Abstract
Background Spontaneous osteonecrosis of the knee (SONK) is a distinct clinical condition occurring in patients without any associated risk factors. There is controversy as to the best method of treatment, and the available literature would suggest that patients with SONK have a worse outcome than those with primary osteoarthrosis when arthroplasty is performed.
We assessed the outcome of medial unicompartmental knee arthroplasty (UKA) using the Oxford prosthesis for end-stage focal spontaneous osteonecrosis of the knee (SONK; Ahlbäck grades III & IV).
Patients and methods We assessed 29 knees (27 patients) with spontaneous osteonecrosis of the knee using the Oxford Knee Score. 26 knees had osteonecrosis of the medial femoral condyle and 3 had osteonecrosis of the medial tibial plateau. All had been operated on using the Oxford Medial Unicompartmental Knee Arthroplasty (UKA). This group was compared to a similar group (28 knees, 26 patients) who had undergone the same arthroplasty, but because of primary osteoarthrosis. Patients were matched for age, sex and time since operation. The mean length of follow-up was 5 (1–13) years.
Results There were no implant failures in either group, but there was 1 death (from unrelated causes) 9 months after arthroplasty in the group with osteonecrosis. The mean Oxford Knee Score in the group with osteonecrosis was 38, and it was 40 in the group with osteoarthrosis.
Interpretation Use of the Oxford Medial UKA for spontaneous focal osteonecrosis of the knee is reliable in the short to medium term, and gives results similar to those obtained when it is used for patients with primary osteoarthrosis.
The treatment of spontaneous osteonecrosis of the knee (SONK) in its early stages is controversial. Forst et al. (Citation1998) reported good results with core decompression by extraarticular drilling of the femoral condyle at the early stages of the disease (Ahlbäck stage I) (Ahlbäck et al. Citation1968). It is, however, known that many patients with early disease and small lesions do well without surgical intervention, and Forst's study contained no control group. It appears that the defining factors as to whether or not osteonecrosis will progress to osteoarthrosis are the size of the lesion, and whether or not it heals before collapse and articular damage ensue (Lotke et al. Citation1982, Lonner and Lotke Citation2001).
Once osteoarthrosis has become established, surgery may be considered. Soucacos et al. (Citation1997) reported the results of proximal tibial osteotomy for the advanced stages of osteonecrosis (Ahlbäck stages III and IV) and suggested that this is a reasonable surgical option for young, active patients. Koshino (Citation1982) followed 37 knees treated with proximal tibial osteotomy, of which only one required knee arthroplasty during the period of review. Several authors have reviewed patients after total knee arthroplasty, with good results. The overall impression is, however, that patients undergoing total knee arthroplasty for osteonecrosis fare slightly worse than those whose diagnosis is primary osteoarthrosis (Bergman and Rand Citation1991, Ritter et al. Citation1991).
Marmor (Citation1993) reported the outcome of fixed bearing unicompartmental prosthesis for osteonecrosis. 30 of 34 knees had good or excellent results and 4 were failures at a mean follow-up of 6 years. Atsui et al. (Citation1997) used a ceramic unicompartmental prosthesis in 10 patients, with good early results and no failures. We report our experience using a mobile-bearing unicompartmental prosthesis for established arthrosis that is secondary to osteonecrosis of the knee, where the prosthesis is inserted by a minimally invasive approach.
Patients and methods
All patients undergoing Oxford Medial Uni-compartmental Knee Arthroplasty (UKA; Biomet-Merck, Bridgend, UK) were followed prospectively at the two centers involved in this study. At the time of surgery, all patients had intact cruciate ligaments, correctable varus deformity and full preservation of the thickness of the articular cartilage in the lateral and patellofemoral compartments, consistent with the selection criteria for Oxford UKA. The surgical technique was as previously described for the Oxford UKA using the minimally invasive approach(The Oxford Phase 3 Unicompartmental Knee, Manual of the Surgical Technique, Biomet-Merck Ltd).
From these patient series, all patients with a primary diagnosis of SONK were identified. This cohort of patients was compared with a control group of patients who had undergone UKA using the Oxford prosthesis for primary medial compartment osteoarthrosis. Cases were matched for age, sex, time since surgery (to within 3 months) and the center at which the surgery was performed.
All patients were assessed clinically and radiographically, and the Oxford Knee Score (OKS) was used as a measure of outcome. The OKS is a patient-based questionnaire that allows the patient to report both levels of functional activity and symptoms, and it has previously been validated for use with patients suffering from degenerative arthrosis of the knee. A Swedish translation of the OKS has been produced and validated (Dunbar et al. Citation2000). Patients are asked a series of 12 questions, and their response scores range from 0 (worst) to 4 (best) for each, giving a total range of 0–48 (Dawson et al. Citation1998). All living patients were contacted, and for the 1 patient who had died due to unrelated causes, we established the state of the implant at the time of death from the hospital records and from the general practitioner.
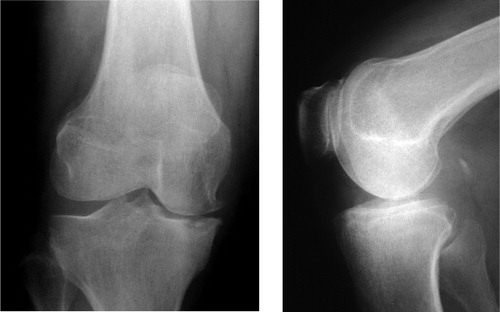
The control group included 26 patients (28 knees) with a mean age of 71 (46–85) years. The mean follow-up time was 4.8 (1-13) years. We identified 27 patients with osteonecrosis; 16 from Oxford and 11 from Skövde. 2 of the Oxford patients had undergone bilateral procedures for osteonecrosis, giving a total of 29 knees. For these patients, an Oxford Knee Score was recorded for each knee. 22 of the patients were female (23 knees) and the mean age was 73 (43–88) years. The medial femoral condyle was affected in 26 of the knees (); in 3, the medial tibial plateau was affected (). Regarding the patient who had died 9 months after surgery, her prosthesis had been intact, functioning and satisfactory at the last clinical review. A total of 28 prostheses were thus available for review. The mean time to review was 5.2 (1–13) years.
Figure 1. Plain anteroposterior and lateral radiographs showing focal osteonecrosis of the medial femoral condyle.

Figure 2. Plain anteroposterior and lateral radiographs showing focal osteonecrosis of the medial tibial plateau.
The pre- and postoperative clinical scores for the group with primary diagnosis of SONK were compared to those from the control group of primary osteoarthritis using Student's t-test. As the inclusion of patients with bilateral implants could be a confounding factor, only one score (the worst for each patient) was included in the statistical comparison. The scores for all knees have been included in the descriptive statistics for each group, however.
Results
In the osteonecrosis group, no knees had undergone revision for either infection or loosening: all patients reported satisfaction with their implant and showed an improvement in their Oxford Knee Score. In the control group, no knees had undergone revision, and all patients were satisfied with the results of their surgery. There was no statistically significant difference between the groups in terms of outcome when using the Oxford Knee Score as a measurement (Table).
Oxford Knee Score (OKS) (mean (SD))
Discussion
Two centers were involved in this study. Both have previously reported similar results using the Oxford prosthesis (Murray et al. Citation1998, Svärd and Price Citation2001). The reliability of this prosthesis has also been verified recently by results from a nonteaching hospital (Rajasekar et al. Citation2004).
As with most cohort studies, the length of follow-up varies for individual patients. We chose not to report on the outcome of the Oxford Knee Score over time. Recovery from UKA with a minimally invasive approach is known to be rapid; late decline in function and increase in pain levels are associated with implant loosening, dislocation of the meniscal bearing and progression of arthrosis in the lateral tibiofemoral compartment. The Oxford Knee Score has been validated in both English- and Swedish-speaking countries, and would be expected to identify patients with these potential problems. None were encountered in this study.
Advancing age in itself can be expected to bring about a steady decline in score, as a result of reduction in functional level. However, we have attempted to counteract this by matching patients for both age and time since surgery. In addition, the Oxford Medial UKA has a well-documented track record and recent work has shown that the sagittal plane kinematics of a knee with an Oxford Medial UKA in situ are similar after 1 and 10 years, implying that the Oxford Medial UKA functions equally well at both early and late time points (Price et al. Citation2004). Recovery from unicompartmental knee arthroplasty has been shown to be faster than recovery from total knee arthroplasty, with function better than preoperative levels by 6 months (Yang et al. Citation2003). We thus deemed it appropriate to include all patients with a minimum follow- up of 1 year, and to use a single comparison of preoperative and latest postoperative score.
The number of patients in this study was small, reflecting the relative rarity of spontaneous osteonecrosis of the knee, and a survival analysis cannot be done because there have been no failures to date in our groups.
There is a small risk of type-2 error because of the small numbers in the cohorts. However, there is overlap of confidence interval ranges for both pre- and postoperative Oxford Knee Scores in the two groups (Table). In addition, the 95% confidence intervals of the differences between the two means for the pre- and postoperative Oxford Knee Scores (Table) add further weight to the argument that the difference in score seen between the group with SONK and that with osteoarthrosis as a primary diagnosis is not statistically significant. Furthermore, a retrospective power calculation can be done. Using the mean and SD from the group with osteoarthrosis (40, SD 6.2, see Table) a significance level of 0.05, a power value of 0.8 and assuming that a 10% change in score (i.e. 4 points) would represent a significant difference, this power calculation suggests that 24 patients in each group would be sufficient for identification of any statistically significant difference. We had 28 knees in each group, but only 26 were used for statistical analysis to counter the potential effect of bilateral procedures.
From a technical point of view, implantation of the Oxford knee is demanding, and certain considerations must be taken into account when using the implant for osteonecrosis. The classic defect in the medial femoral condyle occurs in the weight-bearing area in extension: failure to identify the presence of a crater may result in the unwary surgeon recessing the spigot too deeply and thereby milling too much bone from the medial femoral condyle. This could then cause problems in balancing the extension gap. In addition, because of surrounding bony sclerosis, an attempt should be made to completely excavate any craters in the femoral condyle—or to completely remove the osteonecrotic lesion in the medial tibial plateau so that normal bone can be used as a base for cement impregnation. It may be necessary for large craters to be filled with autologous bone graft harvested from the bone removed at surgery.
No competing interests declared.
- Ahlbäck S, Bauer G C, Bohne W H. Spontaneous osteonecrosis of the knee. Arthritis Rheum 1968; 11: 705–33
- Atsui K, Tateishi H, Futani H, Maruo S. Ceramic unicompartmental knee arthroplasty for spontaneous osteonecrosis of the knee joint. Bull Hosp Jt Dis 1997; 56(4)233–6
- Bergman N R, Rand J A. Total knee arthroplasty in osteonecrosis. Clin Orthop 1991, 273: 77–82
- Dawson J, Fitzpatrick R, Murray D, Carr A. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg (Br) 1998; 80: 63–9
- Dunbar M J, Robertsson O, Ryd L, Lidgren L. Translation and validation of the Oxford-12 item knee score for use in Sweden. Acta Orthop Scand 2000; 71(3)268–74
- Forst J, Forst R, Heller K D, Adam G. Spontaneous osteonecrosis of the femoral condyle: causal treatment by early core decompression. Arch Orthop Trauma Surg 1998; 117: 18–22
- Koshino T. The treatment of spontaneous osteonecrosis of the knee by high tibial osteotomy with and without bone grafting or drilling of the lesion. J Bone Joint Surg (Am) 1982; 64: 47–58
- Lonner J H, Lotke P A. Tibial Osteonecrosis. AAOS Instructional course lectures 2001; 50: 477–81
- Lotke P A, Abend J A, Ecker M L. The treatment of osteonecrosis of the medial femoral condyle. Clin Orthop 1982, 171: 109–15
- Marmor L. Unicompartmental arthroplasty for osteonecrosis of the knee joint. Clin Orthop 1993, 294: 247–53
- Murray D W, Goodfellow J W, O'Connor J J. The Oxford medial unicompartmental arthroplasty. A ten-year survival study. J Bone Joint Surg (Br) 1998; 80: 983–9
- Price A J, Rees J L, Beard D J, Gill R H, Dodd C A. F, Murray D W. Sagittal plane kinematics of a mobile-bearing unicompartmental knee arthroplasty at 10 years: A comparative in vivo fluoroscopic analysis. J Arthroplasty 2004; 19(5)590–7
- Rajasekar C, Das S, Smith A. Unicompartmental knee arthroplasty: 2-12 year results in a community hospital. J Bone Joint Surg (Br) 2004; 86: 983–5
- Ritter M A, Eizember L E, Keating E M, Faris P M. The survival of total knee arthroplasty in patients with osteonecrosis of the medial condyle. Clin Orthop 1991, 267: 108–14
- Soucacos P N, Xenakis T H, Beris A E, Soucacos P K, Georgoulis A. Idiopathic osteonecrosis of the medial femoral condyle: classification and treatment. Clin Orthop 1997, 341: 82–9
- Svärd U C G, Price A J. Oxford medial unicompartmental knee arthroplasty. A survival analysis of an independent series. J Bone Joint Surg (Br) 2001; 83: 191–4
- Yang K Y, Wang M C, Yeo S J, Lo N N. Minimally invasive unicondylar versus total condylar knee arthroplasty–early results of a matched-pair comparison. Singapore Med J 2003; 44(11)559–62