Abstract
Background Malunions or nonunions after displaced talar fractures cause significant disability. Salvage procedures such as corrective arthrodesis do not restore normal foot function.
Methods Between 1994 and 2002, we treated 10 patients (aged 15–50 years) who had painful malunions with secondary anatomical reconstruction, at a mean of 1 year after sustaining displaced fractures of the talar body or neck. 5 patients were classified as type I (malunion and/or residual joint displacement), 2 as type II (nonunion with displacement) and 3 as type III (malunion with partial avascular necrosis, AVN). Correction was by an osteotomy through the malunited fracture or removal of the pseudarthrosis. Internal fixation was achieved with screws and additional bone grafting if necessary.
Results No wound healing problems or infections were seen. Solid union was obtained without redislocation in all cases, with no signs of development or progression of AVN. At a mean of 4 (1–8) years after reconstruction, all patients were satisfied with the result—except one patient who required ankle fusion 8 years after reconstruction. The mean AOFAS Ankle Hindfoot Score increased from 38 to 86 (p < 0.001).
Interpretation Secondary anatomical reconstruction with joint preservation leads to considerable functional improvement in painful talar malunions. Partial AVN does not preclude good to excellent functional results. The quality of the bone stock and joint cartilage (rather than the time from injury) appears to be important for the choice of treatment.
Salvage procedures after talar malunions with joint involvement include reorientating arthrodesis of the ankle, subtalar and/or talonavicular joints, and tibiocalcaneal arthrodesis with or without astragalectomy (Canale and Kelly Citation1978, Frawley et al. Citation1995, Gagneux et al. Citation1997, Kitaoka and Patzer Citation1998, Rockett et al. Citation1998, Liener et al. Citation1999, Asencio et al. Citation2000). Although these measures frequently result in substantial improvement, none of them will restore normal foot function. Anatomical reconstruction of malunited talar fractures thus appears attractive if the joint cartilage is still viable, and no talar collapse or infection has occurred. To date, surgical restoration of the anatomical shape of the talus after malunion of a displaced body or neck fracture with preservation of the essential joints has only been reported anecdotally (Zwipp et al. Citation1998, Monroe and Manoli Citation1999, Hansen Citation2000). We hypothesized that near-normal foot function can be restored in cases of residual deformity after overlooked or improperly treated talus fractures with axial malalignment and joint incongruity.
Patients and methods
Between January 1994 and December 2002, we treated 10 patients with painful residual joint displacement, malunion or nonunion after sustaining a closed fracture of the talar body or neck, with secondary anatomical reconstruction. During the same period, 101 patients with acute talar body and neck fractures had been treated mainly with open reduction and internal fixation at our institution. 26 patients with severe posttraumatic arthrosis, collapse of the talar dome after total avascular necrosis (AVN) or septic talar necrosis were treated with arthrodesis procedures. Mean patient age at the time of secondary reconstruction was 32 (15–50) years. Patients presented with intractable pain, incapacity in weight bearing and severe functional impairment—with restricted range of motion mostly in the ankle, subtalar and mid-tarsal joints—at a mean of 10 (1–45) months after the injury. 7 patients had originally sustained talar neck fracture (3 Hawkins type II, 3 type III and 1 type IV) and 3 patients had sustained a talar body fracture (2 Marti type III and 1 type IV). Ipsilateral injuries to the foot and ankle were seen in 4 patients (2 lateral ankle ligament ruptures, 1 combined ankle and subtalar instability, and 1 malleolar fracture). Initially, 3 patients had been treated operatively with open reduction and K-wire or screw fixation, and 5 patients had been treated nonoperatively. The fracture had been overlooked at first presentation in 2 patients.
The talar deformities were classified as described previously (Zwipp and Rammelt Citation2003) (Table). The malunited fractures were evaluated preoperatively with anteroposterior, dorsoplantar and lateral weight-bearing radiographs. CT scans were obtained for all patients to permit precise preoperative planning. If there was any suspicion of AVN in these investigations, we used MRI to confirm its presence and determine how extensive it was. Patients were classified as type I (malunion and/or residual deformity with joint displacement) in 5 cases, type II (nonunion with joint displacement) in 2 cases and type III (types I or II with partial AVN) in 3 cases. 8 patients with complete AVN and collapse of the talar body (type IV malunions), 2 patients with evidence of osteomyelitis (type V malunions) and 16 patients with type I–III deformities and severe, symptomatic posttraumatic arthrosis were not considered suitable for anatomical reconstruction and were therefore excluded from the study. Routine leukocyte counts and serum levels of C-reactive protein were obtained for all patients considered for secondary reconstruction in order to rule out infection. All patients were evaluated prospectively with respect to activity level, pain, functional deficit, radiographic evidence of posttraumatic arthrosis and/or AVN, clinical presentation of the foot deformity and neurovascular deficit. We used the AOFASankle/hindfoot scale (Kitaoka et al. Citation1994) and the Maryland Foot Score (Sanders et al. Citation1992) to determine hindfoot function.
Classification of posttraumatic talar deformities (Zwipp and Rammelt Citation2003)
Surgery was carried out with a tourniquet being placed at the ipsilateral thigh and the iliac crest draped free in order to allow autologous bone grafting when necessary. Patient position and surgical approach depended on the type and location of the deformity. For malunited fractures of the talar neck we used an anteromedial approach, which allowed exposure of the ankle and talonavicular joints. If the subtalar joint had to be corrected and in cases of additional malunion of the lateral process of the talus, a combined anteromedial and oblique lateral (Ollier's) approach was used. For correction of malunions of the talar body, a medial malleolar osteotomy was performed. In one case of malunited posterior talar body fracture, a posteromedial approach was used. We treated solid malunions with correctional osteotomy along the former fracture plane. We performed a complete resection of the pseudarthrosis until viable bone became visible in cases with nonunion. The resulting defect was filled with autologous bone grafting from the ipsilateral iliac crest. Subchondral drilling was performed in the 3 cases with partial AVN. Additional measures included arthrolysis of the ankle and subtalar joints, revision of the sinus tarsi, and extensor tenolysis. After anatomical reconstruction, fragment fixation was achieved with 3.5-mm screws. In one patient with intraoperative evidence of posttraumatic arthrosis of the subtalar joint, subtalar arthrodesis was performed with 6.5-mm screws while the ankle joint was reconstructed and preserved.
Postoperatively, a split non-weight-bearing below-the-knee cast was applied for 3–5 days and the leg was elevated. The cast was removed for isometric exercises which were begun on the first postoperative day, and otherwise it was retained for soft tissue support. Patients were mobilized with crutches under partial weight bearing of 15 kp. Range of motion exercises of the ankle, subtalar and midtarsal joints were initiated on the second postoperative day. Patients were protected in a special ankle-spanning boot (Variostabil, Adidas Inc., Herzogenaurach, Germany) which has also been used for after-treatment of subtalar and ankle arthrodesis as well as malleolar fractures (Biewener et al. Citation2002). Irrespective of the presence of partial AVN, full weight bearing was allowed after radiographic evidence of bone union at an average of 12 weeks postoperatively.
We followed patients at our outpatient clinic for 6 months. During this time, patients were assessed with respect to subjective satisfaction, pain, early wound complications, sural nerve function, bony union and the presence or absence of avascular necrosis of the talar body. All patients were reevaluated with an extensive protocol at a mean of 4 (1–8) years postoperatively. A questionnaire was filled out regarding residual pain, level of activity, subjective complaints and performance during activities of daily life, work and sports. Clinical examination included assessment of the scar quality, swelling, sural nerve symptoms, hindfoot alignment, the ability to walk on heel or tiptoe, muscular and tendinous problems, hindfoot stability and pain with lateral/medial stress. Range of motion in the ankle, subtalar and midtarsal joints was measured with a goniometer and compared to that of the unaffected side.
Functional results were evaluated with the ankle/hindfoot scale of the American Orthopedic Foot and Ankle society (AOFAS, Kitaoka et al. Citation1994) and the Maryland Foot Score (Sanders et al. Citation1992).
The differences between postoperative scores and preoperative scores were evaluated statistically with the paired Student's t-test. Significance was assumed at p < 0.05. Arthrotic changes of the ankle and mid-tarsal joints were recorded with a modified Bargon scale (Bargon and Henkemeyer Citation1977). The absence of arthrosis was assigned grade 1, mild arthritis (subchondral sclerosis, lateral osteophytes) grade 2, severe arthrosis (subchondral cysts, narrowing of the joint space, uneven joint surfaces) grade 3. The degree of posttraumatic arthritis was compared with the preoperative status of the joints. Bony union and the presence of AVN of the talar body were assessed on anteroposterior and lateral weight-bearing radiographs. AVN was considered to be “partial” if less than one-third of the talar body was involved, and “complete” if more than one-third of the talar body was affected—leading to talar collapse (Rammelt et al. Citation2002).
Results
No postoperative complications such as wound healing problems (diastasis, wound edge necrosis etc.) or infections were seen. Solid union was obtained without redislocation in all cases. No development of AVN was observed after correction of type I and II deformities. In patients with preexisting partial AVN (type III deformity), no progression of the AVN was seen.
All but 1 patient stated that they were fully satisfied with the result, and stated that under the same circumstances they would undergo the procedure again. 1 patient with a talar body fracture progressed to posttraumatic arthritis of the ankle and required ankle fusion 8 years after reconstruction of a malunited Hawkins type III fracture of the talar neck. In one patient, an exostosis causing anterior ankle impingement was removed from the dorsal aspect of the talar neck 1 year after reconstruction. Thereafter, the course was uneventful. Excluding the patient with late ankle arthrodesis, range of motion was reduced by a mean of 8.5° (0–15) at the ankle and 7.0° (0–25) at the subtalar and mid-tarsal joints as compared to the unaffected side. Radiographic arthritic changes progressed in the ankle joint by 1° in 3 patients and by 2° in 1 patient. The latter went on to ankle fusion. Progression of arthrioic changes by 1° in the subtalar and talonavicular joints was noted in 2 patients each.
The mean score according to the AOFAS ankle/hindfoot scale increased significantly from a mean of 38 (26–67) to a mean of 86 (55–100) at the time of follow-up (p < 0.001). The mean Maryland Foot Score increased significantly from a mean of 44 (33–79) to a mean of 87 (48–100) at the time of follow-up (p < 0.001). No statistically significant differences were observed for the three different groups of malunions. The functional results were not affected by the type of fracture, by the presence of early arthrosis or partial AVN, and by the time between injury and correction. The 3 patients who had been treated mainly by open reduction and internal fixation with residual displacement had lower AOFAS scores than those seven who had been treated primarily by closed methods or who had been neglected (74 vs. 92). The same tendency was found with the Maryland Foot Score (72 vs. 94). These differences were not statistically significant, however. The preoperative scores, presence of arthrosis or AVN did not differ between the two groups.
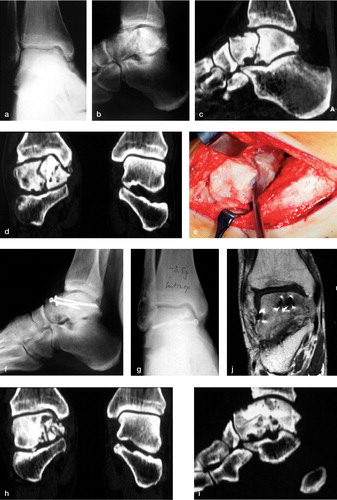
Figure 1. Reconstruction of a displaced talar nonunion (type II deformity). A 50-year-old man presented with a talar non-union and displacement at the ankle joint posterior to the talar neck (a-d) 4 years after a bicycling accident. The fracture had been overlooked initially. Treatment consisted of debridement of the pseudarthrosis (e), bone grafting from the ipsilateral iliac crest and screw fixation (f, g). CT-scanning after surgery showed a congruent joint reconstruction (h, i). MRI at 5 months after surgery showed no signs of AVN (j). At follow-up after 2.5 years, the patient was pain free and had normal function of the ankle and subtalar joints. Weight-bearing radiographs showed no AVN or progression of arthritic changes as compared to the preoperative radiographs (k-m).
Discussion
The unique anatomy of the talus—with its contribution to three essential joints of the foot and two-thirds of cartilage coverage—makes its anatomical integrity and joint congruency indispensable for normal foot function (Hawkins Citation1970, Marti Citation1974). Consequently, posttraumatic deformities of the talus almost invariably lead to painful functional impairment. Typical findings of malunited talar fractures are varus malalignment of the talar neck, nonunion after talar neck or body fractures, joint incongruency, avascular necrosis, posttraumatic arthritis, impingement of the posterior tibial tendons and tarsal tunnel syndrome secondary to prominent malaligned bone fragments (Peterson et al. Citation1977, Canale and Kelly Citation1978, Baumhauer and Alvarez Citation1995, Daniels et al. Citation1996, Zwipp and Rammelt Citation2003). To date, salvage procedures after talar malunions with joint involvement have consisted mainly of arthrodesis of the affected joints. Numerous studies have described ankle, subtalar and talonavicular, tibiotalocalcanear or triple arthodesis for posttraumatic arthritis, malunion, nonunion or AVN (Canale and Kelly Citation1978, Frawley et al. Citation1995, Gagneux et al. Citation1997, Kitaoka and Patzer Citation1998, Rockett et al. Citation1998, Liener et al. Citation1999, Asencio et al. Citation2000, Chou et al. Citation2000, Easley et al. Citation2000). More recently, total ankle arthroplasty has become an alternative to ankle arthrodesis in cases in which only the ankle joint is affected (Hintermann and Valderrabano Citation2003). However, total ankle replacement may be prone to loosening with partial AVN or defective after pseudarthrosis removal in the talus, since some authors have reported that the talar component is more liable to failure than the tibial component (Buechel et al. Citation2003, Knecht et al. Citation2004, Spirt et al. Citation2004). Moreover, for the subtalar and talonavicular joints, no reliable arthroplasty option exists at present.
Figure 2. Reconstruction of a talar malunion with partial AVN (type III deformity). A 21-year-old man presented with painful malfunction of the foot 6 months after non-operative treatment of a displaced fracture of the talar neck (Hawkins Type III) with dislocation at the ankle and subtalar joints (a). Initially, closed reduction was attempted and a below-the-knee cast was applied (b). The lateral radiographs after 6 months showed a considerable step-off in the articular surface, with severe ankle impingement. Reduced radiolucency of the superior aspect of the talar dome indicated partial avascular necrosis (c). Intraoperative aspect of the malunited talus after osteotomy of the medial malleolus (d). Anatomical reconstruction of the ankle and subtalar joints was achieved with a talar neck osteotomy through the former fracture, reorientation of the talar body and screw fixation (e, f).3 years after reconstruction, the patient had an excellent clinical result. No arthrotic changes and no progression of the AVN could be seen (g, h).

Although arthrodeses reportedly provided substantial pain relief, functional impairment prevails and the long-term outcome is limited due to the development of degenerative changes in the adjacent joints (Coester et al. Citation2001, Fuchs et al. Citation2003). The results of triple arthrodesis for the treatment of varus malalignment of the talar neck have been reported to be unsatisfactory (Canale and Kelly Citation1978). Anatomical reconstruction of malunited talar fractures with preservation of the essential joints thus appears attractive. However, this has been reported only anecdotally in the medical literature. Monroe and Manoli (Citation1999) successfully corrected one case of malunion of the talar neck by osteotomy and corticocancellous bone grafting. Mahan and Lamy (Citation1992) treated one case of talar neck nonunion with considerable displacement 9 months after the injury with open reduction and internal fixation of the fracture. The anky-losed subtalar joint was fused with autogenous bone grafting, while the formerly incongruent ankle joints were preserved. None of these cases resulted in avascular necrosis of the talar body. In his textbook, Hansen (Citation2000) describes the technique of open-wedge osteotomy for posttraumatic varus malalignment of the talar neck, as well as clubfoot and other cavovarus foot deformities. However, no numbers or results were reported. We have preliminarily described 4 cases of anatomical reconstruction after malunited talar neck and body fractures of the present series (Zwipp et al. Citation1998). Few authors have reported successful treatment of talar nonunions with bone grafting, but without malalignment and the subsequent necessity of deformity correction (Migues et al. Citation1996, Asencio et al. Citation2000, Hansen Citation2000).
It can only be speculated that to date, the obvious risk of avascular necrosis of the talus and progressive arthrosis has prevented surgeons from attempting secondary reconstruction. Corrective osteotomy of the talus has been carried out for congenital deformities (Klaue Citation1997), and cases of postoperative AVN have been reported for these procedures (Huber et al. Citation2002). In our series of osteotomies after malunited fractures, the blood supply had been disturbed already by the original trauma in 3 cases, leading to partial AVN of the talar body (type III deformity) in these patients. In the other patients, the blood supply had apparently been preserved despite malunion or nonunion of the talus. When performing corrective osteotomy, the original fracture is recreated and no additional compromise of the blood supply should result. In our series, none of the 7 cases with type I and II deformities developed AVN and no progression of the preexisting avascular changes has been observed in the 3 cases of type III deformities. In any case, careful soft tissue dissection is mandatory. To expose the talar body, we performed osteotomy of the medial malleolus rather than extensive soft tissue dissection at the tip of the malleolus—in order to preserve the supply of blood via the “deltoid branch” (Mulfinger and Trueta Citation1970). In patients with impaired vascular supply to the foot because of poorly controlled diabetes or peripheral vascular disease, secondary anatomical reconstruction of the talus should rather not be attempted.
Several clinical studies on talar fractures have shown that neither arthrotic changes nor partial AVN reliably predict outcome after operative treatment (Lorentzen et al. Citation1977, Kundel et al. Citation1995, Rammelt et al. Citation2002, Vallier et al. Citation2003). Complete AVN with collapse of the talar dome carries a significantly worse prognosis. Consequently, we did not attempt secondary reconstruction in 10 patients with Type IV and V deformities (complete AVN or septic necrosis of the talus). In these cases, removal of all necrotic and infected bone combined with bone grafting or shortening and arthrodesis of the affected joints is the treatment of choice (Rzesacz et al. Citation1997, Liener et al. Citation1999, Rammelt et al. Citation2001). In our series, we observed no differences in the functional outcome between cases with and without preexisting partial AVN. We noted mild progression of arthrtic changes on the radiographs at follow-up in the ankle in 3 cases, and in the subtalar and talonavicular joints in 2 cases each. At a mean follow-up of 4 years, these changes did not adversely affect outcome. The average range of motion in the ankle and subtalar joints was within 10° of that on the unaffected side at the time of follow-up. 1 patient developed severe ankle arthritis 8 years after talar reconstruction, and went on to screw arthrodesis of the ankle while the subtalar and talonavicular joints were still intact. This patient was almost free of pain for more than 5 years. The development of posttraumatic arthrosis is determined by the severity of the initial cartilage damage by the trauma, the quality of joint reduction and time to secondary reconstruction in cases of severe joint incongruity. Symptomatic arthrosis has been reported after primary open reduction and internal fixation of talus fractures (Lorentzen et al. Citation1977, Peterson et al. Citation1977, Sneppen et al. Citation1977, Schuind et al. Citation1983, Kundel et al. Citation1995, Rammelt et al. Citation2002, Vallier et al. Citation2003). Thus, the mere possibility of the development of severe arthritis should not preclude the attempt at secondary anatomical reconstruction unless there is severe comminution of the joint surface. Late fusion is still an option in these cases, and leads to predictable results.
Immediately after the injury the fracture had been overlooked completely in 2 cases, it had been treated nonoperatively with closed reduction and casting in 5 cases, and operatively but without proper reduction in 3 cases. Interestingly, the patients who had not been treated with open reduction fared better at follow-up after secondary reconstruction, although these patients did not have a greater incidence of partial AVN or degenerative changes. The repeated surgery possibly represented an additional trauma to the soft tissues, resulting in inferior function at follow-up.
The state of the joint cartilage, the condition of soft tissue and the presence or absence of complete AVN—rather than the time elapsed after the accident—were crucial for the indication for secondary reconstruction as opposed to arthrodesis. Secondary reconstruction was carried out if the soft tissue envelope and the joint cartilage were still viable and had no major defects. Thus, the decision as to whether to reconstruct or fuse the affected joints was frequently made at the time of surgery, as has been explained extensively to the patients. In 16 cases of severe degenerative changes secondary to long-standing joint incongruity arthrodesis of the affected joints had to be performed. These patients were not included in this study.
Other important parameters for patient selection are the absence of any clinical, radiographic and laboratory signs of soft tissue or bone infection, the level of activity, and patient compliance. Anatomical reconstruction of talar malunions and nonunions appears to be beneficial in the young, active and compliant patient who is able to restrict weight bearing and willing to perform an extended protocol of physical therapy in order to prevent disuse osteopenia.
No competing interests declared.
- Asencio G, Rebai M, Bertin R, Megy B, Daude O. Pseud arthrosis et cals vicieux des fractures séparation du talus. Rev Chir Orthop Reparatrice Appar Mot 2000; 86: 173–80
- Bargon G, Henkemeyer H. Ergebnisse röntgenologischer und klinischer Langzeitbeobachtungen nach operativ versorgten Läsionen der tibiofibularen Syndesmose im oberen Sprunggelenk. RÖFO Fortschr Geb Röntgenstr Nuklearmed 1977; 126: 542–5
- Baumhauer J F, Alvarez R G. Controversies in treating talus fractures. Orthop Clin North Am 1995; 26: 335–51
- Biewener A, Rammelt S, Teistler F M, Grass R, Zwipp H. Funktionell ausgerichtete Nachbehandlung von Osteosynthesen des oberen Sprunggelenkes mit dem flexiblen Arthrodesenstiefel (Variostabil). Z Orthop Ihre Grenzgeb 2002; 140: 334–8
- Buechel F F, Sr., Buechel F F, Jr., Pappas M J. Ten-year evaluation of cementless Buechel-Pappas meniscal bearing total ankle replacement. Foot Ankle Int 2003; 24: 462–72
- Canale S T, Kelly F B, Jr. Fractures of the neck of the talus. J Bone Joint Surg (Am) 1978; 60: 143–56
- Chou L B, Mann R A, Yaszay B, Graves S C, McPeake W T, 3rd, Dreeben S M, Horton G A, Katcherian D A, Clanton T O, Miller R A, Van Manen J W. Tibiotalocalcaneal arthrodesis. Foot Ankle Int 2000; 21: 804–8
- Coester L M, Saltzman C L, Leupold J, Pontarelli W. Long-term results following ankle arthrodesis for post-traumatic arthritis. J Bone Joint Surg (Am) 2001; 83: 219–28
- Daniels T R, Smith J W, Ross T I. Varus malalignment of the talar neck. Its effect on the position of the foot and on subtalar motion. J Bone Joint Surg (Am) 1996; 78: 1559–67
- Easley M E, Trnka H J, Schon L C, Myerson M S. Isolated subtalar arthrodesis. J Bone Joint Surg (Am) 2000; 82: 613–24
- Frawley P A, Haert J A L, Young D A. Treatment outcome of major fractures of the talus. Foot Ankle Int 1995; 16: 339–345
- Fuchs S, Sandmann C, Skwara A, Chylarecki C. Quality of life 20 years after arthrodesis of the ankle. A study of adjacent joints. J Bone Joint Surg (Br) 2003; 85: 994–8
- Gagneux E, Gerard F, Garbuio P, Vichard P. Treatment of complex fractures of the ankle and their sequellae using transplantar intramedullary nailing. Acta Orthop Belg 1997; 63: 294–304
- Hansen S T. Functional reconstruction of the foot and ankle. Willliams & Wilkins, Philadelphia 2000; 127–9; 363–4
- Hawkins L G. Fractures of the neck of the talus. J Bone Joint Surg (Am) 1970; 52: 991–1002
- Hintermann B, Valderrabano V. Total ankle replacement. Foot Ankle Clin N Am 2003; 8: 375–405
- Huber H, Galantay R, Dutoit M. Avascular necrosis after osteotomy of the talar neck to correct residual club-foot deformity in children. A long-term review. J Bone Joint Surg (Br) 2002; 84: 426–30
- Kitaoka H B, Alexander I J, Adelaar R S, Nunley J A, Myerson M S, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int 1994; 15: 349–53
- Kitaoka H B, Patzer G L. Arthrodesis for the treatment of arthrosis of the ankle and osteonecrosis of the talus. J Bone Joint Surg (Am) 1998; 80: 370–9
- Klaue K. Planovalgus and cavovarus deformity of the hind foot. A functional approach to management. J Bone Joint Surg (Br) 1997; 79: 892–5
- Knecht S I, Estin M, Callaghan J J, Zimmerman M B, Alliman K J, Alvine F G, Saltzman C L. The Agility total ankle arthroplasty. Seven to sixteen-year follow-up. J Bone Joint Surg (Am) 2004; 86: 1161–71
- Kundel K, Braun W, Scherer A. Spätergebnisse nach zentralen Talusfrakturen. Unfallchirurg 1995; 98: 124–9
- Liener U C, Bauer G, Kinzl L, Suger G. Die tibiokalkaneare Arthrodese. Eine Analyse von 21 Fällen. Unfallchirurg 1999; 102: 848–54
- Lorentzen J E, Christensen S B, Krogsoe O, Sneppen O. Fractures of the neck of the talus. Acta Orthop Scand 1977; 48: 115–20
- Mahan K T, Lamy C. Surgical repair of a talar body nonunion. J Am Podiatr Med Assoc 1992; 82: 454–62
- Marti R. Talus und Calcaneusfrakturen. Die Frakturenbehandlung bei Kindern und Jugendlichen, B G Weber, C Brunner, F Freuler. Springer-Verlag, Berlin Heidelberg New York 1974; 376–87
- Migues A, Solari G, Carrasco N M, Gonzalez Della Valle A. Repair of talar neck nonunion with indirect corticocancellous graft technique: a case report and review of the literature. Foot Ankle Int 1996; 17: 690–4
- Monroe M T, Manoli A, 2nd. Osteotomy for malunion of a talar neck fracture: a case report. Foot Ankle Int 1999; 20: 192–5
- Mulfinger G L, Trueta J. The blood supply of the talus. J Bone Joint Surg (Br) 1970; 52: 160–7
- Peterson L, Goldie I F, Irstam L. Fracture of the neck of the talus. A clinical study. Acta Orthop Scand 1977; 48: 696–706
- Rammelt S, Grass R, Brenner P, Zwipp H. Septische Talusnekrose nach III°ig offener Talusfraktur im Rahmen eines komplexen Fußtraumas (“Floating talus”). Trauma Berufskr 2001; 3(Suppl 2)230–5
- Rammelt S, Gavlik J M, Winkler J, Zwipp H. Medium term results after central talus fractures. Proceedings of the 4th Congress of the European Foot and Ankle Society, SevilleSpain, March, 21–232002, 24
- Rockett M S, De Yoe B, Gentile S C, Zygmunt K. Nonunion of a Hawkin's group II talar neck fracture without avascular necrosis. J Foot Ankle Surg 1998; 37: 156–61
- Rzesacz E H, Culemann U, Illgner A, Reilmann H. Der homologe Talusersatz nach Talektomie bei Infekt und septischer Talusnekrose. Unfallchirurg 1997; 100: 497–501
- Sanders R, Fortin P, DiPasquale A, Walling D, Helfet D, Ross E. The results of operative treatment of displaced intraarticular calcaneal fractures using a CT scan classification. Major fractures of the pilon, the talus and the calcaneus, H Tscherne, J Schatzker. Springer-Verlag, Berlin Heidelberg New York 1992; 175–89
- Schuind F, Andrianne Y, Burny F, Donkerwolcke M, Saric O. Fractures et luxations de l'astragale. Revue de 359 cas. Acta Orthop Belg 1983; 49: 652–89
- Sneppen O, Christensen S B, Krogsoe O, Lorentzen J. Fracture of the body of the talus. Acta Orthop Scand 1977; 48: 317–24
- Spirt A A, Assal M, Hansen S T, Jr. Complications and failure after total ankle arthroplasty. J Bone Joint Surg (Am) 2004; 86: 1172–8
- Vallier H A, Nork S E, Benirschke S K, Sangeorzan B J. Surgical treatment of talar body fractures. J Bone Joint Surg (Am) 2003; 85: 1716–24
- Zwipp H, Rammelt S. Posttraumatische Korrekturoperationen am Fuß. Zentralbl Chir 2003; 128: 218–26
- Zwipp H, Gavlik J M, Rammelt S, Dahlen C. Rekonstruktion fehlverheilter Talusfrakturen. Posttraumatische Korrektureingriffe nach Fehlheilung an Becken und unterer Extremität, J Probst, H Zwipp. Hauptverband der gewerblichen Berufsgenossenschaften, Sankt Augustin 1998; 161–80
