Abstract
During the last decade, two new treatment modalities for osteoporotic vertebral fractures have gained more interest: percutaneous vertebroplasty and kyphoplasty. The techniques and the short-term clinical results and complications have been presented but there is no scientific evidence-based information regarding the efficacy of the procedures, such as randomized controlled trials (RCT). Instead, we have to rely on prospective and retrospective uncontrolled short-term observational studies and case-control studies. These studies have shown consistently that the short-term results after the procedures are favorable as regards both pain relief and functional status. It is currently unknown, however, whether a vertebroplasty or a kyphoplasty gives a better outcome than nonoperative treatment, and whether the long-term results are as favorable as the short-term results.
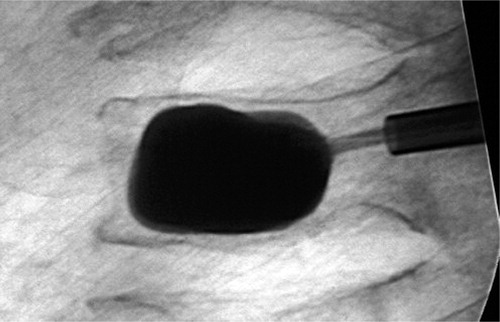
Even if no data can be found to document an increase in osteoporosis during the past 50 years, the number of fragility fractures increased exponentially during the second half of the last century (Obrant et al. Citation1989). The incidence of fractures related to osteoporosis is higher in women than in men, the incidence increases exponentially with age and the fractures occur at sites with a large proportion of trabecular bone (Bengner Citation1987, Obrant et al. Citation1989, Melton and Riggs Citation1995). One of the most devastating of these fractures is the vertebral fracture. The incidence varies in different ethnic settings, being higher in Scandinavian, American and Hong Kong Chinese females that in eastern European females, while the rates in Hong Kong Chinese males and American Caucasian males are lower than in European males (Melton et al. Citation1993, Lau et al. Citation1996, O'Neill et al. Citation1996). The female-to-male ratio is to 2:1 in Caucasians and the prevalence is age-dependent in both men and women (O'Neill et al. Citation1996). The incidence has been reported to increase from less than 20 per 100,000 person-years in men and women under 45 years of age, to 1,200 per 100,000 person-years in men and women aged 85 years and over (O'Neill et al. Citation1996). There has also been a temporal trend described, with an increased incidence of vertebral fractures in Sweden from 1950 to 1983 (Bengner et al. Citation1988). Fracture is also known to be followed by an increased morbidity and mortality, both in men and women (Hasserius Citation2003), and many patients with a vertebral fracture experience a reduction in quality of life, predominantly including back pain, functional limitations, depression, disability and loss of height (Ettinger et al. Citation1988, Citation1992). In the light of all the negative effects on the health of individual patients, and also due to the cost to society, vertebroplasty (VP; ) and kyphoplasty (KP; ) have attracted great interest.
Figure 1. A vertebroplasty performed in the fourth lumbar vertebra of a 67-year-old woman with an osteoporotic fracture.
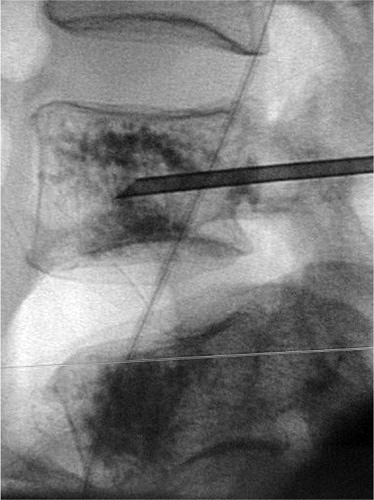
Figure 2. A kyphoplasty performed in the third lumbar vertebra of a 69-year-old man with an osteoporotic fracture.
VP was originally developed by Deramond and Galibert, a French radiologist and a French neurosurgeon, and in 1987 it was presented in the literature as a technique to percutaneously stabilize vertebral bodies affected by a hemangioma (Galibert et al. Citation1987). At the end of the same decade, another French group reported that the technique could also be used to stabilize fractured vertebral bodies (Lapras et al. Citation1989). The method gained further popularity in the United States during the 1990s, mainly for the treatment of osteoporotic fractures. At the end of the millennium, the method was also established in most western European countries (Barr et al. Citation2000, McGraw et al. Citation2002, Diamond et al. Citation2003, Evans et al. Citation2003, Mehbod et al. Citation2003). The VP method was further developed by the introduction of the percutaneous balloon KP technique (Lieberman et al. Citation2001). The aim of the method is not only to stabilize the vertebral body, but also to restore the normal anatomy of the fractured vertebra and to reduce the kyphosis in the injured region. By inflating a balloon in the fractured vertebral body, the KP method is intended to restore the original shape of the compressed vertebral body before the cement fixation (Lieberman et al. Citation2001, Coumans et al. Citation2003, Ledlie and Renfro Citation2003, Phillips et al. Citation2003, Rao and Singrakhia Citation2003, Weisskopf et al. Citation2003, Crandall et al. Citation2004, Donovan et al. Citation2004, Heini and Orler Citation2004, Hillmeier et al. Citation2004, Masala et al. Citation2004). As the shortterm results with both techniques were promising, the methods rapidly attracted attention worldwide.
The aim of this review is mainly to evaluate the clinical outcome after a VP or a KP, based on papers with the highest level of evidence. A Medline (PubMed) literature search in October 2004 allowed us to identify 388 articles on “vertebroplasty”, of which 340 had been published since 2000. A corresponding search for “kyphoplasty” revealed 92 publications, half of them review articles, all of which had been published since 2001. We used no other search motors. We scrutinized all papers, irrespective of when they were published, provided there was an abstract in English. The inclusion criterion was an evidence-based approach. From the relevant papers found, a continued search was undertaken by choosing the connection “related manuscripts” in the PubMed database, and in the reference lists of the accepted papers. This approach was repeated until no more relevant papers were found. By this method, we found no randomized controlled trials (RCT) and only a few articles presenting a controlled observational study; the rest consisted of retrospective or prospective cross-sectional case reports, case-control studies or uncontrolled observational studies. When a variety of papers were found with the same degree of evidence, we elected to present the first paper published and the paper with the largest sample size and the longest follow-up. Thus, this review cannot be regarded as a systematic review—such as a Cochrane review or a meta-analysis.
Operating technique
The VP or KP procedures are recommended to be performed in a hospital setting (either in an inter-ventional radiology room or operating theater) and under sterile conditions. Both methods can be performed with the patient under local or general anesthesia, but there must be the possibility of converting the operation to an open emergency operation in cases of severe bone-cement leak, affecting the spinal canal (Lee et al. Citation2002, Phillips et al. Citation2002, Shapiro et al. Citation2003, Yeom et al. Citation2003, Lin et al. Citation2004). Furthermore, high-quality fluoros-copy, or CT, must be available to guide the surgeon during the operation (McGraw et al. Citation2003). In most centers, prophylactic antibiotics are used. Trocar-cannula systems, of various designs, have in common that they use a large-bore (2.3–2.6 mm) removable central trocar—usually with a sharp tip and a fixed handle matching the cannula. Insertion of the device is usually done transpedicularly in the lumbar and lower thoracic region, while an extrapedicular route lateral to the pedicula, aiming at the central part of the vertebral body, is usually recommended in the higher thoracic region. The entry point is 9 o'clock on the left-hand side and 3 o'clock on the right-hand side, in relation to the pedicel. The introduction of the cannula should be done with slow rotatory hand pressure (some physicians use a mallet), and both the cannulae should be inserted before the cement is injected from both sides simultaneously (Lapras et al. Citation1989, Weisskopf et al. Citation2003, Grohs and Krepler Citation2004, Heini and Orler Citation2004, Hillmeier et al. Citation2004, Masala et al. Citation2004). It is regarded as favorable to insert one cannula into each pedicle, to reduce the pressure in the vertebral body during the injection of bone cement, thus reducing the risk of cardiopulmonary complications (Aebli et al. Citation2003).
At present, the cement generally used for VP or KP is based on polymethylmetacrylate (PMMA) (Lapras et al. Citation1989, Lee et al. Citation2002, Shapiro et al. Citation2003, Yoo et al. Citation2004). Mixing of the cement should be done in a vacuum chamber. We prefer cement with low viscosity, for example Simplex P (Stryker-Howmedica-Osteonics, Rutherford, NJ, USA), together with a contrast medium, at least 10% barium sulfate. Other centres use other types of bone cement, however, and today there exists approved polymethylmethacrylate with up to 30% barium sulfate (Jasper et al. Citation2002). In VP, the cement injection is done by 1–2 mL syringes with a Luer-lock mechanism, and the cement should start to thicken when injected. The gradual injection should be followed by lateral fluoroscopic surveillance, to ensure early detection of cement leaking into the epidural space, vena cava, vena azygos or disc space combined with anterior surveillance to observe any lateral leakage (McGraw et al. Citation2003). 4 mL has been shown experimentally to restore strength to both thoracic and lumbar vertebrae, but to restore stiffness, 4 mL is required in the thoracic region and 6–8 mL in the lumbar region (Belkoff et al. Citation2001, Liebschner et al. Citation2001, Molloy et al. Citation2003). The common recommendation is to use 2–3 mL of cement in the thoracic spine and 3–5 mL of cement in the lumbar spine (Barr et al. Citation2000); when this amount has been injected, the cannulae should be removed immediately. Note that both cannulae should be inserted when injecting the cement, to avoid the first channel being passively filled with cement from the posterior route if the second cannula is injected on a later occasion. Often, the procedure must be supplemented with gentle pressure for some minutes to reduce the risk of hematoma formation due to venous bleeding from the bone cannulae.
The KP technique is similar to that of VP (Lieberman et al. Citation2001, Ledlie and Renfro Citation2003, Rao and Singrakhia Citation2003, Weisskopf et al. Citation2003, Crandall et al. Citation2004, Heini and Orler Citation2004, Masala et al. Citation2004). The insertion routes are the same, with insertion of cannulae from lateral to medial direction under fluoroscopic surveillance. When the tips of the cannulae have passed the plane of the posterior wall of the vertebral body, a drill is introduced to make a channel in the vertebral body, into which the deflated balloon can be inserted. The trocar is then removed and the empty balloon introduced. After checking the positioning by anterior and lateral fluoroscopy, the balloons are inflated with radio-opaque contrast medium by a specifically designed syringe with continuous control of pressure and volume. Once the voids in the vertebral body have been created, in many cases with a partial or complete restoration of the vertebral body height, the balloons are retracted and bone cement is injected using a blunt cannula under low pressure, with visualization by fluoroscopy in two planes. The possibility of injecting the cement under low pressure after having created a cave with the balloon, together with the restoration of vertebral body height, is an obvious theoretical advantage of the KP technique over the VP technique (Tomita et al. Citation2004). There have also been experimental trials that infer that a low injection pressure minimizes the extravasation of the cement (Baroud et al. Citation2003). As soon as the cement has hardened, mobilization can start. In Europe, most patients stay in hospital overnight, but at many centers in the USA, these procedures are performed as day surgery under local anesthesia. Virtually all patients also receive antiresorptive osteoporosis medication after the operation.
Results
We found no prospective randomized or non-randomized controlled clinical trials to help us evaluate the efficacy of the methods. We have had to rely mainly on observational uncontrolled studies and case series. An overwhelming impression from the results is that the patients are almost immediately relieved of back pain, whether after VP or KP (Barr et al. Citation2000, Lieberman et al. Citation2001, McGraw et al. Citation2002, Coumans et al. Citation2003, Diamond et al. Citation2003, Evans et al. Citation2003, Ledlie and Renfro Citation2003, McGraw et al. Citation2003, Mehbod et al. Citation2003, Phillips et al. Citation2003, Rao and Singrakhia Citation2003, Weisskopf et al. Citation2003, Crandall et al. Citation2004, Donovan et al. Citation2004, Grohs and Krepler Citation2004, Heini and Orler Citation2004, Hillmeier et al. Citation2004, Masala et al. Citation2004). Most of these reports have shown a short-term success rate of relieving pain of 75–90%. This conclusion is mostly based on comparison with the preoperative situation, and without comparing with controls. Furthermore, numerous methods have been used to evaluate pain relief.
Vertebroplasty
The largest VP study presented included 488 consecutive patients, where half of the treated patients were interviewed retrospectively by telephone at a mean of 7 months after the procedure (Evans et al. Citation2003). The mean pain relief, estimated by a visual analogue scale (VAS), was reduced from 8.9 preoperatively to 3.4 postoperatively and the walking ability improved in 108 of the 245 patients evaluated. These good results were reported in all age groups and regardless of the number of vertebral fractures treated. The limitations of this study are the retrospective design and the absence of controls. A similar outcome was also reported in 100 patients with osteoporotic compression fractures who were treated with VP and followed prospectively for an average of 21 months (McGraw et al. Citation2002). In this survey, 97 of the patients reported substantial pain reduction, assessed by VAS, with the pain level dropping from 8.9 to 2.0. In another study, it had been possible for the authors to use a control group for comparison (Diamond et al. Citation2003). This is surely one of the very few studies published, if not the only one, in which such an attempt was made. Just 24 h after the procedure, there was a highly significant relief of symptoms in the VP group, whereas there were no longer any differences between the groups after 6–12 months. The result was generally the same when physical function was considered instead. One limitation of this study is the procedure for selection of the controls—comprising individuals who declined percutaneous VP. Although this selection procedure leaves many questions unanswered, the study was nevertheless the first attempt to compare patients who had been operated with patients who had not.
Kyphoplasty
Lieberman et al. (Citation2001) were among the first authors to report outcome after a KP. They followed 30 patients who had been treated for 70 vertebral osteoporotic compression fractures. The KP procedure resulted in some degree of height restoration in about two-thirds of the patients, and a significant improvement in bodily pain and physical function as assessed by the SF-36 scales. Philips et al. (Citation2003) showed that the KP technique improved the wedge-shaped compressed vertebrae by a mean of 9 degrees and Barr et al. (Citation2000) showed that manipulation on the procedural table could affect height restoration. However, in cited studies, roughly one-third of the treated vertebrae showed no anatomical restoration after a KP (Barr et al. Citation2000, Lieberman et al. Citation2001, Phillips et al. Citation2003). Somewhat surprisingly, in neither of these articles does there seem to have been any clear correlation between the age of the fracture and the restoration of height. Another study presented similar results when reporting that the average increase in vertebral body height was 2.5 mm anteriorly, 2.7 mm centrally, and 1.4 mm posteriorly (evaluated by MRI and CT scans), but that 13 of 85 treated vertebrae remained unchanged (Hiwatashi et al. Citation2003). Furthermore, in this study there was no obvious correlation between restoration of height and clinical success. These reports are important, as the literature often infer that a restoration of height is one of the major advantages of the KP procedure. However, it is unclear whether the patients with a height restoration of 2–3 mm have a better long-term outcome than those who do not.
Furthermore, to our knowledge there has only been one study of the KP procedure where the treated patients have been compared with controls treated nonoperatively (Weisskopf et al. Citation2003). This was a small study in which a retrospectively evaluated control group of 20 patients was compared with 18 operated patients. In line with almost all published studies, the operated patients experienced immediate pain relief and functional improvement in this report also compared to the controls. Interestingly, the duration of hospital stay was considerably longer in the nonoperatively treated group.
Adverse side effects
Adverse side effects have been described after both VP and KP (Lieberman et al. Citation2001, Lin et al. Citation2004). Cement leakage has been observed, and there have also been reports of pulmonary edema, myocardial infarction and rib fractures (Padovani et al. Citation1999, Lieberman et al. Citation2001, Jang et al. Citation2002, Aebli et al. Citation2003, Childers Citation2003, Koessler et al. Citation2003, Phillips et al. Citation2003, Rauschmann et al. Citation2004, Yoo et al. Citation2004). There have also been procedure-specific complications for VP and KP, described as cement leakage to the epidural space, disc, vena cava, vena azygos and even cement embolism to the lungs (Padovani et al. Citation1999, Jang et al. Citation2002, Lee et al. Citation2002). So far, to our knowledge, only one case of epidural leakage of cement (resulting in paraparesis) has been reported (Lee et al. Citation2002), and only one case complicated by spondylitis (Yu et al. Citation2004).
There have also been some observations indicating that KP is safer than VP regarding the risk of cement leakage (Phillips et al. Citation2002), while most studies could not support this notion in a convincing way. Also, after KP there seems to be a cement leakage in 10% of cases (Lieberman et al. Citation2001, Phillips et al. Citation2003), or even more (Weisskopf et al. Citation2003), and as we still lack comparative studies between the two techniques, the theoretical advantage of KP over VP has been difficult to verify or reject. However, it is evident that the KP procedure can also result in serious adverse events, including cement extravasation into segmental veins (Weisskopf et al. Citation2003), perioperative pulmonary oedema with myocardial infarction (Lieberman et al. Citation2001, Phillips et al. Citation2003) and rib fractures (Lieberman et al. Citation2001).
There is also lack of knowledge about the long-term results of VP and KP, even if there have been small uncontrolled studies (n = 16) with up to an average of 3 years of follow-up of VP (Legroux-Gerot et al. Citation2004) presenting a small pain reduction compared to the preoperative status. Other studies have reported an additional risk of the procedures in themselves producing altered mechanical forces that induce new vertebral fractures, particularly when adjacent to already operated vertebrae (Baroud et al. Citation2003, Uppin et al. Citation2003, Donovan et al. Citation2004, Kim et al. Citation2004, Wilcox Citation2004). However, today, there has been no study directly comparing the incidence of new vertebral fractures in patients treated with a VP or a KP with the corresponding incidence after nonoperative treatment. The problem of an increased incidence of new verte-bral fractures after a VP or KP treatement has been stressed in a paper by Uppin et al. (Citation2003), where 12% of the patients followed up after two years had new vertebral fractures—mostly in vertebrae adjacent to a previously operated vertebra. It is probable, however, that the complication rate is much higher than this, since in this study notice was only taken of symptomatic vertebral fractures and follow-up was restricted to only 16% of 177 operated patients who returned for a follow-up. The increased risk of sustaining new vertebral fractures in patients treated with a kyphoplasty has been supported by two recent trials in which 10 of 38 operated patients had new vertebral fractures within 8 months of the operation (Fribourg et al. Citation2004), and 23% of 115 operated patients had new vertebral fractures within 11 months of the operation (Harrop et al. Citation2004). This can be compared with a 19% incidence of new vertebral fractures in untreated patients with a vertebral fracture at baseline and followed for 12 months (Lindsay et al. Citation2001). Furthermore, as we know that treatment with bisphosfonates reduces the incidence of new vertebral fractures by close to 50% (Black et al. Citation1996), we can hypothetically estimate the annual incidence in individuals with a vertebral fracture followed by bisphosfonate treatment to be 10%. This incidence should be compared with the incidence in patients treated with a VP or a KP, as they always achieve antiresorptive treatment in addition to the surgery. This theoretical calculation suggests that VP and KP are possibly followed by an increased incidence of new spinal fractures. In addition, most new fractures have been found to be located adjacent to the previously cemented vertebrae (Fribourg et al. Citation2004, Harrop et al. Citation2004), supporting the view that altered mechanical forces may lead to new spinal fractures.
Future perspectives
There is currently an intense degree of research activity, with different workers trying to support or refute the hypothesis of a superior result with VP and KP compared to nonoperative treatment. Although these techniques have gained enormous popularity, little is known about their effectiveness. Since most patients with an osteoporotic vertebral fracture improve even if not treated, the inclusion of an adequate control group is essential for the assessment of any therapeutic intervention. Thus, there are currently several RCTs being carried out, to evaluate the effects of VP or KP compared to standard pharmacological treatment given to a control group. One important problem is that the procedures have already gained popularity, even though they have not been supported by an adequate amount of research data. Because patients demanded VP or KP, a similar study in the USA had to be terminated in advance. Today, Europe and Japan appear to be the only regions in which scientific studies of this kind can be performed, due to the organization of health care and still limited use of the techniques. There is also research in progress in order to find substitutes for conventional bone cement (Jasper et al. Citation2002, Hillmeier et al. Citation2004, Matsuyama et al. Citation2004, Provenzano et al. Citation2004, Tomita et al. Citation2004). Cortoss, a new synthetic cement with a lower exothermic reaction during polymerization, is provided with a double lumen cartridge with specially designed tips for mixing (Szpalski et al. Citation2003). There are other lines of development: ceramic material and combinations of calcium phosphate and hydroxyapatite.The new material quickly attain the same strength as bone, but still they are most used in research studies.
No competing interests declared.
- Aebli N, Krebs J, Schwenke D, Davis G, Theis J C. Cardiovascular changes during multiple vertebroplasty with and without vent-hole: an experimental study in sheep. Spine 2003; 28: 1504–11, discussion 1511-2
- Baroud G, Heini P, Nemes J, Bohner M, Ferguson S, Steffen T. Biomechanical explanation of adjacent fractures following vertebroplasty. Radiology 2003; 229: 606–7, author reply 607-8
- Barr J D, Barr M S, Lemley T J, McCann R M. Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine 2000; 25: 923–8
- Belkoff S M, Mathis J M, Jasper L E, Deramond H. The biomechanics of vertebroplasty. The effect of cement volume on mechanical behavior. Spine 2001; 26: 1537–41
- Bengner U. Epidemiological changes over 30 years in an urban population. Thesis. Lund University, LundSweden 1987
- Bengner U, Johnell O, Redlund-Johnell I. Changes in incidence and prevalence of vertebral fractures during 30 years. Calcif Tissue Int 1988; 42: 293–6
- Black D M, Cummings S R, Karpf D B, Caule J A, Thomson D E, Nevitt M C, Bauer D C, Genant H K, Haskell W L, Marcus R, Ott S M, Torner J C, Quandt S A, Reiss T F, Ensrud K E. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet 1996; 348: 1535–41
- Childers J C, Jr. Cardiovascular collapse death during vertebroplasty. Radiology 2003; 228: 902, author reply 902-3
- Coumans J V, Reinhardt M K, Lieberman I H. Kyphoplasty for vertebral compression fractures: 1-year clinical outcomes from a prospective study. J Neurosurg Spine 2003; 99: 44–50
- Crandall D, Slaughter D, Hankins P J, Moore C, Jerman J. Acute versus chronic vertebral compression fractures treated with kyphoplasty: early results. Spine J 2004; 4: 418–24
- Diamond T H, Champion B, Clark W A. Management of acute osteoporotic vertebral fractures: a nonrandomized trial comparing percutaneous vertebroplasty with conservative therapy. Am J Med 2003; 114: 257–65
- Donovan M A, Khandji A G, Siris E. Multiple adjacent vertebral fractures after kyphoplasty in a patient with steroid-induced osteoporosis. J Bone Miner Res 2004; 19: 712–3, Epub 2004 Feb 9
- Ettinger B, Block J E, Smith R, Cummings S R, Harris S T, Genant H K. An examination of the association between vertebral deformities, physical disabilities and psychosocial problems. Maturitas 1988; 10: 283–96
- Ettinger B, Black D M, Nevitt M C, Rundle A C, Cauley J A, Cummings S R, Genant H K. Contribution of vertebral deformities to chronic back pain and disability. The Study of Osteoporotic Fractures Research Group. J Bone Miner Res 1992; 7: 449–56
- Evans A J, Jensen M E, Kip K E, DeNardo A J, Lawler G J, Negin G A, Remley K B, Boutin S M, Dunnagan S A. Vertebral compression fractures: pain reduction and improvement in functional mobility after percutaneous polymethylmethacrylate vertebroplasty retrospective report of 245 cases. Radiology 2003; 226: 366–72
- Fribourg D, Tang C, Sra P, Delamarter R, Bae H. Incidence of Subsequent Vertebral Fracture after Kyphoplasty. Spine 2004; 29: 2270–6
- Galibert P, Deramond H, Rosat P, Le Gars D. Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie 1987; 33: 166–8
- Grohs J G, Krepler P. Minimal invasive stabilization of osteoporotic vertebral compression fractures. Methods and preinterventional diagnostics. Radiologe 2004; 44: 254–9
- Harrop J S, Prpa B, Reinhardt M K, Lieberman I. Primary and secondary osteoporosis' incidence of subsequent vertebral compression fractures after kyphoplasty. Spine 2004; 29: 2120–5
- Hasserius R. Vertebral deformity and vertebral fracture in the elderly. Thesis. Lund University, LundSweden 2003
- Heini P F, Orler R. Kyphoplasty for treatment of osteoporotic vertebral fractures. Eur Spine J 2004; 13: 184–92, Epub 2004 Feb 25
- Hillmeier J, Meeder P J, Noldge G, Kock H J, Da Fonseca K, Kasperk H C. Balloon kyphoplasty of vertebral compression fractures with a new calcium phosphate cement. Orthopade 2004; 33: 31–9
- Hiwatashi A, Moritani T, Numaguchi Y, Westesson P L. Increase in vertebral body height after vertebroplasty. AJNR Am J Neuroradiol 2003; 24: 185–9
- Jang J S, Lee S H, Jung S K. Pulmonary embolism of polymethylmethacrylate after percutaneous vertebroplasty: a report of three cases. Spine 2002; 27: E416–8
- Jasper L E, Deramond H, Mathis J M, Belkoff S M. Material properties of various cements for use with vertebroplasty. J Mater Sci Mater Med 2002; 13: 1–5
- Kim S H, Kang H S, Choi J A, Ahn J M. Risk factors of new compression fractures in adjacent vertebrae after percutaneous vertebroplasty. Acta Radiol 2004; 45: 440–5
- Koessler M J, Aebli N, Pitto R P. Fat and bone marrow embolism during percutaneous vertebroplasty. Anesth Analg 2003; 97: 293, author reply 294
- Lapras C, Mottolese C, Deruty R, Lapras C, Jr, Remond J, Duquesnel J. Percutaneous injection of methyl-metacrylate in osteoporosis and severe vertebral osteolysis (Galibert's technic). Ann Chir 1989; 43: 371–6
- Lau E M, Chan H H, Woo J, Lin F, Black D, Nevitt M, Leung P C. Normal ranges for vertebral height ratios and prevalence of vertebral fracture in Hong Kong Chinese: a comparison with American Caucasians. J Bone Miner Res 1996; 11: 1364–8
- Ledlie J T, Renfro M. Balloon kyphoplasty: one-year outcomes in vertebral body height restoration, chronic pain, and activity levels. J Neurosurg Spine 2003; 98: 36–42
- Lee B J, Lee S R, Yoo T Y. Paraplegia as a complication of percutaneous vertebroplasty with polymethylmethacrylate: a case report. Spine 2002; 27: E419–22
- Legroux-Gerot I, Lormeau C, Boutry N, Cotten A, Duquesnoy B, Cortet B. Long-term follow-up of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Clin Rheumatol 2004; 23: 310–7, Epub 2004 May 18
- Lieberman I H, Dudeney S, Reinhardt M K, Bell G. Initial outcome and efficacy of “kyphoplasty” in the treatment of painful osteoporotic vertebral compression fractures. Spine 2001; 26: 1631–8
- Liebschner M A, Rosenberg W S, Keaveny T M. Effects of bone cement volume and distribution on vertebral stiffness after vertebroplasty. Spine 2001; 26: 1547–54
- Lin E P, Ekholm S, Hiwatashi A, Westesson P L. Vertebroplasty: cement leakage into the disc increases the risk of new fracture of adjacent vertebral body. AJNR Am J Neuroradiol 2004; 25: 175–80
- Lindsay R, Silverman S L, Cooper C, Hanley D A, Barton I, Broy S B, Licata A, Benhamou L, Geusens P, Flowers K, Stracke H, Seeman E. Risk of new vertebral fracture in the year following a fracture. Jama 2001; 285: 320–3
- Masala S, Cesaroni A, Sergiacomi G, Fiori R, Massari F, Manenti G, Nardi P, Simonetti G. Percutaneous kyphoplasty: new treatment for painful vertebral body fractures. Vivo 2004; 18: 149–53
- Matsuyama Y, Goto M, Yoshihara H, Tsuji T, Sakai Y, Nakamura H, Sato K, Kamiya M, Ishiguro N. Vertebral reconstruction with biodegradable calcium phosphate cement in the treatment of osteoporotic vertebral compression fracture using instrumentation. J Spinal Disord Tech 2004; 17: 291–6
- McGraw J K, Lippert J A, Minkus K D, Rami P M, Davis T M, Budzik R F. Prospective evaluation of pain relief in 100 patients undergoing percutaneous vertebroplasty: results and follow-up. J Vasc Interv Radiol 2002; 13: 883–6
- McGraw J K, Cardella J, Barr J D, Mathis J M, Sanchez O, Schwartzberg M S, Swan T L, Sacks D. Society of interventional radiology quality improvement guidelines for percutaneous vertebroplasty. J Vasc Interv Radiol 2003; 14: S311–5
- Mehbod A, Aunoble S, Le Huec J C. Vertebroplasty for osteoporotic spine fracture: prevention and treatment. Eur Spine J 2003; 12: S155–62, Epub 2003 Sep 19
- Melton L J, 3rd, Lane A W, Cooper C, Eastell R, O'Fallon W M, Riggs B L. Prevalence and incidence of vertebral deformities. Osteoporos Int 1993; 3: 113–9
- Melton L J, 3rd, Riggs B L. Osteoporosis: Etiology diagnosis management. Raven Press, New York 1995; 225–48
- Molloy S, Mathis J M, Belkoff S M. The effect of vertebral body percentage fill on mechanical behavior during percutaneous vertebroplasty. Spine 2003; 28: 1549–54
- Obrant K J, Bengner U, Johnell O, Nilsson B E, Sernbo I. Increasing age-adjusted risk of fragility fractures: a sign of increasing osteoporosis in successive generations?. Calcif Tissue Int 1989; 44: 157–67
- O'Neill T W, Felsenberg D, Varlow J, Cooper C, Kanis J A, Silman A J. The prevalence of vertebral deformity in european men and women: the European Vertebral Osteoporosis Study. J Bone Miner Res 1996; 11: 1010–8
- Padovani B, Kasriel O, Brunner P, Peretti-Viton P. Pulmonary embolism caused by acrylic cement: a rare complication of percutaneous vertebroplasty. AJNR Am J Neuroradiol 1999; 20: 375–7
- Phillips F M, Todd Wetzel F, Lieberman I, Campbell-Hupp M. An in vivo comparison of the potential for extravertebral cement leak after vertebroplasty and kyphoplasty. Spine 2002; 27: 2173–8;, discussion 2178-9
- Phillips F M, Ho E, Campbell-Hupp M, McNally T, Todd Wetzel F, Gupta P. Early radiographic and clinical results of balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures. Spine 2003; 28: 2260–5;, discussion 2265-7
- Provenzano M J, Murphy K P, Riley L H. 3rd. Bone cements: review of their physiochemical biochemical properties in percutaneous vertebroplasty. AJNR Am J Neuroradiol 2004; 25: 1286–90
- Rao R D, Singrakhia M D. Painful osteoporotic vertebral fracture. Pathogenesis, evaluation, and roles of vertebroplasty and kyphoplasty in its management. J Bone Joint Surg (Am) 2003; 85-A: 2010–22
- Rauschmann M A, von Stechow D, Thomann K D, Scale D. Complications of vertebroplasty. Orthopade 2004; 33: 40–7
- Shapiro S, Abel T, Purvines S. Surgical removal of epidural and intradural polymethylmethacrylate extravasation complicating percutaneous vertebroplasty for an osteoporotic lumbar compression fracture. Case report. J Neurosurg Spine 2003; 98: 90–2
- Szpalski M, Gunzburg R, Deramond H. Percutaneous injection of Cortoss synthetic bone filler in the repair of fractures in the vertebral body. Vertebral osteoporotic compression fractures, M Szpalski, R Gunzburg. Lippincott Williams and Wilkins. 2003; 171–7
- Tomita S, Molloy S, Jasper L E, Abe M, Belkoff S M. Biomechanical comparison of kyphoplasty with different bone cements. Spine 2004; 29: 1203–7
- Uppin A A, Hirsch J A, Centenera L V, Pfiefer B A, Pazianos A G, Choi I S. Occurrence of new vertebral body fracture after percutaneous vertebroplasty in patients with osteoporosis. Radiology 2003; 226: 119–24
- Weisskopf M, Herlein S, Birnbaum K, Siebert C, Stanzel S, Wirtz D C. Kyphoplasty - a new minimally invasive treatment for repositioning and stabilising vertebral bodies. Z Orthop Ihre Grenzgeb 2003; 141: 406–11
- Wilcox R K. The biomechanics of vertebroplasty: a review. Proc Inst Mech Eng [H] 2004; 218: 1–10
- Yeom J S, Kim W J, Choy W S, Lee C K, Chang B S, Kang J W. Leakage of cement in percutaneous transpedicular vertebroplasty for painful osteoporotic compression fractures. J Bone Joint Surg (Br) 2003; 85: 83–9
- Yoo K Y, Jeong S W, Yoon W, Lee J. Acute respiratory distress syndrome associated with pulmonary cement embolism following percutaneous vertebroplasty with polymethylmethacrylate. Spine 2004; 29: E294–7
- Yu S W, Chen W J, Lin W C, Chen Y J, Tu Y K. Serious pyogenic spondylitis following vertebroplasty. A case report. Spine 2004; 29: E209–11