Abstract
Background Concurrent head-to-head comparisons of healthcare interventions regarding cost-utility are rare. The concept of favorable cost-effectiveness of total hip or knee arthroplasty is thus inadequately verified.
Patients and methods In a trial involving several thousand patients from 10 medical specialties, 223 patients who were enrolled for hip or knee replacement surgery were asked to fill in the 15D health-related quality of life (HRQoL) survey before and after operation.
Results Mean (SD) HRQoL score (on a 0–1 scale) increased in primary hip replacement patients (n = 96) from 0.81 (0.084) preoperatively to 0.86 (0.12) at 12 months (p < 0.001). In revision hip replacement (n = 24) the corresponding scores were 0.81 (0.086) and 0.82 (0.097) respectively (p = 0.4), and in knee replacement (n = 103) the scores were 0.81 (0.093) and 0.84 (0.11) respectively (p < 0.001). Of 15 health dimensions, there were statistically significant improvements in moving, usual activities, discomfort and symptoms, distress, and vitality in both primary replacement groups. Mean cost per quality-adjusted life year (QALY) gained during a 1-year period was € 6,710 for primary hip replacement, € 52,274 for revision hip replacement, and € 13,995 for primary knee replacement.
Interpretation Hip and knee replacement both improve HRQoL. The cost per QALY gained from knee replacement is twice that gained from hip replacement.
The positive effect of hip and knee replacement surgery on health-related quality of life (HRQoL) is well established (Rissanen et al. Citation1995, Dawson et al. Citation1996, Norman-Taylor et al. Citation1996, Rissanen et al. Citation1996, Towheed and Hochberg Citation1996). In addition, several studies have suggested that total hip arthoplasty (THA) and total knee arthoplasty (TKA) are more cost-effective than many other healthcare interventions (Laupacis et al. Citation1994, James et al. Citation1996, Rissanen et al. Citation1997, Garellick et al. Citation1998, O'shea et al. Citation2002, Segal et al. Citation2004). The estimates of cost-effectiveness, however, have usually been based on results of individual studies comparing only two or a few interventions at a time. Concurrent head-to-head comparisons of several routine healthcare interventions regarding cost-utility in an everyday setting are rare and, consequently, the concept of favorable cost-utility of THA or TKA, compared to many other interventions, is still on a relatively unstable basis.
Our hospital, a large university referral clinic providing secondary and tertiary healthcare services for a population of approximately 1.4 million inhabitants in Southern Finland, has been running a large trial exploring the feasibility of evaluating the utility of routine services since 2002 (Räsänen et al. Citation2005). Data on HRQoL, before and after interventions, are available from several thousands patients for more than 30 medical entities. This approach enables routine estimation of the number of quality-adjusted life years (QALY) gained by various treatments, and thus provides a measure of utility which is a broader concept of the benefit of health care and takes into account individuals preferences. For example, the National Institute for Clinical Excellence uses QALY as the principal measure of health outcome in the National Health Service of England and Wales (Rawlins and Culyer Citation2004). Furthermore, when combined with costs of providing treatment, available from the hospital accounting records, our approach also enables routine comparison of the cost-utility of services offered for the patients. Such data are essential in order to be able to ensure that healthcare is effective and that available resources are allocated to treatments that have been shown to be cost-effective.
This study explores the cost-utility of hip and knee arthroplasty relative to that of a nonoperative strategy, and compares their cost-effectiveness with that of some other common interventions analyzed so far in our project.
Patients and methods
385 consecutive patients entering scheduled hospital treatment in orthopedics between March 2002 and August 2002 were invited to participate and fill in the 15D HRQoL questionnaire. Approximately 6 and 12 months after the operation, a follow-up questionnaire was mailed to all patients who had returned the first questionnaire. Complete data for analysis were available from 279 patients.
In 56/279 cases, the type of the intervention performed was not hip or knee replacement or the patient had returned only one of the two postoperative questionnaires. As we were specifically interested in the cost-utility of THA and TKA, these patients were excluded from further analysis. The remaining 223 cases consisted of 96 primary THAs (11 not using cement, 36 using hybrid technique, 47 using cement, 2 requiring prosthetic replacements), 24 secondary hip operations (14 secondary implantations without bone grafting, 3 repairs with allogenic bone grafts to the femur, 4 with allogenic grafts to the acetabulum, and 3 with grafts around both components) and 103 primary TKAs (101 cemented condylar designs, most of them without patellar component, and 2 demi-prostheses).
Utility of interventions
HRQoL was measured by the 15D HRQoL-instrument (Sintonen Citation1995, Citation2001). It is a generic, 15dimensional, standardized self-administered HRQoL instrument that can be used both as a profile and a single-index score measure. The 15 dimensions are: moving, seeing, hearing, breathing, sleeping, eating, speech, eliminating, usual activities, mental function, discomfort and symptoms, depression, distress, vitality, and sexual activity. For each dimension, the respondent must choose one of the 5 levels that best describes his/ her state of health at the moment (the best level being 1 and the worst level being 5). The valuation system of the 15D is based on an application of the multi-attribute utility theory. A set of utility or preference weights, obtained from the general public through a 3-stage valuation procedure, is used in an additive aggregation formula to generate the utility score, i.e., the 15D score (single index number) over all the dimensions (for details, see http://www.15d-instrument.net/15D). The maximum score is 1 (no problems in any dimension) and the minimum score is 0 (being dead). The minimally important difference (MID) ≥ 0.03 is considered clinically significant or important (Sintonen 1994). In most of the important properties, the 15D compares favorably with other instruments of this kind (Stavem Citation1999, Hawthorne et al. Citation2001, Sintonen Citation2001).
In addition to HRQoL, outcomes in the orthopedic patients were measured by two commonly used disease-specific measures, the Harris hip score (HHS) (Harris Citation1969, Söderman and Malchau Citation2001) and the Knee Society score (KSS) (Insall et al. Citation1989, The Knee Society Citation2005), at baseline and at 12 months postoperatively.
Cost-utility
The standpoint taken for the analysis was that of the healthcare provider. Direct hospital costs were obtained from the Ecomed clinical patient administration system (Datawell Ltd., Finland), where all costs of hospital treatment of individual patients are stored on a routine basis. The summary costs used for analysis covered all relevant specialtyrelated costs (operation, ward, ambulatory visits, laboratory, radiology, pathology) including pre- and postoperative outpatient visits to the hospital from baseline to 12 months. Indirect costs, such as period of disability, were not included.
In the great majority of the patients the indication for operation was arthritis, which does not significantly affect average life expectancy. The HRQoL gain representing the utility of the intervention was thus assumed to last until the end of the remaining statistical life expectancy of each patient (Statistical Yearbook of Finland Citation2003). Although this is not strictly true, as HRQoL of arthroplasty patients deteriorates over the years as symptoms recur, this approach is typically used for the calculation of QALYs gained by medical interventions, and dividing mean costs by the mean number of QALYs gained gives an estimate of cost-utility in the form of cost per QALY. QALYs were calculated using the 12-month effectiveness and cost data. As the gain from treatment is expected to last for many years, whereas the costs accrued during the study period, the number of QALYs are also reported using a discount rate of 5%. Sensitivity analyses were performed varying the discount rate between 1–5%, using the median values of QALY gain and costs, and using the upper and lower values of the 95% confidence interval (CI) for the mean differences in effectiveness of treatment (HRQoL change) and costs.
Ethics
All patients received previously scheduled routine treatment and besides being asked to fill in the 15D questionnaire and to give a written informed consent, were not approached in any other way. The study protocol was approved by the Ethical Committee of the Helsinki and Uusimaa Hospital District on February 4, 2002 (registration number 26/E6/02).
Statistics
Data were analyzed using SPSS for Windows statistical software version 11.0. The results are given as mean and standard deviation (SD), or as percentages. The significance of the differences between baseline and 12-month follow-up HRQoL scores was analyzed with Student's paired t-test for dependent samples. When comparing percentage distributions between the groups, Chi-square test was used. P-values less than 0.05 were considered statistically significant.
Results
Of the 96 primary THA patients (mean age 63 (12) years, 60 females), 72 had primary arthritis, 7 had inflammatory joint disease, 6 posttraumatic or other secondary arthritis, 8 congenital hip abnormality, and 3 had idiopathic or drug-induced aseptic bone necrosis. Of the 24 revision hip replacement patients (mean age 69 (10) years, 12 females), 2 had primary arthritis, 17 had mechanical complications of an earlier prosthesis, 2 inflammatory joint disease, 2 posttraumatic or other secondary arthritis, and 1 had trauma sequelae as the primary diagnosis. In the 103 TKA patients (mean age 69 (11) years, 77 females), the primary diagnosis was primary arthritis in 93 patients, inflammatory joint disease in 4 patients, posttraumatic or other secondary arthritis in 4, mechanical complications of an earlier prosthesis in 1, and Wegener's granulomatosis in 1 patient.
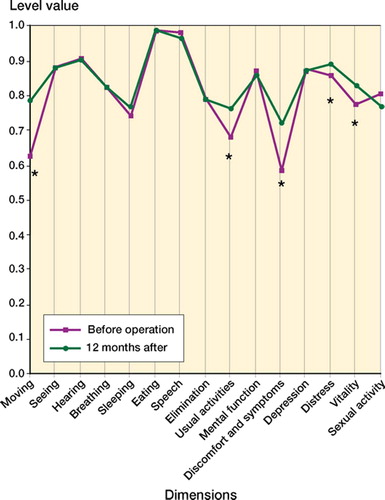
In all groups mean utility score (on a 0–1 scale) had improved, relative to baseline, at both the 6- and 12-month follow-up () but the improvement was not statistically significant in the revision hip replacement group at 12 months. Of the 15 dimensions of health covered by the HRQoL instrument, moving, usual activities, discomfort and symptoms, distress and vitality all improved in a statistically significant manner in both primary replacement groups, whereas the revision operation improved only the dimension moving ().
Figure 1. The 15 dimensions of the 15D instrument before primary hip replacement and 12 months afterwards (*denotes significant improvement from baseline at the p < 0.05 level).
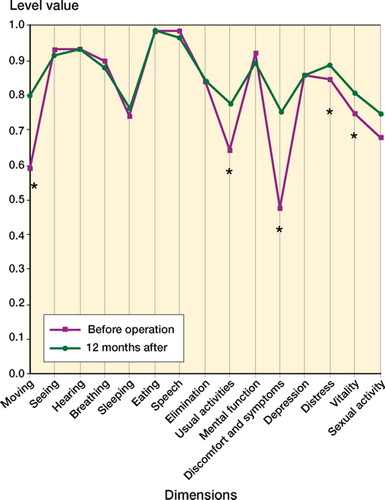
Table 1. Health-related quality of life (HRQoL) and cost data. Values are percentages or means with standard deviations (SD) in parentheses
Those with a favorable result from primary THA (≥ 0.03 increase in the HRQoL score) were significantly younger than patients with a less optimal result (). In primary TKA patients, only shorter waiting time was significantly associated with favorable outcome ().
Table 2. Characteristics of the primary total hip arthroplasty (THA) and primary total knee arthroplasty (TKA) patients whose health-related quality of life (HRQoL) improved in a clinically significant manner (improvement ≥ 0.03 at 12 months) compared to those with little or negative change (HRQoL change < 0.03). Values are percentages or means with standard deviations (SD) in parentheses
Mean HHS score of the primary THA patients before operation was 51 (16) and that of the revision patients was 47 (21). 12 months after the operation, the scores had increased to 81 (33) (p < 0.001) and 74 (35) (p = 0.005), respectively. KSS of the primary TKA patients before operation was 43 (17) and had increased to 88 (27) at 12 months (p < 0.001).
The mean direct hospital costs of primary THA and TKA were fairly similar, but the mean cost of revision hip replacement operations was clearly higher (). The cost per QALY gained was lowest in the primary THA group, followed by primary TKA and revision THA ().
Figure 2. The 15 dimensions of the 15D instrument before revision hip replacement and 12 months afterwards (*denotes significant improvement from baseline at the p < 0.05 level).
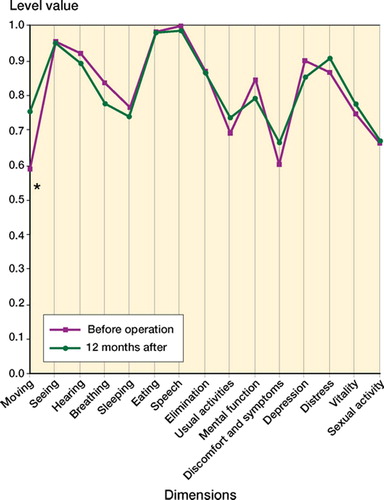
Figure 3. The 15 dimensions of the 15D instrument before knee replacement surgery and 12 months afterwards (*denotes significant improvement from baseline at the p < 0.05 level).
In sensitivity analysis the cost per QALY gained in primary THA ranged from € 4,767 to € 12,340, and that for primary TKA ranged from € 9,874 to 24,021 depending on the assumptions used in the analysis (). Revision hip replacement, if effectiveness was at the lower 95% CI level of the mean observed in the study, would produce a negative QALY gain—precluding the calculation of cost per QALY. By contrast, if effectiveness of revision hip replacement would be at the higher 95% CI level of the mean observed, the cost per QALY, although still being rather high, would sink to € 19,857.
Table 3. Cost-utility analysis: base case and sensitivity analyses (SA) varying the discount rate between 1% and 5%, using median values, and using the upper and lower values of the 95% confidence interval (CI) for the mean differences in treatment effectiveness (improvement in health-related quality of life) and costs. See for explanation of abbreviations
Discussion
Our results confirm earlier findings employing both diseases-specific and generic outcome measures that primary THA and TKA are both effective interventions in improving the HRQoL of patients in a statistically significant manner. The improvement was also of clinical value, as a 0.03 point increase in the 15D score is considered clinically important. As one might expect, significant improvements were found in both primary replacement groups for the dimensions moving and discomfort and symptoms—but also for the dimensions distress, usual activities, and vitality. A clear improvement was also seen in all groups studied using the HHS and KSS disease-specific measures of outcome.
From our data, the cost per QALY gained in primary THA was € 6,710. This is approximately the same as that reported earlier by Segal et al. (Citation2004), but higher than that reported by O'shea et al. (Citation2002). In the latter study HRQoL was, however, assessed by the SF-36 HRQoL instrument, which does not allow reliable calculation of QALYs. A relatively low cost per QALY was also found by James et al. (Citation1996) using the EuroQol HRQoL instrument, but using the Rosser-Index the cost per QALY was 4–8 times higher. In some other studies dating back to the 1990s, the cost of THA per QALY was reported to range from approximately 20,000 US dollars (Laupacis et al. Citation1994) to approximately 32,000 US dollars (Garellic et al. 1998). In the latter study, however, effectiveness was determined using the Nottingham Health Profile, which is not a valid measure for calculating QALYs.
In our hands, the cost per QALY gained in revision hip replacement was 52,274 but the number of revision patients in the study was low, thus precluding solid conclusions about the cost-utility of revision hip replacement surgery.
Knee replacement surgery, although also effective in relieving symptoms and discomfort, did this in our patients at a clearly higher price (€ 13,995 per QALY gained) than hip replacement surgery. This price is also somewhat higher than some earlier estimates (James et al. Citation1996, Lavernia et al. Citation1997, Segal et al. Citation2004). The study by Segal et al., in contrast to ours, was based on conversion of commonly used osteoarthirits outcome scales into a utility-equivalent scale, which may explain the discrepancy between their results and ours.
The major strength of our study is that it reports the cost-utility of THA and TKA in the context of routine follow-up of a large number of interventions performed in a real-world setting in our hospital. Consequently, unlike the situation in many clinical trials, the findings are based on unselected patient material and thus reflect results obtained in normal practice—corresponding to the true everyday effectiveness of treatments. The approach taken is in agreement with the standpoint that economic evaluations are more valid, if effectiveness data reflects normal practice as closely as possible (Bozic et al. Citation2003). Another strength of our study is that the estimate of utility is based on a patientreported outcome. Traditionally, evaluations of medical therapy have used objective endpoints with little relevance to how patients have been affected by the treatment (Bourne et al. Citation2004). However, in the case of THA for example, the use of selfadministered patient questionnaires together with traditional physician-generated assessment may provide a better evaluation of the results (Lieberman et al. Citation1996).
We estimated the cost per QALY from the point of view of the healthcare provider, as only direct hospital costs were included in the analysis. This may be seen as a limitation, as it is well known that patients with hip or knee disorders requiring arthroplasty often also need additional services such as medication, transportation, or help in everyday tasks. The costs of hospital treatment, however, certainly make up the bulk of the total costs of treatment of hip and knee disorder patients (Rissanen et al. Citation1997). Thus, the method of using cost data that are readily available from the hospital accounting system instead of tediously collecting data from individual patients can be defended, and is in fact—in a trial involving several thousand patients—the only feasible way of acquiring reasonably reliable cost data.
Another limitation may be the fact that in the present cost-utility analyses, the comparator to operative treatment was nonoperative treatment with the assumption that HRQoL remains constant over time. This is not always true, as symptoms can often also be relieved, and HRQoL improved, by nonoperative treatment. On the other hand, in many possible arthroplasty candidates HRQoL tends to deteriorate fairly rapidly, which may cancel the positive effects of nonoperative treatment and justify the approach taken in our analysis.
Compared to some other interventions studied in our project so far, the cost per QALY gained in hip replacement surgery was similar to that in angioplastic treatment of coronary heart disease. However, compared to disc herniation surgery, hip replacement surgery was 2–3 times more expensive in relation to the benefit experienced by the patients. Knee replacement surgery is clearly a less cost-effective procedure. However, even the costs per QALY gained in knee replacement surgery can be considered acceptable, as they were clearly below the commonly used threshold level for the cost per QALY (30,000–50,000) and lower than those found in our material for coronary by-pass operations, for example.
The authors are indebted to the patients and staff of the Department of Orthopedic Surgery of Helsinki University Hospital. The invaluable contributions of Professor Pekka Laippala (who died on May 13, 2003) during the early phases of the project are gratefully acknowledged. The study was funded by research grants from the Helsinki and Uusimaa Hospital Group.
No competing interests declared.
Contributions of authors
PR, PP, HS and RPR: contributed to the design of the study, analysis of the results and writing of the manuscript. A-MK: contributed to the analysis of the results and writing of the manuscript. O-PR and MB: contributed to the design of the study and writing of the manuscript.
- Bourne R B, Maloney W J, Wright J G. An AOA (The American Orthopaedic Association) critical issue. The outcome of the outcomes movement. J Bone Joint Surg (Am) 2004; 86: 633–40
- Bozic K J, Rosenberg A G, Huckman R S, Herndon J H. Economic evaluation in orthopedics. J Bone Joint Surg (Am) 2003; 85: 129–42
- Dawson J, Fitzpatric R, Murray D, Carr A. Comparison of measures to assess outcomes in total hip replacement surgery. Qual Health Care 1996; 5: 81–8
- Garellick G, Malchau H, Herberts P, Hansson E, Axelsson H, Hansson T. Life expectancy and cost utility after total hip replacement. Clin Orthop 1998, 346: 141–51
- Harris W H. Traumatic arthritis of the hip after dislocation and acetabular fractures: Treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg (Am) 1969; 51: 737–55
- Hawthorne G, Richardson J, Day N A. A comparison of the Assessment of Quality of Life (AQoL) with four other generic utility instruments. Ann Med 2001; 33: 358–70
- Insall J N, Dorr L D, Scott R D, Scott W N. Rationale of The Knee Society clinical rating system. Clin Orthop 1989, 248: 13–4
- James M, St Leger S, Roswell K V. Prioritising elective care: a cost utility analysis of orthopaedics in the north west of England. J Epidemiol Community Health 1996; 50: 182–9
- The Knee Society. 2005, http://www.kneesociety.org/knee_outcomes.cfm
- Laupacis A, Bourne R, Robareck C, Feeny D, Wong C, Tugwell P, Leslie K, Bullas R. Costs of elective total hip arthroplasty during the first year. Cemented versus noncemented. J Arthroplasty 1994; 9: 481–7
- Lavernia C J, Guzman J F, Gachupin-Garcia A. Cost effectiveness and quality of life in knee arthroplasty. Clin Orthop 1997, 345: 134–9
- Lieberman J R, Dorey F, Shekelle P, Schumacher L, Thomas B J, Kilgus D J, Finerman G A. Differences between patients' and physicians' evaluations of outcome after total hip arthroplasty. J Bone Joint Surg (Am) 1996; 78: 835–8
- Norman-Taylor F H, Palmer C R, Villar R N. Quality-of-life improvement compared after hip and knee replacement. J Bone Joint Surg (Br) 1996; 78: 74–7
- O'shea K, Bale E, Murray P. Cost analysis of primary total hip replacement. Ir Med J 2002; 95: 177–80
- Rawlins M D, Culyer A J. National Institute for Clinical Exellence and its value judgements. BMJ 2004; 329: 224–7
- Rissanen P, Aro S, Slätis P, Sintonen H, Paavolainen P. Health and quality of life before and after hip or knee arthroplasty. J Arthroplasty 1995; 10: 169–75
- Rissanen P, Aro S, Sintonen H, Slätis P, Paavolainen P. Quality of life and functional ability in hip and knee replacements: a prospective study. Qual Life Res 1996; 5: 56–64
- Rissanen P, Aro S, Sintonen H, Asikainen K, Slätis P, Paavolainen P. Costs and cost-effectiveness in hip and knee replacements. A prospective study. Int J Technol Assess Health Care 1997; 13: 575–88
- Räsänen P, Sintonen H, Ryynänen O P, Blom M, Semberg-Konttinen V, Roine R P. Measuring cost-effectiveness of secondary health care: Feasibility and potential utilization of results. Int J Technol Assess Health Care 2005; 21(1)22–31
- Segal L, Day S E, Chapman A B, Osborne R H. Can we reduce disease burden from osteoarthritis?. Med J Aust 2004; 180: S11–7
- Sintonen H. The 15-D measure of health-related quality of life: II Feasibility, reliability and validity of its valuation system. National Center for Health Program Evaluation. National Health and Medical Research Council, Melbourne 1995, Working Paper 42. (http://www.buseco.monash.edu.au/centres/che/pubs/wp42.pdf)
- Sintonen H. The instrument of health-related quality of life: properties and applications. Ann Med 2001; 33: 328–36
- Statistical Yearbook of Finland 2003. Statistics Finland, Helsinki 2003
- Stavem K. Reliability, validity and responsiveness of two multiattribute utility measures in patients with chronic obstructive pulmonary disease. Qual Life Res 1999; 8: 45–54
- Söderman P, Malchau H. Is the Harris Hip Score system useful to study the outcome of total hip replacement. Clin Orthop Rel Res 2001, 384: 189–97
- Towheed T E, Hochberg M C. Health-related quality of life after total hip replacement. Semin Arthritis Rheum 1996; 26: 483–91