Abstract
Background The designs of total ankle prostheses have changed in recent years in order to give better performance. Only a few studies of these ankle prostheses have been published, however, and none on micromotion.
Patients and methods We evaluated 5 patients with rheumatoid arthritis and 5 with osteoarthosis, 4 (3–5) yearsafter arthroplasty with the double-coated STAR prosthesis.
Clinical examination included AOFAS hindfoot score. Standardized a-p and lateral radiographs were taken and RSA analyses were done at regular intervals.
Results There was no difference in results between ankles operated on due to rheumatoid arthritis and due to osteoarthrosis. A rapid initial migration was observed for the tibial components at 6 weeks, but thereafter all but 1 implant seemed stable. The migration pattern for the talar component was similar.
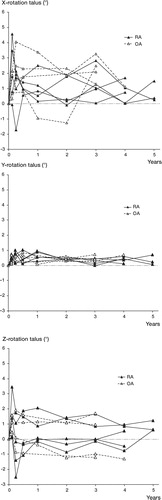
Rotation around the 3 axes was observed for the tibial components at 6 weeks, but not thereafter. The talar components became stable for rotation around the longitudinal and sagittal axes, but not around the transverse axis. 8 out of 10 ankles were painless. The median total AOFAS score was 83 and the median range of motion was 32°. None of the 20 components had changed position and there were no signs of bone resorption.
Interpretation Provided the indication is adequate and the prosthesis has been implanted correctly, the double-coated STAR ankle prosthesis will have a satisfactory fixation to underlying bone.
The Scandinavian Total Ankle Replacement (STAR) was developed and first implanted in 1981 (Kofoed Citation1986). The first version was intended for fixation by bone cement. In its second version, introduced in 1990, the components had an approximately 100-μm-thick hydroxyapatite layer applied to the metal surfaces and were intended for cementless fixation. In the third version, introduced in 1999, the anchoring surfaces have a double coating of both pure titanium and hydroxyapatite.
We evaluated the extent of migration and rotation of the STAR total ankle prosthesis with time in 10 patients with rheumatoid arthritis (RA) or osteoarthritis (OA).
Patients and methods
5 patients (3 women) suffered from rheumatoid arthritis, and 5 (3 women)from osteoarthrosis. The median age was 61 (50–83) years. The preoperative radiographic changes in patients with rheumatoid arthritis were of grade III and IV (Larsen et al. Citation1977) ().
Table 1. Demographic data and clinical outcome
The tibial and talar components are both made of cobalt-chromium alloy and are intended for uncemented fixation. The anchoring surfaces are coated with an approximately 300-μm-thick layer of titanium (ISO 5832), applied by vacuum plasma spray technology. The pore size is 75–200 μm, and porosity 25–35%. In addition, an approximately 25-μm-thick hydroxyapatite layer (porosity 60%) is applied using an electrochemical process.
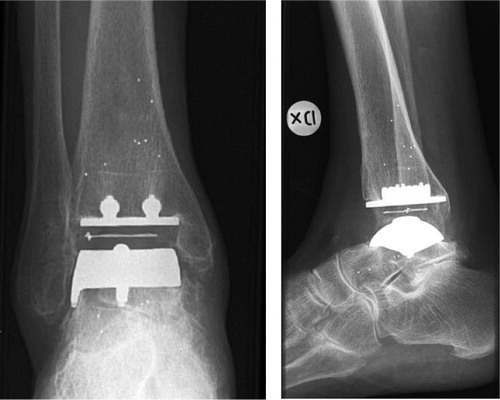
For this study, the manufacturer (W. Link and Co. GmbH, Hamburg, Germany) supplied the tibial and talar components with 3 tantalum beads, each of which had been mounted on the top of metallic towers (). The mobile polyethylene component was sterilized by gamma irradiation in nitrogen-vacuum.
Surgical technique
After having administered prophylactic antibiotics, a tourniquet was applied. The ankle joint was approached via a straight anterior incision, holding the anterior tibial tendon medially. The long extensor to the great toe, the main vessels and the anterior tibial nerve were held laterally. The bone on either side of the joint was excised using the guides belonging to the system. After shaping the talar dome, trials were done to check the cuts and that the components could be seated correctly. The surgical technique has been presented in detail elsewhere (Anderson et al. Citation2004).
Postoperative treatment
Postoperatively, the foot and lower leg were placed in a splint. After 2 days, the wound was inspected and a lower leg cast was applied. Weight bearing was allowed as much as could be tolerated. The cast was changed after 2 weeks. Total time in plaster was 4–5 weeks in OA cases and 6 weeks in RA cases.
Clinical evaluation
The last follow-up was done 4 (3–5) years after surgery. For evaluation of pain and function, we used the AOFAS hindfoot score (Kitaoka et al. Citation1994). The patients were also asked to express whether they were satisfied, somewhat satisfied or dissatisfied, as proposed by Makwana et al. (Citation1995).
Radiographic examination
Conventional a-p and lateral views were obtained 2–3 days after surgery and after 6 and 12 months. Thereafter, the ankles were examined annually. In all cases, the first examination was performed before weight bearing. In order to standardize the films, as exemplified in , we used an image intensifier. The landmarks, lines and angles used to evaluate any change of position of the components have been described previously (Anderson et al. Citation2003).
RSA
For the RSA analyses, we used the uniplanar technique (Selvik Citation1974, Kärrholm Citation1989). The calibration box and the software were supplied by RSA Biomedical, Umeå, Sweden. We used high-resolution films (digital plates) measuring 35 × 43 cm. The ankles were examined after 2–3 days, after 6 weeks, 3 months, 6 months, 1 year, and annually thereafter.
The accuracy of the RSA, i.e. the random error for the method, was determined by double examinations. The patients were examined twice on the same occasion. By making the assumption that no relative movement occurred between the skeleton and the tibial and talar components, respectively, the standard deviation from the expected zero value could be calculated for each component. Using the Student t-distribution, the 99% confidence limits for the smallest significant movement in each direction were determined. 10 double examinations of the tibial component and 9 of the talar component were used for these calculations.
Statistics
We used the Mann-Whitney U-test for comparison of RSA measurements between cases with RA and OA. P-values below 0.05 were considered significant.
Results
Clinical and radiographic evaluation
Surgery was uneventful in all cases and all components were correctly seated. No wound-healing problems were encountered. All patients with RA and 3 of 5 patients with OA reported that their ankle was painless. 2 patients with OA had an AOFAS pain score of 30 points. The median total AOFAS score was 83 (69–96). Median range of motion was 32° (15–40) (). At the last follow-up, none of the 20 components had changed position and no signs of bone resorption were observed around the tibial component.
Radiosterometry
There were no significant differences in any measurements between ankles operated on due to RA and those operated on due to OA (p < 0.1; Mann-Whitney U-test). The levels of significant migration for the tibial and talar components that were determined by double examinations are presented in .
Table 2. The levels of smallest significant migration (mm) and rotation (degrees) at 99% confidence limits in the 3 cardinal axes
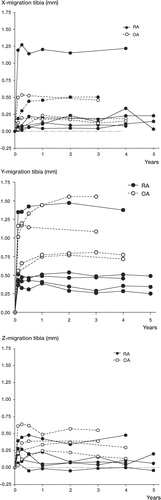
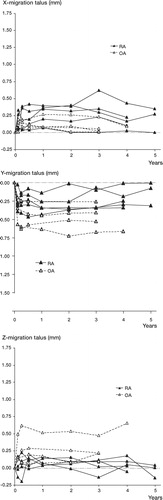
Migration. For the tibia, there was an initial migration in all 3 directions at 6 weeks and all implants remained stable thereafter. The tibial component in one patient with OA migrated proximally for up to two years, however, but it appears to have stabilized. The migration pattern for the talar components was similar to that for the tibial components, with an initial migration followed by stabilization ( and ).
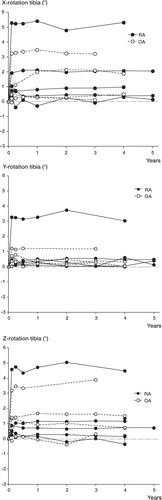
Rotation. For the tibia, there was an initial rotation in all directions for the first 6 weeks and all implants seemed stable regarding rotation thereafter ( and ). After an initial rotation, the talar component was stable in axial and medial-lateral directions, but no stabilization was seen in forward-backward rotation ( and ).
Discussion
This RSA study of ankle prostheses is the first ever published. It was performed after we had implanted more than 60 uncemented STAR prostheses of the second generation, i.e. the single-coated version. By then we had access to the latest set of instruments developed by the manufacturer and a number of trial components produced in our own workshop. This allowed us to make the bone cuts as near perfect as possible and to check that the components were seated correctly before insertion of the definite prosthesis.
The RSA analyses of the uncemented and double-coated STAR ankle prosthesis demonstrated a very limited migration and rotation of the tibial and talar components with time, with the exception of talar rotation in the anteroposterior direction. These observations are difficult to interpret, especially as the clinical scores were in the upper range and most ankles were painless. We did not observe any resorption between metal and bone in the conventional radiographs on the tibial side, and no component had tilted or subsided. The migration values are within the range also observed for hip prostheses. However, the variation in rotation values is higher. This may be explained (1) by the few cases included and (2) as being due to inferior fixation (Stefánsdóttir et al. Citation2004). Whether the higher variability regarding the rotation values is of clinical significance remains to be seen. As with other uncemented prostheses, e.g. tibial plateaus, an initial relatively rapid migration is seen before the components become stable (Nilsson et al. Citation1999, Carlsson et al. Citation2005). With the exception of forward-backward rotation of the talar component, the migrations and rotations seen after the initial 3 months were mainly within the measurement errors of the methods used.
One might have expected inferior results in the cases with rheumatoid arthritis because of the weaker bone, but this was not the case. Processes at the metal-bone interface can easily be seen on the tibial side. However, it should be pointed out that there is no method to reveal what is happening beneath the metallic talar cap. Even if there is no subsidence, either in the conventional radiographs or at the RSA analysis, bone beneath the talar component may become necrotic—leading to a sudden collapse and sinking or tilting of this component.
The radiographic examination for the RSA analysis was more demanding than for hip and knee prostheses, due to the shape of the components and because the “towers” on which the tantalum beads were placed could not be made as high as would have been desirable. However, by placing the leg obliquely relative to the cage and the film and by bending the knee slightly, we finally succeeded in obtaining films that could be analysed satisfactorily.
In a clinical study with a 3–8-year follow-up of 51 uncemented and single-coated STAR ankle prostheses implanted in patients with rheumatoid arthritis and osteoarthrosis, the 5-year survival (with revision for any reason as endpoint) was about 75% (Anderson et al. Citation2003). However, prostheses inserted during the later part of the study had a higher survival rate, indicating that surgical experience plays an important role. In our series of double-coated components, we have shown that the components are stable regarding migration, and up until now, the rotation seen in the forward-backward direction for the talar component has not been of clinical concern. Whether or not the double-coated design can improve the survival rate further requires to be investigated.
We thank Kristina Haage-Hansson, Department of Diagnostic Radiology, Malmö University Hospital, Sweden, for invaluable help with the radiostereometric examinations. No competing interests declared.
- Anderson T, Montgomery F, Carlsson Å. Uncemented STAR total ankle prostheses. Three to eight-year follow-up of fifty-one consecutive ankles. J Bone Joint Surg (Am) 2003; 85: 1321–9
- Anderson T, Montgomery F, Carlsson Å. Uncemented STAR total ankle prostheses. Three to eight-year follow-up of fifty-one consecutive ankles. Technical update. J Bone Joint Surg (Am) 2004; Suppl 1 Part 2: 103–12
- Carlsson Å, Bjöan A, Besjakov J, Önsten I. Cemented tibial component fixation performs better than cementless fixation. A randomized radiostereometric study comparing porous-coated, hydroxyapatite-coated and cemented tibial components for 5 years. Acta Orthop 2005; 76: 362–9
- Kärrholm J. Roentgen stereophotogrammetry. Review of orthopaedic applications. Acta Orthop Scand 1989; 60: 491–503
- Kitaoka H B, Alexander I J, Adelaar R S, Nunley J A, Myerson M S, Sanders M. Clinical rating system for the ankle-hindfoot, midfoot, hallux and lesser toes. Foot Ankle Int 1994; 15: 349–53
- Kofoed H A. A new total ankle joint prostheses. Material sciences and implant in orthopaedic surgery, R Kossowsky, N Kossowsky. Martinus-Nijhoff, Dordrecht 1986; 75–84
- Larsen A, Dale K, Eek M. Radiographic evaluation of rheumatoid arthritis and related conditions by standard radiographic films. Acta Radiolog (Diagn) 1977; 18: 481–91
- Makwana N K, Morrison P, Jones C B, Kirkup J. Salvage operations after total ankle replacement. The Foot 1995; 5: 180–4
- Nilsson K G, Kärrholm J, Carlsson L, Dalén T. Hydroxyapatite coating versus cemented fixation of the tibial component in total knee arthroplasty: prospective randomized comparison of hydroxyapatite-coated and cemented tibial components with 5-year follow-up using radiostereometry. J Arthroplasty 1999; 1: 9–20
- Selvik G. Roentgen stereophotogrammetry. A method for study of the kinematics of the skeletal system. Acta Orthop Scand 1989, Suppl 232, Thesis 1974
- Stefánsdóttir A, Franzén H, Johnsson R, Ornstein E, Sundberg M. Radiostereometric analysis of 22 primary Exeter femoral stems followed for 5 years. Acta Orthop Scand 2004; 75: 408–14