Abstract
Background The results of total hip arthroplasty (THA) in young patients with rheumatoid arthritis (RA) have been reported in only a few studies. On a nationwide level, the outcome of THA in these patients is unknown. We evaluated the population-based survival of THA in patients under 55 years of age with RA and factors affecting the survival.
Patients Between 1980 and 2003, 2,557 primary THAs performed for RA in patients less than 55 years of age were reported to the Finnish Arthroplasty Register.
Results Proximally circumferentially porous-coated uncemented stems had a 15-year survival rate of 89% (95% CI 83–94) with aseptic loosening as endpoint. The risk of stem revision due to aseptic loosening was higher with cemented stems than with proximally porouscoated uncemented stems implanted during the same period (RR 2.4; p < 0.001). In contrast, Cox regression analysis showed that the risk of cup revision was significantly higher for all uncemented cup concepts than for all-polyethylene cemented cups with any cup revision as endpoint. There were no significant differences in survival between the THR concepts.
Interpretations Uncemented proximally circumferentially porous-coated stems and cemented all-poly-ethylene cups are currently the implants of choice for young patients with RA.
In young patients with rheumatoid arthritis (RA), good results have been reported with both uncemented (Keisu et al. Citation2001, Lyback et al. Citation2004) and cemented (Lehtimaki et al. Citation1997, Creighton et al. Citation1998, Lehtimaki et al. Citation1999) femoral components. Loosening of the acetabular component, however, remains a major long-term problem after total hip arthroplasty (THA) in patients with RA (Katsimihas et al. Citation2003). A few register-based studies have reported the results of THA in young patients at the population level (Havelin et al. Citation2000, Malchau et al. Citation2002, Eskelinen et al. Citation2005). To our knowledge, however, no comprehensive nationwide results of THA in young patients (< 55 years) with RA have been published.
We investigated the outcome of THA for RA in patients under 55 years of age from the Finnish Arthroplasty Register.
Patients and methods
Our study is based on information recorded in the Finnish Arthroplasty Register (Paavolainen et al. Citation1991, Puolakka et al. Citation2001b) in patients who underwent THA between 1980 and 2003. The register holds information on 92,083 THAs, each of which has been recorded individually for all patients treated since the register was established. An English translation of the form used for this purpose has been discussed previously (Puolakka et al. Citation2001b). Revisions were linked to the primary operation using the unique personal identification number assigned to each resident of Finland.
Inclusion criteria
During the whole study period (1980–2003), 92,083 primary THAs were performed in Finland. Of these operations, 12,601 (14%) were performed on patients under 55 years of age and RA was the indication in 20% (n 2,557) of these THAs. These 2,557 THAs (1,893 patients) were therefore included in the final analysis. Of the 1,893 patients involved, 35% (n 664) were bilaterally operated while under the age of 55. The median duration of follow-up was 9.7 (0–24) years.
Primary operation
Implant concepts.
The sex, age and personal identification number of the patients and the side affected had been recorded for all primary operations. The number and percentage of different implants used in the operations and the fixation method of each component (cemented or uncemented) were evaluated.
The success rate of different implant concepts was analyzed. For statistical comparisons, stems and cups were divided into 4 groups, and THRs into 3 groups. Stems were classified as uncemented proximally circumferentially porous-coated, uncemented proximally circumferentially HA-coated, uncemented uncoated (including isoelastic, gritblasted and sand-blasted uncemented stems) and cemented (including polished, grit-blasted and sand-blasted cemented stems). Cups were classified as uncemented porous-coated press-fit, uncemented HA-coated press-fit, uncemented smooththreaded and cemented all-polyethylene. THRs were classified as press-fit porous-coated uncemented (proximally porous-coated uncemented stem and press-fit porous-coated uncemented cup), press-fit HA-coated uncemented (proximally HAcoated uncemented stem and press-fit HA-coated uncemented cup) and cemented (cemented stem and cemented all-polyethylene cup). Only implant designs used in 10 or more operations over the whole study period were included in the concept analysis (Appendix 1).
Revision operation.
For a revision arthroplasty the date of the index operation, the design of the revised prosthesis, and the indication for revision were recorded. Indications for revision and the revision burden (expressed as a percentage by dividing the number of revisions done over a certain period by the total number of primary and revision THAs performed over the same period) were analyzed.
Statistics
The endpoint for survival was defined as revision when either one component or the whole implant was removed or exchanged. Both revision for any reason (including exchange of liner) and aseptic loosening served as endpoints. Aseptic loosening was considered as a separate endpoint, because “revision for any reason” included non-implant-related reoperations. Kaplan-Meier survival data were used to construct the survival probabilities of implants at 7, 10, and 15 years. Survival data obtained by Kaplan-Meier analysis were compared by the log-rank test. The Cox multiple-regression model was used to study differences between groups and to adjust for potential confounding factors. The factors studied with the Cox model were: implant concepts, age group (≤ 45 and 46–54 years) and sex. All models included adjustment for differences in age (≤ 45 and 46–54 years) and sex. When the effect of age and sex on implant survival was analyzed with the Cox model, adjustment was also made for implant concepts (Furnes et al. Citation2001). Cox regression analyses provided estimates of survival probabilities and revision risk ratios (RR) for different factors. Estimates from Cox analyses were used to construct adjusted survival curves at mean values of the risk factors. The Wald test was applied to calculate p-values for data obtained from the Cox multiple regression analysis. Differences between groups were considered to be statistically significant if the p-values were less than 0.05 in a two-tailed test. The statistical analyses were done with SPSS software version 12.0.1.
Results
Primary operation
Patient characteristics
Of the 2,557 THAs, 1293 (51%) were performed in patients aged 46–54 years and the rest in patients aged 45 years or younger. Of all THAs, 1,331 (52%) were performed on the right hip. 1,889 (74%) of the patients were females.
The number of hospitals performing THAs for RA on younger patients rose from 19 at the beginning of the period (1980–1981) to 32 in the early years of the next decade (1991–1992), and remained at this level to the end of the study period (2002–2003). Over the whole study period, only 1 hospital (run by a private foundation) performed more than 20 THAs annually on patients with RA. During the last period analyzed (2002–2003), 6 of the 32 hospitals included in the study performed more than 20 THAs annually on patients with RA.
Femoral components ().
Over the whole study period, 71 different femoral components were used, three-quarters (52/71) of them in fewer than 20 operations. 60% of the stems were uncemented. At the end of the study period (2002–2003), the 3 most common stem brands (Bi-Metric, ABG II, and Exeter Universal) accounted for 70% of all stems implanted. The proportion of uncemented stems rose dramatically from the beginning of the study to the early 1990s.
Table 1a. Trends in cementation of femoral and acetabular components implanted in three time periods
Table 1b. The most common femoral and acetabular components implanted in three time periods
Acetabular components ().
During 1980– 2003, 83 different acetabular components were used, three-quarters (60/83) of them in fewer than 20 operations. 82% of the cups were uncemented. At the end of the study period (2002–2003), the 3 most common cup brands (ABG II, Biomet Vision, and Biomet M38) constituted 46% of all cups. The proportion of uncemented cups also rose markedly between the beginning of the study period and the early 1990s, but cemented cups have gained popularity again in the early years of the 21st century.
Revision operation.
During 1980–2003, 605 THA revision operations were performed in patients who had undergone THA for RA at an age younger than 55 years. Thus, the revision burden was 19% for the whole follow-up period. The most common reason for revision was aseptic loosening, which accounted for 82% (n 494) of operations. This was followed by prosthesis dislocation, which accounted for 3.3% (n 20) of revisions. Infection was the reason for revision in 2.8% (n 17) of cases and periprosthetic fracture in 1.8% (n 11) of cases. Fracture of the stem accounted for 1.2% (n 7) of operations and malposition of the prosthesis for 1.0% (n 6) of operations. Other, miscellaneous reasons (including exchange of liner) accounted for 8.3% (n 50) of revisions.
Follow-up results of all primary operations (Table 2)
Stem concepts.
When the whole study period was analyzed, all stem concepts showed < 90% survival rates at 7 years with aseptic loosening as endpoint. At 15 years, the survival rate for proximally porous-coated stems was still 89% (95% CI 83–94), and that of cemented stems 84% (95% CI 81–87); at the same time, the survival rate of uncoated stems had declined to 71% (95% CI 63– 79). Cox regression analysis (with adjustment for age and sex) showed that proximally porous-coated uncemented stems had a significantly lower risk of revision than cemented stems (RR 0.4, 95% CI 0.3–0.6; p < 0.001). Uncoated uncemented stems, in contrast, showed a 1.7-fold (95% CI 1.2–2.5; p = 0.002) increased risk of revision as compared to cemented stems (). In the Cox regression model, the survival of proximally porous-coated uncemented stems was already better than that of cemented stems during the first 7 years of follow up. Even after 7 years of follow-up, there was a trend for porous-coated stems to perform better than cemented ones.
Figure 1. Cox-adjusted survival curves of 2,232 stems, with stem concept as the strata factor. Endpoint was defined as stem revision due to aseptic loosening. Adjustment was made for age and sex.
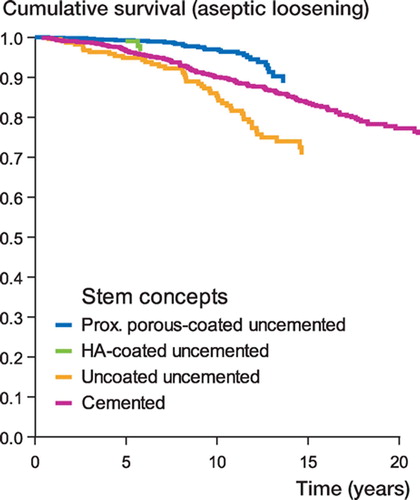
With stem revision for any reason as endpoint, only proximally porous-coated uncemented stems showed a < 90% survival rate at 10 years (). In the Cox model, proximally porous-coated uncemented stems were found to have a 0.5-fold (95% CI 0.4–0.8; p = 0.01) reduced risk of stem revision and uncoated uncemented stems a 1.9-fold (95% CI 1.4–2.6; p < 0.001) increased risk of stem revision as compared to cemented stems.
Table 2a. Survival of stem concepts. Endpoint defined as revision due to aseptic loosening of the stem. 7-, 10-, and 15-year survival rates obtained from the Kaplan-Meier analysis
Table 2b. Survival of stem concepts. Endpoint defined as any stem revision. 7-, 10-, and 15-year survival rates obtained from the Kaplan-Meier analysis
Cohort effect among stem concepts.
Cox regression analysis did not reveal any differences in stem concept survival between the cohorts of 1980–1991 and 1992–2003.
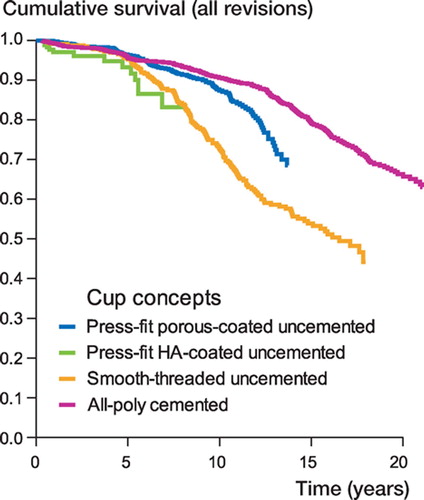
Cup concepts (Table 3)
With aseptic loosening as endpoint, all cup concepts except smooth-threaded uncemented cups showed survival rates of 95% at 7 years. At 15 years, the survival rate of all cup concepts had declined to < 85%. In the Cox regression analysis, smooththreaded cups showed a significantly higher risk of revision (RR 2.7, 95% CI 2.1–3.5; p < 0.001) than all-polyethylene cemented cups ().
Figure 2. Cox-adjusted survival curves calculated for 2,151 cups, with cup concept as the strata factor. Endpoint was defined as cup revision due to aseptic loosening. Adjustment was made for age and sex.
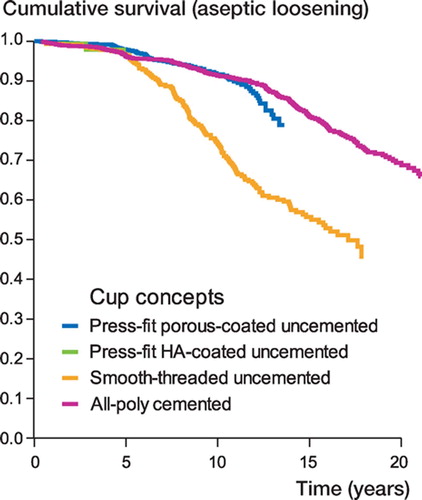
Table 3a. Survival of cup concepts. Endpoint defined as revision due to aseptic loosening of the cup. 7-, 10-, and 15-year survival rates obtained from the Kaplan-Meier analysis
Table 3b. Survival of cup concepts. Endpoint defined as revision due to any cup revision. 7-, 10-, and 15-year vival rates obtained from the Kaplan-Meier analysis
With any cup revision as endpoint, only press-fit porous-coated uncemented cups and all-polyeth-ylene cemented cups showed < 90% survival rates at 7 years. Later, however, the 15-year survival rate of press-fit porous-coated cups declined to < 70%. Smooth-threaded uncemented cups showed an extremely poor survival rate of only 53% at 15 years. In the Cox regression analysis, other cup concepts showed an increased risk of revision as compared to all-polyethylene cemented cups (). Whereas the survival of porous-coated uncemented cups started to decline after 7 years of follow-up, the survival of HA-coated uncemented cups was already poorer than that of all-polyethylene cemented cups during the first 7 years of follow-up.
Cohort effect among cup concepts
In the Cox regression analysis, press-fit porouscoated uncemented cups implanted during 1992– 2003 had a significantly reduced risk of revision compared to cups of the same concept implanted during 1980–1991 with either aseptic loosening or all revisions as endpoint (aseptic loosening, p < 0.001; all revisions, p = 0.03). All-polyethyl-ene cemented cups did not show any significant difference in survival rates between the cohorts of 1980–1991 and 1992–2003.
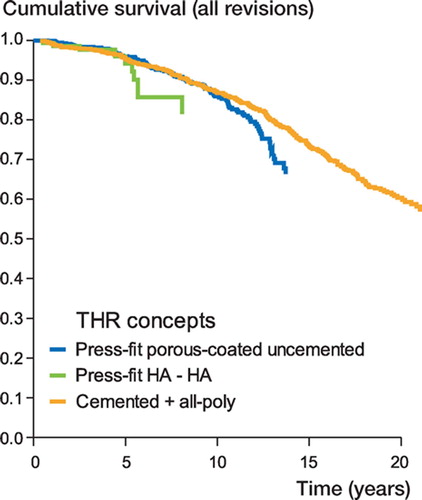
Total hip replacement concepts (Table 4)
With aseptic loosening as endpoint, all THR concepts showed < 90% survival rates at 7 years (). At 15 years, however, the survival rates of both press-fit porous-coated uncemented and cemented THRs had declined to < 80%. In the Cox model, there were no differences in survival between the THR concepts—either during the first 7 years or after 7 years of follow-up.
Table 4a. Survival of THR concepts. Endpoint defined as revision due to aseptic loosening of the stem and/or the cup. 7-, 10-, and 15-year survival rates obtained from the Kaplan-Meier analysis
Table 4b. Survival of THR concepts. Endpoint defined as any revision. 7-, 10-, and 15-year survival rates obtained from the Kaplan-Meier analysis
With all revisions as endpoint, all THR concepts showed ≥ 85% survival rates at 7 years. The survival rates of both press-fit porous-coated uncemented and cemented THRs had declined to < 75% at 15 years (). In the Cox model, there was a trend for poorer survival of porouscoated uncemented THRs than of cemented THRs after 7 years of follow-up, but the difference was not statistically significant (p = 0.05). There was also a trend for poorer overall survival of HAcoated uncemented THRs than of cemented THRs; this difference, however, also lacked statistical significance (p = 0.09).
Sex and age as risk factors
Cox regression analysis of the total data did not reveal any difference in revision risk between sexes when either all revisions or aseptic loosening served as endpoint (with or without adjustment for age and implant concepts). When the risk of stem revision was analyzed with the Cox model, there was a trend towards a greater risk of stem revision in males than in females with adjustment for age and stem concepts (aseptic loosening, p = 0.06; any stem revision, p = 0.05). Analysis of cup revisions suggested that there was no difference in revision risk between genders when either all cup revisions or aseptic loosening served as endpoint (with or without adjustment for age and cup concepts).
With aseptic loosening as endpoint, there was no difference in revision risk between the age groups (with or without adjustment for sex and stem concepts). With any revision as endpoint, younger patients (< 46 years) were found to have a 1.2-fold (95% CI 1.0–1.5; p = 0.03) increased risk of revision as compared to older patients (46–54 years) (with adjustment for sex and implant concepts). When the risk of stem revision was analyzed with the Cox model, there was no significant difference in revision risk between the age groups with either all revisions or aseptic loosening as endpoint (with or without adjustment for sex and stem concepts). However, the younger age group had a higher risk of cup revision than the older age group when either all revisions (RR 1.3, 95% CI 1.1–1.6; p = 0.005) or aseptic loosening (RR 1.3, 95% CI 1.1–1.7; p = 0.008) served as endpoint (with adjustment for sex and cup concepts).
Discussion
The purpose of this study was to evaluate the nationwide results of the most commonly used THR concepts in younger patients with RA in Finland. We found that modern, second-generation uncemented stems with proximal circumferential porous coating provided young RA patients with good longterm survival. Uncemented cups, irrespective of the cup concept, had higher rates of revision than cemented all-polyethylene cups. Problems still clearly arise with polyethylene wear and periprosthetic osteolysis in modern uncemented acetabular components (Harris Citation2003).
. Cox-adjusted survival curves calculated for 1,545 THRs, with THR concept as the strata factor. Endpoint was defined as any revision. Adjustment was made for age and sex.
We acknowledge that the current register-based study has certain limitations. We were not, for example, able to report any subjective outcome measurements on the basis of the Harris hip score or disease-specific quality-of-life questionnaires. Moreover, in register-based analyses involving thousands of patients it is not possible to conduct radiographic analyses—with the result that silent osteolysis, for example, cannot be detected. Nevertheless, register-based studies provide valuable insight into the use of the THA procedure in a particular group of patients, as the number of arthroplasties studied is usually significantly higher in such studies than in clinical studies from single centers. Furthermore, the results can be compared with those from other Nordic arthroplasty registers, which provides a wider view of the results for single implants and also the methods used in THA (Havelin et al. Citation2000, Puolakka et al. Citation2001b, Malchau et al. Citation2002). We used statistical methods to take account of confounding factors (Furnes et al. Citation2001).
In our study, most patients undergoing THA for RA were females, as also noted elsewhere (Creighton et al. Citation1998, Lehtimaki et al. Citation1999, Keisu et al. Citation2001).
A wide range of femoral and acetabular components was used by Finnish orthopedic surgeons for patients with RA during 1980–2003. Over 70% of the brands of implant were used in fewer than 20 operations, however. Similar results have been reported from Norway (Havelin et al. Citation2000). We mainly attribute this phenomenon to commercial influence of orthopedic surgeons. At the end of the study period (2002–2003), the 3 most common and well-documented brands of stem constituted 70% of all stems implanted. With cups, however, the situation was still not optimal, the 3 most common cups accounting for less than 50% of all cups implanted. This may reflect the problem of acetabular component loosening encountered in patients with RA, and the search for the best acetabular solution still goes on.
The risk of deep infection in THA has been reported to be higher in patients with RA than in those with primary OA (Wymenga et al. Citation1992). In our series, however, the number of revision operations due to deep infection performed in patients with RA was no higher than that in patients with primary OA from the same register (Eskelinen et al. Citation2005).
Cemented THA has traditionally been considered the gold standard for the treatment of endstage joint disease due to RA (Colville and Raunio Citation1978, Poss et al. Citation1984). However, the rate of aseptic loosening of acetabular components has been high with that concept, and there have also been reports of femoral component loosening. Poss et al. (Citation1984) documented a 78% incidence of increasing radiolucency around cemented acetabular components in RA 6–11 years after surgery, even though none had been revised. A greater incidence of both acetabular and femoral loosening has been reported in patients with RA than in those with OA (Ranawat et al. Citation1980, Poss et al. Citation1984, Lachiewicz et al. Citation1986) This finding may be attributed to periarticular osteopenia, which has been associated with inactivity, medication (steroid and antimetabolites), regional hyperemia, and increased bone turnover (Bogoch and Moran Citation1999).
Good results have been reported for both uncemented (Keisu et al. Citation2001, Lyback et al. Citation2004) and cemented (Lehtimaki et al. Citation1997, Creighton et al. Citation1998, Lehtimaki et al. Citation1999) femoral components in young patients with RA. In Finland, Lybäck and colleagues (2004) reported a 100% 10-year survival rate (with aseptic loosening as endpoint) for the proximally circumferentially porous-coated Bi-Metric stem in 55 patients with juvenile chronic arthritis (mean age 28 years). Keisu et al. (Citation2001) reported a 100% survival rate for another proximally circumferentially porous-coated uncemented stem brand (Biomet Taperloc) at a mean follow-up of 8 years in patients with RA. What is more, in their series there were no signs of radiographic loosening of the stem.
In Finland, in a series of 1,553 consecutive Charnley low-friction arthroplasties (LFA) in 1,086 patients with RA, Lehtimäki and co-workers (1999) reported a 90% survival rate for the femoral component at 15 years. In another study of Charnley LFA in patients with juvenile chronic arthritis, Lehtimäki and colleagues (1997) reported a 92% survival rate for the femoral component at 15 years. On a nationwide basis, however, the results for proximally circumferentially porous-coated stems seem to be better than those for cemented stems. It appears that modern, proximally porouscoated stems achieve good primary stability and that osseointegration takes place even in patients with poorer bone-stock, such as in RA, thus providing young patients with good long-term results. It is possible, however, that when an acetabular revision is performed and the stem is found to be well-fixed, a cemented stem might become revised more easily than an uncemented one. In a regis-ter-based study, however, this possibility cannot be directly analyzed or excluded.
In the literature, the results of cemented stem fixation with a modern, third-generation cementing technique have been markedly better than the results of fixation with first-generation techniques (Sarmiento et al. Citation1990, Morscher Citation1992). Despite the improved cementing technique used and the systematic instruction of Finnish orthopedic trainees in modern, third-generation cementing techniques during the 1990s, the results for cemented stems did not improve significantly from the 1980s to the 1990s in our young patients with RA. Similar results were obtained in young patients with primary osteoarthritis from the Finnish Arthroplasty Register (Eskelinen et al. Citation2005). The reason for this somewhat confiicting finding remains unclear.
Loosening of the acetabular component remains the most serious long-term problem after THA in patients with RA. As a possible solution to the problem of mechanical loosening, porous-coated cups were introduced in the mid-1980s. Initially, encouraging results were reported by some authors. Morscher (Citation1992) suggested that his uncemented hemispheric cups with molded polyethylene inlay were superior to cemented cups or to other types of uncemented cup, especially in osteopenic patients with RA. In contrast, in a study comparing cemented and uncemented cups in RA, Kirk and coworkers (Citation1993) found no difference in clinical outcome between the 2 groups. In our study, the survival of press-fit porous-coated uncemented cups was no better than that of cemented cups with aseptic loosening as endpoint. Furthermore, when all revisions (including exchange of the polyethylene liner) were taken into account, the survival of uncemented cups was even significantly poorer than that of all-polyethylene cemented ones. In our series, the number of Morscher cups was so low that they were not included in the concept analysis.
The cup/liner incongruity of the two-piece acetabular designs seems to be a common denominator in most brands (Barrack et al. Citation1997, Malchau et al. Citation1997, Puolakka et al. Citation2001a, Young et al. Citation2002, Blacha Citation2004, von Schewelov et al. Citation2004). This problem is accentuated in our study because of the large proportion of Biomet cups. The critical problems encountered with the HexLoc liner have been reported previously from the Finnish Arthroplasty Register (Puolakka et al. Citation1999). The Biomet Vision cup, which has a closed metallic shell of titanium alloy with plasma-sprayed porous coating (plugged screw holes) and a RingLoc liner, was introduced in Finland in 1994. An earlier study documented excellent short-term results with the Biomet Vision cup in young osteoarthritic patients (Eskelinen et al. Citation2006). Still, a longer follow-up time is required to establish whether the Vision cup with a modern uncemented cup concept and a Ringloc liner produces less wear and osteolysis than the first generation of modular uncemented cups. Note that, in our study, press-fit porous-coated uncemented cups were the only concept to show a positive cohort effect, the survival rate for cups implanted during 1992–2003 being higher than that for cups implanted in 1980–1991.
The results for smooth-threaded uncemented cups were catastrophic, which is in accordance with several previous reports (Engh et al. Citation1990, Tallroth et al. Citation1993, Simank et al. Citation1997).
Good mid-term results have been reported for an HA-coated press-fit uncemented acetabular component (Tonino and Rahmy Citation2000, Giannikas et al. Citation2002). Giannikas et al. (Citation2002) published good medium-term results with the uncemented press-fit HA-coated ABG hip but expressed concern about the polyethylene wear of the acetabular insert. In addition, alarming wear and periacetabular osteolysis of the ABG I cup has been reported recently (Duffy et al. Citation2004). In a recent study of 56 patients with an average age of 44 years, Blacha (Citation2004) reported poor results with the ABG I cup, the 9-year survival rate for the cup being 69%, and 59% for the polyethylene liner. The results of our nationwide study support the latter findings: the results for HA-coated uncemented cups were less good than those for cemented cups, even in the short term, when all revisions (including exchange of liner) had been taken into account. To our knowledge, no other clinical or register-based reports have been published on HA-coated uncemented implants in young patients with RA. The findings were similar when younger patients with primary OA were analyzed from the same register (Eskelinen et al. Citation2005). Åkesson and co-workers (Citation1994) have shown that the greater bone turnover in the acetabulum than in the femur may contribute to the higher rate of acetabular component migration and loosening after THA in RA.
In our study, uncemented THR concepts performed no better than the cemented concept. In fact, there was a trend for better results with the cemented THR concept when all revisions were taken into account. With the press-fit porouscoated THR concept, this trend appeared after 7 years of follow-up, which can be attributed mainly to the increased number of liner revisions. What gives cause for concern is that the press-fit HAcoated concept showed a trend of poorer survival during the first 7 years of follow-up. Numerous cup (liner) revisions of the HA-coated cups drastically worsened the results of the press-fit HA-coated concept. In the light of the results of different stem and cup concepts found here, we ask whether a reverse hybrid THR (a proximally circumferentially porous-coated stem and an all-polyethylene cemented cup) might be the solution for young patients with RA. The number of hybrid THRs in our series was too small for valid comparisons, however.
In two large clinical studies, male sex increased the risk of stem revision (Hozack and Rothman Citation1990, Lehtimaki et al. Citation1999). Our study also revealed a trend toward poorer stem survival in males than in females. Men may apply more powerful torque forces to the femoral component, leading to aseptic loosening of the stem. This may partially explain the difference in stem survival between sexes. Our recent nationwide study showed that female osteoarthritic patients had a higher risk of cup revision than male patients (Eskelinen et al. Citation2005). In the present study, however, there was no sex difference in this respect. The reason for this phenomenon remains unclear. It has been well-documented that young age is a risk factor for cup revision, both in patients with RA (Lehtimaki et al. Citation1999) and in those with primary OA (Eskelinen et al. Citation2005). Apparently, young and active patients stress their hip joints more than older patients, increasing the risk of aseptic loosening of the cup.
In conclusion, the outcome of THA depends on many factors including component design, patient selection, and surgical technique. Particulate debris from polyethylene wear and the resulting osteolysis remain the primary factors limiting the longevity of the hip prosthesis (Harris Citation2003). In our large nationwide series, proximally circumferentially porous-coated stems performed better than cemented stems. Accordingly, our findings suggest that the modern, second-generation uncemented stems with proximal circumferential porous coating are a good choice for young patients with RA. On the contrary, uncemented cups do not seem to have any better resistance to aseptic loosening than cemented ones in young patients with RA. Moreover, cup/liner incongruity and back-side wear problems must be resolved if the possible benefits to be gained from porous-coated modular cup designs are not to be lost (Engh et al. Citation1990, McAuley et al. Citation2004). Highly cross-linked polyethylene and optional surface bearings such as ceramic and metal-on-metal articulations may reduce wear and improve the results for uncemented cups. Longterm results will be required, however, to allow us to conclude whether or not they provide a solution to the wear problem.
This study was supported by the Research Foundation of Orion Corporation, Ortopedian ja traumatologian tutkimussäätiö (the Research Foundation of Orthopedics and Traumatology), the Instrumentarium Research Foundation, the Duodecim Foundation, and the Pär Slätis Joint Surgery Research Foundation. The authors thank all orthopedic surgeons in Finland for their assistance with the Arthroplasty Register.
No conflict of interests declared.
Contributions of authors
AE participated in the design of the study, in data analysis and in writing of the manuscript. PPa, IH and VR contributed to the study design and writing of the manuscript. PPu was the statistical supervisor of the Finnish Arthroplasty Register and also performed data analysis.
- Åkesson K, Onsten I, Obrant K J. Periarticular bone in rheumatoid arthritis versus arthrosis. Histomorphometry in 103 hip biopsies. Acta Orthop Scand 1994; 65: 135–8
- Barrack R L, Folgueras A, Munn B, Tvetden D, Sharkey P. Pelvic lysis and polyethylene wear at 5-8 years in an uncemented total hip. Clin Orthop 1997; 211–7, [nr?]:
- Blacha J. High osteolysis and revision rate with the hydroxyapatite-coated ABG hip prostheses: 65 hips in 56 young patients followed for 5-9 years. Acta Orthop Scand 2004; 75: 276–82
- Bogoch E R, Moran E L. Bone abnormalities in the surgical treatment of patients with rheumatoid arthritis. Clin Orthop 1999, 366: 8–21
- Colville J, Raunio P. Charnley low-friction arthroplasties of the hip in rheumatoid arthritis. A study of the complications and results of 378 arthroplasties. J Bone Joint Surg(Br) 1978; 60: 498–503
- Creighton M G, Callaghan J J, Olejniczak J P, Johnston R C. Total hip arthroplasty with cement in patients who have rheumatoid arthritis. A minimum ten-year follow-up study. J Bone Joint Surg (Am) 1998; 80: 1439–46
- Duffy P, Sher J L, Partington P F. Premature wear and osteolysis in an HA-coated, uncemented total hip arthroplasty. J Bone Joint Surg (Br) 2004; 86: 34–8
- Engh C A, Griffin W L, Marx C L. Cementless acetabular components. J Bone Joint Surg (Br) 1990; 72: 53–9
- Eskelinen A, Remes V, Helenius I, Pulkkinen P, Nevalainen J, Paavolainen P. Total hip arthroplasty for primary osteoarthrosis in younger patients in the Finnish arthroplasty register. 4,661 primary replacements followed for 0-22 years. Acta Orthop 2005; 76: 28–41
- Eskelinen A, Remes V, Helenius I, Pulkkinen P, Nevalainen J, Paavolainen P. Uncemented total hip arthroplasty for primary osteoarthritis in young patients. A mid- to longterm follow-up study from the Finnish Arthroplasty Register. Acta Orthop 2006; 77: 57–70
- Furnes O, Lie S A, Espehaug B, Vollset S E, Engesaeter L B, Havelin L I. Hip disease and the prognosis of total hip replacements. A review of 53,698 primary total hip replacements reported to the Norwegian Arthroplasty Register 1987-99. J Bone Joint Surg (Br) 2001; 83: 579–86
- Giannikas K A, Din R, Sadiq S, Dunningham T H. Mediumterm results of the ABG total hip arthroplasty in young patients. J Arthroplasty 2002; 17: 184–8
- Harris W H. Results of uncemented cups: a critical appraisal at 15 years. Clin Orthop 2003, 417: 121–5
- Havelin L I, Engesaeter L B, Espehaug B, Furnes O, Lie S A, Vollset S E. The Norwegian Arthroplasty Register: 11 years and 73,000 arthroplasties. Acta Orthop Scand 2000; 71: 337–53
- Hozack W J, Rothman R H. Long-term survival of the Charnley low-friction total hip arthroplasty. Semin Arthroplasty 1990; 1: 3–6
- Katsimihas M, Taylor A H, Lee M B, Sarangi P P, Learmonth I D. Cementless acetabular replacement in patients with rheumatoid arthritis: a 6- to 14-year prospective study. J Arthroplasty 2003; 18: 16–22
- Keisu K S, Orozco F, McCallum J D, 3rd, Bissett G, Hozack W J, Sharkey P F, Rothman R H. Cementless femoral fixation in the rheumatoid patient undergoing total hip arthroplasty: minimum 5-year results. J Arthroplasty 2001; 16: 415–21
- Kirk P G, Rorabeck C H, Bourne R B, Burkart B. Total hip arthroplasty in rheumatoid arthritis: comparison of cemented and uncemented implants. Can J Surg 1993; 36: 229–32
- Lachiewicz P F, McCaskill B, Inglis A, Ranawat C S, Rosenstein B D. Total hip arthroplasty in juvenile rheumatoid arthritis. Two to eleven-year results. J Bone Joint Surg(Am) 1986; 68: 502–8
- Lehtimaki M Y, Lehto M U, Kautiainen H, Savolainen H A, Hamalainen M M. Survivorship of the Charnley total hip arthroplasty in juvenile chronic arthritis. A follow-up of 186 cases for 22 years. J Bone Joint Surg (Br) 1997; 79: 792–5
- Lehtimaki M Y, Kautiainen H, Lehto U K, Hamalainen M M. Charnley low-friction arthroplasty in rheumatoid patients: a survival study up to 20 years. J Arthroplasty 1999; 14: 657–61
- Lyback C C, Lyback C O, Kyro A, Kautiainen H J, Belt E A. Survival of Bi-Metric femoral stems in 77 total hip arthroplasties for juvenile chronic arthritis. Int Orthop 2004; 28: 357–61
- Malchau H, Wang Y X, Kärrholm J, Herberts P. Scandinavian multicenter porous coated anatomic total hip arthroplasty study. Clinical and radiographic results with 7- to 10-year follow-up evaluation. J Arthroplasty 1997; 12: 133–48
- Malchau H, Herberts P, Eisler T, Garellick G, Soderman P. The Swedish Total Hip Replacement Register. J Bone Joint Surg (Am) 2002; 84(Suppl 2)2–20
- McAuley J P, Szuszczewicz E S, Young A, Engh C A, Sr. Total hip arthroplasty in patients 50 years and younger. Clin Orthop 2004, 418: 119–25
- Morscher E W. Current status of acetabular fixation in primary total hip arthroplasty. Clin Orthop 1992, 274: 172–93
- Paavolainen P, Hamalainen M, Mustonen H, Slätis P. Registration of arthroplasties in Finland. A nationwide prospective project. Acta Orthop Scand 1991, Suppl 241: 27–30
- Poss R, Maloney J P, Ewald F C, Thomas W H, Batte N J, Hartness C, Sledge C B. Six- to 11-year results of total hip arthroplasty in rheumatoid arthritis. Clin Orthop 1984, 182: 109–16
- Puolakka T J, Pajamaki K J, Pulkkinen P O, Nevalainen J K. Poor survival of cementless Biomet total hip: a report on 1,047 hips from the Finnish Arthroplasty Register. Acta Orthop Scand 1999; 70: 425–9
- Puolakka T J, Laine H J, Moilanen T P, Koivisto A M, Pajamaki K J. Alarming wear of the first-generation polyethylene liner of the cementless porous-coated Biomet Universal cup: 107 hips followed for mean 6 years. Acta Orthop Scand 2001a; 72: 1–7
- Puolakka T J, Pajamaki K J, Halonen P J, Pulkkinen P O, Paavolainen P, Nevalainen J K. The Finnish Arthroplasty Register: report of the hip register. Acta Orthop Scand 2001b; 72: 433–41
- Ranawat C S, Dorr L D, Inglis A E. Total hip arthroplasty in protrusio acetabuli of rheumatoid arthritis. J Bone Joint Surg (Am) 1980; 62: 1059–65
- Sarmiento A, Ebramzadeh E, Gogan W J, McKellop H A. Total hip arthroplasty with cement. A long-term radiographic analysis in patients who are older than fifty and younger than fifty years. J Bone Joint Surg (Am) 1990; 72: 1470–6
- Simank H G, Brocai D R, Reiser D, Thomsen M, Sabo D, Lukoschek M. Middle-term results of threaded acetabular cups. High failure rates five years after surgery. J Bone Joint Surg (Br) 1997; 79: 366–70
- Tallroth K, Slätis P, Ylinen P, Paavolainen P, Paavilainen T. Loosening of threaded acetabular components. Radiographic manifestations. J Arthroplasty 1993; 8: 581–4
- Tonino A J, Rahmy A I. The hydroxyapatite-ABG hip system: 5- to 7-year results from an international multicentre study. The International ABG Study Group. J Arthroplasty 2000; 15: 274–82
- von Schewelov T, Sanzen L, Önsten I, Carlsson A. Catastrophic failure of an uncemented acetabular component due to high wear and osteolysis: an analysis of 154 omni-fit prostheses with mean 6-year follow-up. Acta Orthop Scand 2004; 75: 283–94
- Wymenga A B, van Horn J R, Theeuwes A, Muytjens H L, Slooff T J. Perioperative factors associated with septic arthritis after arthroplasty. Prospective multicenter study of 362 knee and 2,651 hip operations. Acta Orthop Scand 1992; 63: 665–71
- Young A M, Sychterz C J, Hopper R H, Jr., Engh C A. Effect of acetabular modularity on polyethylene wear and osteolysis in total hip arthroplasty. J Bone Joint Surg (Am) 2002; 84: 58–63
Appendix. Implant designs included in the concept analysis