Sydney 2018 (pp. 139–153).
- Abdelrahman, Z., Li, M., & Wang, X. (2020). Comparative review of SARS-CoV-2, SARS-CoV, MERS-CoV, and influenza a respiratory viruses. Frontiers in Immunology, 11, 1–14. doi:10.3389/fimmu.2020.552909
- AGÊNCIA NACIONAL DE VIGILÂNCIA SANITÁRIA (ANVISA). (2002). Resolução n° 50, de 21 de fevereiro de 2002. Dispõe sobre o regulamento técnico para planejamento, programação, elaboração e avaliação de projetos físicos de estabelecimentos assistenciais de saúde., Pub. L. No. RDC 50 (2002). Brasilia: Ministério da Saúde.
- Andrade, C. C., Devlin, A. S., Pereira, C. R., & Lima, M. L. (2017). Do the hospital rooms make a difference for patients’ stress? A multilevel analysis of the role of perceived control, positive distraction, and social support. Journal of Environmental Psychology, 53, 63–72.
- ASSOCIAÇÃO BRASILEIRA DE NORMAS TÉCNICAS (ABNT). (2013). NBR 15.575-1 edifícios habitacionais – desempenho. Parte 1: requisitos gerais. Rio de Janeiro, Brasil: ABNT.
- ASSOCIAÇÃO BRASILEIRA DE NORMAS TÉCNICAS (ABNT). (2020). NBR 9.050: 2020: acessibilidade a edificações, mobiliário, espaços e equipamentos urbanos. Rio de Janeiro: ABNT.
- Baker, M. G., Peckham, T. K., & Seixas, N. S. (2020). Estimating the burden of United States workers exposed to infection or disease: A key factor in containing risk of COVID-19 infection. PLoS ONE, 15(4), 4–11. doi:10.1371/journal.pone.0232452
- Bardenhagen, E., Rodiek, S., Nejati, A., & Lee, C. (2018). The seniors’ outdoor survey (SOS tool): A proposed weighting and scoring framework to assess outdoor environments in residential care settings. Journal of Housing for the Elderly, 32, 99–120.
- Bedrosian, N., Mitchell, E., Rohm, E., Rothe, M., Kelly, C., String, G., & Lantagne, D. (2021). A systematic review of surface contamination, stability, and disinfection data on SARS-CoV-2 (Through July 10, 2020). Environmental Science and Technology, 55, 4162–4173.
- Brambilla, A., Lindahl, G., Dell’Ovo, M., & Capolongo, S. (2021). Validation of a multiple criteria tool for healthcare facilities quality evaluation. Facilities, 39, 434–447.
- Brambilla, A., Rebecchi, A., & Capolongo, S. (2019). Evidence based hospital design. A literature review of the recent publications about the EBD impact of built environment on hospital occupants’ and organizational outcomes. Annali di Igiene, 31, 165–180.
- Buonanno, M., Welch, D., Shuryak, I., & Brenner, D. J. (2020). Far-UVC light (222 nm) efficiently and safely inactivates airborne human coronaviruses. Scientific Reports, 10, 1–8.
- Capolongo, S., Gola, M., Brambilla, A., Morganti, A., Mosca, E. I., & Barach, P. (2020). COVID-19 and healthcare facilities: A decalogue of design strategies for resilient hospitals. Acta Biomedica, 91, 50–60.
- Carpman, J. R., & Grant, M. A. (2016). Design that cares: Planning health facilities for patients and visitors (3rd ed.). San Francisco: Jossey Bass.
- Chan, V. W. M., So, S. Y. C., Chen, J. H. K., Yip, C. C. Y., Chan, K. H., Chu, H., … Chung, T. W. H. (2020). Air and environmental sampling for SARS-CoV-2 around hospitalized patients with coronavirus disease 2019 (COVID-19). Infection Control & Hospital Epidemiology, 41, 1258–1265. doi:10.1017/ice.2020.282
- Choi, H., Chatterjee, P., Coppin, J. D., Martel, J. A., Hwang, M., Jinadatha, C., & Sharma, V. K. (2021). Current understanding of the surface contamination and contact transmission of SARS-CoV-2 in healthcare settings. Environmental Chemistry Letters, 19, 1935–1944.
- Codinhoto, R. (2017). Healing architecture. In E. Tsekleves, & R. Cooper (Eds.), Design for Health (pp. 111–153). Oxon: Routledge/Taylor & Francis Group.
- Dargahi, A., Jeddi, F., Vosoughi, M., Karami, C., Hadisi, A., Ahamad Mokhtari, S., … Sadeghi, H. (2021). Investigation of SARS CoV-2 virus in environmental surface. Environmental Research, 195, 110765.
- Diab-El Schahawi, M., Zingg, W., Vos, M., Humphreys, H., Lopez-Cerero, L., Fueszl, A., … Elisabeth Presterl for the ESCMID Study Group on Nosocomial Infections “The decontamination research working group”. (2021). Ultraviolet disinfection robots to improve hospital cleaning: Real promise or just a gimmick? Antimicrobial Resistance and Infection Control, 10, 10–12.
- DuBose, J., MacAllister, L., Hadi, K., & Sakallaris, B. (2018). Exploring the concept of healing spaces. HERD: Health Environments Research & Design Journal, 11, 43–56.
- Elf, M., Anåker, A., Marcheschi, E., Sigurjónsson, Á., & Ulrich, R. S. (2020). The built environment and its impact on health outcomes and experiences of patients, significant others and staff—A protocol for a systematic review. Nursing Open, 7, 895–899.
- Escombe, A. R., Ticona, E., Chávez-Pérez, V., Espinoza, M., & Moore, D. A. J. (2019). Improving natural ventilation in hospital waiting and consulting rooms to reduce nosocomial tuberculosis transmission risk in a low resource setting. BMC Infectious Diseases, 19, 88.
- Fezi, B. A. (2020). Health engaged architecture in the context of COVID-19. Journal of Green Building, 15, 185–212.
- França, A. J. G. L. (2019). Impactos da modelagem da informação para o processo de gestão de um portfólio de estabelecimentos assistenciais de saúde (EASs). Relatório de pesquisa (pós-doutorado) (p. 182). São Paulo: Faculdade de Arquitetura e Urbanismo da Universidade de São Paulo – FAUUSP.
- Ge, T., Lu, Y., Zheng, S., Zhuo, L., Yu, L., Ni, Z., … Zhong, Z. (2021). Evaluation of disinfection procedures in a designated hospital for COVID-19. American Journal of Infection Control, 49, 447–451.
- Gerchman, Y., Mamane, H., Friedman, N., & Mandelboim, M. (2020). UV-LED disinfection of coronavirus: Wavelength effect. Journal of Photochemistry and Photobiology B: Biology, 212, 112044.
- Gola, M., Caggiano, G., De Giglio, O., Napoli, C., Diella, G., Carlucci, M., … Montagna, M. T. (2020). SARS-CoV-2 indoor contamination: Considerations on anti-COVID-19 management of ventilation systems, and finishing materials in healthcare facilities. Annali Di Igiene : Medicina Preventiva e Di Comunità, 33, 381–392.
- Gordon, D., Ward, J., Yao, C. J., & Lee, J. (2021). Built environment airborne infection control strategies in pandemic alternative care sites. HERD: Health Environments Research & Design Journal, 14, 38–48.
- Gormley, M., Aspray, T. J., Kelly, D. A., & Rodriguez-Gil, C. (2017). Pathogen cross-transmission via building sanitary plumbing systems in a full scale pilot test-rig. PLoS ONE, 12, 1–13.
- Heßling, M., & Vatter, P. (2020). Ultraviolet irradiation doses for coronavirus inactivation – review and analysis of coronavirus photoinactivation studies Ultraviolette Bestrahlungsdosen für die Inaktivierung von Coronaviren. GMS Hygiene and Infection Control, 15, 1–8.
- Hou, M., Pantelic, J., & Aviv, D. (2021). Spatial analysis of the impact of UVGI technology in occupied rooms using ray-tracing simulation. Indoor Air, March, 1–14. doi:10.1111/ina.12827
- Houghton, C., Meskell, P., Delaney, H., Smalle, M., Glenton, C., Booth, A., … Biesty, L. M. (2020). Barriers and facilitators to healthcare workers’ adherence with infection prevention and control (IPC) guidelines for respiratory infectious diseases: A rapid qualitative evidence synthesis. Cochrane Database of Systematic Reviews, 1(4), 1–69. doi:10.1002/14651858.CD013582
- Hu, D., Zhong, H., Li, S., Tan, J., & He, Q. (2020). Segmenting areas of potential contamination for adaptive robotic disinfection in built environments. Building and Environment, 184, 1–14. doi:10.1016/j.buildenv.2020.107226
- Ierardi, A. M., Wood, B. J., Arrichiello, A., Bottino, N., Bracchi, L., Forzenigo, L., … Carrafiello, G. (2020). Preparation of a radiology department in an Italian hospital dedicated to COVID-19 patients. La Radiologia Medica, 125, 894–901.
- Jerry, J., O’Regan, E., O’Sullivan, L., Lynch, M., & Brady, D. (2020). Do established infection prevention and control measures prevent spread of SARS-CoV-2 to the hospital environment beyond the patient room? Journal of Hospital Infection, 105, 589–592.
- Jiang, S., & Verderber, S. (2017). On the planning and design of hospital circulation zones: A review of the evidence-based literature. HERD: Health Environments Research & Design Journal, 10, 124–146.
- Kowalski, W. (2009). Ultraviolet germicidal irradiation handbook. Berlin, Heidelberg: Springer Berlin Heidelberg.
- Liu, Y., Ning, Z., Chen, Y., Guo, M., Liu, Y., Gali, N. K., … Lan, K. (2020). Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature, 582, 557–560.
- Mallory-Hill, S., Preiser, W. F. E., & Watson, C. G. (Eds.). (2012). Enhancing building performance. Oxford, UK: Wiley-Blackwell.
- Marquardt, G., Bueter, K., & Motzek, T. (2014). Impact of the design of the built environment on people with dementia: An evidence-based review. Health Environments Research & Design Journal, 8, 127–157.
- Mazuch, R. (2017). Salutogenic and biophilic design as therapeutic approaches to sustainable architecture. Architectural Design, 87, 42–47.
- Messina, G., Della Camera, A., Ferraro, P., Amodeo, D., Corazza, A., Nante, N., … Cevenini, G. (2021). An emerging innovative UV disinfection technology (Part II): Virucide activity on SARS-CoV-2. International Journal of Environmental Research and Public Health, 18, 1–10. doi:10.3390/ijerph18083873
- Miller, S. L. (2015). Upper room germicidal ultraviolet systems for air disinfection are ready for wide implementation. American Journal of Respiratory and Critical Care Medicine, 192, 407–409.
- Momtaz, R. I. (2017). Healing gardens-a review of design guidelines. International Journal of Current Engineering and Technology, 77, 2277–4106.
- Morawska, L., Tang, J. W., Bahnfleth, W., Bluyssen, P. M., Boerstra, A., Buonanno, G., … Yao, M. (2020). How can airborne transmission of COVID-19 indoors be minimised? Environment International, 142, 105832.
- Mphaphlele, M., Dharmadhikari, A. S., Jensen, P. A., Rudnick, S. N., van Reenen, T. H., Pagano, M. A., … Nardell, E. A. (2015). Institutional tuberculosis transmission. Controlled trial of upper room ultraviolet air disinfection: A basis for new dosing guidelines. American Journal of Respiratory and Critical Care Medicine, 192, 477–484.
- Noorimotlagh, Z., Jaafarzadeh, N., Martínez, S. S., & Mirzaee, S. A. (2021). A systematic review of possible airborne transmission of the COVID-19 virus (SARS-CoV-2) in the indoor air environment. Environmental Research, 193, 110612.
- Ono, R., França, A. J. G. L., & Ornstein, S. W. (2018). Formas de apresentação dos resultados. In R. Ono, S. W. Ornstein, S. B. Villa, & A. J. G. L. França (Eds.), Avaliação pós-ocupação: Na arquitetura, no urbanismo e no design – da teoria à prática (pp. 135–148). São Paulo: Oficina de Textos.
- Ono, R., Ornstein, S. W., Villa, S. B., & França, A. J. G. L. (2018). Avaliação pós-ocupação: na arquitetura, no urbanismo e no design – da teoria à prática. São Paulo: Oficina de Textos.
- Organização Pan-Americana de Saúde/Organização Mundial de Saúde (OPAS/OMS). (2017). Doenças cardiovasculares. Organização Pan-Americana de Saúde & Organização Mundial de Saúde. Brasilia, DF: OPAS.
- Passos, R. G., Silveira, M. B., & Abrahão, J. S. (2021). Exploratory assessment of the occurrence of SARS-CoV-2 in aerosols in hospital facilities and public spaces of a metropolitan center in Brazil. Environmental Research, 195, 1–9. doi:10.1016/j.envres.2021.110808
- Pati, D., & Lorusso, L. N. (2018). How to write a systematic review of the literature. HERD: Health Environments Research & Design Journal, 11, 15–30.
- Peyrony, O., Ellouze, S., Fontaine, J.-P., Thegat-Le Cam, M., Salmona, M., Feghoul, L., … Tremorin, M. T. (2020). Surfaces and equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the emergency department at a university hospital. International Journal of Hygiene and Environmental Health, 230, 1–6. doi:10.1016/j.ijheh.2020.113600
- Prasad, S. (2017). Regenerative agents: Patient-focused architectures. Architectural Design, 87, 122–127.
- Ramanathan, K., Antognini, D., Combes, A., Paden, M., Zakhary, B., Ogino, M., … Shekar, K. (2020). Planning and provision of ECMO services for severe ARDS during the COVID-19 pandemic and other outbreaks of emerging infectious diseases. The Lancet Respiratory Medicine, 8(5), 518–526. doi:10.1016/S2213-2600(20)30121-1
- Ratnesar-Shumate, S., Williams, G., Green, B., Krause, M., Holland, B., Wood, S., … Dabisch, P. (2020). Simulated sunlight rapidly inactivates SARS-CoV-2 on surfaces. The Journal of Infectious Diseases, 222, 214–222.
- Redmond, S. N., Dousa, K. M., Jones, L. D., Li, D. F., Cadnum, J. L., Navas, M. E., … Donskey, C. J. (2021). Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) nucleic acid contamination of surfaces on a coronavirus disease 2019 (COVID-19) ward and intensive care unit. Infection Control & Hospital Epidemiology, 42, 215–217.
- Reeve, A., Nieberler-Walker, K., & Desha, C. (2017). Healing gardens in children’s hospitals: Reflections on benefits, preferences and design from visitors’ books. Urban Forestry & Urban Greening, 26, 48–56.
- Rehn, J., & Schuster, K. (2017). Clinic design as placebo—using design to promote healing and support treatments. Behavioural Science, 7(4), 77. https://doi.org/10.3390/bs7040077
- Sagripanti, J. L., & Lytle, C. D. (2020). Estimated inactivation of coronaviruses by solar radiation with special reference to COVID-19. Photochemistry and Photobiology, 96, 731–737.
- Santarpia, J. L., Rivera, D. N., Herrera, V. L., Morwitzer, M. J., Creager, H. M., Santarpia, G. W., … Lowe, J. J. (2020). Aerosol and surface contamination of SARS-CoV-2 observed in quarantine and isolation care. Scientific Reports, 10(1), 1–8. doi:10.1038/s41598-020-69286-3
- Sharafi, S. M., Ebrahimpour, K., & Nafez, A. (2021). Environmental disinfection against COVID-19 in different areas of health care facilities: A review. Reviews on Environmental Health, 36, 193–198.
- SUPLEMENTAR, ANS-AGÊNCIANACIONALDESAÚDE. (2019). Mapa assistencial da saúde suplementar 2018. Rio de Janeiro: ANS.
- Thomazoni, A. D. L. (2016). A definição do partido arquitetônico pautado nos estudos dos fluxos frente à modernização de hospitais complexos. Sao Paulo: Universidade de São Paulo.
- van Hoof, J., Rutten, P. G. S., Struck, C., Huisman, E. R. C. M., & Kort, H. S. M. (2015). The integrated and evidence-based design of healthcare environments. Architectural Engineering and Design Management, 11, 243–263.
- Verderber, S., Gray, S., Suresh-Kumar, S., Kercz, D., & Parshuram, C. (2021). Intensive care unit built environments: A comprehensive literature review (2005-2020). Herd, 18(May). doi:10.1177/19375867211009273
- Vicente, V. A., Lustosa, B. P. R., Grisolia, M. E., Pavini Beato, C., Balsanelli, E., Fruet, V. de S. G., … Souza, E. M. (2021). Environmental detection of SARS-CoV-2 virus RNA in health facilities in Brazil and a systematic review on contamination sources. International Journal of Environmental Research and Public Health, 18(3824), 2–12. doi:10.3390/ijerph18073824
- Villa, S. B., Ono, R., França, A. J. G. L., & Ornstein, S. W. (2018). Procedimentos metodológicos. In R. Ono, S. W. Ornstein, S. B. Villa, & A. J. G. L. França (Eds.), Avaliação pós-ocupação: na arquitetura, no urbanismo e no design – da teoria à prática (pp. 81–94). São Paulo: Oficina de Textos.
- Villanueva, K., Pereira, G., Knuiman, M., Bull, F., Wood, L., Christian, H., … Giles-Corti, B. (2013). The impact of the built environment on health across the life course: Design of a cross-sectional data linkage study. BMJ Open, 3, 1–11. doi:10.1136/bmjopen-2012-002482
- Wang, Z. (2021). Use the environment to prevent and control COVID-19 in senior-living facilities: An analysis of the guidelines used in China. HERD: Health Environments Research & Design Journal, 14, 130–140.
- Wang, Y., Qiao, F., Zhou, F., & Yuan, Y. (2020). Surface distribution of severe acute respiratory syndrome coronavirus 2 in Leishenshan Hospital in China. Indoor and Built Environment, 0, 1–9. doi:10.1177/1420326X20942938
- Weng, C. L., & Kau, L. J. (2021). Planning and design of a full-outer-air-intake natural air-conditioning system for medical negative pressure isolation wards. Journal of Healthcare Engineering, 2021, 1–13. doi:10.1155/2021/8872167
- WORLD HEALTH ORGANIZATION (WHO). (2008). The world health report 2008: Primary health care – now more than ever. Geneva: WHO.
- WORLD HEALTH ORGANIZATION (WHO). (2012). Modern health care delivery systems, care coordination and the role of hospitals (pp. 1–36). Geneva: WHO.
- WORLD HEALTH ORGANIZATION (WHO). (2017). Pandemic influenza risk management: A WHO guide to inform and harmonize national and international pandemic preparedness and response. World Health Organization. Retrieved from https://apps.who.int/iris/handle/10665/259893
- WORLD HEALTH ORGANIZATION (WHO) (2018). Falls: Key facts. Geneva: WHO.
- WORLD HEALTH ORGANIZATION (WHO) (2020). Infection prevention and control during health care when novel coronavirus (nCoV) infection is suspected. Geneva: WHO.
- Wu, S., Wang, Y., Jin, X., Tian, J., Liu, J., & Mao, Y. (2020). Environmental contamination by SARS-CoV-2 in a designated hospital for coronavirus disease 2019. American Journal of Infection Control, 48, 910–914.
- Yin, R. K. (2018). Case study research and applications: Design and methods (6th ed.). Thousand Oaks, CA: Sage Publications.
- Zhang, Y., Tzortzopoulos, P., & Kagioglou, M. (2019). Healing built-environment effects on health outcomes: Environment–occupant–health framework. Building Research & Information, 47, 747–766.
- Zhou, Y., & Ji, S. (2021). Experimental and numerical study on the transport of droplet aerosols generated by occupants in a fever clinic. Building and Environment, 187, 1–14. doi:10.1016/j.buildenv.2020.107402