Abstract
Background Poor bone stock in patients with osteonecrosis of the femoral head may be a reason for poor outcome after hip replacement. One way of studying bone quality is to measure implant migration. We thus investigated the clinical and radiographic results of cementless THR in younger patients with femoral head osteonecrosis.
Patients and methods We studied hips in 41 patients (mean age 48 (25–63) years) with a cementless hip arthroplasty after late stage osteonecrosis. Clinical evaluation was by the Harris hip score, the WOMAC score and the SF-36 score. Stem subsidence was measured with the Ein Bild Roentgen Analyse femoral component analysis (EBRA-FCA) at 3, 12, 24, 60, and 72 months after operation. The average duration of follow-up was 7(1–9) years, with less than 2 years for 2 patients.
Results There was no revision of any hip. No radiographic or clinical stem loosening was seen. After 60 months, the cementless stems showed a median subsidence of –0.7 mm (95% CI: –0.9 to –0.2). No femoral osteolysis occurred. Femoral radiolucent lines, all < 1 mm, were seen in 10 hips. At the latest follow-up the Harris hip score was 83 (23–100) points.
Interpretation Our findings for porous-coated stems in patients with femoral osteonecrosis indicate no greater risk of stem subsidence and rate of osteolysis after an average of 7 years follow-up. Thus, we continue to use uncemented stems in younger patients with femoral osteonecrosis. However, continued follow-up will be necessary to evaluate the long-term outcome.
Severe osteonecrosis of the femoral head is usually treated by total hip replacement (THR) (Mont and Hungerford Citation1995, Lee et al. Citation2004). However, the outcomes reported have not been as good as in patients with osteoarthritis. One explanation may be that patients with osteonecrosis of the femoral head are often younger and more active (Saito et al. Citation1989, Ortiguera et al. Citation1999). Another explanation may be that etiological factors of the osteonecrosis, such as steroid use and alcohol abuse, are associated with poor bone stock and potentially poor device fixation (Sarmiento et al. Citation1990, Brinker et al. Citation1994, Radl et al. Citation2005). Measurement of stem subsidence is an accepted tool for evaluation of the quality of implant fixation whereas early migration indicates subsequent implant failure (Kobayashi et al. Citation1997, Biedermann et al. Citation1999).
To our knowledge there has been no study published that has investigated the quality of fixation of a porous-coated stem in patients with osteonecrosis. Thus, we reviewed the clinical and radiographic results of cementless THR in younger patients with femoral head osteonecrosis and measured stem subsidence by the Ein Bild Roentgen Analyse femoral component analysis (EBRAFCA).
Patients and methods
Between 1992 and 1998, 41 patients (41 hips, mean age 48 (25–63) years, 35 men) with advanced osteonecrosis stages III–IV (Ficat Citation1985) received a cementless THR at our institution.
The presumed cause of osteonecrosis was alcohol abuse in 19 patients, steroid use in 7 patients and unknown in 15 hips. The cementless THRs were done with the porous-coated bicontact stem (Aesculap, Tuttlingen, Germany) with the Harris Galante I cup (Zimmer, Warsaw, IN) in 33 cases, the Duraloc cup (DePuy, Warsaw, IN) in 4 cases, the Fitek cup (Protek, Winterthur, Switzerland) in 2 cases, and the Plasma cup (Aesculap, Tuttlingen, Germany) in 2 cases. Acetabular components were secured with 1–4 screws. In these cementless THRs we used a 28-mm femoral ceramic head (Biolox, CeramTec, Plochingen, Germany) in 39 cases and a 32-mm head (Biolox) in 2 cases. The bicontact cementless stems included the following sizes: 9 (n 1), 10 (n 2), 11 (n 1), 12 (n 6), 13 (n 9), 14 (n 9), 15 (n 6), 16 (n 4), 17 (n 2), and 18 (n 1).
We used the transgluteal approach in all cases (Bauer et al. Citation1979). The patients were mobilized with partial weight bearing during the first 6 weeks after the operation.
Clinical evaluations included standardized patient questionnaires and clinical information sheets (Johnston et al. Citation1990). The Harris hip score, the modified Western Ontario and McMaster Universities disease-specific questionnaire (WOMAC) (Stucki et al. Citation1996) and the Medical Outcomes Study 36-Item Short Form Health Survey (SF36) (Bullinger Citation1995) were performed at the latest follow-up. At scheduled postoperative visits (3, 12, 24, 60, and 72 months after operation) standardized radiographs (anterioposterior, lateral) of the hip were obtained. The follow-up period was on average 6.5 (1–9.3) years, and 2 patients were followed up for less than 2 years. No patient was lost to follow-up.
Analyses of ectopic ossifications (Brooker et al. Citation1973) and of radiolucent lines and osteolysis at the femoral component were performed by two independent observers. Osteolytic lesions were documented and classified on the basis of their size and their location (Gruen regions) according to previously published criteria (Zicat et al. Citation1995). Scalloping, geographic loss of either cortical or trabecular bone was considered to be osteolysis (Hartley et al. Citation2000).
Anteroposterior and lateral radiographs of the hips were digitized using an Optotech scanner (DD10; Optotech, Hannover, Germany). The Ein Bild Roentgen Analyse femoral component analysis (EBRA-FCA) was used for analysis of migration (Biedermann et al. Citation1999). This method has shown a specifity of 100% and a sensitivity of 78% compared to radiostereometric analysis (RSA) for the detection of migration of over 1 mm (Krismer et al. Citation1999, Biedermann et al. Citation1999). All patients gave informed consent and the study was approved by our Institutional Review Board.
Statistics
Data were evaluated with the software SPSS 12.0 for Windows. We used Student's t-test and the Wilcoxon test for subsidence analysis. A p-value of less than 0.05 was regarded as showing statistical significance.
Results
No hips were revised during the follow-up period. In 1 patient, a deep vein thrombosis occurred postoperatively.
Radiographic results
No femoral osteolysis was seen; 10/41 hips showed radiolucent lines of < 1 mm, but none < 1 mm. On the anteroposterior radiographs, radiolucent lines were present in 1 hip in Gruen region I, in 6 hips in region III, in 2 hips in region IV, in 8 hips in region V, and in 1 hip in regions VI and VII. None of the stems were considered loose. Ectopic ossification of Brooker grade I occurred in 11 hips, and of grade II in 4 hips.
EBRA-FCA
The median migration was measured at 3, 12, 24, 60, and 72 months after operation. All hips could not be measured at each follow-up control because their radiographs were not accepted by the software because of failed standardization ().
Number of hips measured by EBRA at each time point
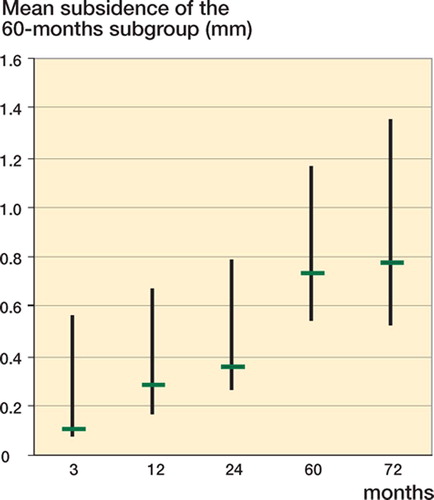
The median subsidence was –0.1 mm (95% CI –0.5 to –0.1) at 3 months after operation and –0.7 mm (95% CI: –0.9 to –0.2) at 60 months after operation (). In a subgroup of 22 patients with a minimum of 5 years follow-up and EBRA examinations that could be analyzed at each follow-up visit, the subsidence was –0.1 mm (95% CI –0.6 to –0.1) 3 months postoperatively and –0.7 mm (95% CI –1.2 to –0.5) after 5 years ().
Figure 1. Mean subsidence in mm, and the 95% confidence interval of the complete group (n = 41) (p < 0.01 at each time point vs. others).
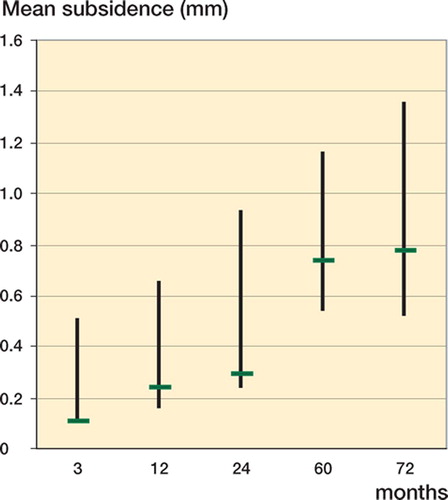
Figure 2. Mean subsidence in mm, and the 95% confidence interval of the subgroup with minimum 60 months of follow-up (n = 22) (p < 0.01 at each time vs. others).
The power to detect a difference in migration was 0.85 for the 3-month vs. 5-year subsidence values. In the 5-year subgroup, the power was 0.74 for the 3-month vs. 5-year values.
1 patient had a migration over 2 mm. The migration after 3, 12, 24 and 60 months was –2.7, –2.8, –3.0, –3.2 mm, respectively. This patient remained asymptomatic at the time of final follow-up at 7 years.
Clinical results
The average Harris hip score was 40 (24–64, SD 10) preoperatively and 83 (23–100, SD 19) at the latest follow-up (p < 0.05).
At the latest follow-up, the overall WOMAC score was 2.0 points (SD 2.6); for pain it was 1.8 (SD 2.7) and for function it was 2.0 (SD 2.6) points. At the latest follow-up, the SF-36 score for the mean somatic and psychiatric subgroups was 40 (SD 13) and 53 (SD 9), respectively.
Discussion
Stem subsidence of 1–2 mm has been considered to be a significant implant migration (Nistor et al. Citation1991, Kärrholm and Snorrason Citation1993, Kärrholm et al. Citation1994). Subsidence of 2 mm or more in 2 years has been found to be predictive of implant failure within 5 years in hip surface arthroplasties (Beaule et al. Citation2005). Several studies using the EBRA have demonstrated clearly that early migration predicts implant failure with high accuracy (Walker et al. Citation1995, Kobayashi et al. Citation1997, Biedermann et al. Citation1999). In order to evaluate the fixation of cementless porous-coated stems in patients with osteonecrosis, we investigated 41 patients (41 hips) and compared our results with those of previously published studies dealing with cementless stems over a comparable follow-up time (Fye et al. Citation1998, Hartley et al. Citation2000, Kim et al. Citation2003, Radl et al. Citation2005). We have been able to demonstrate that cementless fixed stems in younger patients show an excellent clinical and radiographic outcome. The EBRA demonstrated a mean stem subsidence of –0.29 mm 24 months postoperatively and of –0.7 mm at 60 months. No osteolysis was documented; no radiolucent lines of < 1 mm were seen around the stems. No revisions of the acetabular and femoral components were performed during an average follow-up of 6.5 years.
Poor bone stock in patients with osteonecrosis may be responsible for limited osseointegration, with subsequent migration of cementless stems (Sarmiento et al. Citation1990, Brinker et al. Citation1994, Radl et al. Citation2005). To our knowledge, there has been only one published study which measured stem migration in order to evaluate stem stability in patients with osteonecrosis. Radl et al. (Citation2005) investigated stem migration with EBRA and compared the outcome of 31 and 49 cementless hydroxyapa-tite-coated femoral components in osteonecrosis and osteoarthritis patients, respectively. The mean follow-up time was 6 years. They found a poor outcome and increased subsidence of mean –1.5 (-8.8–0) mm for hydroxyapatite-coated stems in patients with femoral osteonecrosis, as compared to –0.6 (-2.8–0.7) mm for the osteoarthritis group. Survivorship analysis with stem revision as the endpoint was 74% in the osteonecrosis group and 98% in the osteoarthritis group at 7.5 years. A poor bone quality associated with the underlying diagnosis was considered to be responsible for this outcome. Thus, Radl et al. recommended a close monitoring of patients with osteonecrosis, including subsidence measurements.
Our data do not confirm the results of that study, despite equal follow-up time and equivalent measurement tools. In contrast to our study, they used hydroxyapatite-coated stems. This type of implant fixation (hydroxyapatite vs. porous coating) may have influenced subsidence and the rate of osteolysis, which was 17% in the study of Radl et al. (Citation2005). However, in our study group we did not find any scalloping osteolysis in the Gruen regions—despite an identical definition of osteolysis. We could not assess the role of subsidence and osteolysis in implant failure since no implant failed in our study group.
The use of cementless implants in patients with osteonecrosis is under debate. One study reported osteolysis in 6 patients and revision in 1 of 35 cementless hips in patients with osteonecrosis after a mean follow-up of 7.5 years (Piston et al. Citation1994). Hartley et al. (Citation2000) were concerned about the rate of revision (21%) in their series of cementless THRs in patients with osteonecrosis. Another study (Kim et al. Citation2003) investigated 50 patients with bilateral osteonecrosis and 48 patients with unilateral osteonecrosis. The patients with bilateral osteonecrosis received a cemented and a cementless THR, while the cases with unilateral disease received a cementless THR. The mean age at the time of surgery was 47 years. The average followup was 9 years. No component had aseptic loosening in either group. The prevalence of osteolysis of the femur was 16% in the group treated with cement and 24% in the group treated without cement. The uncemented THRs were implanted with cobalt-chromium heads (22 mm), as opposed to zirconia heads in the cemented THRs. In contrast, Fye et al. (Citation1998) reported a good-to-excellent outcome at the final follow-up of 7 years in 94% of 72 hips. However, the rate of osteolysis was 2% and the mechanical failure rate of the stems was 6%—which is similar to our results.
Our data on porous-coated stems in patients with femoral osetonecrosis indicate no greater risk of stem subsidence and no higher rate of osteolysis. The long-term outcome is unknown, however.
No competing interests declared.
Contributions of authors
AI was the main investigator and took part in evaluation, interpretation of data, coordination of the study, study design, literature research, and preparation of the manuscript. JL and SG took part in evaluation of the data and literature search, and were in charge of patient visits. NW performed statistical analysis, and took part in evaluation of the data and in study design. CH supervised the study and took part in study design and evaluation of the data; he also performed most of the surgery.
- Bauer R, Kerschbaumer F, Poisel S, Oberthaler W. The transgluteal approach to the hip joint. Arch Orthop Trauma Surg 1979; 95: 47–9
- Beaule P E, Krismer M, Mayrhofer P, Wanner S, Le Duff M, Mattesich M, Stoeckl B, Amstutz H C, Biedermann R. EBRA-FCA for measurement of migration of the femoral component in surface arthroplasty of the hip. J Bone Joint Surg (Br) 2005; 87: 741–4
- Biedermann R, Krismer M, Stockl B, Mayrhofer P, Ornstein E, Franzen H. Accuracy of EBRA-FCA in the measurement of migration of femoral components of total hip replacement. Einzel-Bild-Rontgen-Analyse-femoral component analysis. J Bone Joint Surg (Br) 1999; 81: 266–72
- Brinker M R, Rosenberg A G, Kull L, Galante J O. Primary total hip arthroplasty using noncemented porous-coated femoral components in patients with osteonecrosis of the femoral head. J Arthroplasty 1994; 9: 457–68
- Brooker A F, Bowerman J W, Robinson R A, Riley L H, Jr. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg (Am) 1973; 55: 1629–32
- Bullinger M. German translation and psychometric testing of the SF-36 Health Survey: preliminary results from the IQOLA Project International Quality of Life Assessment. Soc Sci Med 1995; 41: 1359–66
- Ficat R P. Idiopathic bone necrosis of the femoral head. Early diagnosis and treatment. J Bone Joint Surg (Br) 1985; 67: 3–9
- Fye M A, Huo M H, Zatorski L E, Keggi K J. Total hip arthroplasty performed without cement in patients with femoral head osteonecrosis who are less than 50 years old. J Arthroplasty 1998; 13: 876–81
- Hartley W T, McAuley J P, Culpepper W J, Engh C A, Jr, Engh C A, Sr. Osteonecrosis of the femoral head treated with cementless total hip arthroplasty. J Bone Joint Surg (Am) 2000; 82: 1408–13
- Johnston R C, Fitzgerald R H, Jr, Harris W H, Poss R, Muller M E, Sledge C B. Clinical and radiographic evaluation of total hip replacement. A standard system of terminology for reporting results. J Bone Joint Surg (Am) 1990; 72: 161–8
- Kärrholm J, Snorrason F. Subsidence, tip, and hump micromovements of noncoated ribbed femoral prostheses. Clin Orthop 1993, 287: 50–60
- Kärrholm J, Borssen B, Lowenhielm G, Snorrason F. Does early micromotion of femoral stem prostheses matter? 4-7-year stereoradiographic follow-up of 84 cemented prostheses. J Bone Joint Surg (Br) 1994; 76: 912–7
- Kim Y H, Oh S H, Kim J S, Koo K H. Contemporary total hip arthroplasty with and without cement in patients with osteonecrosis of the femoral head. J Bone Joint Surg (Am) 2003; 85: 675–81
- Kobayashi A, Donnelly W J, Scott G, Freeman M A. Early radiological observations may predict the long-term survival of femoral hip prostheses. J Bone Joint Surg (Br) 1997; 79: 583–9
- Krismer M, Biedermann R, Stockl B, Fischer M, Bauer R, Haid C. The prediction of failure of the stem in THR by measurement of early migration using EBRA-FCA. Einzel-Bild-Roentgen-Analyse-femoral component analysis. J Bone Joint Surg (Br) 1999; 81: 273–80
- Lee S B, Sugano N, Nakata K, Matsui M, Ohzono K. Comparison between bipolar hemiarthroplasty and THA for osteonecrosis of the femoral head. Clin Orthop 2004; 5(424)161–5
- Mont M A, Hungerford D S. Non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg (Am) 1995; 77: 459–74
- Nistor L, Blaha J D, Kjellstrom U, Selvik G. In vivo measurements of relative motion between an uncemented femoral total hip component and the femur by roentgen stereophotogrammetric analysis. Clin Orthop 1991, 269: 220–7
- Ortiguera C J, Pulliam I T, Cabanela M E. Total hip arthroplasty for osteonecrosis: matched-pair analysis of 188 hips with long-term follow-up. J Arthroplasty 1999; 14: 21–8
- Piston R W, Engh C A, De Carvalho P I, Suthers K. Osteonecrosis of the femoral head treated with total hip arthroplasty without cement. J Bone Joint Surg (Am) 1994; 76: 202–14
- Radl R, Hungerford M, Materna W, Rehak P, Windhager R. Higher failure rate and stem migration of an uncemented femoral component in patients with femoral head osteonecrosis than in patients with osteoarthritis. Acta Orthop Scand 2005; 76: 49–55
- Saito S, Saito M, Nishina T, Ohzono K, Ono K. Long-term results of total hip arthroplasty for osteonecrosis of the femoral head. A comparison with osteoarthritis. Clin Orthop 1989, 244: 198–207
- Sarmiento A, Ebramzadeh E, Gogan W J, McKellop H A. Total hip arthroplasty with cement. A long-term radiographic analysis in patients who are older than fifty and younger than fifty years. J Bone Joint Surg (Am) 1990; 72: 1470–6
- Stucki G, Meier D, Stucki S, Michel B A, Tyndall A G, Dick W, Theiler R. Evaluation of a German version of WOMAC (Western Ontario and McMaster Universities) Arthrosis Index. Z Rheumatol 1996; 55: 40–9
- Walker P S, Mai S F, Cobb A G, Bentley G, Hua J. Prediction of clinical outcome of THR from migration measurements on standard radiographs. A study of cemented Charnley and Stanmore femoral stems. J Bone Joint Surg (Br) 1995; 77: 705–14
- Zicat B, Engh C A, Gokcen E. Patterns of osteolysis around total hip components inserted with and without cement. J Bone Joint Surg (Am) 1995; 77: 432–9