Abstract
Background Periacetabular osteotomy (PAO) is an effective but technically demanding surgical procedure. We evaluated the efficiency of computer-assisted navigation in PAO and compared it with the traditional approach.
Patients and methods We performed a randomized study of 36 patients undergoing PAO using either the CT-based, computer-assisted navigation technique or the conventional approach. The operative details, radiographic results, and functional outcomes were compared between groups.
Results Patients in the conventional surgery group required an average of 4.4 (2–7) images of intraoperative radiographs, whereas only 0.6 (0–1) images were required in the navigation group. The operation time was 21 min shorter with computer-assisted navigation. No significant difference with regard to operative blood loss, transfusion requirement, correction of deformity, and functional improvement was found. Complications such as intraarticular damage, osteonecrosis, or neurovascular injury were not encountered.
Interpretation A computer-assisted navigation system is a feasible tool to provide real-time image guidance and facilitate PAO. However, it offers little additional benefit when the surgery is done by an experienced surgeon.
Periacetabular osteotomy (PAO) is a well established procedure for the treatment of adult dysplastic hips. With appropriate techniques performed in properly selected patients, PAO has the potential to correct the dysplastic acetabulum, relieve pain, improve function, and to prevent osteoarthritic changes from progression (Crockarell et al. Citation1999, Trumble et al. Citation1999). Several types of PAO have been developed, and most of them are considered technically demanding (Ninomiya and Tagawa Citation1984, Ganz et al. Citation1988, Hsieh et al. Citation2003). Difficulties arise not only from the complex anatomical structures of the pelvis, but also from the limited visualization provided by traditional surgical approaches in which some of the bony cuts have to be done out of the surgeon’s field of view.
To improve the accuracy and safety of difficult orthopedic operations, computer-assisted image-guided techniques have recently been introduced (Amiot and Poulin Citation2004). These techniques—also called navigation surgery—are capable of offering real-time, three-dimensional images to track the position and orientation of surgical instruments (e.g. osteotomes) in space with respect to the patient’s anatomy. Studies have demonstrated the accuracy of these systems in several areas of orthopedic surgery (Fu et al. Citation2004, Jolles et al. Citation2004, Perlick et al. Citation2004). To date, however, there have been few reports on the application of computer-assisted techniques in PAO, and no data have been obtained demonstrating the clinical advantages of this new technology in comparison with those of conventional surgery. The purpose of this prospective study was to provide objective information regarding the outcomes of PAO using a CT-based navigation system and to compare it with that of a conventional “surgeon-controlled” approach.
Patients and methods
Study design and patients
We performed a prospective study on a consecutive series of 36 patients to evaluate the clinical outcomes of PAO using either a CT-based navigation system (the “navigated” group; n = 18) or a conventional technique (the “conventional” group; n = 18). The patients were designated randomly into groups using a table of random numbers. One surgeon (P-H H), experienced in both computer-assisted and conventional PAO, carried out all the operations between November 2002 and August 2003. The criterion for inclusion in the study was a symptomatic adult dysplastic hip that required surgical correction for better femoral head coverage and hip congruency. We considered hips with advanced osteoarthritic changes (Tönnis grade 3; severe narrowing or obliteration of the joint space) a contraindication to this type of reconstruction (Tönnis Citation1987). We also excluded hips with false acetabuli or with severe femoral head deformity that could not be corrected by PAO. All patients taking part in the study gave their informed consent, and the local institutional ethics committee approved the protocol.
Operative technique
The surgical technique of PAO have been described previously in detail (Hsieh et al. Citation2003). Briefly, the patient was placed in the lateral decubitus position under general anesthesia and the transtrochanteric approach was used to facilitate exposure. The osteotomy was completed via a single longitudinal incision approximately 20 cm long, centered over the tip of the greater trochanter. The approach permitted bony cuts done from outside of the pelvis, with simultaneous arthrotomy of the hip joint to directly assess the intraarticular pathology. The fragment was spherical in shape, which allowed easy mobilization with minimal gap formation after redirection of the acetabulum (). The goal of correction was to achieve adequate coverage of the femoral head with optimal congruency of the hip joint and femoral head coverage of < 75% (Cooperman et al. Citation1983), a lateral center-edge angle of < 25° (Wiberg Citation1939), an anterior center-edge angle of < 20° (Lequesne and de Seze Citation1961) and an acetabular angle of < 42° (Sharp Citation1961). The acetabular fragment was fixed with 3 or 4 3.5-mm cortical screws and the greater trochanter was stabilized with 2 6.5-mm cancellous screws. Because osteotomy beyond the surface of the pelvis was a blind endeavor in the “conventional” group, intraoperative radiographic images were required to ensure proper position and orientation of the blades of the osteotomes.
Computer-assisted PAO
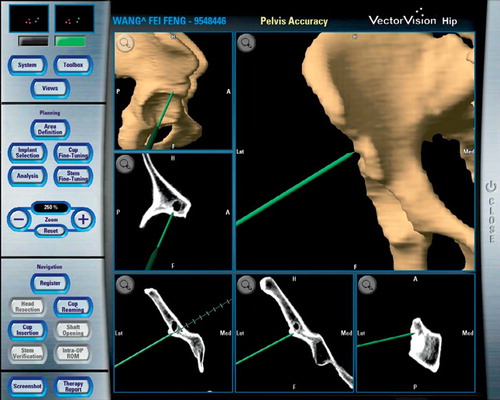
In the “navigated” group, PAO was performed using the CT-based version of BrainLAB’s VectorVision hip navigation software (BrainLAB Inc., Westchester, IL). A preoperative CT scan of the pelvis at 1-mm slice thickness was obtained in all patients according to a standard protocol. The scanned data were then transferred to a workstation to generate a high-resolution three-dimensional model of the patient’s pelvis.
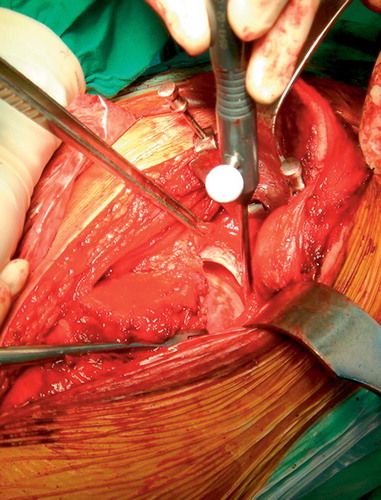
At the beginning of the operation, a reference frame was rigidly fixed to the iliac crest through a separate 1.5-cm incision (). The Brain-LAB navigation screen, along with stereo cameras, was positioned on the opposite side of the surgeon, 2 meters away from the operation table. The correlation between the preoperative image data and the patient’s anatomy was established by a surface-matching process. This step, also termed registration, was done by capturing 15–18 points on bone surface of the anterosuperior iliac spine, the iliac crest, and the acetabulum with an optically tracked probe. The surface of the acetabulum was easily visualized with capsulotomy and manual traction of the leg (). After registration, the accuracy of matching was checked by the navigation system. An error value of 2 mm was considered to be acceptable.
Figure 2. A reference frame is firmly attached to the iliac crest through a separate small incision.
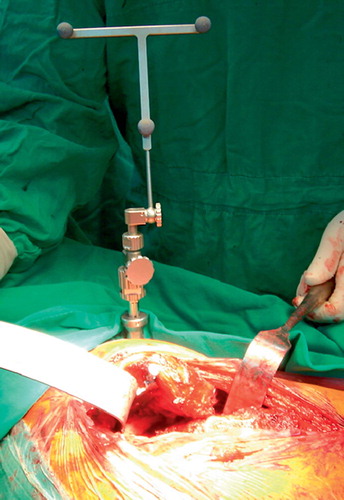
Figure 3. By manual traction of the involved leg, the acetabulum can be visualized. A probe is used to track and register the articular surface.
To incorporate conventional surgical instruments into the computer-assisted system, the existing surgical tools such as the osteotomes were equipped with a navigation adaptor. This enabled specific points of interest, for example, the blade of an osteotome, to be tracked and the position to be visualized in real-time on the navigation screen. The surgeon was then able to perform PAO with continuous, three-dimensional guidance by the navigation system ().
Evaluation
The patients followed a standard rehabilitation protocol after surgery and were examined clinically and radiographically at 3, 6, 12, and 24 months. Operative parameters, including operative time (time from incision to closure), blood loss, amount of transfusion, requirement of intraoperative radiographic images, and estimated radiation exposure of the patients were recorded. Radiographic correction of the deformity, including improvement in femoral head coverage, anterior and lateral center-to-edge (CE) angles, and the acetabular angle, was calculated on the postoperative radiographs. The hip functional scores according to the Merle d’Aubigne and Postel (1954) system were determined preoperatively and at the postoperative controls.
Statistics
We used Chi-square test for categorical data, and a two-tailed Student’s t-test for continuous data (recorded as mean (SD)). P-values less than 0.05 were considered to represent statistical significance.
Results
All patients completed the 2-year follow-up and the 2 groups were matched regarding age, sex, body weight, and side of involvement (). In the “conventional” group, an average of 4.4 (SD 1.6; range 2–7) images of intraoperative radiographs was required to perform a precise PAO while only 0.6 (SD 0.5; range 0–2) images were needed in the “navigated” group (p < 0.001). The estimated radiation exposure was higher in patients in the “conventional” group (p < 0.001). Although the “navigated” group took an extra 26 (SD 4.8; range 17–33) min in setup of the reference frame and registration, the reduced numbers of intraoperative radiographs effectively shortened the operative time for the whole procedure by 21 min. There were no significant differences between the two groups with regard to operative blood loss and the amount of transfusion (Table 2)
Table 1. Patient data, expressed as mean (SD) and range
Satisfactory radiographic correction of the deformity was achieved in all patients, regardless of the group. There were no differences between groups in terms of correction in femoral head coverage, anterior and lateral CE angles, and the acetabular angle (). Similarly, patients in both groups showed improvement in the functional score at the latest follow-up (p = 0.001 in the “navigated” group and p = 0.002 in the “conventional” group). The functional scores were, however, similar in both groups ().
Table 3. Radiographic parameters, expressed as mean (range)
Table 4. Merle d’Aubigne and Postel hip score, expressed an mean (range)
Discussion
The PAO was developed to provide correction of the poorly covered femoral head by reorientation of the dysplastic acetabulum with a series of juxtaarticular bony cuts on the pelvis. Accurate creation of the osteotomies is of paramount importance to the success of this difficult surgery, and a small degree of imprecision can lead to catastrophic failure. Intraarticular injuries, damage to the neurovascular structures, posterior column discontinuity that leads to secondary fragment migration and a fragment that is too thin (with resultant osteonecrosis) are technical errors attributable to a misplaced osteotomy (Davey and Santore Citation1999).
In the literature, only a few studies have reported the results of computer assistance of PAO. Azuma et al. (Citation1990) described a method of preoperative assessment of rotational acetabular osteotomy for dysplastic hips in children by three-dimensional surface reconstruction from CT imaging. This method provided exact anatomical information on acetabular coverage, and precise operative planning is made easier. In 2 case series, Langlotz et al. (Citation1997) and Mayman et al. (Citation2002) introduced the application of CT-based navigation technology in PAO. They concluded that the visualization aids provided by the system were capable of helping to reduce potential risk, and increase safety and accuracy. However, neither study included a comparative patient group or a prospective protocol for treatment and evaluation of patients.
Our study represents a series done by one experienced surgeon who had performed more than 120 PAO, including 10 with the computer-assisted navigation before the initiation of the study. We found that the CT-based navigation techniques offered no additional benefit over the non-computer execution of PAO when performed by an experienced surgeon. We also found no difference with regard to the operative blood loss, transfusion requirement, radiographic correction of the deformity, and the functional outcomes between the groups. Even so, it turned out that the visualization aids afforded by the computer navigation system effectively reduced the need for intraoperative radiographs by providing the surgeon with real-time feedback on the orientation of surgical instruments during this difficult operation. Even in experienced hands, the time required for the whole procedure can be shortened with use of navigation. There is a strong possibility that surgeons who have less experience in PAO would profit more from the application of this system.
The strengths of our study include a randomized design on a consecutive series of patients with complete follow-up, and the fact that one surgeon treated all patients using standard techniques. One weakness is the limited number of patients, with no statistical power to detect minor differences.
The application of computer navigation in PAO required capsulotomy for registration. Opening of the joint offers an opportunity to directly assess intraarticular pathology. However, with a thin fragment created in the rotational acetabular osteotomy (Ninomiya and Tagawa Citation1984), capsulotomy is contraindicated because this may alter blood supply to the osteotomized fragment and lead to osteonecrosis. The design of our modified PAO creates a thick fragment with its vascular supply from the inner side of the pelvis; thus, performance of a capsulotomy is permissable (Hsieh et al. Citation2003).
The computer navigation software we used is currently being used in PAO for preoperative planning, intraoperative planning, and execution of the bone cutting. Once the acetabular fragment has been osteotomized and freed from the pelvis, this version of the software looses its ability to track the fragment in space to guide the reorientation, and proper correction should rely on the surgeon’s own experience to find a new optimal position. This is thought to be a limitation of the current navigation system because only a minor failure in correction angle may lead to a change in joint mechanics (Tönnis and Heinecke Citation1999). Jäger et al. (Citation2004) described a CT-based PAO navigation system that allowed control of the acetabular fragment in 3D, complemented by readout of numerical angles on the screen.
The application of computer-assisted navigation systems in PAO requires additional time for setting up the reference frame and registration. This took as long as 60 min in the earliest cases before we started the study. In our series, however, the procedure took only 26 min after an initial learning curve, which compensated well for the time needed to acquire intraoperative radiographs in the “conventional” group.
The main disadvantages of the CT-based navigation surgery include the considerable cost to acquire the system, the need for an additional radiographic scan procedure and data transfer before surgery, and the time required for registration during surgery. Recently, applications of fiuoroscopic image-assisted technology have been developed. The fiuoroscopic navigation system allows multiple intraoperative images to be stored in the computer workstation. The system can locate the surgery-specific regional anatomy of the captured images. The position of surgical instruments can be tracked by attaching an adapter with reflective markers and then can be virtually overlaid onto the stored images in multiple planes during surgery (Bachler et al. Citation2001, Stockle et al. Citation2003). The use of the CT-free modalities eliminates the acquisition of a preoperative CT scan and the need for a registration process, yet provides accurate clinical information rivaling that of the CT-based methods and may also facilitate and speed up the surgery (Choi et al. Citation2000). Although the application of this new technology in PAO is still under investigation, the authors believe that the future of navigated PAO will involve CT-free navigation.
Although our findings support a role for CT-based navigation in PAO, it seems that the current use of this image-guided technique in PAO is often unnecessary when an experienced surgeon performs the surgery. This technology is expensive and offers only a small amount of additional benefit to the patients. Further advances in this field may soon allow real-time image guidance with fiuoroscopic tracking, which should increase the usefulness of navigation surgery in PAO.
No competing interests declared.
Contributions of authors
PHH performed the operations, collected the data and wrote the manuscript. All authors contributed to study design, data interpretation, and revision of the paper.
- Amiot L P, Poulin F. Computed tomography-based navigation for hip, knee, and spine surgery. Clin Orthop 2004, 421: 77–86
- Azuma H, Taneda H, Igarashi H, Fujiako M. Preoperative and postoperative assessment of rotational acetabular osteotomy for dysplastic hips in children by three-dimen-sional surface reconstruction computed tomography imaging. J Ped Orthop 1990; 10(1)33–8
- Bachler R, Bunke H, Nolte L P. Restricted surface matching--numerical optimization and technical evaluation. Comput Aided Surg 2001; 6(3)143–52
- Choi W W, Green B A, Levi A D. O. Computer-assisted fiuoroscopic targeting system for pedicle screw insertion. Neurosurgery 2000; 47(4)872–8
- Cooperman D R, Wallensten R, Stlberg S D. Acetabular dysplasia in the adult. Clin Orthop 1983; 175: 79–85
- Crockarell J, Jr, Trousdale R T, Cabanela M E, Berry D J. Early experience and results with the periacetabular osteotomy. The Mayo Clinic experience. Clin Orthop 1999, 363: 45–53
- Davey J P, Santore R F. Complications of periacetabular osteotomy. Clin Orthop 1999, 363: 33–7
- Fuss T S, Chen L H, Wong C B, Lai P L, Tsai T T, Niu C C, Chen W J. Computer-assisted fiuoroscopic navigation of pedicle screw insertion: an in vivo feasibility study. Acta Orthop Scand 2004; 75(6)730–5
- Ganz R, Klaue K, Vinh T S, Mast J W. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop 1988, 232: 26–36
- Hsieh P H, Shih C H, Lee P C, Yang W E, Lee Z L. A modified periacetabular osteotomy with use of the transtrochanteric exposure. J Bone Joint Surg (Am) 2003; 85(2)244–50
- Jäger M, Westhoff B, Wild A, Krauspe R. Computer-assisted periacetabular triple osteotomy for treatment of dysplasia of the hip. Z Orthop Ihre Grenzgeb 2004; 142(1)51–9
- Jolles B M, Genoud P, Hoffemeyer P. Computer-assisted cup placement techniques in total hip arthroplasty improve accuracy of placement. Clin Orthop 2004, 426: 174–9
- Langlotz F, Stucki M, Bachler R, Scheer C, Ganz R, Berlemann U, Nolte L P. The first twelve cases of computer assisted periacetabular osteotomy. Comput Aided Surg 1997; 2(6)317–26
- Lequesne M, de Seze S. Le faux profil du bassin. Nouvell incidence radiographique pour l'étude de la hanche. Son utilité dans les dysplasies et les differentes coxopathies. Rev Rhum Mal Osteoartic 1961; 28: 643–52
- Mayman D J, Rudan J, Yach J. The Kingston periacetabular osteotomy utilizing computer enhancement: a new technique. Comput Aided Surg 2002; 7(3)179–86
- Merle d'Aubigne R, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg (Am) 1954; 36: 451–5
- Ninomiya S, Tagawa H. Rotational acetabular osteotomy for the dysplastic hip. J Bone Joint Surg (Am) 1984; 66: 430–6
- Perlick L, Bathis H, Tingart M, Perlick C, Grifka J. Navigation in total-knee arthroplasty: CT-based implantation compared with the conventional technique. Acta Orthop Scand 2004; 75(4)464–70
- Sharp I K, Acetabular dysplasia. The acetabular angle. J Bone Joint Surg (Br) 1961; 43: 268–72
- Stockle U, Konig B, Schaser K, Melcher I, Haas N P. CT and fluoroscopy based navigation in pelvic surgery. Unfallchirurg 2003; 106(11)914–20
- Tönnis D. Congenital dysplasia and dislocation of the hip in children and adults. Springer, New York 1987
- Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg (Am) 1999; 81(12)1747–70
- Trumble S J, Mayo K A, Mast J W. The periacetabular osteotomy. Minimum 2 year followup in more than 100 hips. Clin Orthop 1999, 363: 54–63
- Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint. With special reference to the complication of osteoarthritis. Acta Chir Scand (Suppl 58) 1939; 83: 1–35