Abstract
Background Because of current cost restrictions, we studied the effect of a shorter hospital stay on function, pain and quality of life (QOL) after total hip replacement (THR).
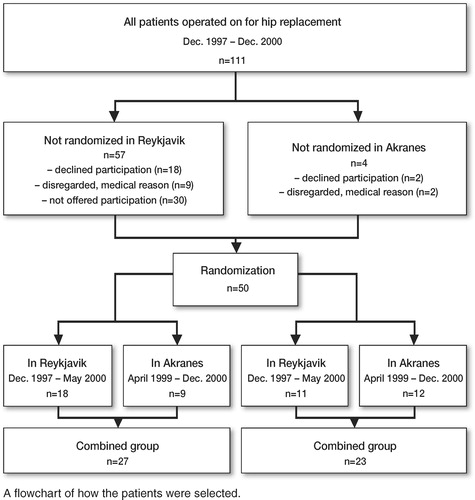
Patients and methods 50 patients from two hospitals were randomized into a study group (SG) of 27 patients receiving preoperative and postoperative education programs, as well as home visits from an outpatient team, and a control group (CG) of 23 patients receiving “conventional” rehabilitation often augmented by a stay at a rehabilitation center.
Results Mean hospital stay was shorter for the SG than for the CG (6.4 days and 10 days, respectively; p < 0.001). During the 6-month study period, there were 9 non-fatal complications in the SG and 12 in the CG (p = 0.3). The difference in Oxford Hip Score between the groups was not statistically significant before the operation, but was better for the SG at 2 months (p = 0.03) and this difference remained more or less constant throughout the study. The overall score from the Nottingham Health Profile indicated a better QOL in the SG.
Interpretation Our preoperative education program, followed by postoperative home-based rehabilitation, appears to be safer and more effective in improving function and QOL after THR than conventional treatment.
In Iceland, the number of THR operations has increased steadily over the past few decades. The current figure is 133 per 100,000. The annual requirement for primary THR in the country is expected to increase by one-third over a period of 20 years, from 221 in 1996 to 300 in 2015 (Ingvarsson et al. Citation1999). One possible way of dealing with cost restrictions by the health authorities is to increase productivity and shorten hospital stay. Before the start of this study in Iceland, the average length of stay after THR at the Landspitalinn University Hospital in Reykjavik was 11 days.
Programs to shorten the length of stay in hospital after THR have been introduced in Scandinavia over the last decade (Kolmert and Barsegård Citation1992, Møiniche et al. Citation1992) and gradual shortening of the hospital stay has been reported (Wong et al. Citation1990, Fisher et al. Citation1997).Unfortunately, many of the existing protocols for postoperative rehabilitation include early transfer to another inpatient rehabilitation unit, which continues to put a strain on hospital resources (Munin et al. Citation1998, Zuckerman Citation1998, Forrest et al. Citation1999). Möller and co-workers (Citation1992) conducted a pilot study and found it feasible to transfer postoperative rehabilitation to the patient’s home. In addition, preoperative education protocols appear to have been effective in shortening the hospital stay (Fischer et al. Citation1997, Weingarten et al. Citation1998, Crowe and Henderson Citation2003) and have had a positive effect on the patient’s ability to cope after undergoing THR (Butler et al. Citation1996, Gammon and Mulholland Citation1996).
Little is known about the functioning and quality of life of patients who are subjected to a shorter stay in hospital. The purpose of this study was to compare the outcome in a group of patients who experienced a shorter hospital stay with preoperative education (augmented with home rehabilitation and nursing) with that in a group of patients who were subjected to current practices in postoperative rehabilitation. We compared the effects of the two treatments on function, pain and quality of life.
Patients and methods
The study was started at the Landspitalinn University Hospital in Reykjavik in December 1997, and at Akranes Hospital in April 1999. The last patient to enter the study was operated at Akranes Hospital in December 2000 (Figure). A posterior approach and the Howse Mk. II implant was used in Reykjavik, but at Akranes Hospital, Charnley hip prostheses were implanted using the Hardinge approach.
Selection of patients
Patients on the waiting list for primary hip replacement at Landspitalinn University Hospital in Reykjavik were invited to participate. Patients diagnosed as having osteoarthosis of the hip, rheumatoid arthritis, primary segmental collapse of the femoral head, and sequelae after developmental diseases and hip trauma, all of whom had been living in their own home, were included. Patients with primary hip fracture, metastastatic tumors, and dementia were excluded.
After the study had started, Landspitalinn Hospital was subjected to financial restrictions and in the second half of the study period, the health authorities had decided to move the unit to another location in Reykjavik. This decision led to problems in recruiting patients to the study, and it was the main reason for the large dropout of eligible patients (Figure). During the same period, a hip replacement unit at the nearby Akranes Hospital was evolving and expanding. Most patients under-going hip replacements at Akranes Hospital were living in the Reykjavik area. We therefore decided to include patients undergoing primary hip replacements at Akranes Hospital also during the latter half of the study period. Patients living in the town of Akranes were also invited to participate.
In Reykjavik, 86 patients were available for randomization during the study period, and 57 patients were contacted. 30 patients from the waiting list could not be contacted and were thus not available for the study. Of those contacted, 18 declined participation and nine others dropped out from participation after being randomized, mainly for medical reasons that meant postponement of the planned operation. At Akranes Hospital, 25 patients fulfilled the inclusion criteria. All were contacted and 21 participated; two declined and two were forced to postpone the operation because of medical contraindications (Figure).
In total, there were 50 patients (26 women) with a mean age of 68 (28–86) years. There were 27 patients (14 women) in the study group (SG), with a mean age of 69 (52–81) years. The remaining 23 patients (12 women) in the control group (CG) had a mean age of 66 (28–86) years. In the SG, 24 patients had osteoarthrosis, 1 had rheumatoid arthritis and 2 had had fractures previously. In the CG, 21 patients had osteoarthrosis, 1 had rheumatoid arthritis and 1 had deformity after Perthes’diseasewarranting a THR.
Study design
Patients were contacted about 2 months before the projected operation. If they were interested in participating in the study, an information booklet was sent by mail. They were contacted again, and if they agreed to participate they were randomized into one of the two groups (SG or CG) by opening a sealed envelope containing a note indicating which group the patient was to be allocated to (Figure).
Control group
The CG was treated according to the clinical procedures already in use, with the exception that they were asked to fill in a general questionnaire on the day before the operation and 2, 4 and 6 months after the operation. Patients in the CG were discharged when rehabilitated, or could be transferred to another rehabilitation facility.
Study group
The patients in the SG participated in a preoperative education and training program, given by a physiotherapist and/or an occupational therapist, about one month before the planned operation. During the education, the patients were informed in detail about postoperative rehabilitation and became familiar with the exercises they were instructed to perform before and after the operation. They became acquainted with various devices to be used for assistance postoperatively and were given these devices prior to the operation. They also received an illustrated brochure containing information on how to move and exercise after the operation.
When an SG patient was discharged (always based on a physician’s decision), a physiotherapist or occupational therapist accompanied the patient home if this was considered necessary. The out-patient nurse administered daily antithrombosis injections, changed wound dressings, removed skin staples and assisted the patient as long as it was needed. During the first 2 weeks after being sent home, the physiotherapist or occupational therapist visited the patient (median number of visits was 4, range 2–9 times) to ensure that the rehabilitation scheme was being followed. The evaluation of the SG patients started on the day before the operation when they filled in the questionnaire, and was done at 2, 4 and 6 months after the operation.
Evaluation
On entry into the study, the patients were asked to fill in a general questionnaire. Function and pain were evaluated using the Oxford Hip Score (OHS) questionnaire (Dawson et al. Citation1996a). The OHS was developed and validated specifically to assess function relating to the hip. It contains 12 questions that are divided equally into two subscales: pain and functional impairment. Each question has 5 response categories (scoring from 1 to 5) and when summed they produce subscale scores of 6–30. Higher scores indicate worse pain and functional impairment. The OHS has been well examined in terms of reliability, validity, and responsiveness to treatment (Dawson et al. Citation1996 b, Citationc, Citationd, Fitzpatrick and Dawson Citation1997).
In addition, the patients answered the Nottingham Health Profile (NHP) (Hunt et al. Citation1986). The NHP is a two-part self-administered health-related questionnaire on quality of life. Part I, used in this study, consists of 38 questions measuring their perceived health status. This is divided into the following 6 domains: lack of energy, pain, emotional reactions, sleep disturbance, social isolation, and physical mobility. The test has been thoroughly tested for reliability and validity (Hunt et al. Citation1980, Citation1986). The NHP has been used to evaluate patients with various diseases and treatments, including hip replacements. It has been found to be an inexpensive method of following up patients with hip replacements (Nilsson et al. Citation1994).
Clinical evaluation was done according to the functional scores of Meurle d’Abuigne and Postel, as modified by Charnley (Citation1972), and the Harris Hip Score (HHS) (Harris Citation1969). Both assessments are administered by staff and are disease-specific. The Meurle d’Abuigne and Postel score is divided into three domains: pain, walking ability, and function on a scale ranging from 1 to 6 points. High scores are associated with normal results within each domain, while low scores indicate the most severe impairment.
The HHS gives a maximum of 100 points, with scores between 90 and 100 indicating good function and excellent results, 80–90 being classified as good, 70–80 as fair, and with lower scores (below 70) signifying poor results. The test has four domains: pain, function, deformity, and motion. Pain and function receive the heaviest weighting (44 and 47 points, respectively). The test has recently been validated and has been found to be useful in evaluating changes after operation in arthritis patients (Söderman et al. Citation2001).
All patients in both groups were evaluated using the general questionnaire, the OHS, NHP, HHS and the d’Abuigne and Postel score prior to operation. 2 months after the operation, all patients were evaluated again using the OHS, NHP, HHS and the d’Abuigne and Postel score. Evaluation at 4 and 6 months was done by means of the OHS and NHP.
The study was approved in Iceland by the National Bioethics Committee and by the Data Protection Commission. It was performed in accordance with the Helsinki agreement, and all patients gave their written informed consent.
Statistics
Description of the outcome is given by number of cases used, median and quartiles (lower and upper) as well as mean and standard deviation. The Friedman test was used to compare measurements over time within each group. Wilcoxon matched-pairs test was used to compare measurements within a group at two different times. The Mann-Whitney U test was used to compare the groups at each time point and the Chi-Square test was used to compare proportions. The level of significance was set at 0.05.
Results
50 patients were entered into the study, of which 27 were randomized to the study group (SG) and 23 to the control group (CG). There was an unequal distribution of the numbers in the SG and CG in Reykjavik (18 and 11), whereas the numbers were roughly equal at Akranes Hospital (9 and 12) (Figure). For the combined groups, the hospital stay for the SG was significantly shorter than for the CG (6.4 days and 10 days, respectively; p < 0.001) (). This statistically significant difference in hospital stay was true for both sites despite a clear difference between sites for the CG, the figure for Akranes Hospital being 12.8 days on average as opposed to 7.6 days for Reykjavik. There was no association between gender and length of hospital stay in either group.
Table 1. Length of hospital stay by treatment group and hospital
All patients in the SG returned directly to their homes, whereas 10/23 of the CG did so. 11 patients from the CG were admitted to a rehabilitation center and 2 went to a patient hotel. The mean time spent at the rehabilitation center was 37 days, and the mean time spent at the patient hotel was 14 days.
5/27 patients in the SG and 11/23 in the CG developed a complication during the time of the study, a difference which was not statistically significant (p = 0.3) (). None of the complications were life-threatening and there were no deaths during the 6 months of follow-up time in the study. 1 patient in the CG was readmitted to the hospital because of a stroke during the study period. 3 of the complications occurred between the second and the fourth month; the remainder had occurred before 2 months.
Table 2. Postoperative complications for the study group (5/27 patients) and control group (11/23 patients)
The success of the operation was evaluated by a number of different methods assessing pre- and postoperative ability of the patients. There was no statistically significant difference between the results of the OHS for the SG and CG groups before the operation (with the results of both hospitals combined). However, the results were in favor of the SG at 2 (p = 0.032), 4 (p = 0.007) and 6 (p = 0.001) months. The difference between the groups observed at 2 months remained more or less constant until the end of the study (). When the different hospitals were examined separately for comparison of the two groups, the same trend was observed but the difference did not reach statistical significance for Akranes Hospital. However, within groups, there was no statistically significant difference between Reykjavik and Akranes (data not shown).
Table 3. Comparison of study group and control group regarding function and pain according to the Oxford Hip Score, and hospital site
Health-related quality of life according to the NHP increased for both groups after the operation. However, the overall score indicated a lower quality of life in the CG. When inspecting the inter-quartile range (IQR), relatively little variance was observed. Before operation, the SG showed better emotional reaction (p = 0.01), and also better values for lack of energy (p = 0.02) and social isolation (p = 0.04). At 2 months follow up, the SG experienced less pain (p = 0.005). At 4 months, there was less emotional reaction (p = 0.02) and less social isolation (p = 0.01) compared to the CG. The SG was also doing better than the CG at 6 months, in four areas: lack of energy (p = 0.007), pain (p = 0.02), physical mobility (p = 0.003) and social isolation (p = 0.03). On the other hand, there were no significant differences in emotional reaction at 6 months, or sleep disturbance at any measurement point. The CG never performed better than the SG on the NHP in any domain and at any time during the study.
There was no significant difference between the groups when using the Harris Hip scale. However, the score was better for the SG both pre- and postoperatively. The median scores for SG and CG before operation were 46 (28–70) and 41 (22–61), respectively. At 2 months, the median score for the SG was 76 (56–93) and for the CG it was 71 (31–83). The results were similar according to the Merule D’Abuigne and Postel score. The SG scored better, and a borderline difference was observed in walking ability to the benefit of the SG (p = 0.05).
Discussion
Our findings suggest that the key to successful early discharge of THR patients may be adequate preoperative education, exercise and training in the use of devices for assistance, and also rehearsal of postoperative physical exercise. When applied in our study, the average hospital stay was successfully shortened from 11 days to 5 days.
There was an unequal distribution of the numbers in the SG and CG in Reykjavik (18 and 11, respectively), whereas the numbers were roughly equal at Akranes Hospital (9 and 12 respectively). At Akranes, the hospital stay was longer, which may be a reflection of the fact that Akranes Hospital is situated in a rural area approximately 50 km from Reykjavik and more cautious measures were taken when discharging patients from that hospital. This longer hospital stay was largely confined to the CG. It is unlikely, however, that this difference affected the results, as there was a highly significant difference in the length of the hospital stay at both sites independently. For this reason, the difference is unlikely to have affected the results from assessment of the intervention.
The reduction in hospital stay seen here was greater than in studies in which an educational program was not used (Wong et al. Citation1999), but similar to that seen in other studies using specific programs designed to shorten hospital stays (Fisher et al. Citation1997, Weingarten et al. Citation1998). These programs differed from our program in that all patients in our SG went home directly. The concept of a hospital-at-home service has already been developed for treating patients with hip fractures and other conditions, with encouraging results (Parker et al. Citation1991, Jones et al. Citation1999, Wilson et al. Citation1999). Similar protocols or pathways have been developed for hip and knee replacement patients also, with no adverse effects on quality of life (Mahomed et al. Citation2000). This finding has been confirmed in our study.
When sending patients home after an operation, the safety of the patients is of considerable importance. All patients in the SG were instructed to contact the hospital or the rehabilitation team if any questions arose. This direct link may have made the patients more confident after the operation, and thus more able to cope, but these patients clearly showed better function, a better quality of life and greater confidence before the operation. The latter consideration may also have contributed to the better outcome. This was independent of gender and age.
Evaluation of the success of the operation with regard to technical issues as well as consideration of function, pain and quality of life is not a straight-forward task. A number of assessment tools have been developed and we applied the 4 tools that are used most commonly (Harris Citation1969, Charnley Citation1972, Hunt et al. Citation1986, Dawson et al. Citation1996a).
The OHS clearly showed a better outcome in the SG than in the CG. This also held true when each study site was analyzed independently. For the other assessment tools, there was a consistent trend in favor of the SG, although not consistently significant statistically. This inconsistency in significant differences when using Harris Hip Score, Merule D’Abuigne and Postel or the NHP scoring may have been due to insufficient power in the study to detect actual differences because of the relatively small number of patients. However, the unidirectional trend toward better outcomes in the SG indicated by all measurement tools used adds strength to the findings.
When tested preoperatively, the SG had better scoring—which may have contributed somewhat to the postoperative results. This tendency may have been because the patients in the SG received their education about 1 month before the operation, but all patients were asked to fill in the questionnaires when admitted to the hospital only a day before the operation. Thus, it is reasonable to assume that the preoperative education had boosted the confidence of the patients in the SG prior to the operation itself.
Despite the same trend in the OHS scores in Reykjavik and Akranes, when examined separately the score did not reach statistical significance for Akranes Hospital. This may have been because Akranes had only about half the number of patients in the SG compared to Reykjavik, and because there was less difference in the scores between the SG and CG at Akranes.Despite this, the first two assessments for the CG reached near-significance statistically in favor of the Akranes group, but there was no other significant difference between the SG and CG at either site.
An obvious drawback in our study was the fact that we were forced to deviate from the original protocol and change from including only patients from the Landspitali University Hospital in Reykjavik. This was reflected in the unequal distribution of the numbers of patients in the various groups. The change was made necessary because major reorganization affecting the Department of Orthopedics at the University Hospital was implemented after the study had started. This was unknown to us and had not been anticipated at the time the study was designed. To accommodate this change, we decided to expand the study to include Akranes Hospital which is situated nearby. A disadvantageous effect on the results might be expected if patients from different hospitals are included in the same material, since different operative methods are often used—as in our study. However, the striking similarity between the results from both hospitals may actually have turned this into an advantage as regards evaluation of the intervention applied in this study. The consistency in the results from both hospitals indicates that there was less bias than might have been expected from the high number of dropouts from the original waiting list, because of internal problems at the hospital and a change in protocol.
In summary, from the point of view of function, pain and quality of life, our results suggest that the length of stay in hospital after THR can be shortened, provided that the patient is offered preoperative education with home-based rehabilitation and nursing after discharge. This in turn might help to optimize the utilization of existing beds for THR.
We are grateful to Asdis Kristjansdottir RPT for invaluable help with data collection and Steinunn Ingvarsdottir RN for the home nursing. Financial support for this study was obtained from the memorial foundation of Helga Jonsdottir and Sigurlidi Kristjansson, Landspitalinn University Hospital Research Foundation, the Icelandic Geriatrical Council Fund, the Göran Bauer Fund and the Swedish Council for Working Life and Social Research.
No competing interests declared.
- Butler G S, Hurley C A M, Buchanan K L, Smith-Van-Horne J. Prehospital education: effectiveness with total hip replacement surgery patients. Patient Education and Counseling 1996; 29: 189–97
- Charnley J. The long-term results of low-friction arthroplasty of the hip performed as a primary intervention. J Bone Joint Surg (Br) 1972; 54: 61–76
- Crowe J, Henderson J. Pre-arthroplasty rehabilitation is effective in reducing hospital stay. Can J Occup Ther 2003; 70(2)88–96
- Dawson J, Fitzpatrick R, Carr A, Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg (Br) 1996a; 78: 185–90
- Dawson J, Fitzpatrick R, Murray D, Carr A. The problem of "noise" in monitoring patient based outcomes: generic, disease-specific and site-specific instruments for total hip replacement. J Health Serv Res Policy 1996b; 1(4)224–31
- Dawson J, Fitzpatrick R, Murray D, Carr A. Comparison of measures to assess outcomes in total hip replacement surgery. Quality in Health Care 1996c; 5: 81–8
- Dawson J, Fitzpatrick R, Frost S, Gundle P, McLardy-Smith P, Murray D. Evidence for the validity of a patient-based instrument for assessment of outcome after revision hip replacement. J Bone Joint Surg (Br) 2001d; 83: 1125–9
- Fisher D A, Trimble S, Clapp B, Dorsett K. Effect of a patient management system on outcomes of total hip and knee arthroplasty. Clin Orthop 1997, 345: 155–60
- Fitzpatrick R, Dawson J. Health-related quality of life and the assessment of outcomes of total hip replacement surgery. Psychol Health 1997; 12: 793–803
- Forrest G P, Roque J M, Dawodu S T. Decreasing length of stay after total joint arthroplasty: effect on referals to rehabiltation units. Arh Phys Med Rehabil 1999; 80: 192–4
- Gammon J, Mulholland C W. Effect of preparatory information prior to elective total hip replacement on post-operative physical coping outcomes. Int J Nurs Stud 1996; 33: 589–604
- Harris W H. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. J Bone Joint Surg (Am) 1969; 51: 737–55
- Hunt S M, McKennan S P, McEwen J, Backett E M, Williams J, Papp E. A quantitative approach to perceived health status: a validation study. J Epidemiol Community Health 1980; 34: 281–6
- Hunt S M, McEwen J, McKenna S P. Measuring health status. Croom Helm. Dover, New Hampshiere 1986
- Ingvarsson T, Hägglund G, Jonsson H, Jr, Lohmander L S. Incidence of total hip replacement for primary osteoarthrosis in Iceland 1982–1996. Acta Orthop Scand 1999; 70(3)229–33
- Jones J, Wilson A, Parker H, Wynn A, Jagger C, Spiers N, Parker G. Economic evaluation of hospital at home versus hospital care: cost minimisation analysis of data from randomised controlled trial. BMJ 1999; 319: 1547–50
- Kolmert L, Barsegård B. En veckas vårdtid realistiskt mål vid total höftledsplastik. Läkartidningen 1992; 89(18)1563–4
- Mahomed N N, Koo Seen Lin M J, Levesque J, Lan S, Bogoch E R. Determinants and outcomes of inpatient versus home based rehabilitation following elective hip and knee replacement. J Rheumatol 2000; 27: 1753–8
- Munin M C, Rudy T E, Glynn N W, Crossett L S, Rubash H E. Early inpatient rehabilitation after elective hip and knee arthroplasty. JAMA 1998; 279(11)847–52
- Møiniche S, Hansen B L, Christensen S-E, Dahl J B, Kehlet H. Patientaktivitet og indlæggelsetid efter hoftealloplastik med balanceret smertebehandling og tidlig mobilisation. Ugeskr Læger 1992; 154(21)1495–9
- Möller G, Goldie I, Jonsson E. Hospital care versus home care for rehabilitation after hip replacement. Int J Technol Assessm Health Care 1992; 8(1)93–101
- Nilsson L T, Franzén H, Carlsson Å S, Önnerfält R. Early radiographic loosening impairs the function of a total hip replacement: The Nottingham Health Profile of 49 patients at five years. J Bone Joint Surg (Br) 1994; 76: 235–9
- Parker M J, Pryor G A, Myles J W. Early discharge after hip fracture: prospective 3-year study of 645 patients. Acta Orthop Scand 1991; 62(6)563–6
- Söderman P, Malchau H. Is the Harris Hip Score system useful to study the outcome of total hip replacement. Clin Orthop 2001, 384: 189–97
- Weingarten S, Riedinger M S, Sandhu M, Bowers C, Ellrodt G, Nunn C, Hobson P, Greengold N. Can practice guidelines safely reduce hospital length of stay? Results from a multicenter interventional study. Am J Med 1998; 105: 33–40
- Wilson A, Parker H, Wynn A, Jagger C, Spiers N, Jones J, Parker G. Randomised controlled trial of effectiveness of Leicester hospital at home scheme compared with hospital care. BMJ 1999; 319: 1542–6
- Wong J, Wong S, Nolde T, Yabsley R H. Effects of an experimental program on post-hospital adjustment of early discharged patients. Int J Nurs Stud 1990; 27: 7–20
- Wong J, Wong S, Brooks E, Yabsley R H. Home readiness and recovery pattern after total hip replacement. J Orthop Nurs 1999; 3: 210–9
- Zuckerman J D. Inpatient rehabilitation after total joint replacement (editorial). JAMA 1998; 279(11)880