A 50-year-old man was referred to our institute for treatment of a hard mass in the left lower leg. About 30 years previously, he had sustained a knife stabbing injury to the left thigh, resulting in a femoral artery rupture which was repaired. He had used a long leg splint for 1 month after the repair to the artery and had suffered pain and swelling of the lower leg after the application of the splint.
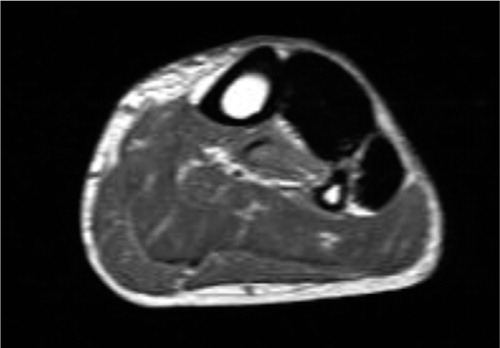
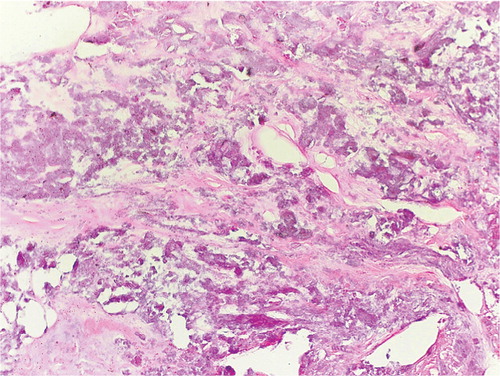
Physical examination revealed a hard mass in the anterolateral aspect of the left lower leg and stiffness of the left ankle and toes. There was numbness over the anterolateral area of the left lower leg. Radiographs showed a radiopaque mass () and MRI showed low signal intensity () in the anterior and lateral compartments of the lower leg. At surgery, the entire anterior and lateral compartments were found to be replaced with calcified material which was removed (). The wound was closed over a suction drain. A short course of prophylactic antibiotic was given and the wound healed without infection. Pathohistological examinations revealed dystrophic calcification ().
Discussion
To our knowledge, only 7 cases of massive ectopic calcification and approximately 16 cases of calcific myonecrosis of the lower limbs have been reported in the English medical literature. The calcification in calcific myonecrosis was either scattered within the necrotic muscle or peripherally around a fusiform mass (O'Keefe et al. Citation1995, Snyder et al. Citation1995, Zohman et al. Citation1998, Wang and Chen Citation2001, Holobinko et al. Citation2003). On the contrary, in our case, the entire anterior and lateral compartments were replaced by calcified material without any viable tissue.
Viau et al. (Citation1983) reported 2 cases of ectopic calcification of the lower extremities 38 and 64 years after the initial trauma, as late sequelae of compartment syndrome. Both cases were treated with incision and drainage with the wounds left open; however, secondary infection developed in both cases, resulting in amputation in one case and recurrent draining sinus in the other. The authors recommended primary wound closure over suction drainage or by needle aspiration of the mass. Österman and Lindholm (Citation1983) reported 4 cases of massive ectopic calcifications in muscles of the lower leg following nerve paralysis due to war injuries or traffic accident. One of the cases was operated and developed a Staphylococcus aureus infection of the wound cavity. Saitoh et al. (Citation2000) described a patient whose ectopic calcification was confined to the flexor hallucis longus muscle, which was resected, resulting in less toe deformity.
In all the reported cases, ectopic calcification was preceded by remote trauma to the extremity. The pathophysiological mechanism that leads to ectopic calcification of the muscle is not known. It is difficult to prove the existence of a compartment syndrome in our patient; however, compartment syndrome can occur after vascular reconstructions (Early et al. Citation1994) and he had experienced severe painful swelling of the lower leg after the femoral artery repair. Compartment syndrome results in muscle necrosis and fibrosis, and may give dystrophic calcification. If excision of the calcification is performed, we suggest primary closure of the wound over a suction drain with compressive dressing to eliminate the problem of dead space, and a short course of prophylactic antibiotic.
- Early J S, Ricketts D S, Hansen S T. Treatment of compartmental liquefaction as a late sequela of a lower limb compartment syndrome. J Orthop Trauma 1994; 8: 445–8
- Holobinko J N, Damron T A, Scerpella P R, Hojnowski L. Calcific myonecrosis: keys to early recognition. Skeletal Radiol 2003; 32: 35–40
- O'Keefe R J, O'Connell J X, Temple H T, Scully S P, Kattapuram S V, Springfield D S, Rosenberg A E, Mankin H J. Calcific Myonecrosis. A late sequela to compartment syndrome of the leg. Clin Orthop 1995, 318: 205–13
- österman K, Lindholm T S. Massive ectopic calcification of the leg following nerve injury. Arch Orthop Trauma Surg 1983; 102: 82–7
- Saitoh S, Hata Y, Murakami N, Seki H, Miyauchi S, Takaoka K. Ectopic calcification following tibial fracture: property analysis. Skeletal Radiol 2000; 29: 609–12
- Snyder B J, Oliva A, Buncke H J. Calcific myonecrosis following compartment syndrome: report of two cases, review of the literature, and recommendations for treatment. J Trauma 1995; 39(4)792–5
- Viau M R, Pedersen H E, Salciccioli G G, Manoli A II. Ectopic calcification as a late sequela of compartment syndrome. Report of two cases. Clin Orthop 1983, 176: 178– 80
- Wang J W, Chen W J. Calcific myonecrosis of the leg: a case report and review of the literature. Clin Orthop 2001, 389: 185–90
- Zohman G L, Pierce J, Chapman M W, Greenspan A, Gandour–Edwards R. Calcific myonecrosis mimicking an invasive soft-tissue neoplasm. A case report and review of the literature. J Bone Joint Surg (Am) 1998; 80: 1193–7