Abstract
We present 3 cases of arthroscopically treated intraarticular osteoid osteoma of the ankle. Emphasis is on the high index of suspicion for this lesion, the appropriate imaging modality and the efficacy of arthroscopic excision of these tumors with superficial location in the talus and tibial plafond.
Case 1 (talar lesion)
A 23-year-old woman presented with left ankle pain lasting several months. The pain was worse at night, was aggravated by activity and relieved with non-steroid antiinflammatory drugs (NSAID). There was a mild swelling of the ankle, extreme tenderness over the anterior joint line, a near-normal motion and a positive dorsiflexion impingement test.
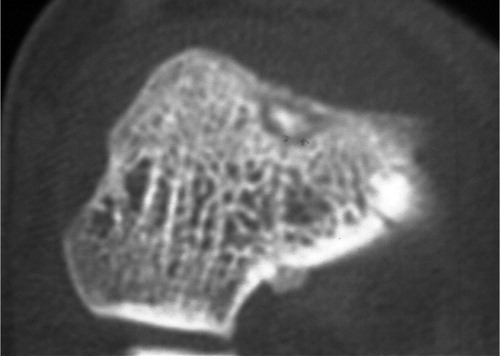
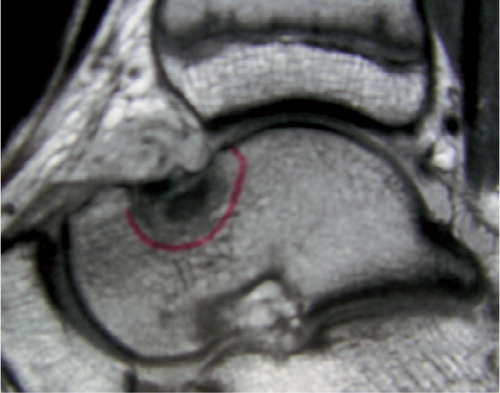
Plain radiographs revealed a small spur on the talar neck (). A triple-phase bone scan demonstrated a hot spot over the anterior talus and tibia, and the initial diagnosis was anterior impingement with synovitis. The patient underwent ankle arthroscopy, where anterior synovitis with mild anterior impingement was noted and a localized synovectomy was performed. Initially relief of symptoms was experienced, but the pain never ceased. MRI of the ankle 5 months after the arthroscopy showed a large area of abnormal signal intensity on T2 weighted images, involving the talar neck. A new bone scan revealed a hot spot over the talar neck and the double density sign (an area of increased uptake surrounding a focus of intense uptake). CT scan of the talus showed a slightly sclerotic nidus measuring 3−4 mm in diameter, just under the cortex of talus anteriorly, surrounded by a relatively lucent halo (). A diagnosis of a subcortical osteoid osteoma of the talar neck was made.
Figure 1. Case 1. Plain radiograph showing a bone spur on the dorsal aspect of the talus: the exostotic osteoid.

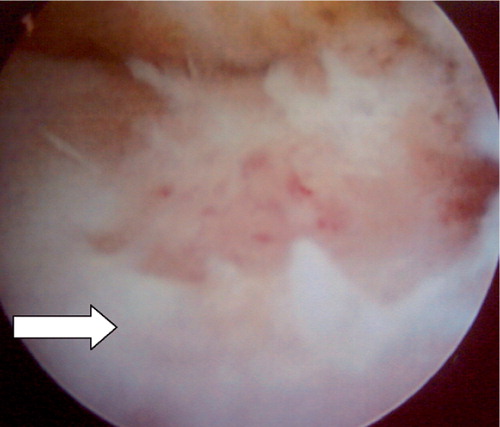
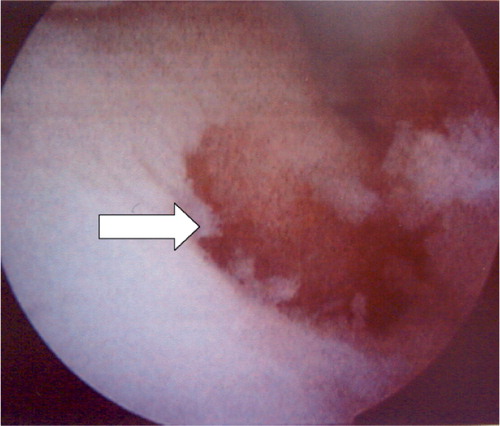
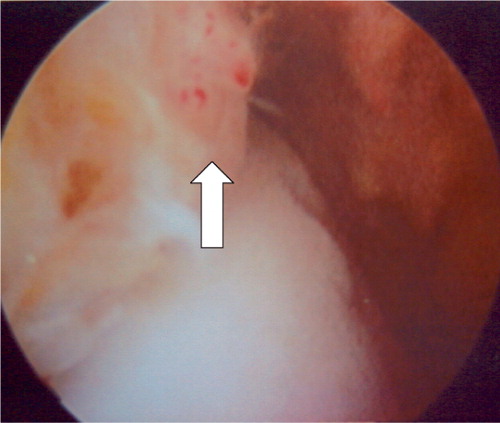
Considering the superficial location of the tumor, an arthroscopic excision was possible. With the patient under spinal anesthesia and supine, arthroscopy was carried out through an anteromedial portal and the lesion was identified in the anteromedial aspect of the talar neck close to the capsular insertion. There was a slight cherry-red elevation, with blood vessels coursing radially towards the lesion and evidence of localized synovitis (). An anterolateral portal was established and the cortex was debrided using a motorized shaver. The nidus was exposed, appearing as hyperemic soft bone and was removed with a small curette. Specimens were sent for histopathology. The remainder of the lesion was debrided using the shaver (). The patient reported immediate postoperative pain relief and was discharged the day after surgery, and could soon assume full weight bearing. Microscopic examination showed an osteoid osteoma. The patient was reviewed after a year and remained asymptomatic.
Case 2 (talar lesion)
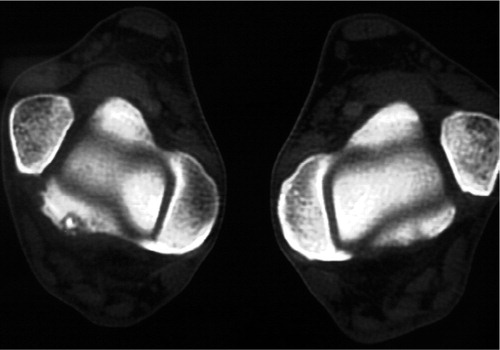
A 13-year-old soccer-playing boy presented after 1 year of ankle pain with spontaneous onset. A CT investigation revealed an 8-mm sclerotic zone surrounding a nidus, and MRI confirmed the findings suggesting an osteoid osteoma surrounded by bone edema ( and ). An arthroscopic excision was made, with findings similar to those from case 1. The sclerotic zone was debrided with a shaver and the softer bone with the nidus was resected with a curette. Histologic examination confirmed the diagnosis and the postoperative pain relief was immediate. At 6 months follow-up, the patient was still asymptomatic.
Case 3 (tibial plafond lesion)
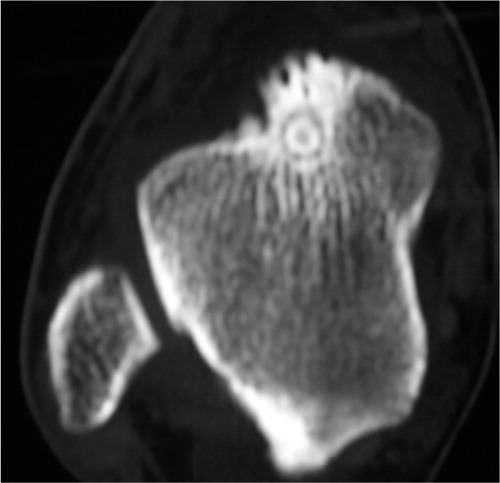
A 31-year-old man had left ankle pain for 3 years, increasing over 3 months. The pain was present at rest and increased at night, and was relieved by NSAID. He had mild swelling of the ankle joint and slightly reduced motion. Plain radiographs of the ankle were normal. Triple-phase bone scan showed increased tracer uptake in all 3 phases in the anterior aspect of the left ankle. CT scan revealed a focal area of low attenuation at the anterior margin of the subarticular surface of the left tibia, and a central area of calcific density measuring 3−4 mm with no evidence of sclerosis or new bone formation (). The diagnosis was a subperiosteal osteoid osteoma involving the tibial plafond.
An arthroscopic excision was performed. A cherry-red elevated lesion was visualized in the medial third of the distal anterior tibia in the jux-taarticular location, measuring 6 mm (). There was local synovitis in the region and the vessels were seen radiating towards the lesion. The thin cortex was shaved and it revealed a central soft, hyperemic region with minimal surrounding sclerosis. This was removed with a curette and sent for histopathology. The remainder of the lesion was debrided with the motorized shaver to healthy cancellous bone, leaving a crater measuring 9 mm. Postoperatively, the patient reported total pain relief. Histology showed an osteoid osteoma. The patient was reviewed after 1 year and continued to be pain-free.
Discussion
The talus is involved in 5−10% of the cases in large series of osteoid osteoma (Kenzora and Abrams Citation1981, Capanna et al. Citation1986). In their study of 40 cases of osteoid osteoma and osteoblastoma of the talus, Capanna et al. (Citation1986) found the talar neck to be most frequently involved, with the tumor often intraarticular and located subperiosteally at the chondro-osseous junction. Several case reports have described talar osteoid osteoma involving the talar neck in this superficial location (Kenzora and Abrams Citation1981, Resnick et al. Citation1995, Chuang et al. Citation1998, Tuzuner and Aydin Citation1998). Involvement of the tibial plafond is rare, and has only been presented in some case reports (Kenzora and Abrams Citation1981, Donley et al. Citation2000).
Historically, intraarticular osteoid osteoma of the ankle has posed a difficult diagnostic challenge with diagnostic delays (Kenzora and Abrams Citation1981, Francesco et al. Citation2002), often mimicking other conditions such as chronic sprain, anterior impingement, stress fracture, osteomyelitis, osteonecrosis or monoarticular arthritis. Furthermore, these tumors have atypical radiological features. Subperiosteal tumors usually lack the intense bone sclerosis seen in other locations, sometimes presenting as a predominantly lucent lesion, and at times appearing like a bony spur, the so-called exostotic osteoid which was present in our patient no. 1 (). Kenzora and Abrams (Citation1981) speculated that osteoid osteoma of the talus may not be discovered even on surgical exploration if the duration of symptoms is less than 3-5 months. These authors suggested that it probably takes more than 1 year for the lesion to mature and develop gross pathological clues as to the location of tumor (Kenzora and Abrams Citation1981). This may explain the delay in case no 1. A high degree of suspicion in the first 3 decades of life and the use of bone scan and CT in combination with conventional radiographs has been recommended for early diagnosis (Capanna et al. Citation1986). MRI may also be used for the diagnosis, but the images may sometimes present a misleading, aggressive appearance (Assoun et al. Citation1994, Hachem et al. Citation1997, Davies et al. Citation2002).
Arthroscopic removal of an intraarticular osteoid osteoma was first reported for the knee (Heuijerjans et al. Citation1986). Subsequently, the technique has been used for excision of osteoid osteoma in the hip, the knee, the ankle and the shoulder. Arthroscopic removal of an osteoid osteoma of the talar neck was first described by Resnick et al. (Citation1995) and later by Tuzuner and Aydin (Citation1998). Both cases involved the talar neck and the tumor was subperiosteal, which makes arthroscopic removal a minimally invasive and effective treatment.
- Assoun J, Richardi G, Railhac J J, Baunin C, Fajadet P, Giron J, Maquin P, Haddad J, Bonnevialle P. Osteoid osteoma: MR imaging versus CT. Radiology 1994; 191: 217–23
- Capanna R, Van Horn J R, Ayala A, Picci P, Bettelli G. Osteoid osteoma and osteoblastoma of the talus. A report of 40 cases. Skeletal Radiol 1986; 15: 360–4
- Chuang S Y, Wang S J, Au M K, Huang G S. Osteoid osteoma in the talar neck: a report of two cases. Foot Ankle Int 1998; 19: 44–7
- Davies M, Cassar-Pullicino V N, Davies A M, McCall I W, Tyrrell P N. The diagnostic accuracy of MR imaging in osteoid osteoma. Skeletal Radiol 2002; 31: 559–69
- Donley B G, Philbin T, Rosenberg G A, Schils J P, Recht M. Percutaneous CT guided resection of osteoid osteoma of the tibial plafond. Foot Ankle Int 2000; 21: 596–8
- Francesco B, Andrea L A, Vincenzo S. Intra-articular osteoid osteoma of the lower extremity: diagnostic problems. Foot Ankle Int 2002; 23: 264–7
- Hachem K, Haddad S, Aoun N, Tamraz J, Attalah N. MRI in the diagnosis of osteoid osteoma. J Radiol 1997; 78: 635–41
- Heuijerjans W, Dandy D J, Harris D. Arthroscopic excision of an intra-articular osteoid osteoma at the knee. Arthroscopy 1986; 2: 215–6
- Kenzora J E., Abrams R C. Problems encountered in the diagnosis and treatment of osteoid osteoma of the talus. Foot Ankle 1981; 2: 172–8
- Resnick R B, Jarolem K L, Sheskier S C, Desai P, Cisa J. Arthroscopic removal of an osteoid osteoma of the talus: a case report. Foot Ankle Int 1995; 16: 212–5
- Tuzuner S, Aydin A T. Arthroscopic removal of an osteoid osteoma at the talar neck. Arthroscopy 1998; 14: 405–9