Abstract
Background Diagnostic ultrasound examination of the shoulder is generally considered to require long experience. We examined the results of an orthopedic surgeon with little experience of ultrasound.
Patients and methods A relatively inexperienced examiner performed preoperative ultrasound scanning of 79 patients with symptoms from the rotator cuff and/or the long head of the biceps muscle. Tears of the rotator cuff and rupture or dislocation of the long head of the biceps muscle were the positive findings of interest. Results were compared to operative findings.
Results In 66 of 79 shoulders, ultrasonographic rotator cuff findings were confirmed at surgery (accuracy 84%). 20 of 26 full-thickness tears were diagnosed correctly. 6 of 7 partial-thickness tears were overlooked. Ultrasound was false positive in 1 case. For the long head of the biceps muscle, all 8 cases of dislocation or rupture of the tendon were diagnosed but differentiation between the two conditions was not possible in 2 cases.
Interpretation Our results may encourage orthopedic surgeons to start using ultrasound as a diagnostic technique for full-thickness tears of the rotator cuff and for pathology in the long head of the biceps muscle.
Ultrasound as a noninvasive diagnostic modality of the soft parts of the shoulder was introduced in the early 1980s. Since then, several studies of experienced radiologists have shown high sensitivity and specificity for demonstration of tears of the rotator cuff, and of rupture and dislocation of the long head of the biceps muscle (Farin et al. Citation1996, Teefey et al. Citation2000, Citation2004, Martin-Hervás et al. Citation2001). Most of these reports emphasize the long learning curve associated with the method. In a search of the literature, however, we found only one study based on early experience (Roberts et al. Citation1998).
Most orthopedic surgeons have little or no experience of diagnostic ultrasound. On the other hand, orthopedic surgeons have the advantage of precise knowledge of the shoulder anatomy—gained through surgical experience—and of clinical understanding of shoulder problems. It is possible that these advantages, coupled with recent improvements in ultrasound equipment, may reduce the need for long ultrasound experience.
In this study, we focused on the early learning curve of an orthopedic surgeon regarding diagnostic ultrasound of the shoulder. We wanted to examine the usefulness of ultrasonography in daily clinical practice as an integral part of several diagnostic techniques, rather than as an isolated diagnostic modality.
Patients and methods
After a 2-day educational course consisting of 8 lessons in ultrasound theory and two afternoons of practical exercises, one of the authors (SM) examined 350 consecutive shoulder patients both clinically and by ultrasound. Patients were referred from general practitioners for chronic shoulder pain. The median age was 54 (21–79) years. In 79 cases, indications for operative treatment were found. Indication was based on the medical history, the clinical findings and, if relevant, on conventional radiographs or MRI. The result from ultrasound was not used as a diagnostic criterion, which means that no patient was excluded from operation because of a negative ultrasound finding. In the referral papers, results from previous radiographs and MRI examinations (all but one as plain MRI) were available in 53 and 39 cases, respectively. The ultrasound examiner was not blinded regarding this information.
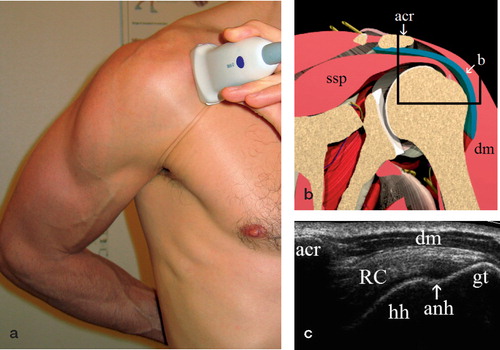
Real-time ultrasound scanning was performed with a Siemens Sonoline Sienna scanner (Siemens Medical Systems, Erlangen, Germany). A 7.5L70 linear array transducer (5.5–9.4 MHz) was used. Patients were seated on a swivel stool with the examiner standing behind. 5 standard views (anterior transversal and longitudinal, lateral transversal and longitudinal, posterior transversal) were acquired and supplemented with dynamic examination. For the lateral views the arm was placed in adduction and internal rotation, which gave a better exposure of the supraspinatus tendon from under the acromion (). For the other views, the arm was placed in adduction and neutral rotation. Bilateral examination was performed if required. The subscapularis, supraspinatus, infraspinatus and biceps tendons were examined in the transverse and longitudinal planes. Diagnostic criteria for pathology of the rotator cuff and the long head of the biceps muscle were used as described in the literature (Middleton et al. Citation1998, Bouffard et al. Citation2000).
Figure 1. Ultrasound examination, lateral longitudinal view, (a) position of the patient and of the transducer, (b) anatomy, (c) ultrasonographic view corresponding to the area within the black rectangle.(Figure 1b reproduced with permission from primal pictures;www.primalpictures.com) Abbreviations:ssp, supraspinatus muscle;acr, acromion;b, bursa;dm, deltoid muscle;RC, rotator cuff;hh, humeral head;anh, anatomical humeral neck;gt, greater tuberosity.
Operation was performed arthroscopically in 66 cases, with examination of the articular and bursal side of the rotator cuff and the intraarticular portion of the long head of the biceps muscle. 13 patients were operated by open technique, with inspection of the intraarticular conditions through the tear in the rotator cuff. In one case with an intact rotator cuff, inspection was done through a longitudinal incision. Operations were performed by experienced surgeons from our orthopedics department who had knowledge of the imaging reports before surgery. The ultrasound examiner did not participate in surgery of the study patients. Final diagnoses after operation are given in .
Table 1. Final diagnosis after surgery (more than one diagnosis possible per patient)
Statistics
Results for sensitivity, specificity, positive and negative predictive values are given twice, once by considering full-thickness tears as the positive finding, and once by considering both full and partial-thickness tears as the positive finding. The 95% confidence intervals (CI) were derived from the binominal distribution (www.swogstat.org/stat/ public/binominal_conf.htm).
Results
Rotator cuff
We found that the results of ultrasound examination and operation corresponded in 66 of 79 cases, which gives an accuracy of 84% (95% CI 76–92) (). Ultrasound allowed correct identification of 20 of 26 full-thickness tears, but only 1 of 7 partial-thickness tears. Ultrasonography demonstrated no tear in 45 of 46 cases that had no evidence of a tear at operation. Among the 13 cases with conflicting results, there were 1 false positive and 11 false negative ultrasound findings. In 1 case of a full-thickness tear, a partial tear was found at ultrasound. In , values for sensitivity, specificity, and positive and negative predictive values together with 95% CI are given twice—once considering full-thickness tears as the positive finding, and once considering both full- and partial-thickness tears as the positive finding.
Table 2. Rotator cuff findings at ultrasound and surgery
Table 3. Results of ultrasound diagnosis (95% CI)
For the 39 patients with a known result from MRI, we analyzed the diagnostic contribution of additional ultrasound. In 10 cases, the results from ultrasound and MRI differed. In 6 of the cases, operation confirmed the ultrasound findings; in 3 cases, operation confirmed the MRI findings. In 1 case, both methods failed ().
Table 4. Ultrasound, MRI and surgical findings in 10 patients where there was disagreement between ultrasonography and MRI
In 3 of the 29 cases with corresponding results from ultrasound and MRI, the findings were not confirmed at surgery. 2 cases of partial-thickness tear and 1 case of full-thickness tear at surgery had normal findings at ultrasound and MRI. Sensitivity and specificity in this subgroup of patients were higher than in the total material (92% and 100%, when considering partial-thickness tears as a negative finding).
Biceps tendon
Ultrasound allowed correct identification of all 4 total ruptures, of 1 partial rupture, and 1 of 3 dislocations of the long head of the biceps muscle. In the 2 remaining cases with surgically verified dislocation, ultrasound found tendon pathology—but could not distinguish between dislocation and rupture. There were no false positive and 67 true negative ultrasonograms (in 4 cases of open surgery, the long head of the biceps muscle was not examined by the surgeon).
Among the 39 patients with known results from MRI, operation disclosed 1 partial and 2 complete ruptures of the long head of the biceps muscle. All 3 were correctly diagnosed by ultrasound, but overlooked by MRI.
Discussion
Due to its good results in several studies and its methodological advantages (), diagnostic ultrasound has been proposed as a primary imaging technique for the soft parts of the shoulder (Matsen et al. Citation1998). Even so, the method has only gained partial acceptance as a diagnostic instrument in orthopedics. This reluctance in applying the method has been justified by its requirement for examiner experience and its long learning curve. This view has been supported by the personal experiences of some authors (Sonnabend et al. Citation1997, Middelton et al. Citation1998, Swen et al. Citation1999, Backhaus et al. Citation2001), but has been documented only to a limited extent in literature. Our results, derived from a novice, indicate that the method is more accessible than expected. There are several possible explanations for the early success of the orthopedic surgeon. Adding diagnostic ultrasound as a routine for shoulder patients at the outpatient clinic would result in higher examination frequency. Temporal closeness of clinical shoulder examination and ultrasound scanning, together with a good clinical understanding of the actual shoulder problem enables the orthopedic surgeon to focus his/her ultrasound examination on the clinical findings. He/she will learn by being confronted with his/her own results during a later operation. Recent progress in ultrasound equipment may also contribute to faster access to the modality (Strobel et al. Citation2004).
Table 5. Methodological advantages of diagnostic ultrasound
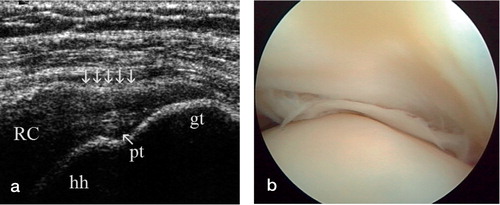
Analysis of our results shows that the positive ultrasound findings were highly reliable. Among 21 positive findings for full-thickness tears of the rotator cuff (), there was only one false positive (in a patient with advanced rheumatic disease). On the other hand, there were 12 false negative results in our study of 79 shoulders. For full-thickness tears, missing 6 of 26 cases is not too far removed from what can be achieved by more experienced examiners (Farin et al. Citation1996, Sonnabend et al. Citation1997, Teefey et al. Citation2004, Ziegler Citation2004) and it confirms the method's competitiveness with other imaging techniques of the soft parts of the shoulder (Farin et al. Citation1966, Swen et al. Citation1999, Teefey et al. Citation2004). For partial-thickness tears (), how-ever, ultrasound did not work well as a diagnostic method in our hands. We overlooked 6 of 7 partial-thickness tears. Results for partial-thickness tears have been inferior to those for full-thickness tears in other studies also, but not as much as in ours (Read and Perko Citation1998, Teefey et al. Citation2000, Citation2004, Martin-Hervás et al. Citation2001). shows our results for full- and partial-thickness tears versus no tears, and for full tears versus partial and no tears in comparison to those from more experienced investigators. As all partial-thickness tears in our material were treated with just debridement and decompression, it seems justifiable from an orthopedic standpoint to regard the result from total versus partial and no tear as the most relevant.
Table 6. Ultrasonographic results for tears in the rotator cuff with surgical inspection as the reference
Figure 2. Full-thickness tear of the rotator cuff, (a) lateral transversal view by ultrasound (same position as in , transducer turned horizontally), (b) arthroscopic, (c) open view.RC-t, rotator cuff tear (for other abbreviations, see ).

Figure 3. Partial-thickness tear of the rotator cuff, (a) lateral longitudinal view by ultrasound and (b) arthroscopic view.pt, partial tear;5 arrows, contour concavity (for other abbreviations, see ).
Our study may be criticized for not having blinded the ultrasound examiner as to results from other diagnostic procedures, especially from MRI. Of our 79 study patients, 39 had undergone MRI prior to ultrasound examination. Comparison of the results from ultrasound for the two groups, however, shows that the group without MRI () had similar results (sensitivity 82%, specificity 100% for full-thickness vs. partial or no tear) to the group with MRI (sensitivity 73%, specificity 96%). Our study cannot provide a result for diagnostic ultrasound as an isolated technique, but it reflects the usefulness of the method as an integrated part of the diagnostic modalities for rotator cuff and biceps tendon problems. Different results from ultrasound and MRI should lead to further examination, e.g. by MR arthrography. The same result from both techniques will increase the probability of a correct diagnosis.
Table 7. Rotator cuff findings at ultrasound and surgery for the group of patients without MRI
- Backhaus M, Burmester G R, Gerber T, Grassi W, Machold K P, Swen W A, Wakefield R J, Manger B. Guidelines for musculoskeletal ultrasound in rheumatology. Ann Rheum Dis 2001; 60: 641–9
- Bouffard J A, Lee S-M, Dhanju J. Ultrasonography of the shoulder. Semin Ultrasound 2000
- Farin P U, Kaukanen E, Jaroma H, Väätäinen U, Miettinen H, Soimakallio S. Findings at ultrasound, double-contrast arthrography, and computed tomography arthrography with surgical correlation. Invest Radiol 1996; 31(7)387–94
- Martin-Hervás C, Romero J, Navas-Acién A, Reboiras J J, Munuera L. Ultrasonographic and magnetic resonance images of rotator cuff lesions compared with arthroscopy or open surgery findings. J Shoulder Elbow Surg 2001; 10(5)410–5
- Matsen F A, Arntz C T, Lippitt S B. Rotator cuff - Imaging techniques. The Shoulder, C A Rockwood, F A Matsen. W B Saunders Co, Philadelphia 1998; 2: 787–93
- Middleton W D, Teefey S A, Yamaguchi K. Sonography of the shoulder. Semin Musculoskelet Radiol 1998; 2(3)211–21
- Read J W, Perko M. Shoulder ultrasound: Diagnostic accuracy for impingement syndrome, rotator cuff tear, and biceps tendon pathology. J Shoulder Elbow Surg 1998; 7(3)264–71
- Roberts C S, Galloway K P, Honaker J T, Hulse G, Seligson D. Sonography for the office screening of suspected rotator cuff tears: early experience of the orthopedic surgeon. Am J Orthop 1998; 7: 503–6
- Sonnabend D H, Hughes J S, Giuffre B M, Farrell R. The clinical role of shoulder ultrasound. Aust NZ J Surg 1997; 67: 630–3
- Strobel K, Zanetti M, Nagy L, Hodler J. Suspected rotator cuff lesions: Tissue harmonic imaging versus conventional US of the shoulder. Radiology 2004; 230(1)243–9
- Swen W A A, Jacobs J W G, Algra P R, Manoliu R A, Rijkmans J, Willems W J, Bijlsma J W J. Sonography and magnetic resonance imaging equivalent for the assessment of full-thickness rotator cuff tears. Arthritis Rheum 1999; 42(10)2231–8
- Teefey S A, Hasan S A, Middleton W D, Patel M, Wright R W, Yamaguchi K. Ultrasonography of the rotator cuff. J Bone Joint Surg (Am) 2000; 82(4)498–504
- Teefey S A, Rubin D A, Middleton W D, Hildebolt C F, Leibold R A, Yamaguchi K. Detection and quantification of rotator cuff tears. J Bone Joint Surg (Am) 2004; 86(4)708–11
- Ziegler D W. The use of in-office, orthopaedist-performed ultrasound of the shoulder to evaluate and manage rotator cuff disorders. J Shoulder Elbow Surg 2004; 13(3)291–7