Abstract
Background The best treatment for primary patellar dislocation has been the subject of debate. Surgery has been recommended for all patients or for special subgroups to improve outcome. We have previously reported similar 2-year results after closed or open treatment. This report concerns 127 patients who were re-evaluated by questionnaire at least 5 years after the primary onset.
Patients and methods At baseline, the patients were randomized regarding closed treatment (57) or individually adjusted proximal realignment operation (70). All patients were re-evaluated after a mean follow-up of 7 (6-9) years.
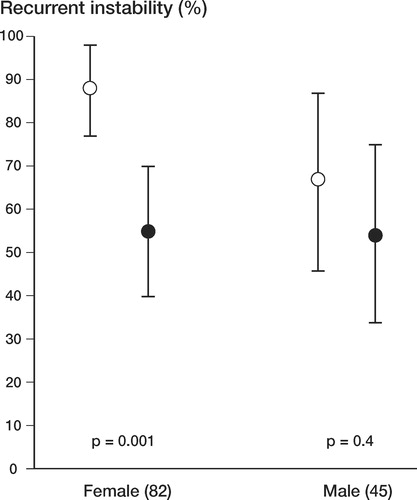
Results The outcomes were similar: the patient's own overall opinion was excellent or good after closed treatment in 81% of cases and after operative treatment in 67%. Mean Kujala and Hughston VAS knee scores were 90 and 94, respectively, after closed treatment and 88 and 89 after operative treatment. The proportions of stable patellae were 30% and 36% for closed treatment and operative treatment, respectively. In a multivariate risk analysis, there was a correlation between a Kujala score of less than 90 and female sex (OR: 3.5; 95% CI: 1.4-9.0), loose bodies on radiographs (4.1; 1.2-15), and also an initial history of contralateral patellar instability (3.6; 0.9-15). There were 2 risk factors for recurrent instability: initial contralateral instability (4.9; 0.9-28) and young age (0.9; 0.8-1.0/year). Girls with open tibial apophysis had the worst prognosis for instability (88%; 95% CI: 77-98).
Interpretation We do not recommend proximal realignment surgery for treatment of primary dislocation of the patella.
Primary dislocation of the patella is usually treated nonoperatively. However, this practice has been challenged (Sargent and Teipner Citation1971). If dislocation is the result of predisposing factors causing malaligment, correcting the malalignment at first presentation might improve the outcome. Primary dislocation of the patella was considered an indication for proximal realignment surgery from the mid-1970s in two institutions in Helsinki. In 1991, a randomized study was set up to justify this operative policy. Surgical realignment was compared with immobilization for 3 weeks followed by functional rehabilitation. The results were similar after 2 years (Nikku et al. Citation1997). We have now reassessed the following by questionnaire after 5 years or more: subjective opinion, stability, knee score and later operations. We also performed a risk analysis of predisposing factors.
Patients and methods
177 patients with primary dislocation of the patella were admitted to two trauma centers in Helsinki, Finland, during the period January 1991 to December 1992. Inclusion criteria were as follows: first lateral dislocation of the patella; injury not more than 14 days old; no previous knee injury/surgery; no tibiofemoral ligament injuries requiring repair; no osteochondral fractures requiring fixation. No power calculations of sample sizes were made, but we expected to get over 40 patients in each group.
On admission, all patients underwent clinical and radiographic assessment, examination under anesthesia (EUA), and arthroscopy. Diagnostic criteria were locked dislocation, dislocatability in EUA, or typical arthroscopic lesions and subluxation (Ficat Citation1970) in EUA. Randomization was performed according to the year of birth (odd/even), offering the same choice of treatment if both knees were affected during the recruitment period of this study. In such bilateral cases, the knee to be included in the study was chosen at random after the 2-year evaluation.
During 1991 and 1992, we randomized 127 patients with primary patellar dislocation either to closed treatment (57 patients, designated group C) or to operative treatment (70 patients, designated group O). Of these patients, 30 and 40, respectively, were under 16 years of age (). The diagnosis was based on: locked dislocation in 68 patients; dislocatability in EUA in 47, and subluxation in EUA combined with typical arthroscopic lesions in 12. In the operative group, 63 patients had repair of the medial retinaculum by suturing, by duplication, or by additional augmentation of the patellofemoral ligament. Of these, 54 had a lateral release. 7 patients, all with subluxation on EUA, had only a lateral release for realignment. The aftercare was identical in groups C and O. We have previously reported this patient series in detail, including their 2-year outcome (Nikku et al. Citation1997).
Table 1. Baseline characteristics of 127 patients with primary patellar dislocation
We recorded the Q-angle (pathological when < 19° for women and when < 16° for men; Woodland and Francis Citation1992), generalized ligamentous laxity (< 3/5 positive; Carter and Wilkinson Citation1964), bilateral femoral neck antetorsion (trochanter prominence test; Ruwe et al. Citation1992) and outward rotation of the tibia, ankle and foot (forced thigh-foot angle; Stuberg et al. Citation1991).
From primary radiographs, we assessed the Insall-Salvati index (pathological < 1.2; 1971) maturation of the tibial apophysis, medial avulsion fracture of the patella, Wiberg class (pathological 2/3–5; Wiberg Citation1941, Baumgartl Citation1966), pathological lateral patellofemoral angle (parallel or opening medially; Laurin et al. Citation1978), displacement greater than 1 mm (Laurin et al. Citation1979), sulcus angle (Brattström Citation1964), and presence of loose body.
We re-evaluated all the 127 patients by questionnaire after a mean of 7.2 (5.7–9.1) years from primary onset. Subjective outcome was assessed by three methods: the patient’s opinion (excellent, good, fair or poor), Kujala patellofemoral score (Kujala al. Citation1993) and Hughston visual analogue scale (VAS, Flandry et al. Citation1991). Redislocations and recurrent subluxations were combined as “instability”, and Tegner activity score (Tegner and Lysholm Citation1985) and later operations were recorded.
Statistics
Comparisons of means and medians between the groups were performed by Mann-Whitney ranksum test and Student’s two-tailed t-test. The chisquare test with continuity correction of Yates, and Fisher’s exact test were used to compare the differences in proportions. Adjustment of groups for dichotomized and continuous parameters was done by logistic and median regression analysis, respectively. Significance was set at 0.05. Confidence intervals (95% CI) for the differences between the groups are given. Risk parameters for the logistic regression model, including the method of treatment, were chosen by prediction in bivariate analyses and by clinical significance, and odds ratios (OR) were calculated.
Results
Outcome was similar in the two treatment groups ()
Subjective opinion. Female sex and initial contralateral patellar instability were associated with a worse subjective opinion in bivariate analysis. 40 of the 45 men assessed their knee as being excellent or good, as compared to 53 of the 82 women. 13 patients had experienced instability of the contralateral patella before the study, but only 5 of them found their study knee to be excellent or good, compared to 88 of the 114 patients without contralateral instability.
Table 2. Results of 127 patients after 7 years of primary patellar dislocation
Knee scores. Knee function was rated by 126 patients with both the Kujala score (mean 85 (10–100)) and with Hughston VAS score (mean 86 (40–100)). Lower scores (Kujala; Hughston) were predicted by female sex (p = 0.001; < 0.001), by higher Q-angle (p = 0.003; 0.002) and by the presence of a loose body on primary radiographs (p = 0.08; 0.03).
Stability and trust. Recurrent instability was predicted by factors such as young age (p < 0.001), a family history of patellar dislocation (p = 0.01), higher Q-angle (p = 0.009), lower forced thigh-foot angle (p = 0.04) and higher sulcus angle (p = 0.01). Girls with an open tibial tuberosity apophysis showed the greatest likelihood of having recurrent patellofemoral instability (Figure).
The significance of skeletal maturity and sex for incidence (95% CI) of recurrent patellar instability at (median) 7-year follow-up, adjusted according to mode of treatment.Open circles correspond to patients with open apophysis of the tibial tubercle at baseline;black circles correspond to patients with closed apophysis.
The number of patients reporting lack of trust in the knee was similar in the two groups (group C: 21/57; group O: 22/69). Lack of trust was associated with female sex (p = 0.01). Contralateral patellar instability was experienced by 13 patients before the study and by 3 during the study. 19 patients had contralateral instability of the patella at the 2-year evaluation and 34 patients had contralateral instability at 7 years.
Later operations. 61 operations were undertaken later: for 13 patients in group C and for 20 patients in group O. These were diagnostic arthroscopies (5 and 8 patients, respectively), therapeutic arthroscopies (5 and 7 patients, respectively), proximal (4 patients and 1 patient, respectively) and distal realignment operations (4 patients and 1 patient, respectively). 5 patients in group O had other knee procedures. Young age (p = 0.002), higher sulcus angle (p = 0.01) and lateral patellar displacement (p = 0.03) were predictive of later operation.
Analysis of risk factors for poor outcome. Poor outcome was defined by two dependent parameters: a Kujala score of less than 90 and recurrent instability of the patella. The logistic regression model had mode of treatment, 6 factors from the patient history, 2 from the clinical examination and 4 from radiographs as independent parameters (). Female gender (OR 3.5) and loose body in radiographs (OR 4.1) were the clearest risks for low Kujala score. Age was predictive of stability. Instability of the contralateral patella at admission was a possible risk factor for both low Kujala score and instability.
Table 3. Logistic regression models for the odds of poor 7-year outcome after primary patellar dislocation
Discussion
In this study, trial surgery did not improve the results achieved by immobilization alone after primary dislocation of the patella. The overall rate of stable patellae at the 7-year follow-up (33%) was lower than expected. The risk analysis emphasized the importance of female gender, young age, bilaterality, and osteochondral fractures on prognosis.
The high risk of redislocation after closed treatment made us change to an operative policy during the 1970s. The natural history of primary patellar dislocation may, however, be stronger than the effect of treatment. There is a trend towards redislocation with longer follow-up time, both in closed-treated and in operative series (Harilainen and Sandelin Citation1993, Mäenpää and Lehto Citation1997). The shorter follow-up of operative series might explain the better results obtained after primary surgery.
Most studies on acute dislocation also include an analysis of risk factors for poor outcome. Recurrent instability seems to be most frequent in children. Cash and Hughston (Citation1988) reported a higher rate of redislocation (60%) in patients under 15 years old. On the contrary, Cofield and Bryan (Citation1977) could not find any prognostic value of age or sex. The risk factors leading to primary dislocation must be clearly separated from the factors tested in this study. The former have been analyzed in cohort studies, but this trial assessed outcome only after the first episode. The similarity of results between our treatment groups made us test other factors that might possibly modify the outcome. The choice of these factors was based on both clinical and bivariate analysis.
Our trial included both children and adults, but congenital and syndrome-related dislocations were excluded. The median age of patients in both groups was 20 years in males and 19 in females. Andersen (Citation1955; n = 201) and Rünow (Citation1983; n = 67) observed a median age at primary dislocation in females between 13 and 14 years in their retrospective studies. The peak incidence for males occurred 2–3 years later, reflecting the spurt in male growth at puberty. They met their patients at a later, recurrent state of instability while our prospective study collected them directly after the primary injury. Other explanations for the differences in median age may be the inclusion criteria, semantic considerations, the different times 1955, 1983, 1991, or pure chance. The age distribution of the patients in these different studies, however, seems to play a very important role for the outcome.
The proportions of females in groups C and O were not identical. Thus, the comparison of the treatment groups had to be redone by adjusting the outcome for age and sex (). The multivariate analysis with the logistic regression model included both the primary therapy and sex. The effect of gender was stronger than the mode of treatment ().
The primary surgery consisted of realigning the extensor mechanism and repairing the medial patellar ligaments according to the extent and location of individual pathoanatomy. All surgeons were familiar with the techniques, and they were at liberty to use the most suitable one(s). The operative group had the advantage of “modern” surgery of the medial structures, but may have had the disadvantage of releasing the lateral stabilizing retinaculum (Conlan et al. Citation1993, Desio et al. Citation1998). The result of our study must be related to the type of surgery, and not just to surgery of any kind. Later operations in both groups may also have acted as a confounding factor. We excluded patients with large osteochondral fractures, but smaller loose bodies also seemed to cause problems ().
Questions about the occurrence of instability were asked twice at the 2-year follow-up and once after 5 years. It was clear that the episodes—and even the side affected—can easily be forgotten. Patients with spontaneous relocation at primary onset might understand the word “redislocation” differently from those who had locked dislocation. This led us to combine various types of instability. This, along with the prospective longitudinal nature of the study, may account for the unusually low incidence of stability (33%). Contralateral patellar instability was found in only one-quarter of the patients. The first dislocation might cause behavioral changes that may protect the other side.
We did not find a better outcome after early operative correction of the posttraumatic pathology, combined with realignment of the extensor mechanism by lateral release. Recurrent patellar instability is most common in skeletally immature girls. This subpopulation should be the focus of further trials.
The authors thank Dr. Hannu Kautiainen for statistical analysis of the data and Dr. Joanne Minford for revision of the manuscript. The study was financially supported by the Finnish Orthopedic Association.
- Andersen P T. En klinisk undersøgelse over luxatio patellae. Det Hoffensbergske Etablissement, København 1955
- Baumgartl F. Anatomische und klinische bedeutung des femoropatellargelenkes. Zbl Chir 1966; 91: 505–16
- Brattström H. Shape of the intercondylar groove normally and in recurrent dislocation of patella. A clinical and X-ray-anatomical investigation. Acta Orthop Scand (Suppl 68) 1964; 1–148
- Carter C, Wilkinson J. Persistent joint laxity and congenital dislocation of the hip. J Bone Joint Surg (Br) 1964; 46: 40–5
- Cash J D, Hughston J C. Treatment of acute patellar dislocation. Am J Sports Med 1988; 16(3)244–9
- Cofield R H, Bryan R S. Acute dislocation of the patella: results of conservative treatment. J Trauma 1977; 17(7)526–31
- Conlan T, Garth W J , Lemons J E. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg (Am) 1993; 75: 682–93
- Desio S M, Burks R T, Bachus K N. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med 1998; 26(1)59–65
- Ficat P. Pathologie fémoro-patellaire1 ed. Masson et Cie, Paris 1970; 1: 234
- Flandry F, Hunt J P, Terry G C, Hughston J C. Analysis of subjective knee complaints using visual analog scales. Am J Sports Med 1991; 19(2)112–8
- Harilainen A, Sandelin J. Prospective long-term results of operative treatment in primary dislocation of the patella. Knee Surg Sports Traumatol Arthroscopy 1993; 1: 100–3
- Insall J, Salvati E. Patella position in the normal knee joint. Radiology 1971; 101: 101–4
- Kujala U M, Jaakkola L H, Koskinen S K, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy 1993; 9(2)159–63
- Laurin C A, Lévesque H P, Dussault R, Labelle H, Peides J P. The abnormal lateral patellofemoral angle: a diagnostic roentgenographic sign of recurrent patellar subluxation. J Bone Joint Surg (Am) 1978; 60(1)55–60
- Laurin C A, Dussault R, Levesque H P. The tangential x-ray investigation of the patellofemoral joint: x-ray technique, diagnostic criteria and their interpretation. Clin Orthop 1979, 144: 16–26
- Mäenpää H, Lehto M U K. Patellar dislocation. The long-term results of nonoperative management in 100 patients. Am J Sports Med 1997; 25(2)213–7
- Nikku R, Nietosvaara Y, Kallio P E, Aalto K , Michelsson J E. Operative versus closed treatment of primary dislocation of the patella. Similar 2-year results in 125 randomized patients. Acta Orthop Scand 1997; 68(5)419–23
- Rünow A. The dislocating patella. Etiology and prognosis in relation to generalized joint laxity and anatomy of the patellar articulation. Acta Orthop Scand (Suppl 201) 1983; 54: 1–53
- Ruwe P A, Gage J R, Ozonoff M B , deLuca P A. Clinical determination of femoral anteversion. J Bone Joint Surg (Am) 1992; 74(6)820–30
- Sargent J R, Teipner W A. Medial patellar retinacular repair for acute and recurrent dislocation of the patella: a preliminary report. J Bone Joint Surg (Am) 1971; 53(2)386
- Stuberg W, Temme J, Kaplan P, Clarke A, Fuchs R. Measurement of tibial torsion and thigh-foot angle using goniometry and computed tomography. Clin Orthop 1991, 272: 208–12
- Tegner Y, Lysholm J. Rating system in evalution of knee ligament injuries. Clin Orthop 1985, 198: 43–9
- Wiberg G. Roentgenographic and anatomic studies on the femoropatellar joint. With special reference to chondromalacia patellae. Acta Orthop Scand 1941; 12: 319–410
- Woodland L H, Francis R S. Parameters and comparisons of the quadriceps angle of college-aged men and women in the supine and standing positions. Am J Sports Med 1992; 20(2)208–11