Abstract
Background Periprosthetic fractures of the greater trochanter through osteolytic cysts are rare. The proper treatment and its influence on the prosthetic survival remains unknown.
Patients and methods We retrospectively evaluated 887 hips with uncemented MicroStructured Omnifit total hip prostheses at a mean follow-up time of 11 (5–14) years. We found 23 (2.6%) fractures of the greater trochanter through a cystic lesion, occurring 4–11 years postoperatively.
Results Nonoperative treatment healed 15 of the 17 fractures that were minimally displaced. At a mean follow-up of 3 (2–5) years after the fracture, 16 had had revision of the components because of excessive wear, loosening, or nonunion.
Interpretation We conclude that a periprosthetic fracture of the greater trochanter through an osteolytic lesion is usually stable and heals without treatment. However, it is associated with poor prosthetic survival because of excessive polyethylene wear.
A fracture of the greater trochanter associated with osteolysis is a rare late complication after total hip arthroplasty (THA) (Heekin et al. Citation1996, Claus et al. Citation2002). Such pathologic fractures may develop after several years following successful uncemented total hip arthroplasty, and result in lateral hip pain and limping. The initial treatment of the fracture, the potential for union of the fracture, and the implications for survival of the prosthesis remain unclear. We began to use the uncemented MicroStructured Omnifit total hip arthroplasty in November 1988. As early as 4 years after surgery, fractures of the greater trochanter in association with osteolysis occurred in some patients. This finding prompted us to review our experience to clarify the incidence and the clinical relevance of this complication.
Patients and methods
From November 1988 through 1993, 1,401 primary hip arthroplasties were implanted in 956 consecutive patients in our center using MicroStructured Omnifit (Osteonics, Allendale, New Jersey) components. We excluded 215 hips that had a bipolar hemiarthroplasty, 198 hips that had cement for fixation of the components, and 101 hips that were unable to complete a 5-year follow-up. Thus, the study group consisted of 887 hips in 672 patients who had a primary uncemented total hip arthroplasty (THA), with a mean follow-up of 11 (5–14) years. The diagnoses for primary THAs were avascular necrosis of the femoral head in 417 hips, osteoarthrosis in 385 hips, rheumatoid arthritis in 52 hips, ankylosing spondylitis in 27 hips and posttraumatic arthrosis following acetabular fracture in 6 hips. There were 433 men and 239 women; and the mean age of the patients was 51 (17–87) years.
The MicroStructured Omnifit THA prosthesis has a metal shell with a modular polyethylene liner that has been sterilized with gamma irradiation in the presence of air. The acetabular cup is made of microstructured titanium alloy and consists of a double-layer coating of American Society for Testing and Materials F-67 Ti beads between 425 and 500 μm in diameter. The femoral stem is straight, double-wedged, and made of cobalt-chromium alloy. All of the femoral components had a circumferential plasma-sprayed porous coating (double layers of 425–500-μm American Society for Testing and Materials F-75 CoCr spherical particles) over their proximal third and a modular femoral head of 32 mm or 26 mm in diameter. The clinical and radiographic follow-ups were carried out postoperatively at 3 months, 6 months, 12 months, and then annually.
We retrospectively reviewed the medical records, radiographs, and operative notes to identify patients with fractures of the greater trochanter associated with a cystic lesion. Osteolysis was defined as a lytic lesion with a scalloped sclerotic border that was not seen on the initial postoperative radiographs. It was differentiated from osteopenia caused by stress shielding in that there is a clear margin around the cyst, an obvious reduction in bone density as compared with the surrounding bone, and the absence of a trabecular pattern in the lesion. The polyethylene linear wear was assessed on serial radiographs using a computer-aided digitizer (Shih et al. Citation1997). The size of the trochanteric osteolysis was measured on the latest radiograph to be taken before the fracture, according to a method that has been decribed previously (Zicat et al. Citation1995).
Statistics
To identify risk factors that might be associated with the occurrence of osteolysis, we compared a number of variables between patients who had osteolysis (either pelvis or femur) and those who did not. These variables included patient factors such as age, gender, body weight, and the diagnosis for THA; and prosthetic factors such as the size of the femoral head and the initial polyethylene thickness. Candidate risk factors were examined independently using univariate logistic regression analysis. All variables were then included in a multiple regression model to determine independently significant predictors of osteolysis. We used a two-tailed Student's t test to compare the annual linear wear rate of the liner and the size of the trochanteric osteolysis between patients who had a fractured trochanter through osteolytic cyst, and patients who had trochanteric osteolysis but without a fracture. For all statistical analyses, a p-value of < 0.05 was considered significant. The Kaplan-Meier survival analysis was used to determine the prosthetic survivorship after fracture, with an endpoint of implant revision for any reason.
Results
We found osteolysis in 252 hips (28%) (203 trochanteric region, 15 acetabular, 34 both), and a pathological fracture of the greater trochanter through the osteolytic lesion in 23 hips (3%). The implants were all stable and not seriously malaligned in any of these 23 patients. The fractures occurred at a mean of 7 (4–11) years postoperatively and were followed for a mean of 4 (2–5) years. In univariate analysis, factors that were significantly predictive of osteolysis included the use of a 32-mm femoral head and the use of a polyethylene liner thinner than 8 mm (). There was no difference regarding age, sex, weight, diagnosis, and average polyethylene thickness between patients who had osteolysis and those who did not. On multiple logistic regression analysis that included all variables, only the use of a thin (< 8 mm) polyethylene liner remained a significant independent predictor of osteolysis, with a relative risk of 2.2 times (95% CI: 1.3–3.9, p = 0.005). The thicknesses of polyethylene and the sizes of the femoral heads used in hips with or without osteolysis are presented in . The annual linear wear rate of the liner was 0.15 (SD 0.6) mm/year in the whole series. Hips with a fractured trochanter had a larger osteolytic lesion and a higher annual wear rate ().
Figure 1. The thickness of polyethylene, and femoral head size used in hips with or without osteolysis.
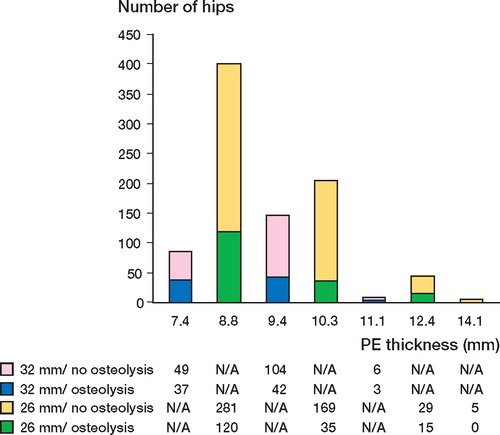
Table 1. Univariate analysis of hips with or without osteolysis
Table 2. Annual linear wear rate and the size of the osteolysis between patients who had a fractured trochanter and patients who had trochanteric osteolysis but no fracture. Values are mean (SD)
16 patients reported no trauma before the fracture, 6 patients slipped without falling, and 1 patient had a fall from riding a bicycle. The fracture was manifested by a sudden episode of lateral hip pain and limp in 14 hips that had no symptoms previously. 7 patients had gradual onset of activity-related pain followed by sudden exacerbation. In 2 other patients, the fracture was asymptomatic and the diagnosis was made by the radiographic findings.
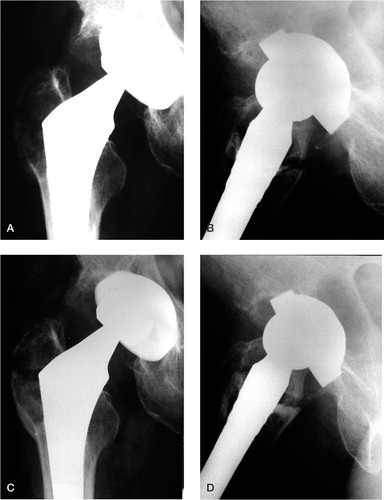
Nonoperative treatment was suggested in 17 patients who had minimal fracture displacement. They were managed with crutch walking, activity restriction and pain-relief medication until the symptoms were resolved. The fracture healed clinically and radiographically in 15 patients at 6–8 weeks (). In 2 hips, however, the fracture did not unite and displaced about 2 cm superiorly.
Figure 2. A 56-year-old man who had THA on the left side 6 years previously presented with gradual onset of lateral hip pain lasting for 2 months without any trauma. The anterior/posterior (A) and the lateral (B) radiographs showed a non-displaced fracture through an osteolytic cyst of the greater trochanter. The prosthesis was well-fixed. 2 years later, the anterior/posterior (C) and the lateral (D) radiographs showed that the fracture had healed. The femoral head was more eccentric, demonstrating polyethylene wear.
2 patients had no symptoms from the fracture. The fractures, although displaced, remained asymptomatic for several years until a revision for reasons other than the fracture.
4 fractures were initially treated with internal fixation, bone grafting of the cyst, and revision of the components (1 metal cup and liner revision, 3 liner and femoral head exchange) because of obvious fracture displacement (). They all healed, one with minimal displacement.
Figure 3A. Anterior/posterior radiograph of a 51-year-old woman taken 7 years after THA, and before the fracture, shows an osteolytic cyst on the greater trochanter and severe polyethylene wear.

Figure 3B. 3 months later, the same patient experienced sudden lateral hip pain after a minor strain. The radiograph showed a displaced fracture through the cyst. She underwent surgery to fix the fracture, bone graft the cyst, and revise the metal shell and the liner.

Figure 3C. A 2-year postoperative radiograph showing that the bone graft had incorporated and the fracture had healed.

Overall, 16 hips had had a revision of the components by the time of the latest follow-up. 12 hips that did not have surgery as acute fracture management had been revised. 5 stems and 3 cups were revised for aseptic loosening. 4 hips underwent femoral head and polyethylene liner exchange because of marked polyethylene wear. The survivorship of the prosthesis 3 years after the fracture was only 37%.
Discussion
Osteolysis and periprosthetic fractures are two well-known complications of total hip arthroplasty (THA). They have usually been discussed separately in the literature, and only rarely and recently has osteolysis been recognized as a risk factor for fractures (Berry Citation2003). Osteolysis of the greater trochanter could decrease the mechanical strength of the host bone and make it susceptible to fracture. The energy required for such a pathological fracture is low: most fractures (16 of 23) in this series developed during normal daily activities without any history of trauma.
It is the current view that wear particles play a major role in inducing osteolysis (Maloney and Smith Citation1996). In our study, inadequate polyethylene thickness (< 8 mm) was an independent risk factor of osteolysis. Although there was no difference comparing the average polyethylene thickness in hips with osteolysis to those without osteolysis, more osteolysis was seen in hips that had a thin liner when polyethylene thickness was dichotomized as less than or greater than 8 mm. It is well known that in a metal-backed prosthesis, polyethylene stress increases rapidly as the polyethylene thickness falls below 8 mm (Bartel et al. Citation1986).
The MicroStructured Omnifit components have a titanium metal shell which is of dual-geometry design and not HA-coated. A modular polyethylene liner which was gamma-irradiated in the presence of air was snap-locked into the shell and fixed at the periphery by metal tabs and a circumferential wire. Polyethylene wear and osteolysis has been a major concern with this type of prosthesis in long-term use (Hellman et al. Citation1999). Improvements in the security of the liner locking mechanism, better conformity of the modular polyethylene insert and the metal cup, and also polishing of the inner aspect of the metal shell, have been improvements introduced recently in an effort to reduce back-side polyethylene wear (Chen et al. Citation1995). Alternative sterilization strategies have been designed to limit or prevent oxidative degradation of the polyethylene and to reduce wear (Sychterz et al. Citation2004).
Implant design and pattern of fixation may also affect the location of osteolysis (Schmalzried et al. Citation1992). We observed more osteolysis in the femur than in the acetabulum (27% as opposed to 6%). One previous study evaluated the same prosthesis after an average of 10 years, and revealed a similar distribution of osteolysis (36% in the femur and 4% in the acetabulum) (Hellman et al. Citation1999). Although it is unclear why this asymmetric distribution developed, we believe that the fact that most (> 80%) metal cups we used were designed with no screw holes may partially explain the difference. The relative lack of accessible pathway for the particulate debris to the periacetabular bone led to lessosteolysis on the pelvic side. In addition, the complex geometry of the pelvis may make diagnosis of osteolysis difficult using plain films, and thus cause the true incidence to be underestimated. Our study and that of Hellman et al. (Citation1999) also indicated that bone ingrowth or fibrous integration on the uncemented femoral components with circumferential porous coating can protect against distal lesions and demonstrate typical periarticular osteolysis. The confinement of bone loss to the proximal portion of the femur increased the possibility of a trochanteric fracture.
Fracture of the greater trochanter in association with osteolysis was first reported in a study of 4 cases (Heekin et al. Citation1996). One later study involving 208 hips with use of the Anatomic Medullary Locking (AML, Depuy, Johnson & Johnson Company, Warsaw, IN) prosthesis reported an incidence of 4% (9 of 208) at a mean of 12 years of follow-up (Claus et al. Citation2002). In our series, the incidence was lower. Although patient profile, degree of activity, and the process used to manufacture the liner may all account for the difference, the design of the prosthesis may be an important factor. The AML femoral stem with its circumferential and extensively porous-coated surface has the inherent risk of stress shielding, which may cause further bone loss in the trochanteric region with a greater chance of pathological fracture (Engh et al. Citation1997). However, as seen in our study, the true incidence may be underestimated since the fractures can be asymptomatic; some patients might not have sought medical attention. The outer border of the greater trochanter is sometimes not visible in the conventional anterolateral pelvic radiographs, making the diagnosis difficult.
We found that the pathological fracture was associated with accelerated wear and more extensive osteolysis. Both lead to poor prosthetic survival. Many of the hips may require revision soon after the fracture. However, since most fractures were considered stable, and in no case was the stability of the femoral component violated by the fracture, closed treatment with limited weight bearing and activities remained a good option. Revision surgery can be delayed until the fracture is stabilized by bony healing or fibrous union.
To avoid progression of osteolysis and pathological fracture, exchange of the polyethylene liner in combination with curettage and bone grafting of the trochanteric cysts represents an aggressive attempt to treat these relatively asymptomatic lesions in patients with well-fixed prostheses. The rationale of this treatment is to heal the cyst and seal the effective joint space in order to remove the cause of osteolysis—the particle generator—by means of changing the polyethylene liner and exchanging the femoral head to a smaller size (26 mm). In one study, this approach prevented progression of femoral osteolysis in 15/17 hips at an average follow-up of 2.5 years (Benson et al. Citation2000).
No competing interests declared.
- Bartel D L, Bicknell V L, Wright T M. The effect of conformity, thickness, and material on stress in ultra-high molecular weight components for total joint replacement. J Bone Joint Surg (Am) 1986; 68: 1041–51
- Benson E R, Christensen C P, Monesmith E A. Particulate bone grafting of osteolytic femoral lesions around stable cementless stems. Clin Orthop 2000, 381: 58–67, (all names)
- Berry D J. Periprosthetic fractures associated with osteolysis: a problem on the rise. J Arthroplasty (Suppl) 2003; 18: 107–11
- Chen P C, Mead E H, Pinto J G, Colwell C W, Jr. Polyethylene wear debris in modular acetabular prostheses. Clin Orthop 1995, 317: 44–56
- Claus A M, Hopper R H, Engh C A. Fractures of the greater trochanter induced by osteolysis with the Anatomic Medullary Locking prosthesis. J Arthroplasty 2002; 17: 706–12
- Engh C A, Jr, Culpepper W J, II, Engh C A. Long-term results of use of the anatomic medullary locking prosthesis in total hip arthroplasty. J Bone Joint Surg (Am) 1997; 79: 177–84
- Heekin R D, Engh C A, Herzwurm M F. Fractures through cystic lesions of the greater trochanter: a cause of late pain after cementless total hip arthroplasty. J Arthroplasty 1996; 11: 757–60
- Hellman E J, Capello W N, Feinberg J R. Omnifit cementless total hip arthroplasty: a 10-year average followup. Clin Orthop 1999, 364: 164–74
- Maloney W J, Smith R L. Periprosthetic osteolysis in total hip arthroplasty: the role of particulate wear debris. Instr Course Lect 1996; 45: 171–82
- Schmalzried T P, Jasty M, Harris W H. Periprosthetic bone loss in total hip arthroplasty. Polyethylene wear debris and the concept of the effective joint space. J Bone Joint Surg (Am) 1992; 74: 849–63
- Shih C H, Lee P C, Chen J H. Measurement of polyethylene wear in cementless total hip arthroplasty. J Bone Joint Surg (Br) 1997; 79: 361–5, (all names)
- Sychterz C J, Orishimo K F, Engh C A. Sterilization and polyethylene wear: clinical studies to support laboratory data. J Bone Joint Surg (Am) 2004; 86(5)1017–22
- Zicat B, Engh C A, Gokcen E. Patterns of osteolysis around total hip components inserted with and without cement. J Bone Joint Surg (Am) 1995; 77: 432–9