Abstract
Background Arthrodesis of the ankle joint using screws or external fixation is often a demanding procedure, notably in patients with rheumatoid arthritis. We investigated whether tibio-talocalcaneal arthrodesis with the use of an intramedullary nail is a safe and simple procedure.
Patients and methods We retrospectively reviewed 25 ankles (25 patients) at median 3 (1–7) years after tibio-talocalcaneal arthrodesis because of rheumatoid arthritis. All had been operated on by retrograde insertion of a retrograde nail. 5 types of nail had been used. Complications, functional outcome scores, and patient satisfaction were determined and the radiographs evaluated for healing.
Results All but 1 ankle had a radiographically healed arthrodesis. We recorded 3 deep infections, all healed—in 2 cases after extraction of the nail—and the arthrodesis healed in all 3 patients. The average functional scores at follow-up were high, considering that the patients suffered from rheumatoid arthritis. 23 patients were satisfied with the outcome. We found a correlation between the functional scores and the general activity of the disease expressed as a Health Assessment Questionnaire score.
Interpretation In patients with rheumatoid arthritis, tibio-talocalcaneal arthrodesis with a retrograde intra-medullary nail results in a high rate of healing, a high rate of patient satisfaction, and relatively few complications.
Several fixation methods have been advocated for arthrodesis of the ankle, including multiple screws, Phemister methods, plates, and various external fixation methods. The fusion rate has improved over the past decade due to refined surgical methods (Adams Citation1948, Charnley Citation1951, Adam and Ranawat Citation1976, Lauge-Pedersen et al. Citation1998a, Hanson and Cracchiolo Citation2002). Most reports review cases with posttraumatic arthrosis, and some include various diagnoses (Buratti et al. Citation1994, Kile et al. Citation1994, Chou et al. Citation2000, Goebel et al. Citation2003).
Today, after the introduction of uncemented prostheses with a meniscus made of polyethylene, total ankle replacement has become a common procedure—especially in rheumatoid arthritis (RA). Earlier, primary fusion of the ankle was the most realistic procedure in RA patients and is still so in patients with a serious malposition of the ankle and/or hindfoot. Thus, it is surprising that a search of the literature revealed only a few reports presenting more than 10 RA cases that had undergone ankle fusion (Moran et al. Citation1991, Stone and Helal Citation1991, Cracchiolo et al. Citation1992, Lauge-Pedersen et al. Citation1998 a, Citationb, Madezo et al. Citation1998, Fujimori et al. Citation1999, Mäenpää et al. Citation2001). The rate of pseudarthrosis and other complications when external fixation or compression screws were used has shown great variation.
Adams (Citation1948) described a case of pseudarthrosis after attempted fusion, which healed after reoperation with a flanged, retrograde intramedullary nail. This method was later adopted by others (Carrier and Harris Citation1991, Stone and Helal Citation1991, Madezo et al. Citation1998, Fujimori et al. Citation1999, Chou et al. Citation2000, Medicino et al. Citation2004) who (taken together) reported approximately 50 RA cases treated with a retrograde intramedullary nail. The outcome was generally satisfactory and there were few complications.
We evaluated the mid-term results of primary ankle fusion using retrograde intramedullary nails in 26 patients with rheumatoid arthritis (). In particular, we studied the healing rate, the possibility of correcting varus-valgus deformities, wound healing problems, and patient satisfaction (Makwana et al. Citation1995). We also compared the clinical result of surgery with the general activity of the patients’disease using the Health Assessment Questionnaire (HAQ) score (Fries et al. Citation1980).
Patients
From 1994 through 2000, 29 feet of 26 patients with rheumatoid arthritis were operated on with a tibio-talocalcaneal arthrodesis using a retrograde intramedullary nail (). The operations were performed at 3 hospitals by 8 surgeons. The diagnosis of rheumatoid arthritis was confirmed in all cases according to the A.C.R. criteria (Arnett Citation1989). None of the ankles had previously been treated surgically. All patients had substantial arthritic changes in their ankle and subtalar joints, and 4 had undergone subtalar fusion.
Table 1. Demographic data and data related to surgery and follow–up
1 patient had died before the follow-up examination, and in 3 patients with bilateral surgery only the ankle first operated on was included in the study. From radiographs, the 3 latter patients had a fused ankle on both sides and the functional scores were essentially the same on both sides. Thus, there remained 25 ankles (of 25 patients) for a follow-up examination at a median of 3 (1–7) years after surgery. We could evaluate the radiographs of all 26 cases after 0.3–8 years, however.
During the period 2001–2002, a retrospective clinical follow-up examination was undertaken by one of the authors (TA), who had not taken part in any of the operations. The radiographs were evaluated by one of the other authors (JB), who was unaware of the clinical results. He classified the ankles as fused or not fused, based on the presence or absence of bridging bone.
Surgical technique
Surgery was performed using a tourniquet and with the patient in the supine position. The introduction of the nail and locking screws was controlled by fluoroscopy. The surgical approach varied between the surgeons, but most commonly an anterior and lateral approach was used. After resection, the aim was to fuse the hind foot in a plantigrade position. Autologous bone was grafted in 18 cases and allograft was used in 1 case. The nails were of 5 designs. The flanged Thornton nail, originally designed for hip fractures and arthrodesis of the hip, was used in 6 cases. The “Revision Nail” (Smith & Nephew, Memphis, TN) was used in 14 cases, the Biomet ankle arthrodesis nail (Biomet Orthopedics, Warsaw, IN) in 3 cases, the AIM nail (DePuy Orthopedic, Warsaw, IN) in 2 cases, and the UHN nail (Synthes, Obersdorf, Switzerland)—originally made for fractures of the humerus—in 1 case. All nails, except the Thornton nail, have holes for proximal and distal transverse screw fixation. Distal fixation through the nail and calcaneus was always used in our series, but proximal fixation through the tibial diaphysis was used only in 11/20 cases (). The distal screws were introduced from the lateral aspect of the foot. Fox et al. (Citation2000) has described in detail the method used to perform a tibio-talocalcanear arthrodesis with a retrograde intramedullary nail.
In one department (Lund), a staple for rotary stabilization was applied over the anterior aspect of the resected ankle joint in 2 cases, after having introduced the intramedullary nail. After surgery, the ankle was stabilized in a below-knee plaster cast for an average of 10 (0–19) weeks. Full weight bearing was allowed after an average of 4 (0–10) weeks. The transverse proximal screws were removed in only 1 of the 13 cases in which these were used (ankle no. 26).
Follow-up
We used the Mazur (Mazur et al. Citation1979) and AOFAS (American Orthopedic Foot and Ankle Society) (Kitaoka et al. Citation1994) ankle scoring systems simultaneously for all patients (). With the patient in supine position, the hind foot was examined with respect to varus-valgus and equinus position. Patient satisfaction was classified as satisfied, somewhat satisfied or dissatisfied according to Makwana et al. (Citation1995). For evaluation of the current activity of the rheumatic disease, we used the HAQ score (Health Assessment Questionnaire) (Fries et al. Citation1980). In the HAQ score, a value of 0 implies no disability and the maximum value of 3 means that the patient is so disabled that daily personal assistance is required.
Table 2A. The AOFAS hind-foot score. In our study the score can reach a maximum of 86 points
Table 2B. The Mazur score. In our study the score can reach a maximum of 90 points
Statistics
Correlation was evaluated by a multiple regression equation.
Results ()
In radiographs, all but one ankle (no. 26) had healed. However, it was not possible to evaluate the time when the ankles were consolidated, as follow-up intervals varied for patients and departments. The Mazur score averaged 64 (29–81) of 90 points possible and the AOFAS score averaged 66 (39–84) of 86 points possible.All but 7 patients reported that their ankle was pain-free and they were thus given 40 points for pain in the AOFAS system. Of the 25 patients who could be examined clinically, 23 were satisfied with the result and 2 were somewhat satisfied.
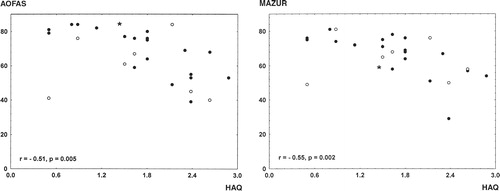
The HAQ score, which represents the activity of rheumatic disease, averaged 1.8 points with a range from 0.5 to 2.88. The total HAQ activity score correlated negatively with the AOFAS and Mazur total scores (r = −0.74, p < 0.001 and r = −0.70, p < 0.001, respectively) ().
Figure 2. Scatter diagrams demonstrating the correlation between HAQ score and AOFAS total score (left) or Mazur total score (right).• group A, ○group B and ☆ group C.
Complications
Wound healing and infection. Ankles no. 1 and 3. Skin necrosis without signs of infection, which healed spontaneously. Ankle no. 22. Deep infection after 6 months. The nail was extracted after 20 months, after which antibiotic treatment was given for several months. Solid radiographic fusion.
Ankle no. 24. Deep infection and skin necrosis. The wound healed after skin transplantation and antibiotic therapy. Radiographically fused.
Ankle no. 25. Deep infection. The nail was extracted after 4 months. Antibiotic therapy was given and the ankle fused, without further intervention. The ankle became radiographically fused.
Ankle no. 26. Skin infection and skin necrosis, which healed uneventfully with antibiotic therapy. Radiographically not fused.
Malposition. 7 cases had a valgus (6) or varus (1) malposition between 6° and 15°. In 4 additional cases, we observed an equinus position between 3° and 10°.
Neurological complications. Remaining sensory loss in the anterior and plantar aspect of the foot was observed in 7 ankles (). This was most probably due to intraoperative injury to a branch of either the sural or the posterior tibial nerve. This sensory loss was not of major inconvenience to the patient.
Discussion
We found that tibio-talocalcaneal arthrodesis with the use of a retrograde intramedullary nail in patients with rheumatoid arthritis resulted in a high radiographic healing rate: 25/26 cases. Of the 10 cases with a residual malposition, all but 1 were satisfied with the result. The method we used cannot always fully correct a severe varus or valgus deformity that is partly located at the talonavicular joint.
The median Mazur score was 68 of 90 points possible and the median AOFAS score was 69 of 86 points possible These scores are at the same level as those in patients operated on with arthrodesis of the ankle due to primary and secondary osteoarthrosis (Anderson et al. Citation2002). We found that the AOFAS and Mazur total scores correlated negatively with the activity of the rheumatic disease (). Thus, these scoring systems do not seem to be optimal instruments for the evaluation of clinical results in patients with rheumatoid arthritis (). In future studies, a simple but relevant outcome score would be highly welcomed. In our opinion, a validated score concentrating on pain and patient satisfaction would be the most realistic tool in RA patients—in whom gait is much impaired by the disease itself and by destruction of other joints.
For many years, external fixation was the most frequently used method of fusing a rheumatoid ankle (Charnley Citation1951, Dereymacker et al. Citation1998). A variety of, and high rate of complications have been reported with this method (Moran et al. Citation1991, Chou et al. Citation2000, Mäenpää et al. Citation2001). Fixation by compression screws is considered to be a less suitable method for rheumatic patients, due to their osteoporotic bone (Cracchiolo et al. Citation1992, Chou et al. Citation2000). There is apparently a need for an alternative and more reliable method. Intramedullary nails can be used safely in patients with rheumatoid arthritis, as their subtalar joints are often fused or diseased. Such nails have also been shown to result in a biomechanically more stable fixation than compression screws (Berend et al. Citation1997). Fixation by an intramedullary nail also allows early weight bearing, which is important in this group of patients. In our patients the proximal screws were not removed before weight bearing, even though removal of the proximal screw is recommended to allow compression in the arthrodesis. Intramedullary nails of different designs all appear to be reliable. It is remarkable that even the primitive Thornton nail, without interlocking screws, also resulted in radiographically confirmed healing in all 6 cases—and none of these nails had a tendency to slide distally and cause pain in the heel.
Patients with rheumatoid arthritis are often disabled due to the fact that many joints are affected. External fixation and compression screws usually imply longer periods of non-or partial weight bearing which, in these patients, may require a long time spent under strict medical care. By using a retrograde intramedullary nail, the time to full recovery and full weight bearing can be reduced.
Generally speaking, wound healing complications, infections, pseudarthrosis, and difficulties in aligning the hindfoot are more frequent in rheumatic cases (Moran et al. Citation1991, Cracchiolo et al. Citation1992, Nasser and Cracchiolo Citation2001). All these problems may become less common with the use of a retrograde intramedullary nail. At the same time, rehabilitation is facilitated. The method seems to work well irrespective of the operating surgeon, since 3 hospitals and 8 surgeons were involved in our series, and 5 types of nails were used.
The most frequent complication in our study was a permanent but tolerable sensory loss on the plantar aspect of the foot. This complication is difficult to avoid, as the branches of the sural and posterior tibial nerve are not seen during the surgical procedure (Berend et al. Citation1997, Fox et al. Citation2000, Mader et al. Citation2003). However, with a blunt dissection distal to the weight-bearing part of the heel, the risk of nerve damage may be minimal.
Today, total ankle replacement is presumably the first choice in RA patients with a well or only slightly malaligned ankle joint, provided that the talar body is preserved. If not, arthrodesis is the treatment of choice. In such cases, tibio-talocalcaneal arthrodesis with a retrograde intramedullary nail is a method that results in a high rate of healing, a high rate of patient satisfaction, and complications that are tolerable. The procedure is not demanding and seems to work well in the hands of different surgeons.
No competing interests declared.
- Adam W, Ranawat C S. Arthrodesis of the hindfoot in rheumatoid arthritis. Orthop Clin North Am 1976; 7: 827–40
- Adams C J. Arthrodesis of the ankle joint. J Bone Joint Surg (Br) 1948; 30: 506–11
- Anderson T, Montgomery F, Besjakov J, Verdier H, Carlson Å. Arthrodesis of the ankle for non-inflammatory conditions - healing and reliability of outcome measurements. Foot Ankle Int 2002; 23: 390–3
- Arnett F C. Revised criteria for the classification of rheumatoid arthritis. Bull Rheum Dis 1989; 38: 1–6
- Berend M E, Glisson R R, Nunley J A. A biomechanical comparison of intramedullary nail and crossed lag screw fixation for tibiotalocalcaneal arthrodesis. Foot Ankle Int 1997; 18: 639–43
- Buratti R A, Johnson J D, Buratti D. Concurrent ankle and subtalar joint arthrodesis. J Foot Ankle Surg 1994; 33: 278–82
- Carrier D A, Harris C M. Ankle arthrodesis with vertical Steinmann's pins in rheumatoid arthritis. Clin Orthop 1991, 268: 10–4
- Charnley J. Compression arthrodesis of the ankle and shoulder. J Bone Joint Surg (Br) 1951; 33: 180–91
- Chou L B, Mann R A, Yaszay B, Graves S C, McPeake W T, III, Dreeben S M, Horton G A, Katcherian D A, Clanton T O, Miller R A, Van Manen J W. Tibiotalocalcaneal arthrodesis. Foot Ankle Int 2000; 21: 804–8
- Cracchiolo A, III, Cimino W R, Lian G. Arthrodesis of the ankle in patients who have rheumatoid arthritis. J Bone Joint Surg (Am) 1992; 74: 903–9
- Dereymaeker G P, Van Eygen P, Driesen R, De Ferm A. Tibiotalar arthrodesis in the rheumatoid foot. Clin Orthop 1998, 349: 43–7
- Fox I M, Shapero C, Kennedy A. Tibiotalocalcaneal arthrodesis with intramedullary interlocking nail fixation. Clin Podiatric Med Surg 2000; 17: 19–31
- Fries J F, Spitz P, Kraines R G, Holman H R. Measurement of patient outcome in arthritis. Arthritis Rheum 1980; 23: 137–45
- Fujimori J, Yoshino S, Koiwa M, Nakamura H, Shiga H, Nagashima, S. Ankle arthrodesis in rheumatoid arthritis using an intramedullary nail with pins Foot Ankle Int. 1999; 20: 485–90
- Goebel M, Mückley T, Gerdesmeyer L, Militz M, Bühren V. Die kombinierte Kompressions-marknagelarthrodese von OSG und USG. Unfallchirurg 2003; 106: 633–41
- Hanson T W, Cracchiolo A, III. The use of a 95° blade plate and a posterior approach to achieve tibiotalocalcaneal arthrosis. Foot Ankle Int 2002; 23: 704–10
- Kile T A, Donnelly R E, Gehrke J C, Werner M E, Johnson K A. Tibiotalocalcaneal arthrodesis with an intramedullary device. Foot Ankle Int 1994; 15: 669–73
- Kitaoka H B, Alexander I J, Adelaar R S, Nunley J A, Myerson M S, Sanders M. Clinical rating system for the ankle-hindfoot, midfoot, hallux and lesser toes. Foot Ankle Int 1994; 15: 349–53
- Lauge-Pedersen H, Knutson K, Rydholm U. Percutaneus ankle arthrodesis in the rheumatoid patient without debridement of the joint. The Foot 1998a; 8: 226–9
- Lauge-Pedersen H, Odenbring S, Knutsson K, Rydholm U. High failure with the dowel technique for fusion of rheu-matoid ankles. The Foot 1998b; 8: 147–9
- Mäenpää H, Lehto M UK, Belt E A. Why do ankle arthrodeses fail in patients with rheumatic disease. Foot Ankle Int 2001; 22: 403–8
- Mader K, Pennig D, Gausepohl T, Patsalis T. Calcaneota-lotibial arthrodesis with a retrograde posterior-to-anterior locked nail as a salvage procedure for severe ankle pathology. J Bone Joint Surg (Am) 2003; 85: 123–8, (Suppl 4)
- Madezo P, De Cussac J B, Gouin F, Bainvel J V, Passuti N. Arthrodèse combinée tibio-talienne et sous-talienne par clou transplantaire dans l'arrière pied rhumatoïde. (Arthrodesis of the hind-foot using a retrograde Küntscher nail in rheumatoid arthritis). Rev Chir Orthop 1998; 84: 646–52
- Makwana N K, Morrison P, Jones C B, Kirkup J. Salvage operations after failed total ankle replacement. The Foot 1995; 5: 180–4
- Mazur J M, Schwartz E, Simon S R. Ankle arthrodesis. Long-term follow-up with gait analysis. J Bone Joint Surg (Am) 1979; 61: 964–75
- Mendicino R W, Catanzariti A R, Saltrick K R, Dombeck M F, Tullis B L, Statler T K, Johnson B M. Tibiotalocalcaneal arthrodesis with retrograde intramedullary nailing. J Foot Ankle Surg 2004; 43: 82–6
- Moran C G, Pinder I M, Smith S R. Ankle arthrodesis in rheumatoid arthritis. Acta Orthop Scand 1991; 62: 538–43
- Nassar J, Cracchiolo A, III. Complications in surgery of the foot and ankle in patients with rheumatoid arthritis. Clin Orthop 2001, 391: 140–52
- Stone K H, Helal B. A method of ankle stabilization. Clin Orthop 1991, 268: 102–6
