Abstract
Background Aseptic loosening of elbow replacements, seen in long-term follow-up, remains a problem. In this study, we attempted to determine the influence of cementing technique, prosthetic position, different component sizes, use of a bone plug, and intraoperative fractures on the development and progression of radiolucent lines and aseptic loosening.
Methods We studied standard radiographs of 125 primary Souter-Strathclyde total elbow prostheses using the Wrightington method. Additionally, 104 preoperative radiographs were available for analysis. We used a Markow statistical model to detect relationships between all factors described above.
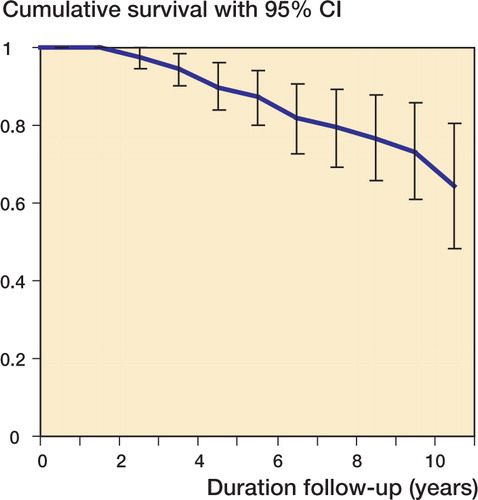
Results After a mean follow-up time of 5.5 (2–19) years, 21 (17%) prostheses had loosened radiographically (10-year survival: 65%). When the humeral component was tilted more medially or more anteriorly, we found development of radiolucent lines at the medial condyle and at the posterior side of the humeral component. However, the progression of these lines was not influenced by these positions. No other prognostic factors for radiolucent lines or aseptic loosening were found.
Interpretation Despite the small number of elbows studied, the weak influence of prosthetic position on aseptic loosening gives more ground for a multifactorial cause for aseptic loosening of the Souter-Strathclyde total elbow prosthesis.
Total elbow replacement is a well-established treatment for the destroyed elbows (Trancik et al. Citation1987, Ferlec Citation1999, Gschwend et al. Citation1999, Rozing Citation2000, Mackay et al. Citation2001, Tanaka et al. Citation2001). The most important factor determining poor survival rates of elbow replacements is aseptic loosening of the humeral component (Kudo and Iwano Citation1990, Hargreaves and Emery Citation1999, Valstar et al. Citation2002, Van der Lugt et al. Citation2004). In this series of 125 Souter-Strathclyde total elbow prostheses, we tried to determine different factors that affect aseptic loosening. Trail et al. (Citation1999) used the Wrightington method for determination of prosthetic position and found that anterior tilting of the humeral component was associated with aseptic loosening. We used this method in our series.
The recent tendency to use larger components of the Souter-Strathclyde prosthesis for primary surgery has improved survival rates, but no scientific basis for this phenomenon has been put forward (Ikävalko et al. Citation2002). In this study, we related the different humeral component sizes of the Souter-Strathclyde to the size of the patient’s humeral bone. In contrast to knee and hip arthroplasties, the use of bone plugs have so far not been proven to be of value in elbow replacements; thus, we analyzed this factor also (Kligman and Roffman Citation2000, Kumar et al. Citation2000, Klapach et al. Citation2001). In addition, we analyzed intraoperative fractures that may jeopardize the survival of prostheses (Trancik et al. Citation1987, Rozing Citation2000). Finally, we tried to determine the association between the amount of bone resorption or dislocation preoperatively, as estimated by radiography, and aseptic loosening by using a new method. All data were analyzed using a Markov model.
Patients and methods
We studied the standard radiographs of 125 primary Souter-Strathclyde total elbow prostheses retrospectively (Stryker Howmedica Osteonics, Limerick, Ireland). All had been inserted at our center. 15 patients had a bilateral replacement. There were 83 women and 27 men, and the average age at operation was 60 (25–79) years. All radiographs were taken while the patient sat on a chair, resting the upper extremity on a table and the radiographs were made for the anteroposterior and lateral direction. For the anteroposterior direction, the shoulder is antefiexed and the elbow should be extended as much as possible. For the lateral view, the elbow should be flexed 90 degrees whereas the shoulder is rotated internally. In this way, the flexed elbow rests on the table in a horizontal position. All patients were followed for at least 2 years. The mean radiographic follow-up time was 5.5 (2–19) years.
The preoperative diagnosis was seropositive rheumatoid arthritis in 94 patients (108 elbows), seronegative rheumatoid arthritis in 9 patients (9 elbows), juvenile chronic arthritis in 2 patients (3 elbows), psoriatic arthritis in 1 patient (1 elbow), synovial chondromatosis in 1 patient (1 elbow), and posttraumatic osteoarthrosis in 3 patients (3 elbows). The Larsen classification for the 120 elbows affected by rheumatoid arthritis was as follows: class III for 10 elbows, class IV for 62 elbows, and class V for 48 elbows (Larsen et al. Citation1977).
The size of the components was determined before the operation by templating on radiographs. The sizes of the humeral components were small for 48 elbows, medium for 64 elbows, and large for 13 elbows, and the ulnar components were either small (66 elbows), medium (54 elbows), or metal-backed (5 elbows, with the snapfit option in 4 elbows). The latter component was used because of insufficient ulnar bone stock. In case of an additional tendency for dislocation after the trial reduction during the operation, we used the snapfit insert.
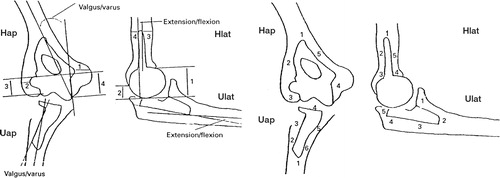
We used the Wrightington method for assessment of all radiographs () (Trail et al. Citation1999). This method consists of 12 position measurements and 21 radiolucent line measurements. All measurements were done by the first author (who was not the operating surgeon) by using a universal goniometer. To assess the position of the prosthesis, we used only the first postoperative radiograph. All elbow prostheses were successively included in the analysis, but the elbow was excluded from the study only if the first postoperative radiograph had been made more than 6 months after the operation (18 elbows), or when aseptic loosening was not the reason for failure (22 elbows). Radiolucent lines are demarcation lines between the cement-bone interfaces seen on a standard radiograph and they were classified as absent, less than 1 mm, 1–2 mm, 2 mm, and greater than 2 mm. Loosening was defined as complete radiolucency (≥ 1 mm) around one or two components which was progressive. Cementing technique was classified as adequate when the thickness of the cement mantle was more than 1 mm and covered the prosthesis completely. When there was a defect in the cement mantle in only one zone (see Wrightington method, ), the mantle was classified as sufficient. Where there were defects in more than one zone, the cement mantle was classified as poor. To determine the component size related to the size of the humeral bone, we performed two measurements: (1) the distance between the medial and lateral condyle of the humeral bone, and (2) the distance between the prosthetic condyles of the humeral component. The ratio of these two distances was calculated. In 46 elbows (37%), a humeral bone plug was applied and the influence of this factor on aseptic loosening was analyzed. 4 intraoperative fractures occurred and the consequences were analyzed.
Figure 1. The Wrightington method for measurement of radiolucent lines (RLLs) and position of the Souter-Strathclyde total elbow prosthesis.The RLLs are divided into zones and are scored in two directions (anteroposterior and lateral direction).
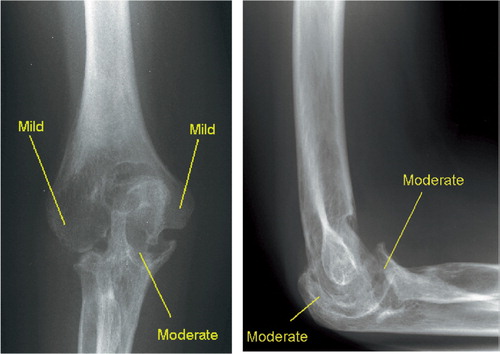
Of the 125 elbows, 104 preoperative radiographs (made up to 6 months before the operation) were available for additional analysis. Firstly, horizontal and vertical dislocation of the elbow was measured (in mm; ), and secondly, bone resorption at four locations (medial and lateral condyles of the humerus, the olecranon, and the coronoid process) was scored as none, minimal, moderate, or severe (). All these observations were done by the first author on standard radiographs as described above. In case of doubt, the senior author assessed the radiographs once again.
Figure 2. Preoperative measurements of the horizontal (A.) and vertical dislocation (B.) on lateral view. Horizontal dislocation is the distance between the posterior cortex of the humerus and the most proximal cortex of the olecranon when the elbow is flexed 90 degrees. Vertical dislocation is the distance between the humeroulnar joint surface and the lowest tip of the humeral medial condyle when the elbow is flexed 90 degrees. In elbows with severe destruction, the dislocation increased in both directions.

Figure 3. The amount of bone resorption in the epicondyles, the olecranon and the coronoid process. coronoideus. The resorption is classified as none, minimal, moderate or severe.
Statistics
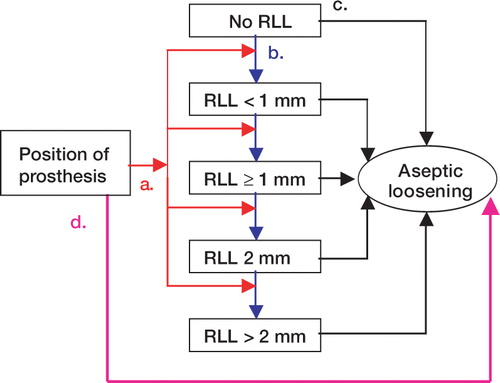
We used a Markov model to describe the development (from none to < 1 mm) and progression of radiolucent lines (Andersen Citation1992, Van Houwelingen Citation1997, Commenges Citation2002)The program we used (MKVPCI version 1.0) allows the time of transition to the next category of radiolucent line width to be interval censored. This means that the exact transition time is only known to lie between two observation times. The effect of the position of the prosthesis on the transition hazards to a subsequent state was assumed to be proportional (significance at p < 0.05 level; ). To analyze the bilaterality problem (15 patients with two elbow prostheses), we fitted a Cox proportional hazards model, correcting for correlation in two different ways. One way was to include a frailty term, and the second way was to use a robust estimate of the standard error (sandwich estimator). With both approaches, the results hardly changed. For the survival of the prosthesis (time to aseptic loosening), related to the preoperative radiographs and to the position of the prosthesis, we used a Cox model (significance at p < 0.05 level). Kaplan-Meier survival curves were obtained for the overall survival of the prosthesis (endpoint: aseptic loosening).
Figure 4. The Markov model for analysis of the radiographs of the Souter-Strathclyde total elbow prosthesis.The RLLs were analysed for different zones around the prosthesis according to the Wrightington method.RLL(s):radiolucent line(s).
Influence of position of the prosthesis on the development and progression of RLLs.
Development and progression of RLLs.
Influence of RLLs on aseptic loosening.
Influence of position of the prosthesis on aseptic loosening, independent of RLLs.
Results
Of the 125 elbow prostheses analyzed, 21 (17%) showed loosening on radiographs. 17 elbows showed loosening of the humeral component, 1 elbow showed loosening of the ulnar component, and in 3 elbows both components loosened simultaneously. The probability of remaining free of aseptic loosening was 89% (SE 3.3%) after 5 years and 65% (SE 8.0%) after 10 years (). In all 125 elbows, the cement mantle was 1 mm or more around both components directly after the operation and no cement defects were noticed; therefore, the quality of the cement mantles was classified as adequate.
Figure 5. Kaplan-Meier survival curve for endpoint aseptic loosening.The 95% confidence interval is given.
The position of components was not obvious in all replacements related to radiolucent lines in this study. On anterioposterior view, the tip of the humeral component was placed in lateral/‘varus’position (102 elbows), neutral position (21 elbows) or medial/‘valgus’position (2 elbows), whereas the tip of the ulnar component was placed in lateral/‘valgus’position (79 elbows), neutral position (40 elbows) or medial/‘varus’position (6 elbows) (). On lateral view the humeral component was tilted anteriorly (61 elbows), posteriorly (30 elbows) or placed in neutral position (34 elbows) while the ulnar component was inserted in extension (99 elbows), flexion (7 elbows) or in neutral position.
Within 1 year after the replacement surgery, lines were found in 18% of the humeral components and in 30% of the ulnar components (). At latest follow-up, these percentages increased to 80% and 76%. When the humeral component was tilted more medially (‘valgus’position on the AP view), we found the development of radiolucent lines at the medial condyle and at the posterior distal zone (Hap4, p = 0.02, and Hlat3, p < 0.01; see ). On the other hand, the progression of these lines was not influenced by this position. If the humeral component was positioned in a more anterior tilt, radiolucent lines occurred more often in Hap4 (p = 0.02) and Hlat2 (p = 0.03), but the progression of these radiolucent lines did not depend on the prosthetic position. For all other humeral and ulnar zones, we could not demonstrate any other statistically significant effect of the position of the humeral component on radiolucent lines. Even no effect of the position was found on the AP view after combining the radiolucent lines of zones Hap2 en Hap3 (lateral side of the prosthesis) and the humeral zones Hap4 and Hap5 (medial side of the component). In 69 elbows (55.2%) radiolucent lines were seen around the ulnar component in Ulat4 en Ulat5 immediately after the operation, but this finding had no effect on the progression of radiolucent lines or aseptic loosening.
Table 1. The relationship (r and standard error) between the angle of the humeral component in the bone (as a continuous variable) and the development and progression of radiolucent lines (second and third column)
We analyzed the relationship between the position (also as a continuous variable, in degrees) of the prosthesis and aseptic loosening, independently of the occurrence of radiolucent lines (, ). The position of the components differed, but no prediction could be made of aseptic loosening whether or not we took the humeral angle on the lateral view as a categorical variable (anterior, neutral, or posterior position) instead of a continuous variable (in degrees). A valgus or a varus position of the humeral component did not have predictive value for aseptic loosening, neither when using continuous analysis (in degrees), nor when using categorical analysis. None of the ulnar positions increased the risk of aseptic loosening.
Figure 6. Lateral and anteroposterior (AP) radiographs of two elbows with small humeral components, taken 5 years after insertion.A.Lateral view of a well-fixed humeral component.B.Lateral view of a migrating humeral component with anterior tilt.C.AP view of a well-fixed humeral component.D.AP view of a migrating humeral component (with a fracture of the medial epicondyle). The ulnar components in all figures show radiolucent lines, but no aseptic loosening was seen.

Table 2. The relationship between the angle of the components (according to the Wrightington method; see and ) and aseptic loosening
We measured the distances between the medial and lateral cortices of the epicondyles and the humeral component (humeral distances 1 and 2 on the AP view; ) and calculated the ratio. Our hypothesis was that a relatively small prosthesis fixed in cancellous bone has less cortical support and will, for that reason, become loose more easily. Although this ratio did vary in the 125 elbows studied (range, 0.51–0.74), we could not demonstrate a relationship with aseptic loosening. Intraoperative fractures occurred in four elbows. In 3 elbows, the medial component fractured and in one elbow the lateral condyle of the humeral bone fractured. The perioperative alignment of these four prostheses had not been changed. 2 of these elbows with intraoperative fractures had aseptic loosening (after 36 and 99 months), but both fractures had healed within 3 months of surgery. 3 medial supracondylar ridges fractured after an average period of 31 (13–56) months postoperatively, after migration of the humeral component. In all of these patients, anterior tilting of the humeral tip had already occurred. We could not find any association between radiolucent lines or aseptic loosening and the use of a humeral bone plug.
Assessment of preoperative radiographs of the elbow had restricted weight in the prediction of aseptic loosening (). Firstly, the Larsen score did not predict the elbows which were at risk for aseptic loosening and, secondly, our scoring method could only prove that bone resorption around the lateral condyle was related to aseptic loosening (p = 0.02).
Table 3. The relationship between preoperative radiographs and aseptic loosening. Narrowing of the pre-operative joint space (negative relationship), increased preoperative resorption of the medial condyle, olecranon, or coronoid process, or increased preoperative dislocation (all positive relationships) were not significantly related. Only preoperative resorption of the lateral condyle showed a significant relationship with aseptic loosening
Discussion
The survival rate was approximately 10% lower after 5 and 10 years of follow-up when radiographic loosening, as previously defined, was used as the endpoint, compared to when the removal of the prosthesis was used as the endpoint (Rozing Citation2000, Van der Lugt et al. Citation2004). This can be explained by the absence of pain even with a loosened prosthesis and delayed revision operation.
Making measurements on standard radiographs, as is done frequently in the outpatient clinic, has some pitfalls. The doctor, responsible for assessment, should realize that such measurements depend on the rotation angle of the upper extremity and on the quality of the radiograph. The Wrightington method was developed to standardize measurements of the Souter-Strathclyde total elbow prosthesis on standard radiographs, but this method requires standardized radiographs of good quality. In contrast to the findings of Trail et al. (Citation1999), our series showed only a minor influence of prosthetic position on aseptic loosening, perhaps because the placement of most prostheses was around the average level and abnormal situations were hardly ever seen. One could postulate that the extremely divergent positions of the prosthesis may be related to aseptic loosening. Hermann and Egund (Citation1998) found that the position of hip prostheses can be ascertained accurately and valid from routine radiographs. Furthermore, Pollock et al. (Citation2001) showed that liner thickness of acetabular components can be determined adequately on radiographs. Thus, we would argue that measurement of component position on standard radiographs is sufficient for clinical assessment of elbow prostheses, but for more detailed position measurements and research purposes, the RSA method is the golden standard (Valstar et al. Citation2002).
Radiolucent lines are difficult to interpret. The definition varies and, furthermore, the meaning of radiolucent lines is not clear (Kwong et al. Citation1992, Freeman Citation1999). As in hip replacements, a radiolucent line around an elbow prosthesis will not always correspond to loosening (Kwong et al. Citation1992). The value of radiolucent lines is restricted for this reason.
The Markov model provides a useful way of analyzing the complex process of aseptic loosening. One weakness of our study, however, is the relatively small amount of elbows relative to the large number of different factors. On the other hand, no obvious statistical trend was seen even after analyzing 125 elbows. The patterns of development and progression of RLLs and aseptic loosening are probably not as clear as one might believe.
The use of a bone plug in elbow prostheses has not been studied extensively. Whereas the efficacy of a bone plug has been proven in hip and knee replacements (better cement mantle and less blood loss), the effect of bone plugs in elbow replacements is not well established (Kligman and Roffman Citation2000, Kumar et al. Citation2000, Klapach et al. Citation2001). In our series the cement mantle was of similar quality in all elbows, and could therefore not predict aseptic loosening.
Preoperative radiographs showed all rheumatic elbows destroyed by arthritis. The frequently applied Larsen score does not enable classification of the amount of dislocation or bone loss (resorption) before the operation. Because of this, we developed an additional scoring list. Validated preoperative scoring methods for bone resorption are needed for research purposes and in order to understand the value of bone resorption prior to joint replacement surgery. Fracture of the medial epicondylar ridge during migration of the humeral component should be prevented. When the migration becomes obvious (e.g. progression of complete radiolucent lines), revision must be considered if fracture of the epicondyle is imminent.
The factors that lead to aseptic loosening of the primary Souter-Strathclyde total elbow prosthesis remain uncertain, and a multifactorial cause seems to be the most plausible explanation.
No competing interests declared.
- Andersen P K. Repeated assessment of risk factors in survival analysis. Stat Methods Med Res 1992; 1(3)297–315
- Commenges D. Inference for multi-state models from interval- censored data. Stat Methods Med Res 2002; 11(2)167–82
- Ferlec D C. Total elbow arthroplasty for treatment of elbow arthritis. J Shoulder Elbow Surg 1999; 8(4)367–78
- Freeman M A. Radiolucent lines: a question of nomenclature. J Arthroplasty 1999; 14(1)1–2
- Gschwend N, Scheier N H, Baehler A R. Longterm results of the GSB III elbow arthroplasty. J Bone Joint Surg (Br) 1999; 81(6)1005–12
- Hargreaves D, Emery R. Total elbow replacement in the treatment of rheumatoid disease. Clin Orthop 1999, 366: 61–71
- Hermann K L, Egund N. Measuring anteversion in the femoral neck from routine radiographs. Acta Radiol 1998; 39(4)410–5
- Ikävalko M, Belt E A, Kautiainen H, Lehto M U. Revisions for aseptic loosening in Souter-Strathclyde elbow arthroplasty. Incidence of revision of different components used in 522 consecutive cases. Acta Orthop Scand 2002; 73(3)257–68
- Klapach A S, Callaghan J J, Goetz D D, Olejniczak J P, Johnston R C. Charnley total hip arthroplasty with use of improved cementing techniques: a minimum twenty-year follow-up study. J Bone Joint Surg (Am) 2001; 83(12)1840–8
- Kligman M, Roffman M. The effect of intramedullary bone plug on femoral stem migration of hydroxyapatite-coated hip arthroplasty. Orthopedics 2000; 23(7)681–5
- Kudo H, Iwano K. Total elbow arthroplasty with a non-constrained surface-replacement prosthesis in patients who have rheumatoid arthritis: a long- term follow-up study. J Bone Joint Surg (Am) 1990; 72(3)355–62
- Kumar N, Saleh J, Gardiner E, Devadoss V G, Howell F R. Plugging the intramedullary canal of the femur in total knee arthroplasty: reduction in postoperative blood loss. J Arthroplasty 2000; 15(7)947–9
- Kwong L M, Jasty M, Mulroy R D, Maloney W J, Bragdon C, Harris W H. The histology of the radiolucent line. J Bone Joint Surg (Br) 1992; 74(1)67–73
- Larsen A, Dale K, Eek M. Radiographic evaluation of rheumatoid arthritis and related conditions by standard reference films. Acta Radiol Diagn (Stockh) 1977; 18(4)481–91
- Mackay D C, Hudson B, Williams J R. Which primary shoulder and elbow replacement? A review of the results of prostheses available in the UK. Ann R Coll Surg Engl 2001; 83(4)258–65
- Pollock D, Sychterz C J, Engh C A. A clinically practical method of manually assessing polyethylene liner thickness. J.Bone Joint Surg (Am) 2001; 83(12)1803–9
- Rozing P. Souter-Strathclyde total elbow arthroplasty. J Bone Joint Surg (Br) 2000; 82(8)1129–34
- Tanaka N, Kudo H, Iwano K, Sakahashi H, Sato E, Ishii S. Kudo total elbow arthroplasty in patients with rheumatoid arthritis. J Bone Joint Surg (Am) 2001; 83(10)1506–13
- Trail I A, Nuttall D, Stanley J K. Survivorship and radiological analysis of the standard Souter- Strathclyde total elbow arthroplasty. J Bone Joint Surg (Br) 1999; 81(1)80–4
- Trancik T, Wilde A H, Borden L S. Captillocondylar total elbow arthroplasty. Two to eight year experience. Clin Orthop 1987, 233: 175–80
- Valstar E R, Garling E H, Rozing P M. Micromotion of the Souter-Strathclyde total elbow prosthesis in patients with rheumatoid arthritis: 21 elbows followed for 2 years. Acta Orthop Scand 2002; 73(3)264–72
- Van der Lugt J C, Geskus R B, Rozing P M. Primary Souter- Strathclyde total elbow prosthesis for rheumatoid arthritis. J Bone Joint Surg (Am) 2004; 86(3)465–73
- Van Houwelingen H C. The future of biostatistics: expecting the unexpected. Stat Med 1997; 16(24)2773–84